Abstract
Vertebral fracture (VFx) is associated with various co-morbidities and increased mortality. In this paper, we have studied the detective value of height loss for VFx using two indices; historical height loss (HHL) which is the difference between the maximal height, and the current height (CH), and CH/knee height (KH) ratio. One-hundred and fifty-one postmenopausal women visiting the outpatient clinic of orthopaedics were studied for their CH, self-reported maximal height, KH, and radiographically diagnosed VFx number(s). VFx was present in 41.1 % of the subjects. Multiple regression analyses revealed that the number of prevalent fractures was a significant predictor of HHL and CH/KH ratio. Receiver operator characteristic curve analysis has shown that for HHL, the area under the curve (AUC) with their 95 %CI in the parentheses was 0.84 (0.77, 0.90), 0.88 (0.83, 0.94), and 0.91 (0.86, 0.96) for ≥1, ≥2, and ≥3 fractures, respectively. For the presence of ≥1 VFx, the cut-off value was 4.0 cm (specificity 79 %; sensitivity 79 %). Regarding the CH/KH ratio, AUC was 0.73 (0.65, 0.82), 0.85 (0.78, 0.93), and 0.91 (0.86, 0.96) for ≥1, ≥2, and ≥3 fractures, respectively. For the presence of ≥1 VFx, the cut-off value was 3.3 (specificity 47 %; sensitivity 91 %). Both cut-off values for HHL and CH/KH ratio had high negative predictivity across the wide range of theoretical VFx prevalence. Thus, HHL and CH/KH were both good detectors of VFx. Our data would be the basis to determine the cut-off value for the screening or case finding of subjects with VFx.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Of the various osteoporotic fractures, vertebral fracture (VFx) is the most prevalent. VFx is associated with various unfavorable consequences. For example, gastroesophageal reflux disease [1], chronic low back pain [2], and impaired respiratory or digestive function are common in those with VFx [3, 4]. Representing such co-morbidities, patients with VFx have impaired quality of life (QOL). Even the morphological fracture, which is incidentally diagnosed by X-ray examination without overt clinical signs or symptoms, is associated with impaired QOL [5–8].
Furthermore, recent studies have shown that VFx is associated with increased mortality [9–12]. In addition, prevalent osteoporotic fracture increases the risk of another fracture by several fold [13–16].
Recently the importance of secondary prevention of osteoporotic fractures is increasingly recognized. In the UK, efforts have been made to deliver appropriate information to such patients in collaboration with the medical staffs. Such a system, called a fracture liaison service, has been proven to be effective in the secondary prevention of osteoporotic fractures [17, 18]. In Japan, similar efforts, called an osteoporosis liaison service, have recently been initiated. Then, of great importance is the case finding of subjects who have sustained an osteoporotic fracture.
VFx is the most problematic, since approximately two-thirds of the VFx patients are without overt clinical symptoms, and a substantial proportion of them are even unaware of their VFx [19, 20]. No doubt BMD measurement by DXA or X-ray examination is useful for the determination of VFx, which, however, would be inappropriate for screening purposes. The screening of subjects with VFx should be done favorably by simple and less costly methods. Since VFx is probably the most important cause of height loss, height measurement can be a good candidate as a tool for the screening of subjects with VFx. The cut-off value of height loss for the prediction of VFx has been reported [20–24], which, however, is almost exclusively limited to the data in Caucasians. Considering the large difference of stature between various nations, such cut-off value must be individually defined for each nation. For this purpose, we have employed the historical height loss (HHL), which was defined as the difference between the maximum height based on the subjects’ recall and the current height (CH), and determined the cut-off value of HHL for the case finding of VFx in the Japanese population.
In the elderly, however, sometimes maximal height or height at youth is unavailable or unreliable. We considered that the ratio of current height (CH) divided by knee height (KH) could be a good alternative to detect VFx, since KH is measurable in most elderly subjects and little affected by aging [25, 26]. Then CH/KH ratio would reflect well the height loss and could be a detector of VFx. Based on these considerations, we have also studied the detective value of CH/KH ratio for VFx, and examined the cut-off value of this index.
