Abstract
During the healing process after bone fracture, soft callus forms adjacent to the fracture site, is replaced by hard callus, and is finally remodeled to the original bone configuration. Although the cambium layer of the periosteum is reported to play an essential role in callus formation, we still lack direct in vivo evidence of this. To investigate the cell lineage of the soft callus, we analyzed the process of fracture healing in Prx1-Cre;ROSA26 reporter (R26R), Col1a1(3.6 kb)-Cre;R26R, Col1a1(2.3 kb)-Cre;R26R, Sox9-CreERT2;R26R, and Sox9-LacZ mice with X-gal staining. In the Prx1-Cre;R26R, in which the cells of the periosteum stained for X-gal before fracture, all cells in the soft callus were X-gal positive, whereas in the Col1a1(3.6 kb)-Cre;R26R mice, the cells in the periosteum before fracture stained for X-gal and the soft callus was partly composed of X-gal-positive cells. In contrast, in the Col1a1(2.3 kb)-Cre;R26R mice, in which the mature osteoblasts in the cambium layer of the periosteum were marked before fracture, no cells in the soft callus at the fracture site were X-gal positive. These results suggest that most of the cells in the soft callus are derived from the mesenchymal progenitors in the periosteum, and not from mature osteoblastic cells. Interestingly, in the Sox9-LacZ mice, Sox9-expressing X-gal-positive cells emerged in the periosteum adjacent to the fracture site 3 days after fracture. We demonstrated this by injecting tamoxifen into the Sox9-CreERT2;R26R mice for 3 days after fracture, so that these Sox9-expressing periosteal cells gave rise to cells in the soft and hard calli. Our findings show that the periosteal cells in which Sox9 expression is induced just after fracture are the major source of the chondrocytes and osteoblasts in the fracture callus.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bone is a highly organized and specialized connective tissue and is composed of two structural types, cortical and cancellous bone. The external and internal surfaces of the cortical bone are covered by the periosteum and endosteum, respectively. Microscopically, the periosteum is composed of an outer fibrous layer containing cells that synthesize collagen fibers and an inner cambium layer consisting of osteoblasts, fibroblasts, and mesenchymal progenitor cells with the capacity to differentiate into osteoblasts and chondrocytes [1]. The spaces in cancellous bone are filled with various types of marrow cells, including multipotent marrow stromal cells.
Broken bones undergo processes of endochondral ossification and intramembranous ossification that recapitulate certain aspects of skeletal development. The fracture healing process is partitioned into four stages based on histological observations [2]. The inflammatory stage begins immediately after the bone is fractured, in association with the disruption of the surrounding soft tissues, bleeding within the fracture area, and distortion of the marrow architecture, which lead to local inflammation and the formation of a hematoma. At this stage, stem cells originating from multiple sources are likely to be committed to and initiate the cell lineages involved in bone repair and vascularization. At the stage of soft callus formation, the adjacent periosteum becomes thickened and cartilage tissues appear outside the bone. Discrete cartilaginous regions grow progressively and bridge the fractured bone fragments. This cartilaginous template of the soft callus is then replaced by bone, resulting in the formation of a hard callus (the hard callus formation stage). The hard callus is remodeled by osteoclasts and osteoblasts and returns to the original cortical and trabecular bone configuration (the bone remodeling stage).
Several possible sources of the cells that produce bone and cartilage at the fracture site have been identified. Although previous studies have reported potential sources of stem cells or progenitor cells in the bone marrow, endosteum, vessel walls, surrounding soft tissues (including muscle and adipose tissues), and the circulation, the periosteum plays a crucial role in fracture healing [3–5]. Periosteal damage or removal results in delayed healing of the fracture [6]. Colnot [7] showed that the periosteum is a major source of osteoblasts and chondrocytes during fracture healing. In particular, the cambium layer is the component of the periosteum essential for bone formation. Ito et al. [8] cultured rabbit periosteal explants and showed that the chondrocyte precursors were located in the cambium layer of the periosteum and that chondrogenesis took place in the juxtaosseous area in the cambium layer. However, we still lack direct in vivo evidence of the progenitor cells in the periosteum and their contribution to fracture healing.
