Abstract
The aim of this study is to meta-analytically assess the efficacy and safety of adjunctive raloxifene for postmenopausal women with schizophrenia. Six studies with 440 patients, including 225 (51.14%) patients on raloxifene and 215 (48.86%) on placebo who completed 13.71 ± 5.09 weeks of treatment, were included in this study. Meta-analysis of Positive and Negative Syndrome Scale total scores and positive, negative, and general symptom scores [standard mean difference (SMD) −0.22 to −0.55, 95% confidence interval (CI) −1.01 to −0.02, p = 0.04–0.01; I 2 = 74–79%] revealed an advantage of adjunctive raloxifene treatment over placebo treatment. There was no significant difference regarding discontinuation rate [risk ratio (RR) = 1.38, p = 0.51] and adverse drug reactions (RR = 1.27, p = 0.57) between the two groups. This meta-analysis showed that adjunctive raloxifene appears to be efficacious and safe for postmenopausal women with schizophrenia. Moreover, raloxifene may be efficacious for patients with less severe symptoms. Future studies with a large sample size are needed to confirm these findings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Schizophrenia is a severe psychiatric disorder with complex clinical manifestations that impairs function across multiple domains (Cariagamartinez et al. 2016). A body of evidence exists to support the idea that lowered estrogen levels are a predictor of schizophrenia (Mortimer 2007). Specifically, studies examining schizophrenia in men and women have produced results leading to the hypothesis that estrogens play an important role in the pathophysiology of schizophrenia (Kumari 2011; Talonen et al. 2017; Taylor and Langdon 2006). Interestingly, it has been shown that several antipsychotic drugs increase serum levels of prolactin which generates a negative feedback cycle lowering estrogen levels (Peuskens et al. 2014). Yet, in women, psychotic symptoms are often exacerbated when the levels of estradiol are decreased (Riecher-Rössler and Häfner 1993), and both human and animal studies suggest estrogen provokes psychoprotective effects in schizophrenia (Kulkarni et al. 2012).
Estrogen can affect neural circuits and neurochemistry implicated in the pathogenesis of schizophrenia (Bethea et al. 2000; Fink et al. 1996). Animal research has shown that estradiol enhances serotonin concentrations, modulates effects on the dopaminergic system in the brain, reduces inflammation, and stimulates metabotropic glutamate receptor signaling (Di 1994; Meitzen and Mermelstein 2011; Sánchez et al. 2013; Sribnick et al. 2005). Human studies have demonstrated a role for estradiol in modulating stress circuitry activity and dysregulating hormone–brain pathways in women with depression (Holsen et al. 2010). Indeed, levels of estrogen in schizophrenic women are lower than in healthy women, and the onset of illness or relapses coincide more frequently during the menstrual cycle when estrogen levels are low (Huber et al. 2001; Riecher-Rössler and Kulkarni 2010).
The use of estradiol as adjuvant treatment in schizophrenia appears promising, as estradiol therapy can reduce psychotic symptoms in women with treatment-resistant schizophrenia (Kulkarni et al. 2014). However, the use of estrogen in long-term treatment has been limited by potentially adverse effects on breast tissue and the endometrium (Corson 2009; Kulkarni et al. 2012). This has led to research regarding the use of selective estrogen receptor modulators (SERM) such as raloxifene to improve psychotic symptoms without adverse side effects. Raloxifene is a first-generation SERM with mixed agonist and antagonist activity (Shang and Brown 2002). Raloxifene has agonist actions on alpha-amino-propionic-acid, N-methyl d-aspartate, and serotonin receptors in basal ganglia, the frontal cortex, and striatum all of which are commonly impaired in schizophrenia (Littleton-Kearney et al. 2002). Raloxifene also acts as an estrogen antagonist in breast and uterine tissue (Moen and Keating 2008). There is also evidence to indicate that raloxifene could be useful for treating mood disorder and psychotic symptoms in postmenopausal women (Jarkova et al. 2002; Wong et al. 2003).
However, the results of randomized controlled trials (RCTs) regarding the efficacy and safety of raloxifene for postmenopausal women with schizophrenia have been mixed. Thus, we conducted this meta-analysis of RCT in order to assess the efficacy and safety of adjunctive raloxifene.
Methods
This work applied the Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) guidelines without prepublication of the review protocol (Moher et al. 2014).
Search strategy and selection criteria
Electronic searches were carried out to retrieve studies without language restriction using the following databases: PubMed, Embase, Cochrane Library, PsycINFO, CNKI, and WanFang Data; from database inceptions to August 1th, 2017. We used the following keywords: raloxifene; antipsychotics; schizophrenia; postmenopause; and RCTs (and the Chinese equivalents) were in the searches. A set of search terms were [(Raloxifene OR Raloxifene hydrochloride) AND Postmenopausal women) and (Schizophrenia OR Schizoaffective Disorder OR Schizophreniform Disorder OR Dementia Praecox) AND (random* OR RCT OR control* OR compare* OR placebo)] were also utilized. The search strategy and keywords were modified to meet different database needs. We also searched for unpublished trials using the trial registers, ClinicalTrials.gov (clinicaltrials.gov), and the International Clinical Trials Registry Platform (apps.who.int/trialsearch/) using the search term “schizophrenia and raloxifene and postmenopause.” Reference lists of retrieved studies and review articles were manually searched for additional studies relevant for the meta-analysis. Conference abstracts (from the Schizophrenia International Research Society from 2006 to 2017) and unpublished studies where a full report was not available, were included when data was provided by the authors.
