Abstract
The aim of osteoporosis treatment is to prevent future fractures. Although concurrent treatment has been used very frequently for osteoporosis in clinical practice, there are no data on accurate and verified effectiveness of concurrent treatment for fracture prevention in patients with osteoporosis. To clarify the clinical usefulness of concurrent treatment, the Japan Osteoporosis Society has authorized the establishment of the A-TOP (Adequate Treatment of Osteoporosis) research group. The objective of this research is to establish a design for a clinical trial to prove whether concurrent treatment using both alfacalcidol (1-alpha-hydroxycholecalciferol) and alendronate is more effective as compared to treatment using alendronate alone in terms of fracture prevention. The present study was named JOINT (Japanese Osteoporosis Intervention Trial) and is based on a method using national, prospective, randomized, open-labeled, blinded endpoints focusing on postmenopausal osteoporosis with a high risk for fracture. The patients were mainly selected by practitioners and allocated randomly by a central registration system into two groups, of which one received 5 mg/day of alendronate alone, and the other received 1 μg/day of 1-alpha-hydroxycholecalciferol (alfacalcidol) in addition to the alendronate. The endpoints focused primarily on fracture prevention, and the patients’ quality of life (QOL) and change in body height, as well as adherence and the adverse events of the treatments were evaluated secondarily. To obtain sufficient statistical power in the events during a 2-year observation period, the patients who are expected to have higher risk were selected to participate in this study, and it was decided that the final plan would involve 890 patients per group (two-sided alpha = 0.05, power = 0.8). Data collection began in November 2003. Correspondence regarding the registration of the investigator and the progress of the study was conducted through a web system from the Public Health Research Foundation to practitioners.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Osteoporosis, which is characterized by compromised bone strength and increased susceptibility to fractures, which lead to deterioration in the QOL and increased mortality, is a national burden on an aging society [1, 2]. However, recent studies indicate that treatment with a parathyroid hormone, bisphosphonates or a selective estrogen receptor modulator (SERM) [3–9] may decrease the risk of fractures in patients with osteoporosis.
Although bisphosphonate treatment currently represents the most powerful form of treatment available for fracture prevention in osteoporotic patients, it has not succeeded in completely preventing osteoporotic fractures [3–5, 7–9]. Therefore, concurrent treatment of osteoporosis has been frequently used by Japanese practitioners without any concrete evidence regarding fracture reduction. Since the concept of evidence-based medicine (EBM) has been introduced to clinical practice since the 1990s [10], the Japan Osteoporosis Society and the Japanese Society of Bone Mineral Research have edited the clinical guideline for treatment of osteoporosis (Chief editor: Hajime Orimo [11]). However, the writers recognized that there was a lack of evidence in the effectiveness of concurrent treatment of osteoporosis. Furthermore, it was expected that the patients who visit clinics have varying degrees of risk of fracture, which may differ from the degree of those who participated in development trials for bisphosphonates. This possibility would make it easier to obtain pragmatic evidence in general clinical practice.
Starting in 2000, the Japan Osteoporosis Society had planned to investigate the effectiveness of treatment of osteoporosis in order to provide evidence to general practitioners. Before constructing evidence, some feasibility studies were required to confirm the consensus in the diagnosis of incident fractures among the researchers and to elucidate the risk of future fractures in the patient population. In addition to these efforts in the field of osteoporosis, the Japanese government also established an ethical guideline for clinical trials [12], and the International Committee of Medical Journal Editors launched a clinical trial registry [13]. Such kinds of progress in the circumstances of clinical trials have enabled for investigator-initiated clinical trials in general practice.
The Adequate Treatment of Osteoporosis (A-TOP) study group was established in 2000 [11] in affiliation with the Japan Osteoporosis Society and organized a team for clinical trial management. The team consisted of clinical investigators (planning and analysis), foundation (funding) managers, officers from non-profit organization (data management) and several companies (data collection). This was the first joint team to create the post-making evidence for osteoporosis. In November 2003, A-TOP initiated a randomized clinical trial referred to as the Japanese Osteoporosis Intervention Trial (JOINT). The purpose of JOINT was to confirm the clinical significance of concurrent use of osteoporotic drugs. The first protocol, named JOINT-01, was initiated in 2002, but was suspended the following year due to a change in drug labeling. A second protocol, named JOINT-02, was established to clarify the effect of adding 1-alpha-hydroxycholecalciferol (alfacalcidol) to alendronate (ALN), using the incident fracture rate as the primary endpoint. In this paper, the rationale, organization and study design of JOINT-02 are introduced.