The transcription factor Sox9 is expressed in all chondroprogenitor cells and plays an essential role in chondrogenesis [9]. Cell fate mapping in Sox9-Cre;ROSA26 reporter (R26R) mice revealed that Sox9-expressing limb bud mesenchymal cells give rise to both chondrocytes and osteoblasts, indicating that Sox9 defines osteochondroprogenitor cells during skeletogenesis [10]. We also generated a mouse strain that inducibly expresses Cre recombinase in Sox9-expressing cells [11]. An IRES-CreERT2-pA cassette was inserted into the 3′ untranslated region of the Sox9 gene, resulting in Cre recombinase expression directly under Sox9 cis-regulatory control via the production of a bicistronic Sox9-Cre recombinase mRNA. The administration of tamoxifen to offspring of crosses between Sox9-CreERT2 and R26R mice efficiently induced the expression of the Cre reporter in Sox9-expressing cells. The advantage of this genetic system in examining gene expression patterns is that the R26R strain provides a permanent lineage record through its constitutive X-gal expression in cells that express Cre recombinase, even transiently, in the precursor cells of different cell lineages. Therefore, this mouse line has been useful for tracing Sox9-expressing osteochondroprogenitor cells in vivo. The purposes of this study are to investigate the cell lineage of the soft callus in vivo, using several Cre drivers. We found that osteochondroprogenitor cells are initiated in the periosteum adjacent to the fracture site and are the major source of the soft callus.
Materials and methods
Animals
Prx1-Cre mice, Col1a1(2.3 kb)-Cre mice, Sox9-LacZ knock-in mice, Sox9-CreERT2 mice, and R26R mice have been reported previously [11–15]. Col1a1(3.6 kb)-Cre mice were purchased from the Jackson Laboratory.
Tibia fracture model
Eight-week-old Prx1-Cre;R26R, Col1a1(3.6 kb)-Cre;R26R, Col1a1(2.3 kb)-Cre;R26R, Sox9-LacZ, and Sox9-CreERT2;R26R mice were used to prepare the tibia fractures. Each mouse was anesthetized with 50–100 mg/kg pentobarbital administered intraperitoneally. The skin, subcutaneous tissues, and fascia were incised along the anterior part of the left leg and retracted medially, and the tibia was exposed. The mid-diaphysis of the tibia was fractured using scissors, without stripping off the periosteum. Three to five animals were analyzed for each mouse line.
Histological analysis
The fractured tibiae were collected 3, 5, 7, 14, 21, or 28 days after surgery as indicated in each mouse line. The fresh tibia samples were quickly embedded in OCT compound medium (Sakura Finetek) for cryosectioning and sectioned at a thickness of 8 μm. After the sectioned samples were fixed in 0.2 % glutaraldehyde/2 % formaldehyde, they were stained by 0.15 % (w/v) Alcian blue (pH 2.5) and hematoxylin/eosin or with X-gal solution overnight at 37 °C and counterstained with Nuclear Fast Red as described previously [16].
Results
Process of fracture healing in mouse tibia
We first clarified the process of callus formation during the healing of mouse tibia fractures using histology with Alcian blue and hematoxylin/eosin staining (Fig. 1a, b). On day 3 after surgery, the periosteum adjacent to the fracture site started to thicken. On day 7, soft callus formation was distinguished by Alcian blue staining, and the soft callus was replaced by bone to form the hard callus. On day 14, the soft callus had diminished, and a large part of the callus was occupied by hard callus. On days 21 and 28, the hard callus was remodeled, and newly formed periosteum and bone marrow were detected.
A process of tibial fracture healing. Longitudinal sections through a mouse tibia stained with Alcian blue and hematoxylin/eosin. a Low magnification. b High magnification of the dotted box in (a). PO periosteum, BM bone marrow, SC soft callus, HC hard callus, RB remodeled bone. Scale bar 1 mm for (a) and 500 μm for (b)
Cells derived from Prx1-promoter-active multipotent mesenchymal cells and Col1a1(3.6 kb)-promoter-active premature mesenchymal cells predominantly contribute to soft callus formation in fracture healing
We clarified the cell lineage of the soft callus using Prx1-Cre;R26R mice. Because Prx1 is expressed in the multipotent mesenchymal cells of mouse limb buds as early as E9.0, before either an osteoblastic or a chondrogenic lineage has been separated [12], all mesenchymal tissues are derived from Prx1-expressing multipotent cells. On day 0 before fracture, X-gal-positive cells were found in the periosteum, cortical bone, and endosteum. A small number of X-gal-positive cells were also detected in the bone marrow of the diaphysis (Fig. 2a, b). The cells in the growth plate and metaphyseal bones were X-gal positive. On day 7 after surgery, all cells in the soft callus were X-gal positive (Fig. 2c, d), and on day 14, all the cells in both the soft callus and hard callus were stained for X-gal (Fig. 2e, f). On days 21 and 28, X-gal-positive cells were detected in the remodeled bones and the newly formed periosteum (Fig. 2g–j). Thus, all the cells in the callus may have derived from cells that originated from Prx1-expressing mesenchymal cells.
