Abstract
Nitrogen-containing bisphosphonates such as zoledronic acid (ZOL) and pamidronate have been widely and successfully used for the treatment of cancer patients with bone metastases and/or hypercalcemia. Accumulating recent reports have shown that cancer patients who have received these bisphosphonates occasionally manifest bisphosphonate-related osteonecrosis of the jaw (BRONJ) following dental treatments, including tooth extraction. However, little is known about the pathogenesis of BRONJ to date. Here, to understand the underlying pathogenesis of BRONJ, we examined the effects of ZOL on wound healing of the tooth extraction socket using a mouse tooth extraction model. Histomorphometrical analysis revealed that the amount of new bone and the numbers of blood vessels in the socket were significantly decreased in ZOL-treated mice compared to control mice. Consistent with these results, ZOL significantly inhibited angiogenesis induced by vascular endothelial growth factor in vivo and the proliferation of endothelial cells in culture in a dose-dependent manner. In contrast, etidronate, a non-nitrogen-containing bisphosphonate, showed no effects on osteogenesis and angiogenesis in the socket. ZOL also suppressed the migration of oral epithelial cells, which is a crucial step for tooth socket closure. In addition, ZOL promoted the adherence of Streptococcus mutans to hydroxyapatite and the proliferation of oral bacteria obtained from healthy individuals, suggesting that ZOL may increase the bacterial infection. In conclusion, our data suggest that ZOL delays wound healing of the tooth extraction socket by inhibiting osteogenesis and angiogenesis. Our data also suggest that ZOL alters oral bacterial behaviors. These actions of ZOL may be relevant to the pathogenesis of BRONJ.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bisphosphonates are stable analogues of naturally occurring pyrophosphate-containing compounds and have high affinity for bone minerals [1]. Bisphosphonates are selectively uptaken by osteoclasts and strongly inhibit bone resorption by inducing apoptosis in osteoclasts [2, 3]. Consequently, bisphosphonates have been widely and successfully used in a variety of bone diseases associated with excessive osteoclast activity, including osteoporosis, Paget’s disease, and fibrous dysplasia [4–6]. Another clinical application of bisphosphonates is for metastatic and osteolytic bone disease. Hortobagyi et al. first reported the usefulness of bisphosphonates in the treatment of osteolytic bone metastases of breast cancer [7]. Bisphosphonates are now established as an effective therapeutic intervention for bone metastases of breast, lung, and prostate cancers [8–16].
Bisphosphonates contain two phosphonate groups attached to a single carbon atom, forming a P–C–P structure that is important for inhibition of bone resorption [17]. Bisphosphonates can be divided into two groups based on the presence or absence of a nitrogen atom [17]. Nitrogen atom-containing bisphosphonates exhibit more powerful inhibition of bone resorption, and they strongly induce apoptosis of osteoclasts by inhibiting the mevalonate pathway and the prenylation of small G-proteins [18]. Of note, bisphosphonates including alendronate, risedronate, and zoledronic acid (ZOL), which contain nitrogen atoms, were found to be more potent than bisphosphonates that did not have a nitrogen atom [19].
As bisphosphonates are selectively adsorbed to mineral surfaces in bone, only inflammation and ulceration of the upper gastrointestinal tract have been reported as adverse effects [13]. However, Marx et al. first reported in 2003 that cancer patients who received bisphosphonates occasionally showed osteonecrosis of the jaw (BRONJ) following dental treatments [20], and Ruggiero et al. subsequently reported 63 cases that were identified as having BRONJ [21]. The major manifestation of BRONJ is exposed necrotic bones associated with infection, which is accompanied by pain, swelling, paresthesia, suppuration, soft tissue ulceration, and intra- or extraoral sinus tracts [22]. BRONJ usually occurs more frequently in patients receiving nitrogen-containing bisphosphonates via parenteral route than oral administration [23–28]. Although the reported frequency of BRONJ is not high [29], it causes complicated problems in the dental treatment of patients receiving bisphosphonates. Therefore, the establishment of appropriate mechanism-based management of BRONJ has been awaited. However, little is known about the pathogenesis of BRONJ to date.
It is proposed that BRONJ occurs by a combination of multiple factors. The multiple and diverse pharmacological actions of bisphosphonates and the unique biological characteristics of the oral cavity are likely to be involved in the development of BRONJ. ZOL has been reported to inhibit angiogenesis, which is an essential event for wound healing of the extraction socket [30, 31]. Accordingly, bisphosphonates may possibly delay wound healing of the tooth socket by inhibiting angiogenesis, leading to BRONJ. In addition, BRONJ may be associated with changes in oral bacterial behaviors, because the jaw bones are the only site in which BRONJ is developed. In support of this notion, biofilm formation and the extensive growth of oral bacteria such as Actinomyces were observed at the site of BRONJ [32, 33], raising the possibility that bisphosphonates affect the growth and infectious activity of oral bacteria.
To understand the underlying mechanism of BRONJ, we investigated the effects of ZOL on wound healing of the tooth extraction socket using the mouse tooth extraction model. We also examined whether bisphosphonates modulate the behaviors of oral bacteria.
Materials and methods
Reagents
Zoledronic acid (ZOL) (2-(imidazol-l-yl)-1-hydroxyethylidene-1,1-bisphosphonate) and etidronate (ETI) (disodium (1-hydroxyethylidene) diphosphonate) were provided by Novartis Pharma (Basel, Switzerland) and Dainippon Sumitomo Pharma (Osaka, Japan), respectively.