Rationale and aims
In 2002, the Japan Society of Osteoporosis sent a letter to randomly selected practitioners and enclosed a questionnaire regarding whether concurrent treatment using bisphosphonate and another drug was being utilized to treat osteoporosis. Surprisingly, 87.8% (79/90 practitioner) of the doctors who responded did have experience using concurrent treatment [14]. The most frequent drugs used in concurrent treatment with amino-bisphosphonate were alfacalcidol (93.7%), followed by calcitonin (50.6%), as there were expectations for these drugs to exhibit more potent inhibition of fracture occurrence or more significant increase in BMD, even though there was no apparent evidence. In addition to the lack of evidence related to fracture prevention, the safety profile of concurrent treatment had not been evaluated. Thus, evaluations of the effectiveness and safety of concurrent treatment were urgently required. Etidronate [15] and ALN [8, 9] were used as the drugs to confirm anti-fracture effectiveness in comparison to alfacalcidol in Japanese osteoporotic patients. However, these clinical trials were carried out at specific institutions and were initiated by experts in accordance with tight regulations. As a result, there may have been differences in the selected treatment and in the backgrounds of the patients between treatments conducted at these institutions and those conducted in general practice. In addition, the adherence of the treatment is expected to be lower in general practice than in institutions with experts who are committed to developmental trials. Thus, pragmatic study is urgently needed to evaluate whether bisphosphonates are effective to the same extent at the level of general practitioners as compared to the prior study (Phase III study).
Feasibility studies
The Japan Osteoporosis Society started discussions to execute a national clinical trial for obtaining evidence regarding the effectiveness of concurrent treatment in 2000. An executive committee of A-TOP was organized in 2002 and planned on forming a consensus regarding judgment standards for pre-existing fractures and incident vertebral fractures [16]. Morphometric criteria for incident fractures combined with a semi-quantitative assessment were thought to provide useful information on the study of clinical osteoporosis, especially for international comparisons. Next, to assume the number of participants in the clinical trial, the incident fracture rate and the risk of incident fracture were analyzed in the patient population, and the number of participants with sufficient statistical power [17] was calculated. Bone resorption marker was an independent risk factor for incident vertebral fractures in Japanese women. When the newly discovered risk factor was incorporated into the inclusion criteria in addition to conventional selection criteria such as age, prevalent fractures and bone mineral density, a reduction of about 40% in the estimated sample size was achieved. Thus, measurement of bone resorption markers is useful in reducing the sample size and the observation period in fracture-prevention studies carried out for developing drugs used to treat osteoporosis.
Materials and methods
Study design
Objective
JOINT was the first national, prospective, randomized, multicenter, open-labeled, blinded endpoints, controlled trial for osteoporosis made up mainly of practitioners of investigators in Japan. The objective of JOINT-02 was to clarify additive efficacy in terms of fracture prevention and safety, QOL and adherence in simultaneous use of alfacalcidol and ALN.
Subjects, intervention and endpoints
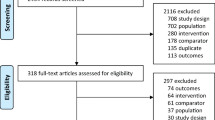
Confirmations regarding the patients were made by practitioners based on the inclusion and exclusion criteria (Table 1) after obtaining written informed consent. The participants were selected by the practitioners and registered by Japan Clinical Research Support Unit (JCRSU), and then randomly allocated with a modified minimization method using age, number of pre-existing vertebral fracture number, bone mineral density (BMD) and value of bone metabolic marker into the group to be administered only ALN or the group that was to be administered both ALN and alfacalcidol. Registration and allocation of the participants were carried out on the Internet. After initiation of the assigned treatment, clinical data were collected at intervals of half a year for 2 years by I’cros Co., Ltd., through their visiting data collection service. Data were input to the database using a web system developed by ING Corporation. The primary endpoint was to compare the incident vertebral fracture rate between the intervention arms. The secondary endpoints were to compare the differences in the time to first incident vertebral fracture, non-vertebral fracture rate, bone mineral density, adherence, QOL and safety (Fig. 1). In addition, sub-group analyses categorized by baseline characteristics such as age, body mass index (BMI), serum 25-hydroxyl vitamin D levels, the number of pre-existing vertebral fractures and fracture grade were candidate factors. If participants wanted to change the designated treatment because of side effects or occurrence of fractures, they were permitted to do so, and follow-up observations were continued. Please see Table 1 and Fig. 1.
