Abstract
To explore the skeletal effects and the potential underlying mechanisms of treatment with two thiazolidinediones (rosiglitazone and pioglitazone) or metformin in insulin-resistant mice, 24 female, 12-week-old C57BL6J ob/ob mice were evaluated according to the following treatment groups for 6 weeks: placebo group, pioglitazone group (Pio), rosiglitazone group (Rosi), and metformin group (Met). Bone mineral density (BMD), bone microarchitecture, bone histomorphometry, and expression of three phenotype-specific gene markers, including bone morphogenetic protein 2 (Bmp2), runt-related transcription factor 2 (Runx2), and fatty acid-binding protein 4 (Fabp4), were compared across the four groups. At the femur, the Met group had the highest BMD (0.084 ± 0.001 g/cm2) and trabecular bone volume/total volume (0.644 ± 0.018 %) and the lowest trabecular spacing (Tb.Sp.) (0.143 ± 0.008 μm), whereas the Rosi group had lower BMD (0.076 ± 0.003 g/cm2) and a relatively higher degree of Tb.Sp. (0.173 ± 0.024 μm). A histomorphometric analysis revealed that in the Rosi group the number of adipocytes was fourfold higher than in the placebo group and fivefold higher than in the Met group, whereas the highest osteoid width and mineral apposition rate were found in the Met group (49.88 ± 48.53 μm and 4.46 ± 1.72 μm/day). Furthermore, the Rosi group displayed the highest level of Fabp4 gene expression, which was accompanied by normal expression levels of Bmp2 and Runx2. Seemingly, metformin is a bone-friendly antidiabetic drug. Rosiglitazone had adverse effects on the skeleton at the trabecular bone even in insulin-resistant mice, whereas no evidence of adverse effects was found for pioglitazone.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes affects a large proportion of the Chinese population. The age-standardized prevalence of total diabetes and prediabetes among women was 8.8 % and 14.9 %, respectively, accounting for 42.2 million women with diabetes and 72.1 million women with prediabetes [1]. Compared to individuals without diabetes, women with diabetes have a greater risk for developing bone fractures, which consequently can lead to significant morbidity and mortality [2, 3]. In the past decade, the skeletal effects of treatments with oral hypoglycemic drugs, specifically, the secondary osteoporosis and limb fractures that result from thiazolidinedione (TZD) treatment, have been of great concern worldwide.
TZD, an agonist of peroxisome proliferator-activated receptor-gamma (PPAR-γ), acts as an insulin sensitizer and is widely prescribed for the management of conditions that are characterized by insulin resistance, especially type 2 diabetes (T2DM). Recently, increasing amounts of evidence indicate that TZD treatment can have adverse skeletal consequences, not only for elderly postmenopausal women but also for premenopausal women with different ethnic backgrounds [4–9]. The most common explanation is that bone is a target of TZD drugs [10]. Osteoblasts and adipocytes are derived from a common multipotential mesenchymal stem cell (MSC) progenitor via the activation of PPAR-γ2 by TZD. In animal studies, the activation of PPAR-γ by TZDs such as rosiglitazone has been shown to cause bone loss that results from an increase in marrow adipocytes and a decrease in osteoblasts, which lead to a reduction in bone formation rate [11]. Either rosiglitazone or pioglitazone treatment was able to simultaneously stimulate adipogenesis and inhibit osteoblastogenesis [10]. However, this unbalanced bone remodeling is likely more complicated than it appears to be. Lazarenko et al. [12] demonstrated that the mechanisms of rosiglitazone-induced bone loss are distinct for different stages of the life cycle. This bone loss may be the consequence of upregulated bone resorption in aged animals or it may be caused by downregulated bone formation in adult animals.
In addition to TZD, metformin is the most important oral antidiabetic drug in the biguanide class. This drug may be beneficial not only for diabetes but also for fragility fractures in postmenopausal women with T2DM as a result of its role in promoting bone formation [13, 14].
