Abstract
Despite exercise or physical activity (PA) being effective on depression and weight management generally, its effectiveness remains uncertain during postpartum. This systematic review aimed to determine the efficacy of exercise or PA interventions on postnatal depression (PND) and weight loss, with a subsequent aim to identify more effective intervention approaches. Using PRISMA guidelines, data searches conducted across six databases. Nine studies fulfilled our inclusion criteria. Based on identified studies (some with high-quality RCT designs), there was inconsistency as to whether exercise or PA simultaneously reduced PND symptoms and assisted weight loss (or related body composition indices). Two (22.2%) identified changes in both outcomes with small effect sizes. Four studies (44.4%) reported changes in one outcome, typically PND with variable effect sizes, while three studies (33.3%) reported no effect. Studies implemented different exercise/PA modalities (commonly walking) and incorporated various support strategies to assist intervention participation and adherence. Studies identified as most likely to associate with PND and/or weight loss changes were those with supervision (1–1, group), structure (weekly frequency, scheduled durations and moderate intensity), which adhered to specific exercise/PA guidelines over an extended postpartum period (e.g. 12 weeks +) and were supplemented by several psycho-social support strategies (e.g. educational information, exercise/PA advice, and counselling). Future studies need to carefully address prior study methodological weaknesses (e.g. study design, inclusion criteria, measurement, reporting, assessing confounding factors), further examine proposed more beneficial exercise/PA intervention approaches, and consider how exercise/PA could be best delivered in practice to benefit women’s postpartum health.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
For a new mother, the postpartum period can be associated with substantial psychological and physiological challenge and change. At this time, women often experience mental and physical fatigue (Dennis and Ross 2005), disrupted sleep (Meades and Ayers 2011), mood disturbance, social isolation (O’Hara and Swain 1996), lowered self-esteem (Beck 2001), anxiety (including those related to parenting) and can subsequently lead to postnatal depression (PND; Robertson et al. 2004). PND is considered as a form of major depressive disorder (American Psychiatric Association 2013a, b) and has an estimated prevalence of 10–15% in western societies (Muzik et al. 2009; O’Hara and Swain 1996). PND typically refers to an episode of depression (mild-severe in nature) that can occur between the birth of a newborn to across the first year postpartum (Lindahl et al. 2005; Marcus et al. 2003) and is often medically and psychologically associated with dysfunction in cognitive, emotional and psychological capacities. However, from evolutionary perspectives (Brüne 2015; Thornhill and Furlow 1998; Tracey 2005), PND has been viewed as an outcome of psychological challenge and adaptation (not dysfunction) in which a mother is searching and evaluating for ways to continue (or cease) in providing care and support for her off-spring (Hagen 1999).
PND is of significant concern due to some of the potential mal-adaptive health risks to both mother and baby. For example, PND can include dissociated emotional attachment and loathing of the newborn (Grace et al. 2003) and has been shown to detrimentally affect cognitive and emotional development in the child (Kim-Cohen et al. 2005; Murray et al. 1999; Hay et al. 2003). PND has been associated with suicide ideation (Howard et al. 2011), while more severe depression episodes have been associated with suicide attempts (Gressier et al. 2016). In terms of physiological change, the postpartum period is also associated with physical (anthropometric) body change, due to body shape changes from pregnancy, mobility constraints during pregnancy and following birth and post-birth weight retention. It is estimated that between 14 and 20% of women gain 5 kg—relative to their pre-pregnancy weight—at 1 year postpartum (Walker 2007). Postpartum weight retention has been identified as a significant contributor to obesity risk postpartum, including for women who were normal weight pre-pregancy (Endres et al. 2015). The potential for weight gain during the initial year of parenthood can also be compounded from being less active or more sedentary (Doran and Davis 2011; Evenson et al. 2004; Vernon et al. 2010) along with changes in nutritional behaviour (e.g. high caloric intake; Milgrom et al. 2011; Peterson et al. 2002). Becoming overweight and obese is also worthy of consideration due to its predicted inter-relationships with psychological and physical health (Herring et al. 2008). For instance, lowered self-esteem, efficacy and distress in the postpartum period have been associated with weight gain and PND (Clark et al. 2009; Nagl 2015; Silveira et al. 2015). A desire to restore pre-pregnancy body shape may also be evident (Haas et al. 2005), and therefore, body shape, weight and image concerns can be prevalent affecting psychological health. Independently, excess postpartum weight has also been identified as a predictor of PND occurrence (Jenkin and Tiggermann 1997; LaCoursiere et al. 2006).