Tibia fracture in Prx1-Cre;R26R mice. a X-gal-positive cells are found in the periosteum, cortical bone, and endosteum on day 0 (scale bar 1 mm). b High magnification of (a). Arrowheads indicate X-gal-positive cells in the bone marrow (scale bar 100 μm). c, e Soft and hard calli are X-gal positive on days 7 and 14. d, f High magnification of (c) and (e). g, i Remodeled bone and the newly formed periosteum are X-gal positive on days 21 and 28. h, j High magnification of (g) and (i). MB metaphyseal bone, GP growth plate, PO periosteum, EO endosteum, BM bone marrow, SC soft callus, HC hard callus, RB remodeled bone. Scale bar 1 mm for (c, e, g, i) and 500 μm for (d, f, h, j)
Next, we induced fractures in the tibiae of Col1a1(3.6 kb)-Cre;R26R mice, in which the Col1a1(3.6 kb) promoter is active in premature mesenchymal cells and osteoblastic cells. On day 0 before fracture, X-gal-positive cells were found in the periosteum, cortical bone, and endosteum. A small number of X-gal-positive cells were also detected in the growth plate and the bone marrow of the diaphysis. (Fig. 3a, b). The cells in the metaphyseal bones were X-gal positive. On day 7 after surgery, a large number of X-gal-positive cells dramatically emerged in the thickened periosteum adjacent to the fracture site, and a proportion of the cells in the soft callus stained for X-gal (Fig. 3c–e). On days 14 and 21, most cells in the soft and hard calli and in the newly formed periosteum were X-gal positive (Fig. 3f–i). On day 28 after surgery, X-gal-positive cells were localized in the remodeled bones (Fig. 3j). These findings suggest that although Col1a1(3.6 kb)-expressing cells located in the periosteum, endosteum, and/or bone marrow may contribute to the formation of the soft callus, a proportion of the cells in the soft callus are probably derived from Col1a1(3.6 kb)-promoter-active mesenchymal progenitors in the periosteum adjacent to the fracture site.
Tibia fracture in Col1a1(3.6 kb)-Cre;R26R mice. a X-gal positive-cells are found in the periosteum, cortical bone, and endosteum on day 0 (scale bar 1 mm). b High magnification of (a). Arrows indicate X-gal-positive cells in the periosteum and endosteum. Arrowheads indicate X-gal-positive cells in the bone marrow (scale bar 100 μm). c Cells in the soft callus and the thickened periosteum adjacent to the fracture site are X-gal positive on day 7. d, e High magnification of the dotted bone and the solid box in (c). f Cells in the hard callus are X-gal positive on day 14. g High magnification of the dotted box in (f). h, j X-gal-positive cells are detected in the remodeled bone and the newly formed periosteum on days 21 and 28. i High magnification of the dotted box in (h). MB metaphyseal bone, GP growth plate, PO periosteum, EO endosteum, BM bone marrow, SC soft callus, HC hard callus. Scale bar 1 mm for (c, f, h, j) and 500 μm for (d, e, g, i)
Mature osteoblasts in the periosteum and endosteum do not give rise to chondrocytes in the soft callus
To identify the cells in the periosteum that contribute to the formation of the soft callus, we marked mature osteoblasts using Col1a1(2.3 kb)-Cre;R26R mice. On day 0 before fracture, X-gal-positive cells were detected in the cambium layer of the periosteum and endosteum, indicating that they were mature osteoblasts (Fig. 4a, b). The cells in the cortex and a small number of cells in the metaphyseal bones were X-gal positive. However, in contrast, there were no X-gal-positive cells in the bone marrow of the diaphysis. On days 7 and 14 after surgery, a large number of X-gal-positive cells were detected in the hard callus but not in the soft callus (Fig. 4c–f). On days 21 and 28, X-gal-positive cells were detected in the remodeled bones (Fig. 4g–j). These results indicate that the Col1a1 (2.3 kb)-expressing mature osteoblasts in the periosteum and endosteum did not give rise to the cells in the soft callus.