To investigate the pathophysiology of the skeletal effects of antidiabetic drugs, we examined bone mineral density (BMD), bone microarchitecture, bone histomorphometry, and the expression of phenotype-specific gene markers, including bone morphogenetic protein 2 (Bmp2), runt related transcription factor 2 (Runx2), and adipocyte fatty acid-binding protein 4 (Fabp4), in 12-week-old female C57BL6J ob/ob mice. These data were then used to further explore the skeletal effects of treatment with two types of TZDs (rosiglitazone and pioglitazone) and metformin and to provide insight into the underlying mechanisms responsible for TZD-related bone loss in women with T2DM.
Materials and methods
Experimental animals and treatment regime
Twenty-four 12-week-old sexually mature female C57BL6J ob/ob mice were obtained from the Model Animal Research Center of Nanjing University. This type of mouse is one of the best animal models for the study of insulin sensitizers [15]. The animals, which were identified by ear punches, were housed (three per cage) with free access to water and were maintained at a constant temperature and a 12-h light/12-h dark cycle. The animal treatment and care protocols conformed to Directive 2010/63/EU for animal experimentation and were conducted according to a Shanghai Tongji University Animal Care and Use Committee-approved protocol. The animals were placed into the following treatment groups, which consisted of six animals per group: placebo group, pioglitazone group (Pio), rosiglitazone group (Rosi), and metformin group (Met). The doses of pioglitazone hydrochloride (Actos, Takeda, Japan), rosiglitazone maleate (Avandia, GlaxoSmithKline, King of Prussia, PA), and metformin hydrochloride (Glucophage, Bristol-Myers Squibb, USA) were 12, 20, and 150 mg/kg body weight/day by gavage, respectively. The animals were fed every day for 6 weeks, and the food intake per cage as well as the body weight and fasting blood glucose levels (FBG) of individual animals were monitored every week. To assess FBG, the mice were fasted but had free access to water at 3 PM the day before testing. To permit dynamic bone histomorphometric measurements, mice were intraperitoneally injected with 5 mg/kg body weight calcein at 13 and 14 days before being killed and 30 mg/kg tetracycline 3 and 4 days before death [16].
BMD measurements
Immediately after death, the left femur and lumbar spine 2–5 (L2–L5) of each animal were dissected for the measurement of BMD, using the fan-beam dual-energy X-ray absorptiometry (DXA) machine (Hologic QDR-4500) with small animal software (Hologic, Bedford, MA, USA). Internal variations of the repeated measures for the murine lumbar spine and femur BMD were determined to be 1.7–2.0 %.
Microcomputed tomography (micro-CT) analysis
After the BMD measurements were made, the left femur and L2–L5 of each animal were fixed in Millonig’s phosphate-buffered 10 % formalin (pH 7.4). After 24 h, the femur was dehydrated successively in 70 %, 95 %, and 100 % ethanol and was analyzed without additional sample preparation using a micro-CT 45-μm scanner (eXplore Locus; GE Healthcare, USA). The volumetric parameters of bone volume (BV), total volume (TV), and the calculated ratio of BV/TV (%) as well as trabecular thickness (Tb.Th., μm), trabecular number (Tb.N., no./mm), and trabecular spacing (Tb.Sp., μm) were assessed to investigate the effect of each antidiabetic drug on the microarchitecture of the spongiosa and trabecular bone.
Bone histomorphometry
Following death, the right femurs were embedded undecalcified in methyl methacrylate. Adjacent sections were stained with Masson–Goldner trichrome, and two sections were left unstained for the evaluation of calcein and tetracycline labeling. Histomorphometric examination was performed in a blinded, unbiased manner using imaging system software (simple PCI system; Hamamatsu, Sewickley, PA, USA). Variables were measured and reported as previously described [10, 12, 17, 18] using the terminology recommended by the Histomorphometry Nomenclature Committee of the American Society for Bone and Mineral Research (ASBMR) [19]. Static measurements and histodynamic parameters were measured from five different microscopic fields at 100 × magnification. The number of adipocytes within the examined tissue area as well as the individual adipocyte area and diameter were also determined. These data are expressed as the total adipocyte number per tissue area (no./mm2) and the adipocyte diameter (μm). The histodynamic parameters for mineral apposition rate (MAR, μm/day) in the metaphysis of the proximal femur were measured from the same specimens as described.