Materials and methods
Subjects
The study subjects were 151 patients visiting the outpatient clinic of the Orthopedic Department, Hyogo Medical College. This study was approved by the ethics committee of Sasayama Medical Center, and conforms with the Declaration of Helsinki. Written informed consent was obtained from the subjects after explaining the purpose of this study. Exclusion criteria were as follows: subjects with pre-existing metabolic bone disease, and those with severe skeletal deformities that hinder the anthropometric measurement or the X-ray diagnosis of the skeleton. Consecutive patients meeting such criteria were encouraged to participate in the study. The background profiles of subjects are shown in Table 1.
Measurement of current height and knee height (KH)
CH was measured with a wall-mounted stadiometer. Immediate precision error (expressed as the within-subject standard deviation), 6-month precision, and 12-month precision have been reported to be 0.17, 0.38, and 0.42 cm, respectively [27]. The stadiometer was calibrated prior to each use with a 60-cm rod of a metal alloy resistant to temperature-induced change in length.
KH was measured at a sitting position, with the subject's leg raised, the knee and ankle both at a 90° angle [28].
Maximal height was obtained by the patient's recall. Historical height loss (HHL) was defined as the difference between the maximal height and the CH.
Diagnosis of vertebral fracture (VFx)
The diagnosis of vertebral fracture was made by one of the authors (KY). Lateral and anteroposterior radiographs of the thoracic and lumbar spine were taken, and semi-quantitatively assessed by KY as follows: grade 0, normal; grade 1, a decrease in the height of any vertebra of 20–25 %; grade 2, a decrease of more than 25 % to less than 40 %; grade 3, a decrease of 40 % or more [29, 30].
Statistical analyses
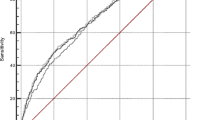
Data were analyzed with SPSS 19.0J. Comparison of the two independent variables was made by Student’s t test or Mann–Whitney test. Multiple regression analyses were performed to identify the independent variables that affect the HHL and CH/KH ratio. The value of the variables for detecting VFx was analyzed using the receiver operator characteristic (ROC) curve. The detective value was evaluated by the area under the curve (AUC) with the larger value indicating the better diagnostic value. The appropriate cut-off value was determined using Youden’s index [31]. Then, with the cut-off value thus determined, the sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and positive likelihood ratio (with 95 %confidence intervals; 95 %CI) were calculated.
Results
Comparison of the characteristics between subjects with fracture and without fracture
The number of subjects without and with VFx was 89 (58.9 %) and 62 (41.1 %), respectively. Those with VFx were older and had lower CH (Table 1). Subjects with VFx had lost more height (7.0 cm; Q1, Q3 4.0, 11.9) than those without VFx (2.0 cm; Q1, Q3 0.8, 3.6). There was a significant difference between subjects with VFx and without it in CH/KH ratio (3.2 ± 0.1 vs 3.4 ± 0.1), which remained significant after adjustment for age (data not shown).
Evaluation of the relationship between historical height loss and prevalent vertebral fracture
By regression analysis, the relationship between HHL and the number of prevalent fractures was defined as: HHL (cm) = 0.17 × age + 1.30 × number of fractures − 8.31 (r 2 = 0.54, p < 0.001). The height loss per each fracture was 1.30 cm with a 95 %CI from 1.04 to 1.55 cm. (data not shown).
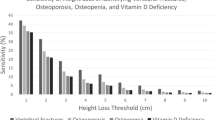
The detective ability and cut-off value of HHL for VFx were evaluated by ROC analysis. For the presence of one or more VFx, AUC was 0.84 (95 %CI, 0.77, 0.90), and the cut-off value was determined to be 4.0 cm with the specificity and sensitivity being 79 % and 79 %, respectively. At the VFx prevalence of 41.1 % in the current study population, PPV and NPV was 71 % (95 %CI, 64, 78) and 85 % (95 %CI, 78, 90), respectively. With HHL ≥ 4.0 cm, the likelihood ratio was 3.61 (95 %CI; 2.54, 4.99).