The following selection criteria were used for study inclusion, collectively known as the acronym, PICOS: Participant (P): Postmenopausal women with schizophrenia by any diagnostic criteria, such as DSM-IV (Hu 2003). Only choose postmenopausal women who chose raloxifene which is a selective estrogen receptor modulator commonly used for clinical treatment of postmenopausal women, such as for osteoporosis (Naylor et al. 2016). Also, at present, raloxifene treatment for mental disorders is primarily concentrated in postmenopausal women with schizophrenia (Rodante and Usall 2014). Intervention (I): Raloxifene plus antipsychotics. Comparison (C): Antipsychotics plus placebo or antipsychotics plus raloxifene. Outcomes (O): Efficacy and safety. Study design (S): All relevant RCTs were included while non-randomized and open-label studies were not. Studies with a cross-over design were also excluded because raloxifene is likely to have long-term effects on psychotic symptoms (Lafuente and Esquifino 2002). In addition, when studies were reported to be randomized but methods were not clear, authors will be contacted to substantiate study design. If studies reported results for both men and women, authors were contacted for female data only. RCTs of all durations were included, as hormone modulation is well-known to have rapid onset. Indeed, studies of raloxifene treatment for schizophrenia showed that the majority of symptoms improved in as little as 4 weeks (Usall et al. 2016; Kulkarni et al. 2016). Therefore, trials of all treatment duration were included, and mean change from baseline to study endpoint were identified.
Data extraction and outcome measures
Two independent investigators conducted data extraction and assessment of study quality. Researchers reviewed the included studies and used the same predetermined checklist to extract relevant information from each study, including study objective, study design, sample demographics (such as population, diagnostic criteria, duration of illness, dose of drugs), and experimental outcomes. A third investigator examined the results, and a consensus was reached. Moreover, study authors were contacted to obtain missing information or for clarification. Any discrepancies identified during data entry were resolved by discussion. The primary outcome measure was Positive and Negative Syndrome Scale (PANSS) total scores. The key secondary outcomes were as follows: PANSS positive and negative scores, general symptoms scores, discontinuation rate, and adverse drug reaction.
Assessment of study quality
The modified Jadad scale (Jadad et al. 1996) and risk of bias (Higgins and Green 2008) were used to assess the quality of each study. The criteria of high quality were defined as a Jadad score of 4–7. The grading of recommendations assessment and evaluation (GRADE) system was used to assess the quality of evidence and the strength of recommendations of the result of the meta-analysis (Balshem et al. 2011). The overall level of evidence was rated as “high,” “moderate,” “low,” or “very low.”
Data synthesis and statistical analysis
Some of the included studies did not provide sufficient data directly for meta-analysis, therefore we contacted but received no response. As a result, GetData Graph Digitizer 2.25 software (http://getdata-graph-digitizer.com/) was used to digitize and extract the data in order for inclusion in the meta-analysis. Specifically, this occurred with an important dose-related study (Kulkarni et al. 2010) comprising three parts: raloxifene 120 mg (n = 13), raloxifene 60 mg (n = 9), and placebo (n = 13). We referred to the Cochrane Handbook, as well as the methodology in the Cochrane Effective Practice and Organization of Care Group (Alderson et al. 2004; Mowatt et al. 2001). In brief, the “sharedrplacebo” group was split (n = 13) into two placebo comparisons groups with smaller sample size, (n = 6 and n = 7). RevMan 5.2 software was then used for meta-analysis (Green 2008). The random effects or fix effects model was performed to combine all studies. Standard mean differences (SMD), and 95% confidence interval (CI) were calculated using the inverse-variance method for continuous data (PANSS scores). Risk ratio (RR) ± 95% CI was calculated using the Mantel-Haenszel method for dichotomous data (discontinuation rate and adverse drug reactions). For each pooled outcome, p < 0.05 of the Z test was used to determine the significance of overall effect. There was obvious heterogeneity when I 2 > 50% or p < 0.1 using the chi-square test. For outcomes, reasons were sought explaining the heterogeneity by conducting a sensitivity analysis (i.e., removing the study that SMD > 0.8 (Alderson et al. 2004)).There were only six studies included in the meta-analysis, so it was not possible to assess publication bias [which requires at least ten studies (Sterne and Higgins 2011)]. All analyses were considered significant at the level of p < 0.05.