Tibia fracture in Col1a1(2.3 kb)-Cre;R26R mice. a X-gal-positive cells are found in the periosteum, cortical bone, and endosteum on day 0 (scale bar 1 mm). b High magnification of (a) (scale bar 100 μm). c, e Cells in the hard callus are X-gal positive on days 7 and 14. d, f High magnification of (c) and (e). g, i Cells in the remodeled bone are X-gal positive on days 21 and 28. h, j High magnification of (g) and (i). MB metaphyseal bone, GP growth plate, PO periosteum, EO endosteum, BM bone marrow, SC soft callus, HC hard callus, RB remodeled bone. Scale bar 1 mm for (c, e, g, i) and 500 μm for (d, f, h, j)
Sox9-expressing cells emerge transiently in the periosteum adjacent to the fracture site
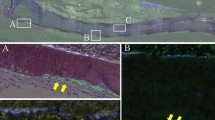
Our previous approaches based on mouse genetics have demonstrated that Sox9 defines osteochondroprogenitor cells, and that Sox9 is essential for chondrogenesis [9, 10]. Therefore, Sox9 expression should be induced in the cells that differentiate into chondrocytes in the soft callus. To investigate Sox9 expression closely during an early stage of fracture healing, we induced fractures in Sox9-LacZ knock-in mice [14]. On day 0 before surgery, there were no X-gal-positive cells in the bones, including in the periosteum, endosteum, and bone marrow (Fig. 5a, b). In contrast, the growth plate chondrocytes were X-gal positive. On day 3 after surgery, a small number of X-gal-positive cells emerged in the cambium layer of the periosteum adjacent to the fracture site (Fig. 5c–e). On day 5, X-gal-positive cells were located only in the soft callus and the thickened periosteum adjacent to the fracture site (Fig. 5f, g). These findings indicate that Sox9-expressing chondroprogenitor cells are induced in the periosteum adjacent to the fracture site.
Tibia fracture in Sox9-LacZ mice. a No X-gal-positive cells are found in the bones on day 0 (scale bar 1 mm). b High magnification of (a). Growth plate chondrocytes are X-gal positive (scale bar 100 μm). c Low magnification of fractured tibia on day 3. d High magnification of the dotted box in (c). No X-gal-positive cells are apparent around the fracture site. e High magnification of the dotted boxes in (d). A small number of X-gal-positive cells are found in the periosteum adjacent to the fracture site (arrowheads). f Low magnification of the fractured tibia on day 5. g High magnification of the dotted boxed in (f). All chondrocytic cells in the soft callus are X-gal positive. A large number of X-gal-positive cells are apparent in the thickened periosteum adjacent to the fracture site. MB metaphyseal bone, GP growth plate, PO periosteum, EO endosteum, BM bone marrow, SC soft callus. Scale bar 1 mm for (c, d, f) and 100 μm for (e, g)
Sox9-expressing cells in the periosteum predominantly contribute to the formation of the soft callus during fracture healing
To trace the fate of Sox9-expressing chondroprogenitor cells in the periosteum adjacent to the fracture site, we injected tamoxifen peritoneally into Sox9-CreERT2;R26R mice for 3 days after surgery [11]. On day 3 after surgery and tamoxifen injection, no X-gal-positive cells were detected in the bones, including the periosteum, endosteum, and bone marrow (Fig. 6a, b). In contrast, the growth plate chondrocytes were X-gal positive. On day 5, X-gal-positive cells were detected in the thickened periosteum and the soft callus (Fig. 6c, d). On days 7 and 14, the cells in the soft and hard calli were X-gal positive (Fig. 6e–h). On day 28, X-gal-positive cells were detected in the newly formed periosteum and the remodeled bone tissues (Fig. 6i, j). These results indicate that the periosteal cells in which Sox9 expression was induced just after fracture gave rise to the chondrocytes and osteoblasts in the fracture callus and the cells in the newly formed periosteum during fracture healing.