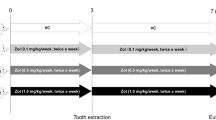
Animal model of tooth extraction
Male C57BL/6J mice 6 weeks of age were obtained from SLC Japan (Hamamatsu, Japan). The right upper first molar was extracted using an iridectome under anesthesia with pentobarbital (0.05 mg/g body weight; Dainippon Sumitomo Pharma). ZOL (250 μg/kg/day) and ETI (250 μg/kg/day) were injected subcutaneously from 7 days before the tooth extraction to 4 days after the extraction. Animals were maintained in an animal room with free access to drinking water and basic diet under controlled conditions and a 12 h:12 h light/dark cycle.
All animal experiments were approved by the Institutional Animal Care and Use Committee of Osaka University Graduate School of Dentistry.
Histological analysis
Five days after tooth extraction, animals were anesthetized with pentobarbital (50 mg/kg BW) and perfused with 4% paraformaldehyde in 0.1 M phosphate buffer through the left cardiac ventricle. The maxilla of the mice was removed, postfixed in the same fixative for 24 h, and decalcified in 10% ethylenediaminetetraacetic acid (EDTA) at room temperature for 2 weeks. Paraffin sections (4 μm thick) were cut using conventional methods and stained with hematoxylin and eosin. The new bone formation area (mm2) and total tooth extraction socket area (mm2) were measured using Image Pro-Plus software (Media Cybermetics, Silver Spring, MD, USA). Data are expressed as the percentage of new bone formation area/total tooth extraction area.
Immunohistochemistry
Paraffin sections were deparaffinized, microwaved for 5 min in 0.01 M citrate buffer, and blocked with 1% bovine serum albumin (BSA) for 30 min. After treatment with 0.3% H2O2 for 30 min, sections were blocked with 1% BSA in phosphate-buffered saline (PBS) for 1 h and incubated overnight at 4°C with rabbit anti-CD31 pAb (1:100; Pharmingen, San Diego, CA, USA). All sections were then treated with biotinylated antirabbit IgG Ab (1:200; Vector Laboratories, Burlingame, CA, USA) for 30 min, followed by reaction with the Vectastain Elite ABC reagent for 30 min. After rinsing in PBS, 3,3′-diaminobenzidine tetrahydrochloride (Vector) was used as a substrate for visualization of the immunocomplex, and the sections were counterstained with hematoxylin. Six sections were chosen from each sample, and the number of CD31-positive vessels was counted under a light microscope. The data were expressed as the number of CD31-positive vessels/mouse.
Cell culture
The murine bone marrow sinus-derived endothelial cell line (BMEC; generously provided by Dr. Hawley, University of Toronto, Toronto, Canada) and human endothelial cell line ECV304 (a generous gift from Dr. Nariaki Matsuura, University of Osaka, Osaka, Japan) were maintained in Dulbecco’s modified Eagle’s medium (DMEM) (pH 7.4, Sigma) supplemented with 10% fetal bovine serum and 100 μg/ml kanamycin sulfate (Meiji Seika, Tokyo, Japan). Human umbilical vein endothelial cells (HUVEC) were maintained in DMEM (pH 7.4, Sigma) supplemented with 10% fetal bovine serum and 100 μg/ml kanamycin sulfate. The mouse oral epithelium cell line foec-6 was kindly provided by Dr. Yasuhiro Tomo-oka (Tokyo University of Science, Chiba, Japan). Cells were cultured in a humidified atmosphere of 5% CO2 in air.
Dorsal air sac assay
The dorsal air sac assay was performed according to the procedure of Oikawa et al. [34]. Briefly, both sides of a Millipore ring (Millipore, Billerica, MA, USA) were covered with Millipore filters of 0.45-μm pore size using MF cement. Millipore chambers containing PBS, recombinant human vascular endothelial growth factor (rhVEGF) (10 ng/ml), and rhVEGF with 10 μM ZOL were implanted into the preformed air sac in the dorsum of anesthetized female BALB/cA mice (Charles River, Yokohama, Japan). On day 5, the implanted chambers were removed from mice, and newly formed blood vessels were counted under a light microscope in each group. The data were expressed as the number of vessels/mouse.
Cell proliferation assay
The cell proliferation assay was performed using cell proliferation reagent WST-1 (Roche), as described previously [35]. Briefly, bone marrow endothelial cells (BMECs) and ECV-304 cells were plated into 96-well plates (2000/well) and incubated at 37°C in a 5% CO2 atmosphere with or without ZOL and ETI. On day 3, 10 μl cell proliferation reagent WST-1 was added to each well and incubated for 1 h. The cell number was determined by absorption at 450 nm using a microplate reader (Bio-Rad).
Three-dimensional culture of BMECs in collagen gel
Three-dimensional culture of BMECs was performed according to the procedure of Yang and Nandi [36]. Briefly, a mixture of collagen (Cellmatrix type IA; Nitta Gelatin, Tokyo, Japan) and fivefold-condensed DMEM containing ZOL (0.1, 1, or 10 μM) was poured into a 12-well plate and incubated until collagen had gelled, forming a base. Then, 1 ml of the collagen mixture including BMECs (5000 cells/ml) was added to the base as the second gel. These gels were overlaid with DMEM containing 10% FBS. The cells were cultured for 2 weeks with ZOL (0.1, 1, or 10 μM), and the overlaid DMEM was changed every 3 days. BMECs cultured in collagen gel were fixed with 10% formalin in PBS and photographed at the same scale under a light transmission inverted photomicroscope.