Sample size
Assumptions regarding the fracture rate in the ALN group were made based on a paper by Kushida et al. (Phase III trial for alendronate), in which it is reported that there was a 12.2% fracture rate during observations conducted over 2 years [8]. Since there are not much data on concurrent use of ALN and alfacalcidol [18], the authors’ expectations were such that the effects of ALN would be added to those of alfacalcidol and that the hazard ratio of the alfacalcidol combined arm to ALN alone would be 0.64 [19]. The sample size was then estimated to be 890 cases per arm (two-sided alpha = 0.05, power = 0.8), taking account of a dropout rate of 10% referring to the value of the prior clinical trial of fracture intervention [4].
Fracture evaluation
X-ray films of conventional lateral radiographs of lumbar and thoracic vertebrae were taken and collected by I’cros Co., Ltd. After masking the patient’s information, two independent readers (orthopedist, TN and radiologist, MF) simultaneously reviewed films from T4 to L4 in chronological sequence and graded vertebral fracture based on a semi-quantitative method [20]. Before the start of the study, these two observers held meetings to make adjustments between their own criteria for grading vertebral fractures. When the diagnosis of pre-existing fractures made by the reviewers differed from those made by the practitioners, the reviewers’ diagnosis was adopted preferentially. If inconsistencies arose between the readers in diagnosing pre-existing and incident vertebral fractures, the two readers negotiated between themselves to reach a consensus. Incident bone fractures other than those of the vertebrae were comprehended from the chart, and the occurrence of fractures was confirmed based on X-ray films or a record of the operation.
Clinical data
BMD at the lumbar vertebrae, hip (proximal femur), distal radius (dual energy X-ray absorptiometry) or left-sided second metacalpal bone (microdensitometry) was measured at baseline and at 6-month intervals for 2 years at each institute. The data of BMD obtained from the different machines and from different bone sites were calculated as the percentage change in each time point from the baseline value. The statistical difference in change of BMD between the group that received combined treatment and the group that was administered only ALN was compared based on each set of data for BMD for the different bone sites. Body height was measured at baseline, 12 and 24 months. Bone turnover markers (urinary type I collagen cross-linked N-telopeptide or urinary excretion of deoxypyridinoline) were measured at baseline and again 6 months after initiating treatment. QOL was assessed by using self-administered questionnaires (JOQOL and EQ-5D) at baseline and at 6, 12 and 24 months after initiating treatment [21]. Serum samples were sent to the central laboratory (SRL Co., Japan), and 25-hydroxyl vitamin D concentrations were measured. Other routine biochemical examinations were carried out at baseline and at 2 years after initiating treatment in order to estimate biochemical adverse events. All adverse events were reported to JCRSU, coded by MedDRA, and categorized as either “known” or “unknown.” If an unknown adverse effect occurred, it was reported to the investigator and ethical committee.
Ethics and registration
Ethical issues regarding protocol were reviewed by the ethical committee for JOINT under the Declaration of Helsinki (Dr. Rikushi Morita, Chairman). If it turned out that a patient was at a disadvantage under observation, the ethical committee was given permission to stop the protocol. This study was registered at UMIN-CTR (University Hospital Medical Information Network—Clinical Trial Registry) with the number C000000001.
Statistical analysis
Analysis of the intent to treat principle was applied to the statistical analysis. Efficacy analysis uses a full analysis set (FAS), and all of the enrolled patients are applied to the analysis except for patients without efficacy data, patients who do not correspond to inclusion criteria and patients who do not receive treatment. The PPS (protocol per set) group is defined as consisting of patients without any serious protocol violation.
Recruitment of the practitioner
The explanatory meeting of the protocol and registration was held in all of Japan. The executive members of the A-TOP research group were responsible for the presentation of the protocol and for the recruitment of study institutions and practitioners. The A-TOP committee created the WEB site on the Internet so that the registration of the study could be executed directly. I’cros Co., Ltd., was also involved as a collaborator in calling practitioners.