Results
Search results
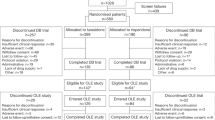
A total of 110 references were obtained from the electronic search (Fig. 1). All were published in English. After removing duplicates (n = 32), a further 65 articles were excluded based on title and abstract inspection. Thirteen studies were subjected to full-text inspection. During the stage of quality appraisal and data extraction, seven articles were omitted due to the following reasons: (1) the production of multiple publications from single studies had occurred on two occasions; Usall et al. (2011) and Huertaramos et al. (2014) shared the same clinicaltrials.gov identifier (NCT01041092). Specifically, Usall et al. focused on improvement in symptoms of psychosis, while Huerta-Ramos et al. reported only cognitive improvement. Usall et al. (2016) and Labad et al. (2016) also shared the same clinicaltrials.gov identifier (NCT01573637). Labad et al. only reported the relationship between genetic variation and improvement of negative symptoms. Therefore, these two articles (Huertaramos et al. 2014; Labad et al. 2016) were excluded. (2) Three articles (Kindler et al. 2015, 2016; Weickert et al. 2015) had cross-over design, and did not meet the inclusion criteria. (3) Two articles (Bratek et al. 2016; Torrey and Davis 2012) were reviews. Finally, six RCTs (Gilda Kianimehr et al. 2014; Kulkarni et al. 2016; Kulkarni et al. 2010; Usall et al. 2016, 2011; Weiser et al. 2017) met the selection criteria for the meta-analysis and one, the Kulkarni et al. 2010, included two treatment arms.
Study and sample characteristics
Six studies comparing adjunctive raloxifene (n = 225) with placebo (n = 215) lasting 13.71 ± 5.09 weeks (range = 8–24 weeks, median = 12 weeks) were analyzed (Table 1). A total of 440 patients (sample size range = 33–200) were included. Of the six RCTs, two were conducted in Australia (two RCTs, n = 91), while the others were in Iran (two RCTs, n = 103), Spain (one RCT, n = 46), and Romania (one RCT, n = 200) respectively. Just one study (Weiser et al. 2017) evaluated the efficacy of raloxifene in severely ill, decompensated postmenopausal women with schizophrenia. All participants met the DSM-IV or DSM-IV-TR diagnostic criteria and all studies used the PANSS scale to assess psychiatric symptoms of patients. The dosage of raloxifene was 60 or 120 mg.
Quality assessment
All included studies were RCTs. The methods of sequence generation were not described in two studies (Gilda Kianimehr et al. 2014; Weiser et al. 2017), and allocation concealments were not described in three studies (Gilda Kianimehr et al. 2014; Kulkarni et al. 2010; Weiser et al. 2017). In addition, two studies (Kulkarni et al. 2016, 2010) did not have complete outcome data, and did not provide pertinent data, such as mean and standard deviation. Two other studies (Usall et al. 2011, 2016) were biased, as reporting was selective and another study (Kulkarni et al. 2010) were partially sponsored by a pharmaceutical company (Table 2). The Jadad score and the number of low risk judgments were 5.50 ± 0.55 (range = 5–6, median = 5.5) and 5.33 ± 0.82 (range = 4–6, median = 5.5), respectively. All studies were of high quality and the evidence quality of six outcome measures was assessed by GRADE approach ranging from low (50%) to moderate (50%) (Table 3).
Primary outcomes
Meta-analysis of PANSS scale total scores showed a superiority in efficacy of adjunctive raloxifene in the treatment group compared to the placebo group [SMD −0.55, (95% CI −1.01, −0.09), p = 0.02; I 2 = 77%, Fig. 2]. In order to explain the heterogeneity, a sensitivity analysis was conducted, and after one outlier (SMD = 0.26) study (Weiser et al. 2017) was removed, the results were considered robust [SMD −0.70, (95% CI −0.96, −0.44), p < 0.00001; I 2 = 0%].
Secondary outcome
Meta-analysis of positive symptom scores showed that the adjunctive raloxifene treatment group was superior compared to the placebo group [SMD −0.22, (95% CI −0.41, −0.02), p = 0.03; I 2 = 79%, Fig. 3a]. In order to explain the heterogeneity, a sensitivity analysis was conducted, and after two outlier (SMD = 1.17 and 0.15) studies [one treatment arm (raloxifene 60 mg) of study (Kulkarni et al. 2010) and (Weiser et al. 2017)] were removed, the results remained robust [SMD −0.64, (95% CI −0.92, −0.37), p < 0.00001; I 2 = 41%]. Meta-analysis of negative symptom scores [SMD −0.46, (95% CI −0.89, −0.02), p = 0.04; I 2 = 74%, Fig. 3b] and general symptom scores [SMD −0.55, (95% CI −0.99, −0.11), p = 0.01; I 2 = 75%, Fig. 3c] showed a superiority in efficacy of adjunctive raloxifene. The heterogeneity ceased when one study (Weiser et al. 2017) was remove. The results also showed a superiority of adjunctive raloxifene in improvement of negative symptom scores [SMD −0.57, (95% CI −0.83, −0.31), p < 0.0001; I 2 = 0%] and general symptom scores [SMD −0.69, (95% CI −0.95, −0.42), p < 0.00001; I 2 = 0%].