Matrigel network formation assay
The effect of bisphosphonates on tubule formation was assessed using the matrigel network formation assay described by Kubota et al. [37]. Briefly, 100 μl Matrigel (Becton–Dickinson, Sparks, MD, USA) was plated into 96-well plates and incubated at 37°C. HUVECs were cultured for 48 h with or without ZOL and ETI, and then were plated on top of the Matrigel. After 20 h, the total length of tubule formation was measured under an inverted microscope.
Caspase assay
The caspase-3/7 activity in cell extracts and culture supernatants was determined using Caspase-Glo 3/7 Assay (Promega) according to the manufacturer’s protocol. Briefly, cells were cultured in 96-well plates and treated with bisphosphonates for 24 h. Cell lysis and substrate addition were performed using Caspase-3/7 Glo reagents. The luminescence emitted by each sample was measured with a luminometer.
In vitro wound healing assay
NIH3T3 cells and foe-6 cells were plated in 12-well plates and cultured in DMEM containing 10% fetal calf serum (FCS) until the cells became 80% confluent. The monolayer was wounded by scraping a line across the well using a sterile 1-ml blue pipette tip, which then was rinsed several times with medium to remove dislodged cells. Cells were then cultured for 15 h with or without ZOL, and the wound monolayer was photographed. Migratory activity of the cells was determined by measuring the width of the monolayer wounds, and data were quantified as the percent of control.
Hydroxyapatite adhesion assay
The adhesion of oral bacteria to hydroxyapatite was determined by a saliva-coated hydroxyapatite (SHA) adhesion assay, as described previously [38]. The SHA suspension was added to an individual cup of a vacuum filtration device containing a mixed cellulose-ester membrane (0.45 μM pore size; Toyo Roshi Kaishya, Osaka, Japan), and vacuum was applied. The membrane was washed three times in buffered KCl to remove the loosely bound SHA. Then, PBS alone or 100 μM ZOL in PBS was added to the cup and incubated at room temperature for 30 min. Then, radiolabeled Streptococcus (S.) mutans bacteria were added to the cup and incubated at room temperature for 30 min. Unbound cells were decanted, and the SHA-binding membrane was washed four times with buffered KCl. The radioactivity of the SHA-binding membrane was measured using a liquid scintillation spectrometer.
Colony formation assay for oral bacteria
Dental plaque samples were obtained from healthy subjects and resuspended in PBS using ultrasonic applications. Resuspended oral plaque bacteria were incubated for 24 h at 37°C with ZOL (10 nM–10 mM). These samples were then spread on a Todd Hewitt broth containing 0.3% yeast extract (THY) agarose plate, and the number of white colonies was counted after 24 h of incubation.
Statistical analysis
All data were expressed as the mean ± SD. The data were analyzed by one-way analysis of variance (ANOVA) followed by Fisher’s protected least squares difference (PLSD) post hoc test (StatView; SAS Institute, Cary, NC, USA) for determination of differences between groups. Student’s t test or Welch’s t test was conducted when the two groups were compared. P values < 0.05 were considered significant.
Results
ZOL delayed wound healing of the tooth extraction socket by inhibiting osteogenesis and angiogenesis
To examine the effect of ZOL on wound healing of the tooth extraction socket, ZOL was subcutaneously injected daily for 7 days before extraction of the right first molar (Fig. 1). New bone formation in the tooth extraction socket was clearly suppressed in mice treated with ZOL (Fig. 2a). Histomorphometric measurements revealed that ZOL significantly decreased the area of new bone (Fig. 2b). Because angiogenesis is the essential step in wound healing, ZOL possibly inhibited microvessel development during tooth socket healing. Using immunohistochemical examination, we observed that the formation of CD31-positive (CD31(+)) blood vessels was significantly reduced in mice treated with ZOL (Fig. 2c). These data suggest that ZOL delayed the tooth socket healing process by inhibiting new bone formation and angiogenesis.
The tooth extraction protocol. a Photograph of tooth extraction in a C57BL/6 mouse. The upper right first molars (dotted circular line) were extracted under anesthesia using an iridectome. b Experimental protocol of zoledronic acid (ZOL) administration. ZOL (5 μg/mouse/day) was injected subcutaneously from 7 days before the tooth extraction to 4 days after the extraction. All mice were killed at day 5, and organs were harvested and processed for histological examination
Histological analysis of the tooth extraction socket in mice treated with phosphate-buffered saline (PBS) and zoledronic acid (ZOL). a Representative histological view of tooth extraction socket in mice treated with PBS and ZOL. PBS-treated mice (left) showed new active bone formation. In contrast, ZOL-treated mice (right) showed decreased new bone formation. Hematoxylin and eosin (H&E) stain: ×100. b Quantitative analysis of new bone formation in the tooth extraction socket. The new bone formation area was determined as described in “Materials and methods”. Quantitative data are shown as bone area/total area (%). Values are the mean ± SD (n = 10/group). *P < 0.05 versus PBS. c Effects of ZOL on angiogenesis in the tooth extraction socket. The number of CD31(+) vessels was counted in the tooth extraction socket. Values are the mean ± SD (n = 10/group). *P < 0.05 versus PBS
Antiangiogenic effect of ZOL in vivo and in vitro
To further evaluate the antiangiogenic effect of ZOL, we performed a dorsal air sac assay, which allowed us to monitor angiogenesis in vivo. Treatment with rhVEGF dramatically induced new vessel formation, which was characterized by a red zigzag line (Fig. 3a, b). ZOL reduced the number of newly formed blood vessels induced by rhVEGF (Fig. 3c, d). We next examined the effect of ZOL on the proliferation of endothelial cells in culture. Treatment with ZOL inhibited the proliferation of bone marrow endothelial cells (BMECs) and human endothelial-like cells (ECV304) in monolayers and collagen gel cultures in a dose-dependent manner, respectively (Fig. 4). Moreover, the matrigel network formation assay revealed that ZOL suppressed tubule formation by HUVECs (Fig. 5). Taken together, these data indicate that ZOL suppressed angiogenesis by inhibiting endothelial cell proliferation and migration.