RNA isolation and quantitative real-time RT-PCR analysis
Total RNA was isolated from the right tibia of each animal, and the gene expression in the entire bone was analyzed using quantitative real-time reverse transcription-polymerase chain reaction (RT-PCR) (LightCycler Instrument, Roche, Germany). Immediately after the animal was killed, all remaining soft tissue was removed from the tibia, which was then cut into pieces and homogenized in TRIzol reagent (Life Technologies, Grand Island, NY, USA). Next, RNA isolation was performed as described by the manufacturer, and real-time RT-PCR was performed as previously described [20]. Levels of 18S rRNA were used to correct for intersample variation.
Statistical analysis
After establishing homogeneity of variance and a normal distribution of the data, statistically significant differences between groups were determined using one-way analysis of variance (ANOVA) followed by a post hoc Student–Neuman–Keuls analysis and SPSS (Statistical Package for the Social Sciences) 17.0 software (SPSS, Chicago, IL, USA). In all cases, P values < 0.05 were considered significant. Histomorphometric data were analyzed using SPSS as well, and all values are presented as the mean ± SD.
Results
Baseline characteristics
The pre- and post-treatment body weights and FBG levels for each of the four groups are summarized in Table 1. Before treatment, there were no differences in FBG or body weight among the four groups. After the 6-week treatment, the post-treatment FBG levels of animals in the Pio, Rosi, and Met groups were lower than the pre-treatment values and significantly lower than the values from the placebo group, whereas no differences were found among the three hypoglycemic treatments. After 6 weeks of feeding and compared with the pre-treatment body weights, the average post-treatment body weights increased significantly in all four groups. Notably, the greatest gain in body weight was observed when the Rosi group was compared to the placebo group (P = 0.006) and the Met group (P = 0.007); however, there was no significant difference between the Pio and Rosi groups.
Analysis of bone microarchitecture and BMD
Bone microarchitecture parameters and BMD values of the femora are shown in Table 2. Compared with the placebo, Pio, and Rosi groups, the Met group had significantly higher BV/TV ratios and lower Tb.Sp. values. Although the Rosi group had a relatively higher degree of Tb.Sp. (0.173 ± 0.024 μm), there were no significant differences in BV/TV, Tb.Th, Tb.N, and Tb.Sp. among the placebo, Pio, and Rosi groups. Furthermore, the femoral BMD value for the Met group was significantly higher than that of the Rosi group (P = 0.009).
At L2–L5, however, no significant differences in BMD value or the analyzed bone microarchitecture parameters were observed in mice treated with the two TZD drugs, metformin, or placebo (Table 3).
Histomorphometric analysis of bone formation and adipocytes
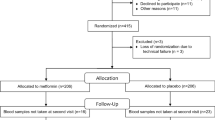
As shown in Fig. 1 and Table 4, the highest osteoid width and MAR values were found in the Met group, whereas significantly increased bone marrow fat content, increased numbers of adipocytes, decreased osteoid width, and lower MAR values were detected in the Rosi group. The number of adipocytes in the Rosi group was almost fivefold higher than that of the Met group and was fourfold higher than of the placebo and the Pio groups. The adipocyte diameter, however, was similar between the four groups. No significant differences in the static or dynamic parameters were found between the placebo group and the Pio group.