In one study (Usall et al. 2016), eight patients in the raloxifene group (n = 38) did not finish the study: three patients had changes in medication during the study, three patients refused to participate, one patient suffered a worsening in psychopathology, and one patient decided not to participate due to dizziness. In the placebo group (n = 32), five patients did not finish the study, five patients refused to participate, and one patient presented unrelated adverse effects. In another study (Kulkarni et al. 2016), three patients in the raloxifene group (n = 26) did not finish the study, two patients missed the experimental drug >2 days after week 6, and one patient withdrew after week 8. In the placebo group (n = 30), four patients did not finish the study, one patient went abroad after week 4, one patient missed the experimental drug >2 days after week 6, one patient withdrew after week 8, and one patient was hospitalized after week 10.
Meta-analysis of all-cause discontinuation showed no significant difference between adjunctive raloxifene treatment and the placebo (RR = 1.38, p = 0.51). Similarly, no difference was found between the two groups regarding discontinuation due to worsening in psychopathology (RR = 2.54, p = 0.56) and adverse effects (RR = 2.54, p = 0.56). Five of the six studies (Gilda Kianimehr et al. 2014; Kulkarni et al. 2016; Usall et al. 2016, 2011; Weiser et al. 2017) reported adverse drug reaction. In the current study, no significant difference was found between adjunctive raloxifene treatment and the placebo in adverse drug reaction (RR = 1.27, p = 0.57). In the raloxifene group (n = 205), the adverse drug reactions were constipation (1.46%, RR = 1.50, p = 0.64), dry mouth (0.98%, RR = 5.00, p = 0.29), restless leg syndrome (0.49%, RR = 3.00, p = 0.49), dizziness (0.49%, RR = 2.54, p = 0.56), pneumonia (0.49%, RR = 3.00, P = 0.50), binge drinking (0.49%, RR = 3.44, p = 0.44), marijuana use (0.49%, RR = 3.44, p = 0.44), and nonadherence to the antipsychotic regiment (0.49%, RR = 3.44, p = 0.44).
Discussion
Main findings
Based on data suggesting estrogens play a protective role in the pathophysiology of schizophrenia, raloxifene have been studied as a candidate adjunctive therapy to available antipsychotics in postmenopausal women with schizophrenia. Meta-analysis of six RCTs (n = 440) showed that adjunctive raloxifene was significantly superior to the placebo group in the reducing overall symptoms of schizophrenia. In addition, raloxifene was generally safe and well-tolerated as discontinuous and adverse reaction occurred at similar frequency between raloxifene and the placebo.
In this study, we found a significant heterogeneity (I 2 = 74—79%) in meta-analysis of PANSS scores and therefore a sensitivity analysis was conducted. After one outlier study (Weiser et al. 2017) was removed, the heterogeneity was reduced (I 2 = 0—69%), and the results of meta-analysis become more robust. In Weiser et al.’s (2017) study, results did not support the use of raloxifene to reduce symptoms in severely ill, decompensated, postmenopausal women with schizophrenia. This result indicated that raloxifene may be efficacious for patients with less severe symptoms. Moreover, it is possible that individual differences in response to antipsychotic drugs could have increased the standard deviation of the improvement in PANSS scores in the aforementioned study. Interestingly, the heterogeneity in meta-analysis of PANSS positive score was negated (I 2 = 69% to I 2 = 41%) by removing one study [one treatment arm (raloxifene 60 mg) (Kulkarni et al. 2010)] reporting a null effect. A dose of 60 mg/day is the documented dose for the approved indications of raloxifene, but as negative symptoms are more resistant to treatment than positive symptoms (Millan et al. 2014), Kulkarni et al. (2010) found that a 120 mg/day dose of raloxifene was more effective than either a 60 mg/day dose of raloxifene or placebo in recovery of total and general psychotic symptoms. Usall et al. (2016) found the effect of 60 mg/day of raloxifene on positive symptoms was not as effective when compared to other symptoms (negative and general psychopathology). Nevertheless, clinical trials and case reports have shown that adjunctive raloxifene at doses of 60 and 120 mg is beneficial in postmenopausal women with schizophrenia for the treatment of positive, negative, and general psychopathology symptoms (Sharma et al. 2012). Usall et al. (2011) also found a significant effect on positive and general psychopathological symptoms following the addition of raloxifene (60 mg/day), although a small sample size and short follow-up time could partly explain this finding.
Usall et al. (2016) provided data for 24 weeks of treatment, whereas most others only provided data for only 12 weeks. Interestingly, Usall et al. (2011) performed a 12-week follow-up study to assess the utility of raloxifene in treating psychotic symptoms in postmenopausal women with schizophrenia exhibiting prominent negative symptoms, and found that raloxifene (60 mg/day) significantly reduced not only negative symptoms but also positive and general psychopathological symptoms. These results were confirmed by the same group 5 years later, when a study of 70 women was conducted for 24-week duration. However, they found that raloxifene improved negative, general, and total but not positive symptoms. Another 12-week follow-up study conducted by Gilda Kianimehr et al. (2014) with a sample size of 46 patients found raloxifene (120 mg/day) was only effective in treating positive symptoms. The discrepancies between the findings may be related to several issues involving sample characteristics, including small sample sizes and differences in the severity of positive symptoms.