Inhibitory effects of zoledronic acid on angiogenesis in vivo assessed by the dorsal air sac assay. a–c Representative view of angiogenesis (dotted ovals). Millipore chambers containing PBS, human recombinant vascular endothelial growth factor (rhVEGF) (VEGF, 10 ng/ml), and rhVEGF with 10 μM zoledronic acid (VEGF + ZOL) were implanted into mice and photographed at day 5. ZOL inhibited new vessel formation induced by VEGF. d Quantitative analysis of new vessel formation. Data are expressed as the number of vessels/mouse. Values are the mean ± SD (n = 5/group). *P < 0.01 versus VEGF
Effects of zoledronic acid on endothelial cell proliferation in monolayer culture (a) and three-dimensional culture (b). ECV304 cells (a) and bone marrow endothelial cells (BMEC) (b) were cultured for 72 h with the indicated concentrations of zoledronic acid (ZOL). Viable cells were measured with the WST-1 assay as described in “Materials and methods”. Values are the mean ± SD (n = 8/group). *P < 0.05 versus control (Cont). c Representative images of BMECs in the three-dimensional culture system. BMECs were cultured in collagen gels for 14 days with the indicated concentrations of ZOL. ZOL inhibited the proliferation of BMECs with a lower concentration (1 μM) than in monolayer culture. O.D. optical density
Effects of zoledronic acid on tubule formation by HUVECs. a Representative micrographs of HUVECs grown in the absence (control, Cont) or presence of zoledronic acid (ZOL) (10 μM). Tubule formation was decreased in HUVECs treated with ZOL. b Tubule formation was quantified by estimating the total length of tubule formation (mm) under an inverted microscope. Values are the mean ± SD (n = 6/group). *P < 0.01 versus control (Cont)
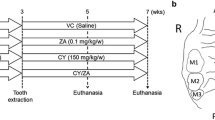
Non-nitrogen-containing BPs had no effect on tooth socket healing and angiogenesis
Several clinical studies have reported that the incidence of BRONJ in patients receiving non-nitrogen-containing bisphosphonates such as etidronate (ETI) is significantly less than in patients receiving ZOL. Therefore, we next examined whether ETI affected wound healing of the tooth extraction socket or angiogenesis. We observed no marked histological differences in wound healing of the tooth extraction sockets between PBS- and ETI-treated groups (Fig. 6a). Histomorphometrical analysis also showed that ETI had no effect on new bone formation or angiogenesis in the tooth extraction socket (Fig. 6b, c). Moreover, ETI did not suppress the proliferation of BMECs (Fig. 6d) or tubule formation by HUVECs (Fig. 6e).
Effect of etidronate (ETI) on wound healing of the tooth extraction socket and angiogenesis. a Representative histological view of the tooth extraction socket in mice treated with PBS and ETI. ETI had no effect on wound healing of the tooth extraction socket. H&E staining: ×100. b Effects of ETI on new bone formation in the tooth extraction socket. The new bone formation area was determined as described in “Materials and methods”. Quantitative data are shown as bone area/total area (%). Values are the mean ± SD (n = 10/group). *P < 0.05 versus PBS. c Effects of ETI on angiogenesis in the tooth extraction socket. The number of CD31(+) vessels was counted in the tooth extraction socket. Values are the mean ± SD (n = 10/group). *P < 0.05 versus PBS. d BMECs were cultured for 72 h with the indicated concentrations of etidronate (ETI). Viable cells were measured using the WST-1 assay as described in “Materials and methods”. Values are the mean ± SD (n = 8/group). Cont control, OD optical density. e Representative micrographs of HUVECs grown in the absence (PBS) or presence of ETI (10 μM). ETI had no effect on tubule formation by HUVECs
ZOL increased the caspase activity in endothelial cells and oral epithelial cells
ZOL strongly inhibit bone resorption by inducing apoptosis in osteoclasts. These data raise the possibility that ZOL delayed the wound healing of tooth extraction socket through inducing apoptosis of osteoblasts, endothelial cells, and oral epithelial cells. Therefore, we next examined the caspase activity in response to ZOL and ETI. Neither ZOL nor ETI had any effect on caspase3/7 activity in osteoblastic MC3T3-E1 cells (Fig. 7). Interestingly, we found that ZOL increased caspase 3/7 activity in HUVECs and oral epithelial cells (foec-6), whereas ETI had no effect on casapase 3/7 activity (Fig. 7). These data suggest that the apoptosis triggered by ZOL in endothelial cells and oral epithelial cells would contribute to the delay of wound healing in the tooth extraction socket.
Effect of ZOL and ETI on caspase-3/7 activity in osteoblastic cells (MC3T3-E1), oral epithelial cells (foec-6), and endothelial cells (HUVECs). Cells were treated with the indicated concentrations of ZOL and ETI for 24 h, and Caspase-3/7 activity was determined as described in “Materials and methods”. n, nM; μ, μM. Untreated cells and cycloheximide (100 μg/ml)-treated cells were used as negative and positive controls. The caspase-3/7 activity is represented as the percentage of that of control. Values are the mean ± SD (n = 4/group). *P < 0.05 versus Control
Inhibition of migratory activity of oral epithelial cells by ZOL
A detailed analysis revealed that there was a delay in closure of the tooth extraction socket in ZOL-treated mice, whereas complete closure of the surgical extraction site was observed in all control mice. These observations suggest that ZOL inhibits migration of oral epithelial cells from the socket margin, resulting in an open socket. In support of this notion, the wound healing assay demonstrated that ZOL inhibited the migration of oral epithelial cells (foec-6) but not mouse NIH-3T3 fibroblasts (Fig. 8a, b).