As shown Table 2, detective values were determined across a wide range of theoretical fracture prevalence that might be encountered in clinical practice by applying the sensitivity and specificity corresponding to HHL ≥ 4.0 cm. The PPV was low across most of the range. In contrast, the NPV remained high at the prevalence rates likely to be encountered in most clinical practice, and dropped below 80 % only at the prevalence exceeding 50 %.
As shown in Table 3, the cut-off values of HHL were 4.0, 4.4, and 6.0 cm for one or more, two or more, and three or more fractures, respectively.
Evaluation of the relationship between CH/KH ratio and prevalent vertebral fracture
Similarly, the relationship between CH/KH ratio and the number of prevalent fractures was defined as: CH/KH ratio = −0.01 × age − 0.03 × number of fractures + 3.74 (r 2 = 0.38, p < 0.001). The CH/KH ratio per fracture was −0.03 with a 95 %CI from −0.04 to −0.02 (data not shown).
The detective value of CH/KH ratio was also studied by ROC analysis. AUC was 0.73 (95 %CI, 0.65, 0.82) for one or more fractures. For the presence of one or more VFx, the cut-off value was determined to be 3.3 with the specificity and sensitivity being 47 and 91 %, respectively. At the VFx prevalence in the current subjects, PPV and NPV were 54 % (95 %CI, 48, 57) and 88 % (95 %CI, 75, 95), respectively. With CH/KH ratio ≤3.3, the likelihood ratio was 1.70 with a 95 %CI from 1.35 to 1.95.
In CH/KH ratio, The PPV was low across most of the range. The NPV remained high at the prevalence rates likely to be encountered in the daily clinical practice (Table 4).
Cut-off value for the detection of various numbers of VFx is shown in Table 5. For detecting two or more, or three or more fractures, a cut-off value of CH/KH ratio was ≤3.2.
Discussion
Recently, “Guideline for the Prevention and Treatment of Osteoporosis 2011” was published in Japan [32], which will be abbreviated as “Guideline 2011” hereafter. It states that the measurement of height and weight is useful for the screening of osteoporosis, and BMD measurement or X-ray examination is recommended to those with height loss greater than 2 cm (grade B). In our present study, ROC analysis has yielded the excellent AUC value of 0.84 (95 %CI; 0.77, 0.90) with a cut-off of 4.0 cm. Such difference is likely to arise from the methodological reasons as discussed below.
Height loss can be evaluated by two methods. One is the historical height loss (HHL) which was employed in our study. It is an index for the prevalent VFx [2, 21, 22, 33, 34]. The other method is the prospective one based on the serial height measurements, which will reflect the incidence of new VFx [24, 35, 36]. The latter would not be suitable to identify those with prevalent VFx in the screening of large number of subjects. Although the description on the usefulness of height loss in “Guideline 2011” apparently refers to the prediction of prevalent VFx, the distinction of these two methods is not mentioned, and papers based on both methods are cited [24, 35].
Furthermore, two methods are available for estimating HHL. One is the measurement height (MH), in which the subjects’ current maximal height is directly measured. MH, however, has some technical errors including one inherent in the measuring device, positioning variability and true biological changes over time. The other is the subject's tallest recalled height (TRH). Comparing these two methods, it is obvious that TRH is more suitable for the screening purpose.
Briot et al. [33] have reported that previous VFx was the best predictor of a HHL of 3 cm or more and also that of 6 cm or more using multivariable analysis. They have also shown by multivariable analysis that the cut-off value of 4 cm predicted well the presence of VFx. This value, however, does not seem to be fully validated for its clinical usefulness since such parameters as PPV and NPV are not given.
In another paper, Siminoski et al. [21], reported that likelihood ratio (LR) for VFx was 2.8 (95 %CI; 1.3, 6.0) in subjects with HHL between 6.1 cm and 8.0 cm, whereas it was not significantly different from unity in those with less HHL. They have concluded that HHL less than 6 cm rules out prevalent VFx and subjects with HHL more than 6 cm should have spine radiographs. With this threshold, the sensitivity and specificity were 30 and 94 %, respectively. In our study, the cut-off value was determined to be 4.0 cm with the specificity and sensitivity being 79 % and 79 %, respectively. With regard to the difference from our threshold, several reasons might be considered. First, their subjects were Caucasians. Second, we have used “Youden’s Index” for the calculation of HHL threshold, while Siminoski et al. [21] have screened various cut-off values starting from 0 to 8 cm with 2.0 cm intervals. For the purpose of screening or case-finding, however, there remains the possibility that by employing their high threshold, a significant number of subjects with VFx may be overlooked considering the low sensitivity. Our cut-off value with good sensitivity and specificity might have usefulness for screening purposes of prevalent VFx.