Additionally, raloxifene was found not only to improve psychotic symptoms but also cognitive function. In this meta-analysis, there were no studies that met the criteria for analyzing cognitive function, and as such, this topic was not discussed. Animal studies have shown that raloxifene can enhance working memory, increase forebrain neurogenesis and synaptic plasticity, repair neuronal and synaptic connectivity, and reduce oxidative stress and neuroinflammation (Khan 2016). In humans, functional magnetic resonance imaging studies revealed raloxifene adjunct therapy improved probabilistic association learning and increased neuronal activity in specific brain regions associated with schizophrenia (Kindler et al. 2015). Huertaramos et al. (2014) reported that raloxifene (60 mg) had a positive effect on verbal memory processing and executive functions. However, findings by Yaffe et al. (2005) concluded that cognitive benefits were evident with 120 mg but not 60 mg of raloxifene in postmenopausal women (Yaffe et al. 2005). These inconsistent results require further clarification.
The majority of studies used in the current meta-analysis showed that overall, discontinuation rates and adverse events were not significantly different between the raloxifene and placebo groups. Raloxifene is known to act an agonist on bone tissue, while it has antagonist effects on breast and uterine tissue, and thus inhibit the negative effects of estrogens on uterine and breast tissue. Furthermore, studies have shown that raloxifene has no effects on the incidence of central nervous events and vaginal symptoms (Davies et al. 1994; Rodante and Usall 2014). In a controlled trial with raloxifene, Davies et al. (1994) found that vaginal bleeding, hot flashes, and leg cramps were greater in postmenopausal women treated with raloxifene, but did not cause any discontinuations. However, longer-term studies will need to assess long-lasting treatment effects.
A meta-analysis by Heringa et al. (2015) analyzing 24 RCT (n = 1149) reported that estrogens and SERMs were effective in the treatment of women with schizophrenia. Furthermore, the group performed a subgroup analysis that yielded significant results for the SERM raloxifene (3 studies with 127 patients) in postmenopausal women for total and negative, but not positive symptoms. Two recent RCT (Kulkarni et al. 2016; Usall et al. 2016) were added to the current meta-analysis which found that raloxifene improved positive symptoms in postmenopausal patients with schizophrenia. The results of the current meta-analysis indicated that there was no significant difference regarding adverse drug reactions between the raloxifene and placebo groups. Therefore, compared to other estrogen-altering compounds, raloxifene is safer, and thus should be considered as a preferred drug for adjunctive hormonal therapy of for postmenopausal women with schizophrenia. Additionally, the lack of adverse effects on uterine and breast tissue also makes raloxifene advantageous over other estrogen-altering drugs (Chua et al. 2005).
Limitations
Several limitations need to be acknowledged. (1) The sample sizes were relatively small in the current study. In addition, the publication bias of the present meta-analysis was not tested because only a small number of RCTs were found. (2) Some of the included studies did not provide sufficient data for meta-analysis directly, and although the authors were contacted, we received no response. Therefore, GetData Graph Digitizer was utilized to extract data, which may have resulted in certain inaccuracies. (3) Due to inadequate available information, the genetic variants for augmentation therapy in patients could not be examined. (4) All studies had relatively short treatment durations (8–24 weeks), thus the long-term effects of raloxifene could not be examined. Nevertheless, the validity of the major findings in the study have been supported by more recent clinical studies. (5) This meta-analysis focused on the effect of raloxifene on postmenopausal women with schizophrenia. Raloxifene also can be used for the treatment of chronic schizophrenia in men and premenopausal women (Khodaie-Ardakani et al. 2015; Kindler et al. 2016; Weickert et al. 2015) and future studies need to consider the effects of raloxifene on different populations.
Conclusions
This study showed that adjunctive raloxifene appears to be efficacious and safe for postmenopausal women with schizophrenia. Adjunctive raloxifene treatment did not have greater discontinuation or adverse drug reactions compared to the placebo. Moreover, raloxifene may be efficacious for patients with less severe symptoms. However, given the low to moderate quality of the evidence of the included studies, these results must be considered suggestive and not definitive. Better designed studies that include more detailed descriptions of the methods employed are needed to confirm (or disprove) these results. In addition, future studies with a large sample size are needed to confirm these findings, and the long-term effects of raloxifene on psychopathology should be examined.