Effect of zoledronic acid (ZOL) on the migratory activity of fibroblasts (NIH3T3) and oral epithelial cells (foec-6) in a wound healing assay. a Representative phase-contrast images of the wounded cell monolayers of NIH3T3 cells and foec-6 cells. NIH3T3 cells and foec-6 cells were treated with zoledronic acid (ZOL) at the indicated concentrations, and phase-contrast images were captured at 0 or 15 h. Double-headed arrows indicate the width of the wound. b Quantitative analysis of the migratory activity. Data are expressed as the percentage of wound closure quantified by measuring the average width of the wounds and represent the means ± SD (n = 4). *Significantly different from control (Cont) at 15 h (P < 0.01). n, nM; μ, μM
Effect of ZOL on oral bacteria adhesion and growth
Because occurrence of BRONJ is restricted to the maxilla and mandible, bisphosphonates may influence the biological behavior of oral bacteria that were observed in BRONJ. The hydroxyapatite adhesion assay demonstrated that ZOL increased the adhesive activity of S. mutans on hydroxyapatite (Fig. 9a). Moreover, ZOL increased the growth of oral plaque bacteria (Fig. 9b). These data indicate that ZOL increases oral bacterial activity, triggering oral bacterial infection.
a Effects of zoledronic acid on the adhesion of Streptococcus (S.) mutans to hydroxyapatite. [3H]-Labeled S. mutans were reacted with PBS- or ZOL-treated hydroxyapatite for 30 min, and adherent S. mutans were quantitated by measuring radioactivity. Values are the mean ± SD (n = 4/group). *P < 0.05 versus PBS. b Effects of zoledronic acid on the proliferation of oral plaque bacteria. Resuspended oral plaque bacteria were incubated for 24 h at 37°C with the indicated concentrations of ZOL and then spread on Todd Hewitt broth containing 0.3% yeast extract (THY) agarose plates. The number of white colonies was counted after 24 h incubation. Values are the mean ± SD (n = 5/group). *P < 0.05 versus control (Cont). n, nM; μ, μM
Discussion
In this study, we first examined the effects of ZOL on tooth socket healing using an animal model of tooth extraction to gain insights into the pathogenesis of BRONJ. ZOL is reported to be associated with the highest incidence of BRONJ. Histological and immunohistochemical examinations showed that ZOL markedly delayed wound healing of the tooth extraction socket with an inhibition of new bone formation. Moreover, we also found that ZOL reduced the number of blood vessels in the extraction socket and the proliferation and migration of endothelial cells in culture, suggesting that ZOL inhibits angiogenesis critical to the healing of the tooth extraction socket. Consistent with this notion, recent studies have reported that ZOL is a potent inhibitor of angiogenesis [39–41]. Of note, ZOL also decreased oral epithelial cell migration, suggesting that epithelial closure of the tooth extraction socket is disturbed by ZOL. After tooth extraction, ZOL deposited in the alveolar bone may be released into the tooth socket cavity and affect oral epithelial cells that migrate from the socket edge to cover the extraction wound [42]. Coverage by oral epithelial cells is critical not only to successful wound healing but also for protection of the socket from oral bacterial infection. In addition, the delay in wound healing of tooth socket likely causes prolonged exposure of alveolar bone to oral bacteria. These results collectively suggest that ZOL delays the wound healing of the tooth extraction socket.
Although ZOL significantly delayed wound healing of the tooth extraction socket in our experimental model, these mice did not manifest representative symptoms of BRONJ such as necrotic bone exposure with accumulated oral bacterial colonies as seen in patients. Thus, it is still unclear whether ZOL is directly involved in the pathogenesis of BRONJ. In preliminary experiments, we treated mice with ZOL combined with doxorubicin (100 μg/mouse, i.p.) and/or dexamethasone (400 μg/mouse, i.p.) in clinically relevant settings. In contrast to our expectation, however, even combined administration of these agents did not induce any discernible symptoms of BRONJ (data not shown).
One possible explanation for the failure of inducing distinctive BRONJ in our study could be the absence of bacteria in the oral cavity of mice used here. There were probably very few bacteria in the oral cavity of these mice because they were maintained in germ-free conditions. Our in vitro data showed that ZOL promoted proliferation of oral bacteria from healthy individuals and attachment of S. mutans to hydroxyapatite, suggesting that ZOL can change the oral environment to conditions that facilitate the induction of BRONJ so long as bacteria are present. Alternatively, it is also possible that age, periodontal diseases, impaired immunosurveillance, and underlying malignant diseases or osteoporosis may have contributed to the induction of BRONJ in patients. Allen and Burr reported that treatment with alendronate in beagle dogs caused matrix necrosis in the mandible [43]. More recently, Sonis et al. also showed that combined administration of ZOL and dexamethasone resulted in ONJ in rats with no inflammation and oral bacterial infection [44]. These models should be useful for the study of the mechanism of BRONJ and the development of appropriate therapeutic interventions for BRONJ. Unfortunately, however, these animal models do not represent BRONJ seen in patients in terms of the absence of bacterial colonies. A critical role of oral bacteria in the pathogenesis of BRONJ is supported by the accumulating clinical observations that elimination of dental plaque that substantially consists of oral bacteria or administration of antibiotics before dental surgery significantly reduces the frequency of BRONJ in patients [45–47]. Further modifications of the experimental protocol and techniques may be necessary for the development of representative BRONJ in rodents.