TRH, however, is not free from artifact errors such as “over-reported height” [21, 33, 37, 38]. In the paper using TRH, the amount of height that had been lost from the tallest stature was underestimated both in those without prevalent VFx and those with VFx by 0.7 ± 2.5 and 1.6 ± 3.3 cm, respectively [21]. Thus, caution is required in the interpretation of TRH.
These considerations have led us to investigate the possible usefulness of knee height as the parameter to reflect the height at youth. Bunout et al. [39] reported that knee height can be used as an accurate measurement of height loss in the elderly, and also a significant predictor of femur and spine bone mineral densities in addition to hip circumference. In previous reports, including theirs, however, the possible usefulness of the CH/KH ratio to predict the prevalent VFx has not been described. In the current data, AUC was 0.73 (95 %CI; 0.65, 0.82), and the cut-off value was decided to be 3.3 with a specificity of 47 % and sensitivity of 91 %. Thus, from the current data, this ratio had detective value for the prevalent VFx, although less than that of HHL.
Comparing the two parameters, the cut-off value of HHL in our study was dependent on the VFx numbers, whereas that of the CH/KH ratio was not. One of the reasons might be the far smaller standard deviations of the CH/KH ratio, resulting in the lower sensitivity. Thus, HHL might be a more sensitive index for detecting VFx than the CH/KH ratio. Sensitivity and specificity are independent of the disease prevalence in the study population, and denote the characteristics of the diagnostic test. In contrast, PPV and NPV are influenced by the prevalence. Then, we have evaluated these values across the various theoretically simulated prevalence ranges. HHL and CH/KH ratio were both characterized by the low PPV and high NPV. Thus, high NPV suggests that HL less than 4.0 cm or CH/KH ratio greater than 3.3 is indicative of the absence of VFx with moderate to high accuracy. Considering the low PPV, however, HHL ≥ 4.0 cm and CH/KH ratio ≤ 3.3 suggests, but does not confirm the prevalence of VFx. From these characteristics, HHL and CH/KH ratio are likely to be of value for the screening purpose.
The limitation of our data would be twofold. First, the number of subjects studied is moderate. Second, the study subjects are limited to those attending the osteoporosis clinic of the orthopedics department. Thus, the current subjects may not represent the general population. Nevertheless, both of the two indices; HHL and CH/KH ratio had good values of AUC, sensitivity, and specificity, suggesting the clinical relevance of our data.
In summary, we have presented the cut-off values for HHL and CH/KH ratio to detect VFx in the Japanese population for the first time. Although additional studies including more subjects are required, the current data would be the basis to decide the cut-off values in the future guideline.