References
Alderson P, Green S, Higgins JPT (2004) Cochrane Reviewers’ Handbook 4.2.2 [updated march 2004]. John Wiley & Sons, Ltd, Chichester
Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, Brozek J, Vist GE, Falckytter Y, Meerpohl J, Norris S (2011) GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 64:401–413. https://doi.org/10.1016/j.jclinepi.2010.07.015
Bethea CL, Mirkes SJ, Shively CA, Adams MR (2000) Steroid regulation of tryptophan hydroxylase protein in the dorsal raphe of macaques. Biol Psychiatry 47:562–576. https://doi.org/10.1016/S0006-3223(99)00156-0
Bratek A, Krysta K, Drzyzga K, Barańska J, Kucia K (2016) The role of selective estrogen receptor modulators in the treatment of schizophrenia. Psychiatr Danub 28:45–48
Cariagamartinez A, Saizruiz J, Alelúpaz R (2016) From linkage studies to epigenetics: what we know and what we need to know in the neurobiology of schizophrenia. Front Neurosci 10:202. https://doi.org/10.3389/fnins.2016.00202
Chua WL, de Izquierdo SA, Kulkarni J, Mortimer A (2005) Estrogen for schizophrenia. Cochrane Database Syst Rev 4:CD004719
Corson SL (2009) Breast cancer after use of estrogen plus progestin in postmenopausal women. N Engl J Med 360:573–587. https://doi.org/10.1056/NEJMoa0807684
Davies GC, Huster WJ, Lu Y, Plouffer L, Lakshmanan M (1994) Adverse events reported by postmenopausal women in controlled trials with raloxifene. Obstet Gynecol 93:558–565. https://doi.org/10.1016/S0029-7844(98)00476-1
Di PT (1994) Modulation of brain dopamine transmission by sex steroids. Rev Neurosci 5:27–41. https://doi.org/10.1515/REVNEURO.1994.5.1.27
Fink G, Sumner BE, Rosie R, Grace O, Quinn JP (1996) Estrogen control of central neurotransmission: effect on mood, mental state, and memory. Cell Mol Neurobiol 16:325–344. https://doi.org/10.1007/BF02088099
Gilda Kianimehr FF, Hashempoor S, Khodaei-Ardakani M-R, Rezaei F, Nazari A, Kashani L, Akhondzadeh S (2014) Raloxifene adjunctive therapy for postmenopausal women suffering from chronic schizophrenia: a randomized double-blind and placebo controlled trial. DARU Journal of Pharmaceutical Sciences 22:55–62. https://doi.org/10.1186/2008-2231-22-55
Green S (2008) Cochrane handbook for systematic reviews of interventions: Cochrane book series. Naunyn-Schmiedeberg's Arch Exp Pathol Pharmakol 5:S38. https://doi.org/10.1002/9780470712184
Heringa SM, Begemann MJ, Goverde AJ, Sommer IE (2015) Sex hormones and oxytocin augmentation strategies in schizophrenia: a quantitative review. Schizophr Res 168:603–613. https://doi.org/10.1016/j.schres.2015.04.002
Higgins JP, Green S (2008) Cochrane handbook for systematic reviews of interventions: Cochrane book series. Wiley-Blackwell, Hoboken, pp 102–108. https://doi.org/10.1002/9780470712184
Holsen LM, Spaeth SB, Lee JH, Ogden LA, Klibanski A, Whitfield-Gabrieli S, Goldstein JM (2010) Stress response circuitry hypoactivation related to hormonal dysfunction in women with major depression. J Affect Disord 131:379–387. https://doi.org/10.1016/j.jad.2010.11.024
Hu RJ (2003) Diagnostic and statistical manual of mental disorders ( DSM-IV ). Encyclopedia of the Neurological Sciences 35:4–8. https://doi.org/10.1016/B0-12-226870-9/01070-4
Huber TJ, Rollnik J, Wilhelms J, Von ZMA, Emrich HM, Schneider U (2001) Estradiol levels in psychotic disorders. Psychoneuroendocrinology 26:27–35. https://doi.org/10.1016/S0306-4530(00)00034-2
Huertaramos E, Iniesta R, Ochoa S, Cobo J, Miquel E, Roca M, Serranoblanco A, Teba F, Usall J (2014) Effects of raloxifene on cognition in postmenopausal women with schizophrenia: a double-blind, randomized, placebo-controlled trial. European Neuropsychopharmacology the Journal of the European College of Neuropsychopharmacology 24:223–231. https://doi.org/10.1016/j.euroneuro.2013.11.012
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, Mcquay HJ (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17:1–12. https://doi.org/10.1016/0197-2456(95)00134-4
Jarkova NB, Martenyi F, Masanauskaite D, Walls EL, Smetnik VP, Pavo I (2002) Mood effect of raloxifene in postmenopausal women. Maturitas 42:71–75. https://doi.org/10.1016/S0378-5122(01)00303-6
Khan MM (2016) Neurocognitive, neuroprotective, and cardiometabolic effects of raloxifene: potential for improving therapeutic outcomes in schizophrenia. CNS Drugs 30:589–601. https://doi.org/10.1007/s40263-016-0343-6
Khodaie-Ardakani MR, Khosravi M, Zarinfard R, Nejati S, Mohsenian A, Tabrizi M, Akhondzadeh S (2015) A placebo-controlled study of raloxifene added to risperidone in men with chronic schizophrenia. Acta Medica Iranica 53:337–345