In the present study, we showed that ZOL inhibited the proliferation of endothelial cells and migratory activity of oral epithelial cells. Interestingly, ZOL has also been reported to show antitumor activity by inhibiting cancer cell proliferation [48, 49]. One of the possible mechanisms by which ZOL exhibited antiproliferative effects is the disruption of the mavalonate pathway. ZOL inhibits the formation of farnesyl diphosphate (FPP) and geranylgeranyl diphosphate (GGPP) by suppressing FPP synthase and GGPP synthase [18]. As FFP and GGPP are important for the posttranslational prenylation of small signaling GTPase, the disruption of mevalonate pathway by ZOL is likely to account for the antiproliferative activity in endothelial cells. However, further studies are needed to explain how ZOL inhibited oral epithelial cell migration.
In this context, it is notable that ZOL increased bacterial adhesion to hydroxyapatite and the proliferation of oral bacteria. These data suggest that ZOL may cause increased bacterial biofilm formation on tooth surfaces, which could be a major cause of BRONJ. Previous studies reported that nitrogen-containing bisphosphonates (alendronate, pamidronate, and risedronate) inhibited Trypanosoma cruzi farnesyl pyrophosphate synthase [50]. Similarly, it was also shown that nitrogen-containing bisphosphonates at low micromolar concentrations reduced the growth of several types of bacteria [51]. In contrast to our results, these reports suggest that nitrogen-containing bisphosphonates are inhibitory but not stimulatory for oral bacteria. The reasons for the discrepancies between previous and our results are unknown. ZOL may have actions distinct from those of other nitrogen-containing bisphosphonates. Differences in bisphosphonate concentrations or oral bacteria examined may be also attributable. Whatever the actions are, the results of our study suggest that bisphosphonates modulate oral bacterial behaviors.
ETI, a bisphosphonate without a nitrogen atom, had no effects on wound healing of the tooth extraction socket and failed to show antiangiogenic effects in our study. These findings may be relevant to clinical reports that BRONJ was rarely seen in patients receiving ETI. The reasons for the rare occurrence of BRONJ in ETI-treated patients are unknown at the moment but might be partly lack of antiangiogenic action. Moreover, differences in affinity to bone minerals, uptake into cells, pharmacological potency, drug metabolism, and mechanism of actions in causing apoptosis [18, 52] may be involved. Further studies are needed to dissect the contrasting effects between ZOL and ETI in the pathogenesis of BRONJ.
In conclusion, our results suggest that treatment with ZOL delayed wound healing of the tooth extraction socket by inhibiting osteogenesis and angiogenesis. It is also suggested that ZOL inhibits epithelial closure of the tooth extraction socket by inhibiting oral epithelial cell proliferation and motility. Moreover, ZOL may increase the opportunity of oral bacterial infection by promoting proliferation and attachment to tooth surfaces. However, the role of ZOL in the pathogenesis of BRONJ remains still unclear and to be elucidated because we failed to cause representative BRONJ in this study.
References
Rogers MJ, Watts DJ, Russell RG (1997) Overview of bisphosphonates. Cancer (Phila) 80:1652–1660
Licata AA (2005) Discovery, clinical development, and therapeutic uses of bisphosphonates. Ann Pharmacother 39:668–677
Michaelson MD, Smith MR (2005) Bisphosphonates for treatment and prevention of bone metastases. J Clin Oncol 23:8219–8224
Delmas PD (2005) The use of bisphosphonates in the treatment of osteoporosis. Curr Opin Rheumatol 17:462–466
DiCaprio MR, Enneking WF (2005) Fibrous dysplasia. Pathophysiology, evaluation, and treatment. J Bone Joint Surg [Am] 87:1848–1864
Reid IR, Miller P, Lyles K, Fraser W, Brown JP, Saidi Y, Mesenbrink P, Su G, Pak J, Zelenakas K, Luchi M, Richardson P, Hosking D (2005) Comparison of a single infusion of zoledronic acid with risedronate for Paget’s disease. N Engl J Med 353:898–908
Hortobagyi GN, Theriault RL, Porter L, Blayney D, Lipton A, Sinoff C, Wheeler H, Simeone JF, Seaman J, Knight RD (1996) Efficacy of pamidronate in reducing skeletal complications in patients with breast cancer and lytic bone metastases. Protocol 19. Aredia Breast Cancer Study Group. N Engl J Med 335:1785–1791
Ashcroft AJ, Davies FE, Morgan GJ (2003) Aetiology of bone disease and the role of bisphosphonates in multiple myeloma. Lancet Oncol 4:284–292
Berenson JR, Hillner BE, Kyle RA, Anderson K, Lipton A, Yee GC, Biermann JS (2002) American Society of Clinical Oncology clinical practice guidelines: the role of bisphosphonates in multiple myeloma. J Clin Oncol 20:3719–3736