Results and discussion
Several principles had to be considered for acceptance of concurrent treatment: firstly, the concurrent treatment should be clinically and statistically significantly more effective than the basic treatment; secondly, the concurrent treatment should be of the same level of safety as single treatment; thirdly, the concurrent treatment should be cost-effective. Although these principles should be evaluated before adopting concurrent treatment, the authors have applied concurrent treatment to osteoporosis widely, without any background evidence. Among these principles, the authors have decided to evaluate the first two issues, effectiveness and safety, in the present study. Since this type of evaluation is absolutely required by a clinician, a researcher-initiative study was considered as being the most suitable type of evaluation. This was the reason why the authors decided to use a researcher-initiative clinical trial in determining the effectiveness of concurrent treatment for osteoporosis. The JOINT-02 protocol was the first randomized, controlled trial conducted nationwide for osteoporosis in Japan initiated by researchers, and its scale was also the largest ever. It was therefore necessary for various organizations to collaborate together, and there have been no previous reports on how to manage the PROBE trial in Japan. This is why we wanted to report the design of JOINT-02. In this paper, we have presented the organization of the A-TOP research group and execution of the JOINT 02 protocol. This is because we believe that this report should help a researcher who is willing to build a new nationwide investigation that is constructed by an organization of clinical research work.
Since the primary aim of JOINT-02 was to determine whether concurrent treatment using ALN and alfacalcidol is superior to treatment using ALN alone in terms of fracture prevention, true (“hard”) endpoints such as vertebral fractures or long bone fractures were selected as the primary endpoint. The diagnosis of whether vertebral fractures were present or not on the X-ray films was made by two independent reviewers who did not have any information about the patient; when the judgment of fractures was split between the two reviewers, the reviewers negotiated with each other. Identifying vertebral fractures is more difficult than identifying long bone fractures due to some cases of new vertebral fractures not showing clinical symptoms and the shape of the vertebral body making it difficult at times to recognize whether there is a fracture. Therefore, to avoid misdiagnosis, diagnosis of pre-existing and incident vertebral fractures was made by two different observers. In cases where there was a discrepancy in the diagnosis of vertebral fractures between the reviewers and the practitioner, which occurred with regard to pre-existing fractures, the reviewers’ judgment was given priority over that of the practitioner.
Surrogate (“soft”) endpoints such as change in BMD or bone turnover markers were considered to be inadequate as primary endpoints in making conclusive statements regarding the efficacy of concurrent treatment. In this type of study, the soft endpoint (BMD or biomarkers) will connect dropout bias less effectively than the case-selected hard endpoint, because such markers are not able to be made blind to the clinicians. Furthermore, previous studies indicate that changes in BMD or bone markers do not predict future fractures [22–24].
In recent literature, it has been reported that poor adherence of bisphosphonates leads to a decline in the beneficial effects of this drug on bone [25–28]. It is expected that in contrast to prior developmental trials, this current study may have a higher dropout rate, since in a researcher-initiative study, the registered practitioner is not forced to maintain adherence very strictly. As a result, adherence in the present study may resemble the actual circumstances of adherence to bisphosphonate treatment by a general practitioner. It will be interesting to determine whether adherence in this study modifies fracture prevention by alendronate.
Although a careful plan for this study has been set up, the results will be applied to osteoporosis patients with the same background as the present study population, but not adapted to the entire osteoporosis population. Despite this limitation, we believe that the results will give us very important information regarding the concurrent treatment of osteoporosis.