Tibia fracture in Sox9-CreERT2;R26R mice. The mice were injected with tamoxifen for 3 days after surgery. a No X-gal-positive cells are found in the bones on day 0 (scale bar 1 mm). b High magnification of (a). Growth plate chondrocytes are X-gal positive (scale bar 100 μm). c Cells in the soft callus are X-gal positive on day 5. d High magnification of (c). e, g X-gal-positive cells are found in the soft and hard calli on days 7 and 14. f, h High magnification of the dotted boxes in (e) and (g). i The cells in the remodeled bone and the newly formed periosteum are positive for X-gal on day 28. j High magnification of the dotted box in (i). Arrowheads indicate X-gal-positive cells in the periosteum. MB metaphyseal bone, GP growth plate, PO periosteum, EO endosteum, BM bone marrow, SC soft callus, HC hard callus, RB remodeled bone. Scale bar 1 mm for (c, e, g, i) and 500 μm for (d, f, h, j)
Discussion
During the process of fracture healing, multipotent mesenchymal progenitor cells must be recruited to the fracture site. These cells differentiate into chondrocytes and osteoblasts and contribute to the formation of the soft and hard calli. Several sources of these cells have been detected. Tavassoli and Crosby [17] and Friedenstein et al. [18] demonstrated the existence of mesenchymal stem cells in the bone marrow. Farrington-Rock et al. [3] and Brighton and Hunt [19] reported that pericytes can potentially differentiate into chondrocytes. Lee et al. [5] and Usas et al. [20] showed evidence that muscle-derived cells adjacent to the bone tissues play a role in fracture healing because of their osteogenic potential. Circulating progenitor cells in the bloodstream are also recruited to the fracture site through the stromal cell-derived factor-1/CXCR4 axis and develop a favorable environment for fracture healing by enhancing angiogenesis and osteogenesis [21]. However, when Colnot [7] performed cell lineage analyses by transplanting bone grafts, she demonstrated that the bone itself is the main local source of cells for bone repair. Osteoblasts and osteocytes originate from the periosteum, bone marrow, and endosteum, indicating that these three tissues contribute simultaneously to the formation of new bone. Chondrocytes within the fracture callus are primarily derived from the periosteum. This finding is supported by previous studies [22]. Periosteal damage or removal delays fracture healing because the local sources of multipotent mesenchymal progenitor cells are thereby removed.
The current mouse genetics approach, based on the Cre/loxP recombination system, allows us to define cell lineages at the cellular level. In this study, we first demonstrated that the osteochondroprogenitor cells in the periosteum make a distinct cellular contribution to the soft callus. Prx1 is a homeobox-containing gene that starts to be expressed in all limb bud mesenchymal cells at E9.0, before Sox9 is expressed [12]. We have previously reported that conditional Sox9-null mutants harboring a Prx1-Cre transgene showed a complete lack of both cartilage and bone in their limbs [9]. Moreover, in Prx1-Cre;R26R embryos, all the cells in the skeletal elements, the fibroblasts in the connective tissues, and the tendon cells and the synovial cells were X-gal positive. Hence, Prx1-expressing undifferentiated limb bud mesenchymal cells, including Sox9-expressing osteochondroprogenitor cells, differentiate into all the mesenchymal cell populations. In Prx1-Cre;R26R mice, the periosteum, endosteum, and a small number of the cells in the bone marrow were X-gal positive, and almost all of the soft callus was also X-gal positive. This finding corresponds, in part, to that of Kawanami et al. [23] in Prx1-CreER transgenic mice. They found that Prx1-expressing periosteal cells differentiated into chondrocytes and osteoblasts in the fracture callus, further supporting the notion that Prx1-expressing cells in the periosteum are osteochondroprogenitor cells. We also analyzed fracture healing in Col1a1(3.6 kb)-Cre;R26R mice. The 3.6-kb Col1a1 promoter is active in mesenchymal progenitor cells, immature preosteoblasts, and mature osteoblasts [24]. In the Col1a1(3.6 kb)-Cre;R26R mice, the cells in the periosteum, endosteum, and a small number of the cells in the bone marrow were X-gal positive, and a proportion of the cells in the soft callus were X-gal positive. In contrast, in Col1a1(2.3 kb)-Cre;R26R mice, a few cells in the periosteum and endosteum were X-gal positive because the 2.3-kb Col1a1 promoter is active in mature osteoblasts and osteocytes [25, 26], but no chondrocytes in the soft callus were X-gal positive. The contribution to callus formation during fracture healing of cells that are Prx1- and Col1a1(3.6 kb)-promoter silent before fracture has not yet been clarified. However, our results indicate that a large proportion of chondrocytes in the soft callus at the fracture site are probably derived from cells originating from Prx1-promoter-active mesenchymal progenitor cells in the bone tissue. Col1a1(3.6 kb)-expressing cells in the periosteum also partly contribute to the formation of the soft callus.