Examination of the histological appearance of the proximal femora from the placebo, pioglitazone, rosiglitazone, and metformin groups. Mineralized bone tissue is stained green; osteoid is stained red. Unstained areas in the bone marrow represent empty spaces previously occupied by adipocytes. Adipocytes were recognized based on the distinct appearance of round empty spaces in the processed specimens. ×100
The expression of phenotype-specific gene markers
The expression of Bmp2, Runx2, and Fabp4 is presented in Table 5. In contrast to our expectations, no significant differences in Runx2 expression were detected across the four groups. The expression of this osteoblast-specific transcription factor was not suppressed by either rosiglitazone or pioglitazone treatment. The expression of Bmp2 in the Rosi group was similar to that of the placebo group, whereas it was significantly downregulated by treatment with pioglitazone and metformin. As expected, the highest expression of Fabp4 was detected in the Rosi group when compared to the placebo, Pio, and Met groups (P = 2.50E − 5, 2.88E − 6, and 2.76E − 6, respectively).
Discussion
TZD and metformin are two types of priority antidiabetic drugs that are commonly prescribed for patients with insulin resistance. Animal studies demonstrated that rosiglitazone administration resulted in significant decreases in total body BMD, bone formation rate, bone volume, trabecular width, and trabecular number, and this was also accompanied with an increase in trabecular spacing and fat content in the bone marrow of 6-month-old nondiabetic C57BL/6 mice. The expression of the osteoblast-specific genes Runx2/Cbfa1, Dlx5, and alpha1(I)collagen were decreased, whereas the expression of the adipocyte-specific fatty acid-binding protein aP2 was increased simultaneously [10]. However, in young and growing (4-week-old) animals, only the bone formation rate was significantly suppressed by rosiglitazone treatment, whereas no other osteoblast parameters were significantly affected [12].
The effects of pioglitazone on the skeleton are controversial, as opposing conclusions have been drawn from several clinical studies. In 2009, Toulis et al. [21] reported that pioglitazone treatment may not be associated with an increased fracture risk in women or men with T2DM. In contrast, Dormandy et al. [22] from the same year demonstrated a higher rate of bone fractures in pioglitazone-treated female patients. In premenopausal patients with polycystic ovary syndrome (PCOS), pioglitazone treatment significantly decreased lumbar and hip bone mineral density along with decreased bone turnover [23].
Metformin has been demonstrated to induce the differentiation and mineralization of osteoblasts via activation of the AMP-activated protein kinase (AMPK) signaling pathway, and also to induce Bmp2 expression in vitro. In ovariectomized (OVX) rats, metformin enhanced osteoblast differentiation, prevented bone loss, and decreased tartrate-resistant acid phosphatase (TRAP)-positive cells [14]. Furthermore, metformin may inhibit osteoclast differentiation [24] and stimulate osteoblast differentiation through the transactivation of Runx2 via the AMPK/USF-1/SHP regulatory cascade in vitro [25, 26].
In the current study, we investigated the effects of rosiglitazone, pioglitazone, and metformin on the skeleton in C57BL6J ob/ob mice using DXA, micro-CT, and histomorphometric analyses. Consistent with the foregoing study [10], we observed that rosiglitazone treatment decreased femoral BMD accompanied by an increased bone marrow fat content and a decreased MAR compared with placebo and metformin treatments. However, no adverse effect on the bones caused by pioglitazone treatment was found in our study. Moreover, metformin treatment conferred significant positive effects on bones when compared to the rosiglitazone and placebo treatments. We observed different impacts of metformin on femur and lumbar spine consequent to their different composition. Because the femur is mainly composed of cortical bone whereas the lumbar spine is mainly composed of cancellous bone, we concluded that the effects of metformin differ for these two types of bone tissue. No changes in spongiosa microarchitecture were found to result from rosiglitazone and pioglitazone therapies. Moreover, the expression of phenotype-specific gene markers, such as bone formation marker (Bmp2), osteoblast-specific transcription factor (Runx2), and adipocyte-specific marker (Fabp4), was not simply downregulated or upregulated along with the BMD and bone microarchitecture changes. In the Rosi group, the expression of Runx2 and Bmp2 was not downregulated, whereas the expression of adipocyte-specific marker (Fabp4) was upregulated almost sixfold compared to the placebo group.