Evidence also strongly suggests that excess postpartum weight and obesity can have onward detrimental health outcomes. In their systematic review and meta-analysis, Luppino et al. (2010) highlighted a reciprocal relationship between baseline obesity and depression and subsequent status. Obesity and depression are associated with inflated risks of chronic depression (Cooper and Murray 1995) and lowered cardio-respiratory fitness (Evenson et al. 2004; Mottola 2002). If not addressed, weight gain has also been associated with obesity later in life (Rooney and Schauberger 2002; Schmitt et al. 2007), metabolic syndrome (Walker 2007) and ultimately a heightened risk of maternal mortality (Dietz et al. 2005). Considered together, existing evidence points toward potentially important interacting relationships, and progressively detrimental development trends over time associated with PND, depression and weight gain. Therefore, the importance of protecting and assisting psychological and physical health in postpartum women is significant.
Presently, clinical management of PND predominantly utilises antidepressant medication, psychotherapy or a combination as a front line approach (Dennise et al. 2007; Eninarson 2009), while only excessive weight gain leading to morbid obesity is typically—at present—associated with clinical intervention. The more typical approaches to PND management have highlighted concerns, particularly with reference to the efficacy of antidepressants for patients with different depression severities (Kirsch et al. 2008; Moncrieff and Kirsch 2005): concerns of adverse medication effects while breastfeeding (Kim et al. 2010) and higher drop-out rates from pharmacological treatment (12–40%; Kirsch et al. 2008). Psychotherapy also has limitations. In their systematic review, Dennis and Ross (2005) identified that while PND patients collectively preferred non-pharmacological options due to the reduced likelihood of side effects or harm from long-term use, they often also lacked interest in psychotherapy due to fear of further social judgement or a lack of therapist support and reassurance. Being unable to disclose emotions and feelings in treatment settings was described a common barrier in seeking help and treatment. On this basis, the identification, trialling and evaluation of feasible, cost-effective, adjunct treatments, such as exercise or PA that can improve psychological (PND) and physiological (postpartum weight) health outcomes have clinical treatment and patient significance. To prevent and protect again PND and weight gain associated detrimental health outcomes, exercise or physical activity (PA) can be considered either as an alternative, but complimentary, treatment intervention or as a beneficial lifestyle behaviour that could better meet the concerns of mothers. Specifically, helping reduce potential dependency on pharmaceutical treatment (and side effects), being low-cost, being self-controlled, and self-managed which can be done in a more preferable social-environmental context.