References
Miyakoshi N, Kasukawa Y, Sasaki H, Kamo K, Shimada Y (2009) Impact of spinal kyphosis on gastroesophageal reflux disease symptoms in patients with osteoporosis. Osteoporos Int 20:1193–1198
Ettinger B, Black DM, Nevitt MC, Rundle AC, Cauley JA, Cummings SR, Genant HK (1992) Contribution of vertebral deformities to chronic back pain and disability. The Study of Osteoporotic Fractures Research Group. J Bone Miner Res 7:449–456
Graat-Verboom L, Smeenk FW, van den Borne BE, Spruit MA, Donkers-van Rossum AB, Aarts RP, Wouters EF (2012) Risk factors for osteoporosis in Caucasian patients with moderate chronic obstructive pulmonary disease: a case control study. Bone 50:1234–1239
Dam TT, Harrison S, Fink HA, Ramsdell J, Barrett-Connor E, Osteoporotic Fractures in Men (MrOS) Research Group (2010) Bone mineral density and fractures in older men with chronic obstructive pulmonary disease or asthma. Osteoporos Int 21:1341–1349
Martin AR, Sornay-Rendu E, Chandler JM, Duboeuf F, Girman CJ, Delmas PD (2002) The impact of osteoporosis on quality-of-life: the OFELY cohort. Bone 31:32–36
Lips P, Cooper C, Agnusdei D, Caulin F, Egger P, Johnell O, Kanis JA, Kellingray S, Leplege A, Liberman UA, McCloskey E, Minne H, Reeve J, Reginster JY, Scholz M, Todd C, de Vernejoul MC, Wiklund I (1999) Quality of life in patients with vertebral fractures: validation of the Quality of Life Questionnaire of the European Foundation for Osteoporosis (QUALEFFO). Working Party for Quality of Life of the European Foundation for Osteoporosis. Osteoporos Int 10:150–160
Oleksik A, Lips P, Dawson A, Minshall ME, Shen W, Cooper C, Kanis J (2000) Health-related quality of life in postmenopausal women with low BMD with or without prevalent vertebral fractures. J Bone Miner Res 15:1384–1392
Adachi JD, Loannidis G, Berger C, Joseph L, Papaioannou A, Pickard L, Papadimitropoulos EA, Hopman W, Poliquin S, Prior JC, Hanley DA, Olszynski WP, Anastassiades T, Brown JP, Murray T, Jackson SA, Tenenhouse A, Canadian Multicentre Osteoporosis Study (CaMos) Research Group (2001) The influence of osteoporotic fractures on health-related quality of life in community-dwelling men and women across Canada. Osteoporos Int 12:903–908
Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA (1999) Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet 353:878–882
Hasserius R, Karlsson MK, Nilsson BE, Redlund-Johnell I, Johnell O, European Vertebral Osteoporosis Study (2003) Prevalent vertebral deformities predict increased mortality and increased fracture rate in both men and women: a 10-year population-based study of 598 individuals from the Swedish cohort in the European Vertebral Osteoporosis Study. Osteoporos Int 14:61–68
Cauley JA, Thompson DE, Ensrud KC, Scott JC, Black D (2000) Risk of mortality following clinical fractures. Osteoporos Int 11:556–561
Lee YK, Jang S, Jang S, Lee HJ, Park C, Ha YC, Kim DY (2012) Mortality after vertebral fracture in Korea: analysis of the National Claim Registry. Osteoporos Int 23:1859–1865
van Staa TP, Leufkens HG, Cooper C (2002) Does a fracture at one site predict later fractures at other sites? A British cohort study. Osteoporos Int 13:624–629
Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA 3rd, Berger M (2000) Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res 15:721–739
Lindsay R, Silverman SL, Cooper C, Hanley DA, Barton I, Broy SB, Licata A, Benhamou L, Geusens P, Flowers K, Stracke H, Seeman E (2001) Risk of new vertebral fracture in the year following a fracture. J Am Med Assoc 285:320–323
Kanis JA, Johnell O, De Laet C, Johansson H, Oden A, Delmas P, Eisman J, Fujiwara S, Garnero P, Kroger H, McCloskey EV, Mellstrom D, Melton LJ, Pols H, Reeve J, Silman A, Tenenhouse A (2004) A meta-analysis of previous fracture and subsequent fracture risk. Bone 35:375–382
McLellan AR, Gallacher SJ, Fraser M, McQuillian C (2003) The fracture liaison service: success of a program for the evaluation and management of patients with osteoporotic fracture. Osteoporos Int 14:1028–1034
Wallace I, Callachand F, Elliott J, Gardiner P (2011) An evaluation of an enhanced fracture liaison service as the optimal model for secondary prevention of osteoporosis. JRSM Short Rep 10:8