References
NIH Consensus Development Panel on Osteoporosis Prevention, Diagnosis, and Therapy (2001) Osteoporosis prevention, diagnosis, and therapy. JAMA 285:785–795
Oleksik A, Lips P, Dawson A, Minshall ME, Shen W, Cooper C, Kanis J (2000) Health-related quality of life in postmenopausal women with low BMD with or without prevalent vertebral fractures. J Bone Miner Res 15:1384–1392
Black DM, Cummings SR, Karpf DB, Cauley JA, Thompson DE, Nevitt MC, Bauer DC, Genant HK, Haskell WL, Marcus R, Ott SM, Torner JC, Quandt SA, Reiss TF, Ensrud KE (1996) Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture Intervention Trial Research Group. Lancet 348:1535–1541
Cummings SR, Black DM, Thompson DE, Applegate WB, Barrett-Connor E, Musliner TA, Palermo L, Prineas R, Rubin SM, Scott JC, Vogt T, Wallace R, Yates AJ, LaCroix AZ (1998) Effect of alendronate on risk of fracture in women with low bone density but without vertebral fractures: results from the Fracture Intervention Trial. JAMA 280:2077–2082
Harris ST, Watts NB, Genant HK, McKeever CD, Hangartner T, Keller M, Chesnut CH 3rd, Brown J, Eriksen EF, Hoseyni MS, Axelrod DW, Miller PD (1999) Effects of risedronate treatment on vertebral and nonvertebral fractures in women with postmenopausal osteoporosis: a randomized controlled trial. Vertebral Efficacy with Risedronate Therapy (VERT) Study Group. JAMA 282:1344–1352
Ettinger B, Black DM, Mitlak BH, Knickerbocker RK, Nickelsen T, Genant HK, Christiansen C, Delmas PD, Zanchetta JR, Stakkestad J, Glüer CC, Krueger K, Cohen FJ, Eckert S, Ensrud KE, Avioli LV, Lips P, Cummings SR (1999) Reduction of vertebral fracture risk in postmenopausal women with osteoporosis treated with raloxifene: results from a 3-year randomized clinical trial. Multiple Outcomes of Raloxifene Evaluation (MORE) Investigators. JAMA 282:637–645
Shiraki M, Kushida K, Fukunaga M, Kishimoto H, Taga M, Nakamura T, Kaneda K, Minaguchi H, Inoue T, Morii H, Tomita A, Yamamoto K, Nagata Y, Nakashima M, Orimo H (1999) A double-masked multicenter comparative study between alendronate and alfacalcidol in Japanese patients with osteoporosis. The Alendronate Phase III Osteoporosis Treatment Research Group. Osteoporos Int 10:183–192
Kushida K, Shiraki M, Nakamura T, Kishimoto H, Morii H, Yamamoto K, Kaneda K, Fukunaga M, Inoue T, Nakashima M, Orimo H (2002) The efficacy of alendronate in reducing the risk for vertebral fracture in Japanese patients with osteoporosis. Curr Ther Res 63:606–620
Kushida K, Shiraki M, Nakamura T, Kishimoto H, Morii H, Yamamoto K, Kaneda K, Fukunaga M, Inoue T, Nakashima M, Orimo H (2004) Alendronate reduced vertebral fracture risk in postmenopausal Japanese women with osteoporosis: a 3-year follow-up study. J Bone Miner Metab 22:462–468
Sckett DL, Rosenberg WMC, Gray JAM, Haynes RB, Richardson WS (1996) Evidence based medicine; what it is and what it isn’t. Br Med J 312:71–72
Japanese Osteoporosis Guideline 2006, Chief editor: Hajime Orimo, Life science Publish corp (article in Japanese)
Ministry of Health, Labour and Welfare. http://www.imcj.go.jp/rinri/main/02.htm (article in Japanese)
DeAngelis CD, Drazen JM, Frizelle FA, Haug C, Hoey J, Horton R, Kotzin S, Laine C, Marusic A, Overbeke AJ, Schroeder TV, Sox HC, Van Der Weyden MB (2004) International Committee of Medical Journal Editors. Clinical trial registration: a statement from the International Committee of Medical Journal Editors. JAMA 292:1363–1364
Shiraki M, Ohta H, Hosoi T, Kuroda T, Orimo H (2003) A-TOP study plane (3), survey of bisphosphonate. Osteoporosis Jpn 11:665–669 (article in Japanese)
Fujita T, Orimo H, Inoue T, Kaneda K, Sakurai M, Morita R, Morii H, Yamamoto K, Takaoka K (1993) Double-blind multicenter comparative study with alfacalcidol of etidronate disodium (EHDP) in involutional osteoporosis. Clin Eval 21:261–302
Fukunaga M, Nakamura T, Shiraki M, Kuroda T, Ohta H, Hosoi T, Orimo H (2004) Absolute height reduction and percent height ratio of the vertebral body in incident fracture in Japanese women. J Bone Miner Metab 22:104–110