Growing evidence in related clinical fields identifies exercise and/or PA as a potentially effective, feasible and cost-effective adjunct treatment of depression (Bridle et al. 2012; Craft and Perna 2004). In Josefsson et al. (2014) review, aerobic exercise was identified as effective in managing adult depressive disorder regardless of symptom severity (i.e. mild-severe). Their pooled point estimate (i.e. =−0.77; Z = −4.14, p < 0.001) suggested a 33% reduction in depression-associated symptoms in favour of exercise relative controls. Further, individual studies have trialled exercise on PND patients using cohort (Currie and Develin 2002; May 1995; Wilkinson et al. 2003) and randomised control trial (RCT) designs (Fjeldsoe et al. 2009; Norman et al. 2010) in different study settings. Survey studies have also evaluated the effect of low-intensity aerobic activities such as pram walking, suggesting significant improvements in women’s well-being and marked PND symptom reductions (May 1995; Currie and Develin 2002; Wilkinson et al. 2003). Likewise, studies examining the effect of exercise or PA interventions in overweight and obese populations have shown consistent improvements in body composition and body fat indices (Asbee et al. 2009; Keller et al. 2014; Luoto et al. 2010; Schoenborn et al. 2013). Most recently, individual RCT studies have examined the possible benefit of exercise or PA interventions on both PND and body composition (e.g. weight) outcomes. These interventions have ranged from unsupervised (Albright et al. 2012) to supervised walking (Keller et al. 2014), yoga and pilates (Ko et al. 2012) to aerobic and resistance training interventions (Lecheminant et al. 2014). With a growing number of studies in this area, we felt it was logical and valuable to synthesise the available evidence to date.
Study purpose
With no prior systematic or meta-analytical studies, the purpose of this review was to determine the effectiveness of exercise or PA interventions on PND and weight loss simultaneously. Identifying whether exercise or PA has simultaneous PND treatment (e.g. symptom reduction and mood improvement) and patient preference benefits, along with potential cardio-respiratory, body composition (i.e. weight management) and long-term health protection benefits, is significant on several levels. Positive findings would help highlight how potential side effects or other barriers associated with treatment could potentially be avoided, and importantly how exercise/PA treatment can provide multiple holistic (i.e. mind and body) health benefits for mothers in the postpartum period. Positive findings would provide further growing support and recommendation for exercise and/or PA as an effective treatment in clinical postpartum populations. An initial secondary aim of this review was to identify the more effective exercise or PA intervention approaches. This would then help identify and recommend effective exercise or PA modalities and corresponding content for clinical and applied practice. From a research perspective, it would also begin to identify the avenues for where further examination and testing of intervention structure and content is required to increase the likelihood of effective intervention.
Materials and methods
Search strategy
Adhering to PRISMA guidelines (Moher, Liberati, Tetzlaff, Altman, and The PRISMA Group 2009), electronic database searches were performed using MEDLINE, CINAHL, Scopus, PsycInfo, EMBASE, Cochrane Library, Science Direct and Web of Science from earliest record to 1st of July 2016. The search strategy combined the following terms: ‘depression’ or ‘depressed’ or ‘clinically depressed’ or ‘major depression’ or ‘major depressive disorder’ or ‘depressive symptoms’ or ‘depressive episode’ AND ‘weight loss’ or ‘weight management’ or ‘weight control’ or ‘body mass index’, ‘body composition’ or ‘waist circumference’ or ‘body mass’ or ‘body image’ or ‘adiposity’ or ‘overweight’ or ‘obesity’ or ‘body weight’ or ‘body fat percentage’ or ‘fat mass’ AND ‘exercise’ or ‘aerobic exercise’ or ‘resistance training’ or ‘exercise intervention’ or ‘exercise program’ or ‘structured training’ or ‘exercise training’ or ‘progressive resistance training’ or ‘weight lifting’ or ‘muscle strengthening’ or ‘weight training’ or ‘physical activity’ or ‘walking’ or ‘pram walking’ or ‘pedometers’ or ‘step counts’ or ‘incidental activity’ AND ‘postnatal’ or ‘postpartum’ or ‘postpartum period’ or ‘postnatal period’ or ‘post pregnancy’ or ‘after birth’ or ‘after pregnancy’.