Coleman RE (2002) Future directions in the treatment and prevention of bone metastases. Am J Clin Oncol 25:S32–S38
Djulbegovic B, Wheatley K, Ross J, Clark O, Bos G, Goldschmidt H, Cremer F, Alsina M, Glasmacher A (2001) Bisphosphonates in multiple myeloma. Cochrane Database Syst Rev 4:CD003188
Ferretti G, Fabi A, Carlini P, Papaldo P, Cordiali Fei P, Di Cosimo S, Salesi N, Giannarelli D, Alimonti A, Di Cocco B, D’Agosto G, Bordignon V, Trento E, Cognetti F (2005) Zoledronic-acid-induced circulating level modifications of angiogenic factors, metalloproteinases and proinflammatory cytokines in metastatic breast cancer patients. Oncology 69:35–43
Hillner BE, Ingle JN, Chlebowski RT, Gralow J, Yee GC, Janjan NA, Cauley JA, Blumenstein BA, Albain KS, Lipton A, Brown S (2003) American Society of Clinical Oncology 2003 update on the role of bisphosphonates and bone health issues in women with breast cancer. J Clin Oncol 21:4042–4057
Hillner BE, Weeks JC, Desch CE, Smith TJ (2000) Pamidronate in prevention of bone complications in metastatic breast cancer: a cost-effectiveness analysis. J Clin Oncol 18:72–79
Osanai T, Tsuchiya T, Ogino T, Nakahara K (2006) Long-term prevention of skeletal complications by pamidronate in a patient with bone metastasis from endometrial carcinoma: a case report. Gynecol Oncol 100:195–197
Smith MR (2005) Zoledronic acid to prevent skeletal complications in cancer: corroborating the evidence. Cancer Treat Rev 31(Suppl 3):19–25
Rogers MJ, Gordon S, Benford HL, Coxon FP, Luckman SP, Monkkonen J, Frith JC (2000) Cellular and molecular mechanisms of action of bisphosphonates. Cancer (Phila) 88:2961–2978
Luckman SP, Hughes DE, Coxon FP, Graham R, Russell G, Rogers MJ (1998) Nitrogen-containing bisphosphonates inhibit the mevalonate pathway and prevent post-translational prenylation of GTP-binding proteins, including Ras. J Bone Miner Res 13:581–589
Russell RG, Rogers MJ (1999) Bisphosphonates: from the laboratory to the clinic and back again. Bone (NY) 25:97–106
Marx RE (2003) Pamidronate (Aredia) and zoledronate (Zometa) induced avascular necrosis of the jaws: a growing epidemic. J Oral Maxillofac Surg 61:1115–1117
Ruggiero SL, Mehrotra B, Rosenberg TJ, Engroff SL (2004) Osteonecrosis of the jaws associated with the use of bisphosphonates: a review of 63 cases. J Oral Maxillofac Surg 62:527–534
Pires FR, Miranda A, Cardoso ES, Cardoso AS, Fregnani ER, Pereira CM, Correa ME, Almeida JP, Alves Fde A, Lopes MA, de Almeida OP (2005) Oral avascular bone necrosis associated with chemotherapy and biphosphonate therapy. Oral Dis 11:365–369
Assael LA (2004) New foundations in understanding osteonecrosis of the jaws. J Oral Maxillofac Surg 62:125–126
Hellstein JW, Marek CL (2004) Bis-phossy jaw, phossy jaw, and the 21st century: bisphosphonate-associated complications of the jaws. J Oral Maxillofac Surg 62:1563–1565
Jimenez-Soriano Y, Bagan JV (2005) Bisphosphonates, as a new cause of drug-induced jaw osteonecrosis: an update. Med Oral Patol Oral Cir Bucal 10(Suppl 2):E88–E91
Melo MD, Obeid G (2005) Osteonecrosis of the jaws in patients with a history of receiving bisphosphonate therapy: strategies for prevention and early recognition. J Am Dent Assoc 136:1675–1681
Olson KB, Hellie CM, Pienta KJ (2005) Osteonecrosis of jaw in patient with hormone-refractory prostate cancer treated with zoledronic acid. Urology 66:658
Vannucchi AM, Ficarra G, Antonioli E, Bosi A (2005) Osteonecrosis of the jaw associated with zoledronate therapy in a patient with multiple myeloma. Br J Haematol 128:738
Ruggiero SL, Dodson TB, Assael LA, Landesberg R, Marx RE, Mehrotra B (2009) American Association of Oral and Maxillofacial Surgeons position paper on bisphosphonate-related osteonecrosis of the jaws: 2009 update. J Oral Maxillofac Surg 67:2–12
Fournier P, Boissier S, Filleur S, Guglielmi J, Cabon F, Colombel M, Clezardin P (2002) Bisphosphonates inhibit angiogenesis in vitro and testosterone-stimulated vascular regrowth in the ventral prostate in castrated rats. Cancer Res 62:6538–6544
Wood J, Bonjean K, Ruetz S, Bellahcene A, Devy L, Foidart JM, Castronovo V, Green JR (2002) Novel antiangiogenic effects of the bisphosphonate compound zoledronic acid. J Pharmacol Exp Ther 302:1055–1061
Hellstein JW, Marek CL (2005) Bisphosphonate osteochemonecrosis (bis-phossy jaw): is this phossy jaw of the 21st century? J Oral Maxillofac Surg 63:682–689
Sedghizadeh PP, Kumar SK, Gorur A, Schaudinn C, Shuler CF, Costerton JW (2008) Identification of microbial biofilms in osteonecrosis of the jaws secondary to bisphosphonate therapy. J Oral Maxillofac Surg 66:767–775
Oikawa T, Sasaki M, Inose M, Shimamura M, Kuboki H, Hirano S, Kumagai H, Ishizuka M, Takeuchi T (1997) Effects of cytogenin, a novel microbial product, on embryonic and tumor cell-induced angiogenic responses in vivo. Anticancer Res 17:1881–1886