Kindler J, Weickert CS, Skilleter AJ, Catts SV, Lenroot R, Weickert TW (2015) Selective estrogen receptor modulation increases hippocampal activity during probabilistic association learning in schizophrenia. Neuropsychopharmacology Official Publication of the American College of Neuropsychopharmacology 40:2388–2397. https://doi.org/10.1038/npp.2015.88
Kindler J, Weickert CS, Schofield PR, Lenroot R, Weickert TW (2016) Raloxifene increases prefrontal activity during emotional inhibition in schizophrenia based on estrogen receptor genotype. Eur Neuropsychopharmacol 26:1930–1940. https://doi.org/10.1016/j.euroneuro.2016.10.009
Kulkarni J, Gurvich C, Lee SJ, Gilbert H, Gavrilidis E, De CA, Berk M, Dodd S, Fitzgerald PB, Davis SR (2010) Piloting the effective therapeutic dose of adjunctive selective estrogen receptor modulator treatment in postmenopausal women with schizophrenia. Psychoneuroendocrinology 35:1142–1147. https://doi.org/10.1016/j.psyneuen.2010.01.014
Kulkarni J, Gavrilidis E, Worsley R, Hayes E (2012) Role of estrogen treatment in the management of schizophrenia. CNS Drugs 26:549–557. https://doi.org/10.2165/11630660-000000000-00000
Kulkarni J, Gavrilidis E, Wang W, Worsley R, Fitzgerald PB, Gurvich C, Van RT, Berk M, Burger H (2014) Estradiol for treatment-resistant schizophrenia: a large-scale randomized-controlled trial in women of child-bearing age. Mol Psychiatry 20:1–8. https://doi.org/10.1038/mp.2014.33
Kulkarni J, Gavrilidis E, Gwini SM, Worsley R, Grigg J, Warren A, Gurvich C, Gilbert H, Berk M, Davis SR (2016) Effect of adjunctive raloxifene therapy on severity of refractory schizophrenia in women: a randomized clinical trial. Jama Psychiatry 73:947–954. https://doi.org/10.1001/jamapsychiatry.2016.1383
Kumari V (2011) Sex differences and hormonal influences in human sensorimotor gating: implications for schizophrenia. Curr Top Behav Neurosci 8:141–154. https://doi.org/10.1007/7854_2010_117
Labad J, Martorell L, Huerta-Ramos E, Cobo J, Vilella E, Rubio-Abadal E, Garcia-Pares G, Creus M, Núñez C, Ortega L (2016) Pharmacogenetic study of the effects of raloxifene on negative symptoms of postmenopausal women with schizophrenia: a double-blind, randomized, placebo-controlled trial. European Neuropsychopharmacology the Journal of the European College of Neuropsychopharmacology 26:1683–1689. https://doi.org/10.1016/j.euroneuro.2016.08.006
Lafuente A, Esquifino AI (2002) Effects of long-lasting raloxifene treatment on serum prolactin and gonadotropin levels in postmenopausal women. july 1 - july 15 -OT 12hrs (7/1,3,4) july 16 - july 31 - OT 4hrs (7/31) paid aug 1 - aug 15 -OT 1511hrs (8/1,2,3,4) paid 147:461–465. https://doi.org/10.1530/eje.0.1470461
Littleton-Kearney MT, Ostrowski NL, Cox DA, Rossberg MI, Hurn PD (2002) Selective estrogen receptor modulators: tissue actions and potential for CNS protection. Cns Drug Reviews 8:309–330. https://doi.org/10.1111/j.1527-3458.2002.tb00230.x
Meitzen J, Mermelstein PG (2011) Estrogen receptors stimulate brain region specific metabotropic glutamate receptors to rapidly initiate signal transduction pathways. J Chem Neuroanat 42:236–241. https://doi.org/10.1016/j.jchemneu.2011.02.002
Millan MJ, Fone K, Steckler T, Horan WP (2014) Negative symptoms of schizophrenia: clinical characteristics, pathophysiological substrates, experimental models and prospects for improved treatment. Eur Neuropsychopharmacol 24:645–692. https://doi.org/10.1016/j.euroneuro.2014.03.008
Moen MD, Keating GM (2008) Raloxifene: a review of its use in the prevention of invasive breast cancer. Drugs 68:2059–2083. https://doi.org/10.2165/00003495-200868140-00008
Moher D, Liberati A, Tetzlaff J, Altman DG (2014) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Revista Española De Nutrición Humana Y Dietética 18:889–896. https://doi.org/10.1136/bmj.b2535
Mortimer AM (2007) Relationship between estrogen and schizophrenia. Expert Rev Neurother 7:45–55. https://doi.org/10.1586/14737175.7.1.45
Mowatt G, Grimshaw JM, Davis DA, Mazmanian PE (2001) Getting evidence into practice: the work of the Cochrane effective practice and organization of care group (EPOC). J Contin Educ Health Prof 21:55–60. https://doi.org/10.1002/chp.1340210109
Naylor KE, Jacques RM, Peel NFA (2016) Response of bone turnover markers to raloxifene treatment in postmenopausal women with osteopenia. Osteoporos Int 27:2585–2592. https://doi.org/10.1007/s00198-016-3573-z