Study eligibility criteria
Inclusion criteria applied for this review were as follows: (a) research published in English-language peer-reviewed journals, (b) unpublished work identified via bibliographic searches and manual searches using keywords, (c) examining postpartum women and who were diagnosed with postnatal depression, (d) randomised, non-randomised (experimental) or cohort studies, (e) interventions that included exercise or PA, (f) interventions lasting ≥4 weeks (i.e. to avoid identifying studies examining acute effects of exercise or PA), (g) women aged 18–55 and were 1 week to 24 months postpartum, (h) studies that assessed postnatal depression using a validated instrument and (i) studies that assessed body weight/composition (e.g. body mass index, body fat percentage). Editorial letters, commentaries, case studies and discussion/review articles were excluded. Interventions that used outdoor or adventure activities were also excluded, since their effects could be theoretically derived from factors independent to exercise or PA. Eligible studies were required to have reportedly examined the effect of exercise or PA on both quantitative measures of mental and physical health. To assist with identifying appropriate studies, ‘exercise’ was defined as any structured (e.g. systematically organised and supervised such as attending regular exercise sessions (e.g. resistance training under supervision) and repetitive physical activity that had the objective of improving or maintaining physical fitness (Caspersen et al. 1985). PA was defined as a bodily movement initiated by skeletal muscles that included movements ranging from low-high physical intensity and was not necessarily structured or with specific fitness outcomes (e.g. walking; Caspersen et al. 1985). These definitions were applied when defining the types of interventions in identified studies.
Data extraction
Following the systematic search, screening and identification of studies, inclusion was determined by two reviewers (MS and DH) who independently reviewed studies against eligibility criteria. When a study was identified as meeting criteria, it was confirmed via the second reviewer, and data extraction occurred using a standardised pre-constructed form. Data regarding participant characteristics (e.g. age and postpartum week), study design, intervention description and outcome measures were extracted and collated. After data extraction was complete, reviewers crosschecked data to confirm accuracy. Any discrepancies were discussed for consensus, with disagreements resolved by discussion with a third reviewer (SC). Reviewers were not blinded to names of authors, institutions or journal of publication. Study authors were contacted if additional information was required to complete data extraction adequately. The lead author of three studies was contacted using correspondence information, with necessary data returned in one case.
Study quality assessment
Methodological quality was assessed using the Downs and Black 27 item checklist (Downs and Black 1998). The tool assesses quality criteria such as a clear description of the aims, interventions, outcome measurements and participants, representativeness of groups, appropriateness of statistical analyses and correct reporting. The checklist was slightly modified so that the final item (number 27)—relating to statistical power—was scored consistently with other items (i.e. unable to determine = 0 and yes = 1). One extra item was added related to exercise or PA supervision; therefore, our tool consisted of 28 items (Table 1). Summed scores ranged from a possible 0 to 28 points, where scores >20 were considered ‘good study quality’, 11–20 moderate and <11 considered poor (Downs and Black 1998). Studies were independently rated by two reviewers (MS and DH) and checked for internal (intra-rater) consistency across items before score amalgamation. Disagreements between ratings were resolved via the third reviewer (SC).
Data analysis
Originally, it was intended that meta-analytical approaches would be conducted on extracted data. However, due to the limited number of studies identified and missing data within individual studies (and which was unavailable after follow-up), we were unable to conduct such meta-analytical steps. Nonetheless, where complete or partially data was available (e.g. pre-post intervention or control), individual study effect size estimates were generated using Hedge’s g (Hedges and Olkin 1985). Effect sizes were adapted and generically classified as small (−0.2), moderate (−0.5) and large (−0.8) based on Cohen’s (2013) recommendations.
Results
Study identification inclusion
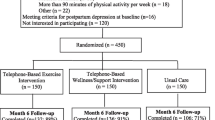
The systematic database search identified 10,134 potentially relevant studies, with two identified from manual searching. Following the removal of duplicates resulting from the database search, 8099 studies were initially screened based on reviewing study titles and abstracts when set against generic eligibility criteria. Screening removed 8039 of initially identified studies, leaving 60 studies for full review by two reviewers using eligibility criteria. Independent reviewing and consensus lead to the retainment of nine included articles. Figure 1 summarises the screening and selection process leading to a final list of included studies.