The Fabp4 gene encodes the adipocyte fatty acid-binding protein and plays an important role in fatty acid uptake, transport, and metabolism. Cabre et al. [27] demonstrated that the plasma FABP4 level and the level of peripheral blood mononuclear cell PPAR-γ activity were significantly higher in TZD-treated T2DM patients than in non-TZD-treated T2DM patients. Furthermore, TZD treatment increased Fabp4 mRNA levels, intracellular protein levels, and extracellular secretion from human adipocytes. As expected, the highest Fabp4 expression was detected along with the highest fat content in the bone marrow for the Rosi group. In contrast, Fabp4 expression in the Pio group was similar to that of the placebo and the metformin treatment groups.
In general, bone morphogenetic proteins (BMPs) are characterized as potent bone-inducing molecules. BMP cytokines are produced mainly by mesenchymal lineage cells, which control osteoblast and adipocyte differentiation and are essential for bone formation and bone homeostasis. Under conditions of TZD treatment, however, in vitro studies have confirmed that Bmp2 activity strongly stimulates adipogenic differentiation of murine 3T3-L1 preadipocytes. Therefore, Sottile and Seuwen [28] demonstrated that Bmp2 can act as a potent adipogenic agent if activated concurrently with TZD treatment. Additional studies have indicated that type IB and IA BMP receptors transmit different signals to Bmp2 and play critical roles in both the specification and the differentiation of osteoblasts and adipocytes [29]. Nonetheless, Bmp2 expression induced by high glucose can be suppressed by pioglitazone [30]. Therefore, we suggest that the significantly increased fat content in the bone marrow may result from not only upregulated Fabp4, but also Bmp2 expression, in addition to the rosiglitazone treatment. Compared to rosiglitazone treatment, the downregulated Fabp4 and Bmp2 expression associated with metformin treatment resulted in a lower fat content in the bone marrow, a higher femoral BMD, and improved bone microarchitecture. Moreover, the suppressed Bmp2 expression and the normal Runx2 and Fabp4 expression induced by pioglitazone contributed to improved skeletal phenotypes in the Pio treatment group compared to the Rosi group.
Runx2 is a member of the RUNX family of transcription factors and encodes a nuclear protein with a Runt DNA-binding domain. This protein is essential for osteoblastic differentiation and skeletal morphogenesis, acting as a scaffold for nucleic acids and regulatory factors involved in skeletal gene expression. In this study, no significant difference in Runx2 expression was observed for the placebo group or for groups treated with any one of the three hypoglycemic drugs. Rosiglitazone treatment induced lower trabecular BMD as well as defects in parameters of bone microarchitecture, which occurred in parallel with increased Fabp4 expression and normal Bmp2 and Runx2 gene expression. We suggest that the mechanism responsible for rosiglitazone-related bone loss may not be simply the inverse relationship between osteoblasts and adipocytes or the potential downregulated bone formation in insulin-resistant mice.
In summary, we conclude the following points regarding the skeletal effects of hypoglycemic drug treatment. First, metformin is a bone-friendly, antidiabetic drug. It downregulated adipogenesis in insulin-resistant obese mice to maintain BMD, antagonizes bone loss, and protects bone microarchitecture. Second, rosiglitazone treatment had adverse skeletal effects even in young female insulin-resistant mice at the trabecular bone. Third, under rosiglitazone therapy, the expression of Bmp2 and Fabp4 worked together to increase fat content in the bone marrow and to damage the BMD and bone microarchitecture of the trabecular bone, although the expression of the osteoblast-specific gene (Runx2) was not downregulated in C57BL6J ob/ob mice. Thus, the TZD-induced osteoblast–adipocyte relationship must be more complicated than previously assumed. Last, compared with rosiglitazone, no evidence of adverse skeletal effects was found to result from pioglitazone treatment in C57BL6J ob/ob mice.