We have previously shown that Sox9 defines osteochondroprogenitor cells [9]. In Sox9-LacZ mice, no cells in the periosteum express Sox9, suggesting that the multipotent mesenchymal cells in the periosteum are not committed osteochondroprogenitor cells in the healthy condition. However, 3 days after a fracture occurs, the periosteal cells in the cambium layer adjacent to the fracture site transiently express Sox9. Therefore, we injected tamoxifen into Sox9-CreERT2;R26R mice for 3 days after fracture to label the Sox9-expressing periosteal cells and traced the fate of those cells. Interestingly, many X-gal-positive cells were detected in and around the soft and hard calli, indicating that the Sox9-expressing periosteal cells adjacent to the fracture site give rise to chondrocytes and osteoblasts in the fracture callus and in the newly formed periosteal tissues overlying the callus. Kawanami et al. [23] showed that Prx1-expressing periosteal cells differentiate into undifferentiated cells, some of the chondrocytes in the soft callus, osteoblasts, and cells in the newly formed periosteum. Taking all these findings together, multipotent mesenchymal progenitor cells in the periosteum that originate from Prx1-expressing mesenchymal cells give rise to Sox9-expressing osteochondroprogenitor cells during fracture healing, a process that recapitulates endochondral ossification in limb bud development. Sox9-expressing osteochondroprogenitor cells, possibly derived from Col1a1(3.6 kb)-expressing cells, emerged in the thickened periosteum adjacent to the fracture site and make a major contribution to the formation of the soft callus.
In conclusion, this cell lineage analysis using a mouse genetics approach has demonstrated that the periosteum plays a central role in soft callus formation during fracture healing. The multipotent mesenchymal progenitor cells in the periosteum are committed to becoming Sox9-expressing osteochondroprogenitor cells shortly after a fracture occurs and differentiate into chondrocytes, osteoblasts, and periosteal cells. Further research is required to confirm how much Sox9-expressing osteochondroprogenitor cells contribute to fracture repair, and to isolate a pure population of Sox9-expressing cells from the periosteum, to determine the cellular and molecular characteristics of the periosteal osteochondroprogenitor cells.
References
Squier CA, Ghoneim S, Kremenak CR (1990) Ultrastructure of the periosteum from membrane bone. J Anat 171:233–239
Schindeler A, McDonald MM, Bokko P, Little DG (2008) Bone remodeling during fracture repair: the cellular picture. Semin Cell Dev Biol 19:459–466
Farrington-Rock C, Crofts NJ, Doherty MJ, Ashton BA, Griffin-Jones C, Canfield AE (2004) Chondrogenic and adipogenic potential of microvascular pericytes. Circulation 110:2226–2232
Zuk PA, Zhu M, Mizuno H, Huang J, Futrell JW, Katz AJ, Benhaim P, Lorenz HP, Hedrick MH (2001) Multilineage cells from human adipose tissue: implications for cell-based therapies. Tissue Eng 7:211–228
Lee JY, Qu-Petersen Z, Cao B, Kimura S, Jankowski R, Cummins J, Usas A, Gates C, Robbins P, Wernig A, Huard J (2000) Clonal isolation of muscle-derived cells capable of enhancing muscle regeneration and bone healing. J Cell Biol 150:1085–1100
Kojimoto H, Yasui N, Goto T, Matsuda S, Shimomura Y (1988) Bone lengthening in rabbits by callus distraction. The role of periosteum and endosteum. J Bone Joint Surg Br 70:543–549
Colnot C (2009) Skeletal cell fate decisions within periosteum and bone marrow during bone regeneration. J Bone Miner Res 24:274–282
Ito Y, Fitzsimmons JS, Sanyal A, Mello MA, Mukherjee N, O’Driscoll SW (2001) Localization of chondrocyte precursors in periosteum. Osteoarthritis Cartilage 9:215–223
Akiyama H, Chaboissier MC, Martin JF, Schedl A, de Crombrugghe B (2002) The transcription factor Sox9 has essential roles in successive steps of the chondrocyte differentiation pathway and is required for expression of Sox5 and Sox6. Genes Dev 16:2813–2828