Hata K, Nishimura R, Muramatsu S, Matsuda A, Matsubara T, Amano K, Ikeda F, Harley VR, Yoneda T (2008) Paraspeckle protein p54nrb links Sox9-mediated transcription with RNA processing during chondrogenesis in mice. J Clin Invest 118:3098–3108
Yang J, Nandi S (1983) Growth of cultured cells using collagen as substrate. Int Rev Cytol 81:249–286
Kubota Y, Kleinman HK, Martin GR, Lawley TJ (1988) Role of laminin and basement membrane in the morphological differentiation of human endothelial cells into capillary-like structures. J Cell Biol 107:1589–1598
Matsumoto M, Tsuji M, Sasaki H, Fujita K, Nomura R, Nakano K, Shintani S, Ooshima T (2005) Cariogenicity of the probiotic bacterium Lactobacillus salivarius in rats. Caries Res 39:479–483
Muller S, Migianu E, Lecouvey M, Kraemer M, Oudar O (2005) Alendronate inhibits proliferation and invasion of human epidermoid carcinoma cells in vitro. Anticancer Res 25:2655–2660
Ribatti D, Nico B, Mangieri D, Maruotti N, Longo V, Vacca A, Cantatore FP (2007) Neridronate inhibits angiogenesis in vitro and in vivo. Clin Rheumatol 26:1094–1098
Yamagishi S, Abe R, Inagaki Y, Nakamura K, Sugawara H, Inokuma D, Nakamura H, Shimizu T, Takeuchi M, Yoshimura A, Bucala R, Shimizu H, Imaizumi T (2004) Minodronate, a newly developed nitrogen-containing bisphosphonate, suppresses melanoma growth and improves survival in nude mice by blocking vascular endothelial growth factor signaling. Am J Pathol 165:1865–1874
Reid IR (2009) Osteonecrosis of the jaw: who gets it, and why? Bone (NY) 44:4–10
Allen MR, Burr DB (2008) Mandible matrix necrosis in beagle dogs after 3 years of daily oral bisphosphonate treatment. J Oral Maxillofac Surg 66:987–994
Sonis ST, Watkins BA, Lyng GD, Lerman MA, Anderson KC (2009) Bony changes in the jaws of rats treated with zoledronic acid and dexamethasone before dental extractions mimic bisphosphonate-related osteonecrosis in cancer patients. Oral Oncol 45:164–172
Dimopoulos MA, Kastritis E, Bamia C, Melakopoulos I, Gika D, Roussou M, Migkou M, Eleftherakis-Papaiakovou E, Christoulas D, Terpos E, Bamias A (2009) Reduction of osteonecrosis of the jaw (ONJ) after implementation of preventive measures in patients with multiple myeloma treated with zoledronic acid. Ann Oncol 20:117–120
Montefusco V, Gay F, Spina F, Miceli R, Maniezzo M, Teresa Ambrosini M, Farina L, Piva S, Palumbo A, Boccadoro M, Corradini P (2008) Antibiotic prophylaxis before dental procedures may reduce the incidence of osteonecrosis of the jaw in patients with multiple myeloma treated with bisphosphonates. Leuk Lymphoma 49:2156–2162
Ripamonti CI, Maniezzo M, Campa T, Fagnoni E, Brunelli C, Saibene G, Bareggi C, Ascani L, Cislaghi E (2009) Decreased occurrence of osteonecrosis of the jaw after implementation of dental preventive measures in solid tumour patients with bone metastases treated with bisphosphonates. The experience of the National Cancer Institute of Milan. Ann Oncol 20:137–145
Clezardin P (2005) Anti-tumour activity of zoledronic acid. Cancer Treat Rev 31(Suppl 3):1–8
Winter MC, Holen I, Coleman RE (2008) Exploring the antitumour activity of bisphosphonates in early breast cancer. Cancer Treat Rev 34:453–475
Montalvetti A, Bailey BN, Martin MB, Severin GW, Oldfield E, Docampo R (2001) Bisphosphonates are potent inhibitors of Trypanosoma cruzi farnesyl pyrophosphate synthase. J Biol Chem 276:33930–33937
Martin MB, Grimley JS, Lewis JC, Heath HT III, Bailey BN, Kendrick H, Yardley V, Caldera A, Lira R, Urbina JA, Moreno SN, Docampo R, Croft SL, Oldfield E (2001) Bisphosphonates inhibit the growth of Trypanosoma brucei, Trypanosoma cruzi, Leishmania donovani, Toxoplasma gondii, and Plasmodium falciparum: a potential route to chemotherapy. J Med Chem 44:909–916
Frith JC, Monkkonen J, Blackburn GM, Russell RG, Rogers MJ (1997) Clodronate and liposome-encapsulated clodronate are metabolized to a toxic ATP analog, adenosine 5′-(beta, gamma-dichloromethylene) triphosphate, by mammalian cells in vitro. J Bone Miner Res 12:1358–1367
Acknowledgments
We are grateful to Dr. Yoshinosuke Hamada and Dr. Nariaki Matsuura (Department of Functional Diagnostic Science, Osaka University Graduate School of Medicine) for technical support and helpful discussion. This work was supported in part by Ministry of Education, Science, Sports and Culture Grants-in-Aid for Scientific Research A (TY) and The 21st Century COE Program (TY).
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Kobayashi, Y., Hiraga, T., Ueda, A. et al. Zoledronic acid delays wound healing of the tooth extraction socket, inhibits oral epithelial cell migration, and promotes proliferation and adhesion to hydroxyapatite of oral bacteria, without causing osteonecrosis of the jaw, in mice. J Bone Miner Metab 28, 165–175 (2010). https://doi.org/10.1007/s00774-009-0128-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-009-0128-9