References
Yang W, Lu J, Weng J, Jia W, Ji L, Xiao J, Shan Z, Liu J, Tian H, Ji Q, Zhu D, Ge J, Lin L, Chen L, Guo X, Zhao Z, Li Q, Zhou Z, Shan G, He J (2010) Prevalence of diabetes among men and women in China. N Engl J Med 362:1090–1101
Vestergaard P (2007) Discrepancies in bone mineral density and fracture risk in patients with type 1 and type 2 diabetes: a meta-analysis. Osteoporos Int 18:427–444
Janghorbani M, Van Dam RM, Willett WC, Hu FB (2007) Systematic review of type 1 and type 2 diabetes mellitus and risk of fracture. Am J Epidemiol 166:495–505
Kahn SE, Zinman B, Lachin JM, Haffner SM, Herman WH, Holman RR, Kravitz BG, Yu D, Heise MA, Aftring RP, Viberti G (2008) Rosiglitazone-associated fractures in type 2 diabetes: an analysis from A Diabetes Outcome Progression Trial (ADOPT). Diabetes Care 31:845–851
Aubert RE, Herrera V, Chen W, Haffner SM, Pendergrass M (2010) Rosiglitazone and pioglitazone increase fracture risk in women and men with type 2 diabetes. Diabetes Obes Metab 12:716–721
Douglas IJ, Evans SJ, Pocock S, Smeeth L (2009) The risk of fractures associated with thiazolidinediones: a self-controlled case-series study. PLoS Med 6:e1000154
Berberoglu Z, Yazici AC, Demirag NG (2010) Effects of rosiglitazone on bone mineral density and remodelling parameters in postmenopausal diabetic women: a 2-year follow-up study. Clin Endocrinol (Oxf) 73:305–312
Loke YK, Singh S, Furberg CD (2009) Long-term use of thiazolidinediones and fractures in type 2 diabetes: a meta-analysis. CMAJ 180:32–39
Jones SG, Momin SR, Good MW, Shea TK, Patric K (2009) Distal upper and lower limb fractures associated with thiazolidinedione use. Am J Manag Care 15:491–496
Rzonca SO, Suva LJ, Gaddy D, Montague DC, Lecka-Czernik B (2004) Bone is a target for the antidiabetic compound rosiglitazone. Endocrinology 145:401–406
Viccica G, Francucci CM, Marcocci C (2010) The role of PPARgamma for the osteoblastic differentiation. J Endocrinol Invest 33:9–12
Lazarenko OP, Rzonca SO, Hogue WR, Swain FL, Suva LJ, Lecka-Czernik B (2007) Rosiglitazone induces decreases in bone mass and strength that are reminiscent of aged bone. Endocrinology 148:2669–2680
Adami S (2009) Bone health in diabetes: considerations for clinical management. Curr Med Res Opin 25:1057–1072
Kanazawa I, Yamaguchi T, Yano S, Yamauchi M, Sugimoto T (2008) Metformin enhances the differentiation and mineralization of osteoblastic MC3T3-E1 cells via AMP kinase activation as well as eNOS and BMP-2 expression. Biochem Biophys Res Commun 375:414–419
Srinivasan K, Ramarao P (2007) Animal models in type 2 diabetes research: an overview. Indian J Med Res 125:451–472
Bloebaum RD, Willie BM, Mitchell BS, Hofmann AA (2007) Relationship between bone ingrowth, mineral apposition rate, and osteoblast activity. J Biomed Mater Res A 81:505–514
Ali AA, Weinstein RS, Stewart SA, Parfitt AM, Manolagas SC, Jilka RL (2005) Rosiglitazone causes bone loss in mice by suppressing osteoblast differentiation and bone formation. Endocrinology 146:1226–1235
Ma L, Ji JL, Ji H, Yu X, Ding LJ, Liu K, Li YQ (2010) Telmisartan alleviates rosiglitazone-induced bone loss in ovariectomized spontaneous hypertensive rats. Bone (NY) 47:5–11