Akiyama H, Kim JE, Nakashima K, Balmes G, Iwai N, Deng JM, Zhang Z, Martin JF, Behringer RR, Nakamura T, de Crombrugghe B (2005) Osteo-chondroprogenitor cells are derived from Sox9 expressing precursors. Proc Natl Acad Sci USA 102:14665–14670
Soeda T, Deng JM, de Crombrugghe B, Behringer RR, Nakamura T, Akiyama H (2010) Sox9-expressing precursors are the cellular origin of the cruciate ligament of the knee joint and the limb tendons. Genesis 48:635–644
Martin JF, Olson EN (2000) Identification of a prx1 limb enhancer. Genesis 26:225–229
Nakanishi R, Akiyama H, Kimura H, Otsuki B, Shimizu M, Tsuboyama T, Nakamura T (2008) Osteoblast-targeted expression of Sfrp4 in mice results in low bone mass. J Bone Miner Res 23:271–277
Zhu J, Nakamura E, Nguyen MT, Bao X, Akiyama H, Mackem S (2008) Uncoupling Sonic hedgehog control of pattern and expansion of the developing limb bud. Dev Cell 14:624–632
Soriano P (1999) Generalized lacZ expression with the ROSA26 Cre reporter strain. Nat Genet 21:70–71
Hogan B, Costantini F, Beddington R (1994) Manipulating the mouse embryo: a laboratory manual. Cold Spring Harbor Laboratory Press, New York
Tavassoli M, Crosby WH (1968) Transplantation of marrow to extramedullary sites. Science 161:54–56
Friedenstein AJ, Petrakova KV, Kurolesova AI, Frolova GP (1968) Heterotopic of bone marrow: analysis of precursor cells for osteogenic and hematopoietic tissues. Transplantation 6:230–247
Brighton CT, Hunt RM (1997) Early histologic and ultrastructural changes in microvessels of periosteal callus. J Orthop Trauma 11:244–253
Usas A, Ho AM, Cooper GM, Olshanski A, Peng H, Huard J (2009) Bone regeneration mediated by BMP4-expressing muscle-derived stem cells is affected by delivery system. Tissue Eng Part A 15:285–293
Matsumoto T, Kawamoto A, Kuroda R, Ishikawa M, Mifune Y, Iwasaki H, Miwa M, Horii M, Hayashi S, Oyamada A, Nishimura H, Murasawa S, Doita M, Kurosaka M, Asahara T (2006) Therapeutic potential of vasculogenesis and osteogenesis promoted by peripheral blood CD34-positive cells for functional bone healing. Am J Pathol 169:1440–1457
Ozaki A, Tsunoda M, Kinoshita S, Saura R (2000) Role of fracture hematoma and periosteum during fracture healing in rats: interaction of fracture hematoma and the periosteum in the initial step of the healing process. J Orthop Sci 5:64–70
Kawanami A, Matsushita T, Chan YY, Murakami S (2009) Mice expressing GFP and CreER in osteochondroprogenitor cells in the periosteum. Biochem Biophys Res Commun 386:477–482
Boban I, Jacquin C, Prior K, Barisic-Dujmovic T, Maye P, Clark SH, Aguila HL (2006) The 3.6 kb DNA fragment from the rat Col1a1 gene promoter drives the expression of genes in both osteoblast and osteoclast lineage cells. Bone 39:1302–1312
Dacic S, Kalajzic I, Visnjic D, Lichtler AC, Rowe DW (2001) Col1a1-driven transgenic markers of osteoblast lineage progression. J Bone Miner Res 16:1228–1236
Kalajzic I, Kalajzic Z, Kaliterna M, Gronowicz G, Clark SH, Lichtler AC, Rowe D (2002) Use of type I collagen green fluorescent protein transgenes to identify subpopulations of cells at different stages of the osteoblast lineage. J Bone Miner Res 17:15–25
Acknowledgments
We thank James F. Martin, Philippe Soriano, Chisa Shukunami, and Richard R. Behringer for their valuable help. This work was supported by Grants-in-Aid for Scientific Research from the Japanese Ministry of Education, Culture, Sports, Science, and Technology (#21249078 and #23659717 to HA and #22791376 to KY).
Conflict of interest
All authors have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
H. Murao and K. Yamamoto contributed equally to this work.
About this article
Cite this article
Murao, H., Yamamoto, K., Matsuda, S. et al. Periosteal cells are a major source of soft callus in bone fracture. J Bone Miner Metab 31, 390–398 (2013). https://doi.org/10.1007/s00774-013-0429-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-013-0429-x