Shiraki M, Kuroda T, Nakamura T, Fukunaga M, Hosoi T, Orimo H, Makino K, Adequate Treatment of Osteoporosis (A-TOP) Research Group (2006) The sample size required for intervention studies on fracture prevention can be decreased by using a bone resorption marker in the inclusion criteria: prospective study of a subset of the Nagano Cohort, on behalf of the Adequate Treatment of Osteoporosis (A-TOP) Research Group. J Bone Miner Metab 24:219–225
Frediani B (1998) Effects of combined treatment with calcitriol plus alendronate on bone mass and bone turnover in postmenopausal osteoporosis two year of continuous treatment. Clin Drug Invest 15:235–244
Cranney A, Guyatt G, Griffith L, Wells G, Tugwell P, Rosen C (2002) Summary of meta-analyses of therapies for postmenopausal osteoporosis. Endocr Rev 23:570–578
Genant HK, Jergas M, Palermo L, Nevitt M, Valentin RS, Black D, Cummings SR (1996) Comparison of semiquantitative visual and quantitative morphometric assessment of prevalent and incident vertebral fractures in osteoporosis. The Study of Osteoporotic Fractures Research Group. J Bone Miner Res 11:984–996
JOQOL Osteoporosis Diagnostic Criteria Review Committee: Japanese Society for Bone and Mineral Research (2001) Diagnostic criteria for primary osteoporosis: year 2000 revision. J Bone Miner Metab 19:331–337
Delmas PD, Seeman E (2004) Changes in bone mineral density explain little of the reduction in vertebral or nonvertebral fracture risk with anti-resorptive therapy. Bone 34:599–604
Earstell R, Barton I, Hannon RA, Chines A, Garnero P, Delmas PD (2003) Relationship of early changes in bone resorption to the reduction in fracture risk with risedronate. J Bone Miner Res 18:1051–1056
Seibel MJ, Naganathan V, Barton I, Grauer A (2004) Relationship between pretreatment bone resorption and vertebral fracture incidence in postmenopausal osteoporotic women treated with risedronate. J Bone Miner Res 19:323–329
Yood RA, Emani S, Reed JI, Lewis BE, Charpentier M, Lydick E (2003) Compliance with pharmacologic therapy for osteoporosis. Osteoporos Int 14:965–968
Gallagher AM, Rietbrock S, Olson M, van Staa TP (2008) Fracture outcomes related to persistence and compliance with oral bisphosphonates. J Bone Miner Res 23:1569–1575
Kamatari M, Koto S, Ozawa N, Urao C, Suzuki Y, Akasaka E, Yanagimoto K, Sakota K (2007) Factors affecting long-term compliance of osteoporotic patients with bisphosphonate treatment and QOL assessment in actual practice: alendronate and risedronate. J Bone Miner Metab 25:302–309
Rabenda V, Hiligsmann M, Reginster JY (2009) Poor adherence to oral bisphosphonate treatment and its consequences: a review of the evidence. Expert Opin Pharmacother 10:2303–2315
Acknowledgments
The authors express thanks to the chairman (Dr. Rikushi Morita) and the members of the ethics committee: Ms. Mamiko Matsumura, Dr. Tetsuro Inoue, Dr. Isao Yoshimura, Dr. Mitsuyoshi Nakajima, Tooru Ebihara, R.Ph., Mr. Shinya Hattori and Mr. Kousaku Uchida. This JOINT study was sponsored by the Public Health Research Foundation. The authors would like to thank those who participated as clinical investigators in JOINT-02. The authors also thank the Japan Arteriosclerosis Prevention Fund, Teijin Pharma Limited, Asahi Kasei Corporation, Takeda Pharmaceutical Company Limited, GE Healthcare Japan, Toyo Medic Co., Ltd., Banyu Pharmaceutical Co., Ltd., and Dainippon Sumitomo Pharma Co., Ltd., for their generous donations.
Author information
Authors and Affiliations
Corresponding author
Additional information
For the A-TOP (Adequate Treatment of Osteoporosis) Research Group.
About this article
Cite this article
Shiraki, M., Kuroda, T., Miyakawa, N. et al. Design of a pragmatic approach to evaluate the effectiveness of concurrent treatment for the prevention of osteoporotic fractures. J Bone Miner Metab 29, 37–43 (2011). https://doi.org/10.1007/s00774-010-0188-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-010-0188-x