Parfitt AM, Drezner MK, Glorieux FH, Kanis JA, Malluche H, Meunier PJ, Ott SM, Recker RR (1987) Bone histomorphometry: standardization of nomenclature, symbols, and units. Report of the ASBMR Histomorphometry Nomenclature Committee. J Bone Miner Res 2:595–610
Bustin SA (2000) Absolute quantification of mRNA using real-time reverse transcription polymerase chain reaction assays. J Mol Endocrinol 25:169–193
Toulis KA, Goulis DG, Anastasilakis AD (2009) Thiazolidinedione use and the risk of fractures. CMAJ 180:841–842 (author reply 842–843)
Dormandy J, Bhattacharya M, van Troostenburg de Bruyn AR (2009) Safety and tolerability of pioglitazone in high-risk patients with type 2 diabetes: an overview of data from PROactive. Drug Saf 32:187–202
Glintborg D, Andersen M, Hagen C, Heickendorff L, Hermann AP (2008) Association of pioglitazone treatment with decreased bone mineral density in obese premenopausal patients with polycystic ovary syndrome: a randomized, placebo-controlled trial. J Clin Endocrinol Metab 93:1696–1701
Mai Q, Zhang Z, Xu S, Lu M, Zhou R, Zhao L, Jia C, Wen Z, Jin D, Bai X (2011) Metformin stimulates osteoprotegerin and reduces RANKL expression in osteoblasts and ovariectomized rats. J Cell Biochem 112:2902–2909
Jang WG, Kim EJ, Bae IH, Lee KN, Kim YD, Kim DK, Kim SH, Lee CH, Franceschi RT, Choi HS, Koh JT (2011) Metformin induces osteoblast differentiation via orphan nuclear receptor SHP-mediated transactivation of Runx2. Bone (NY) 48:885–893
Zhen D, Chen Y, Tang X (2010) Metformin reverses the deleterious effects of high glucose on osteoblast function. J Diabetes Complicat 24:334–344
Cabre A, Lazaro I, Girona J, Manzanares JM, Marimon F, Plana N, Heras M, Masana L (2007) Fatty acid binding protein 4 is increased in metabolic syndrome and with thiazolidinedione treatment in diabetic patients. Atherosclerosis 195:e150–e158
Sottile V, Seuwen K (2000) Bone morphogenetic protein-2 stimulates adipogenic differentiation of mesenchymal precursor cells in synergy with BRL 49653 (rosiglitazone). FEBS Lett 475:201–204
Chen D, Ji X, Harris MA, Feng JQ, Karsenty G, Celeste AJ, Rosen V, Mundy GR, Harris SE (1998) Differential roles for bone morphogenetic protein (BMP) receptor type IB and IA in differentiation and specification of mesenchymal precursor cells to osteoblast and adipocyte lineages. J Cell Biol 142:295–305
Zhang M, Zhou SH, Zhao S, Li XP, Liu LP, Shen XQ (2008) Pioglitazone can downregulate bone morphogenetic protein-2 expression induced by high glucose in human umbilical vein endothelial cells. Pharmacology 81:312–316
Acknowledgments
We are grateful to Dr. Guo-Ying Zhu, Dr. Xiao Chen, Dr. Hui-Min Yan, and Dr. Hui Xie for their excellent and generous assistance. The study was supported by the Shanghai Science & Technology Development Fund (Project No. 08411963100) and the Shanghai Natural Science Foundation 11ZR1427300 (Science and Technology commission of Shanghai municipality).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
C. Wang and H. Li contributed equally to this work.
About this article
Cite this article
Wang, C., Li, H., Chen, SG. et al. The skeletal effects of thiazolidinedione and metformin on insulin-resistant mice. J Bone Miner Metab 30, 630–637 (2012). https://doi.org/10.1007/s00774-012-0374-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-012-0374-0