Peuskens J, Pani L, Detraux J, De HM (2014) The effects of novel and newly approved antipsychotics on serum prolactin levels: a comprehensive review. CNS Drugs 28:421–453. https://doi.org/10.1007/s40263-014-0157-3
Riecher-Rössler A, Häfner H (1993) Schizophrenia and oestrogens—is there an association? Eur Arch Psychiatry Clin Neurosci 242:323–328. https://doi.org/10.1007/BF02190244
Riecher-Rössler A, Kulkarni J (2010) Estrogens and gonadal function in schizophrenia and related psychoses, vol 8. Springer, Berlin, pp 155–171. https://doi.org/10.1007/7854_2010_100
Rodante D, Usall J (2014) Raloxifene as adjuvant in the treatment of schizophrenia: a review of efficacy and safety issues. J of Symptoms and Signs 3:229–237
Sánchez MG, Morissette M, Di PT (2013) Oestradiol modulation of serotonin reuptake transporter and serotonin metabolism in the brain of monkeys. J Neuroendocrinol 25:560–569. https://doi.org/10.1111/jne.12034
Shang Y, Brown M (2002) Molecular determinants for the tissue specificity of SERMs. Science 295:2465–2468. https://doi.org/10.1126/science.1068537
Sharma E, Raveendranathan D, Shivakumar V, Jayaram N, Rao NP, Venkatasubramanian G (2012) Beneficial effects of add-on raloxifene in schizophrenia. Archives of Women's Mental Health 15:147–148. https://doi.org/10.1007/s00737-012-0259-1
Sribnick EA, Wingrave JM, Matzelle DD, Wilford GG, Ray SK, Banik NL (2005) Estrogen attenuated markers of inflammation and decreased lesion volume in acute spinal cord injury in rats. J Neurosci Res 82:283–293. https://doi.org/10.1002/jnr.20622
Sterne JAC, Higgins JPT (2011) Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 343:d4002. https://doi.org/10.1136/bmj.d4002
Talonen S, Väänänen J, Kaltiala-Heino R (2017) Gender differences in first onset schizophrenia spectrum psychoses. Nordic Journal of Psychiatry 2:1–8. https://doi.org/10.1080/08039488.2016.1245783
Taylor R, Langdon R (2006) Understanding gender differences in schizophrenia: a review of the literature. Curr Psychiatr Rev 2:255–265. https://doi.org/10.2174/157340006776875987
Torrey EF, Davis JM (2012) Adjunct treatments for schizophrenia and bipolar disorder: what to try when you are out of ideas. Clinical Schizophrenia & Related Psychoses 5:208–216. https://doi.org/10.3371/CSRP.5.4.5
Usall J, Huertaramos E, Labad J, Cobo J, Núñez C, Creus M, Parés GG, Cuadras D, Franco J, Miquel E (2011) Raloxifene as an adjunctive treatment for postmenopausal women with schizophrenia: a 24-week double-blind, randomized, parallel, placebo-controlled trial. The Journal of clinical psychiatry 72:1552–1557. https://doi.org/10.4088/JCP.10m06610
Usall J, Huerta-Ramos E, Labad J, Cobo J, Nunez C, Creus M, Pares GG, Cuadras D, Franco J, Miquel E, Reyes JC, Roca M, Group R (2016) Raloxifene as an adjunctive treatment for postmenopausal women with schizophrenia: a 24-week double-blind, randomized, parallel, placebo-controlled trial. Schizophr Bull 42:309–317. https://doi.org/10.1093/schbul/sbv149
Weickert TW, Weinberg D, Lenroot R, Catts SV, Wells R, Vercammen A, O'Donnell M, Galletly C, Liu D, Balzan R (2015) Adjunctive raloxifene treatment improves attention and memory in men and women with schizophrenia. Mol Psychiatry 20:S339–S340. https://doi.org/10.1038/mp.2015.11
Weiser M, Levi L, Burshtein S, Hagin M, Matei VP, Podea D, Micluția I, Tiugan A, Păcală B, Grecu IG, Noy A, Zamora D, Davis JM (2017) Raloxifene plus antipsychotics versus placebo plus antipsychotics in severely ill decompensated postmenopausal women with schizophrenia or schizoaffective disorder: a randomized controlled trial.[J]. J Clin Psychiatry 23:1–14. https://doi.org/10.4088/JCP.15m10498
Wong J, Seeman MV, Shapiro H (2003) Case report: raloxifene in postmenopausal women with psychosis: preliminary findings. Am J Geriatr Psychiatr 11:697–698. https://doi.org/10.1176/appi.ajgp.11.6.697
Yaffe K, Krueger K, Cummings SR, Blackwell T, Henderson VW, Sarkar S, Ensrud K, Grady D (2005) Effect of raloxifene on prevention of dementia and cognitive impairment in older women: the multiple outcomes of raloxifene evaluation (MORE) randomized trial. Am J Psychiatr 162:683–690. https://doi.org/10.1176/appi.ajp.162.4.683
Funding
This study was funded by the Natural Science Foundation of Liaoning Province (Project No. 2015020481).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Wang, Q., Dong, X., Wang, Y. et al. Raloxifene as an adjunctive treatment for postmenopausal women with schizophrenia: a meta-analysis of randomized controlled trials. Arch Womens Ment Health 21, 31–41 (2018). https://doi.org/10.1007/s00737-017-0773-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00737-017-0773-2