Lauritzen JB, Schwarz P, Lund B, McNair P, Transbøl I (1993) Changing incidence and residual lifetime risk of common osteoporosis-related fractures. Osteoporos Int 3:127–132
Vogt TM, Ross PD, Palermo L, Musliner T, Genant HK, Black D, Thompson DE (2000) Vertebral fracture prevalence among women screened for the Fracture Intervention Trial and a simple clinical tool to screen for undiagnosed vertebral fractures. Fracture Intervention Trial Research Group. Mayo Clin Proc 75:888–896
Siminoski K, Warshawski RS, Jen H, Lee K (2006) The accuracy of historical height loss for the detection of vertebral fractures in postmenopausal women. Osteoporos Int 17:290–296
Kaptoge S, Armbrecht G, Felsenberg D, Lunt M, O’Neill TW, Silman AJ, Reeve J, EPOS Study Group (2004) When should the doctor order a spine X-ray? Identifying vertebral fractures for osteoporosis care: results from the European Prospective Osteoporosis Study (EPOS). J Bone Miner Res 19:1982–1993
North American Menopause Society (2006) Management of osteoporosis in postmenopausal women: 2006 position statement of The North American Menopause Society. Menopause 13:340–367
Huang C, Ross PD, Lydick E, Davis JW, Wasnich RD (1996) Contributions of vertebral fractures to stature loss among elderly Japanese-American women in Hawaii. J Bone Miner Res 11:408–411
Chumlea WC, Guo SS, Steinbaugh ML (1994) Prediction of stature from knee height for black and white adults and children with application to mobility-impaired or handicapped persons. J Am Diet Assoc 94:1385–1388
Cockram DB, Baumgartner RN (1990) Evaluation of accuracy and reliability of calipers for measuring recumbent knee height in elderly people. Am J Clin Nutr 52:397–400
Bland JM, Altman G (1996) Statistics notes: measurement error. Br Med J 313:744
Lee RD, Nieman DC (2007) Nutritional assessment, 4th edn. McGraw-Hill, New York
Genant HK, Wu CY, van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8:1137–1148
Mori S, Soen S, Hagino H, Nakano T, Ito M, Fujiwara S, Kato Y, Tokuhashi Y, Togawa D, Endo N, Sawaguchi T (2013) Diagnostic criteria of vertebral fracture. Osteoporos Jpn 21:25–32
Akobeng AK (2007) Understanding diagnostic tests 3: receiver operating characteristic curves. Acta Paediatr 96:644–647
Orimo H (ed) (2011) Japanese Guidelines for the Prevention and Treatment of Osteoporosis, 2011 edition (in Japanese). Life Science Publishing, Tokyo
Briot K, Legrand E, Pouchain D, Monnier S, Roux C (2010) Accuracy of patient-reported height loss and risk factors for height loss among postmenopausal women. CMAJ 182:558–562
Ismail AA, Cooper C, Felsenberg D, Varlow J, Kanis JA, Silman AJ, O’Neill TW (1999) Number and type of vertebral deformities: epidemiological characteristics and relation to back pain and height loss. European Vertebral Osteoporosis Study Group. Osteoporos Int 9:206–213
Siminoski K, Jiang G, Adachi JD, Hanley DA, Cline G, Ioannidis G, Hodsman A, Josse RG, Kendler D, Olszynski WP, Ste Marie LG, Eastell R (2005) Accuracy of height loss during prospective monitoring for detection of incident vertebral fractures. Osteoporos Int 16:403–410
Kleerekoper M, Nelson DA, Peterson EL, Tilley BC (1992) Outcome variables in osteoporosis trials. Bone 13(suppl):S29–S34
Nores JM, Remy JM, Nenna AD (1990) The value of span measurements in osteoporosis. Br J Clin Pracr 44:154
Cline MG, Meredith KE, Boyer JT, Burrows B (1989) Decline of height with age in adults in a general population sample: estimating maximum height and distinguishing birth cohort effects from actual loss of stature with aging. Hum Biol 61:415–425
Bunout D, Barrera G, de la Maza MP, Leiva L, Gattas V, Hirsch S (2007) Height reduction, determined using knee height measurement as a risk factor or predictive sign for osteoporosis in elderly women. Nutrition 23:794–797
Acknowledgments
This work was supported by the Health Labour Sciences Research Grant (Principal Investigator; Shumpei Niida).
Conflict of interest
All authors have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Yoh, K., Kuwabara, A. & Tanaka, K. Detective value of historical height loss and current height/knee height ratio for prevalent vertebral fracture in Japanese postmenopausal women. J Bone Miner Metab 32, 533–538 (2014). https://doi.org/10.1007/s00774-013-0525-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-013-0525-y