Characteristics of included studies
Table 2 provides an overview of studies meeting inclusion criteria. Eight studies were peer review publications and one was an unpublished thesis. Study designs included four RCTs, one randomised trial (no control group, but a different intervention), one randomised control pilot study, one cohort tracking and two quasi-experimental design studies. Five trials were conducted in the USA, with others conducted in Sweden, Canada, Greece and Taiwan. Seven studies used local community infrastructure for their study settings such as women and infant clinics, community centres, community health clinics, health fairs and postpartum classes. One study recruited participants through an out-patient clinic and implemented their intervention at a University fitness centre (Ko et al. 2012). Claesson et al. (2014) recruited via an ante-natal care clinic. Studies included a total of 975 participants.
Inclusion criteria within included studies
Inclusion criteria within studies were primarily based on postnatal stage. The earliest recruitment was from birth to 11 weeks postpartum (Claesson et al. 2014), 4 weeks (Dritsa et al. 2009) and 6 weeks (Keller et al. 2014; Ko et al. 2012; Lecheminant et al. 2014; Montgomery et al. 2007). In Albright et al. study, women were recruited from 8 weeks to 12 months postpartum. The latest recruitment onset was 30 weeks (7 months approx.) to 24 months postpartum (Krummel et al. 2010). In relation to age, only one study specified an age bracket (i.e. 18–40 years; Keller et al. 2014), while Krummel et al. (2010) stated an entry point of >18 years old with no upper age limit. In terms of PND eligibility criteria, included studies applied different cut-off scores based on the tool administered. Edinburgh Postnatal Depression Scale (EPDS) cut-off scores of 10 or greater were specified by Claesson et al. (2014), Albright et al. (2012) and Dritsa et al. (2009). Ko et al. used a cut-off of 15 on the Center for Epidemiological Studies Depression Scale (CES-D) questionnaire, while Lecheminant et al. (2014) did not specify. Keller et al. (2014) used EPDS a total score ≥ 12 and scores ≥16 to indicate major depression. Krummel et al. (2010) and Montgomery et al. (2007) incorporated the Beck Depression Inventory (BDI) scale, but did not specify the cut-off score. Seven studies stipulated recruitment of postnatally depressed women without any other health comorbidities and complications (Claesson et al. 2014; Dritsa et al. 2009; Ko et al. 2012; Krummel et al. 2010; Lecheminant et al. 2014; Montgomery et al. 2007; Zourladani and Tsaloglidou 2011), while two studies specified being sedentary as an additional criteria (Albright et al. 2012; Keller et al. 2014).
Five studies reported inclusion criteria for BMI. Keller et al. (2014) examined only overweight and obese women with BMIs of ≥25.0 and ≥30.0 kg/m2, respectively. Similarly, Claesson et al. (2014) included women with BMI ≥30.0 kg/m2; Lecheminant et al. (2014) included women with a weight > 2.27 kg above their self-reported pre-pregnancy weight. Montgomery et al. (2007) included women who had a BMI of ≥1.0 above self-reported pre-pregnancy and BMI of ≥24 kg/m2. Krummel et al. (2010) permitted eligibility as long as women were not underweight. Albright et al. (2012) included women with BMIs between 18.5 and 40 kg/m2, while three studies had no BMI criteria (i.e. Dritsa et al. 2009; Zourladani and Tsaloglidou 2011; Ko et al. 2012).
PND assessment
Research teams completed the assessment of PND symptoms across all included studies. Four studies utilised the EPDS (Cox et al. 1987) to assess symptom severity (Dritsa et al. 2009; Albright et al. 2012; Keller et al. 2014; Claesson et al. 2014). Two studies (i.e. Ko et al. 2012; Lecheminant et al. 2014) screened participants using the CES-D (Radloff 1997) and two (i.e. Montgomery et al. 2007; Krummel et al. 2010) used the BDI (Beck et al. 1996). Zourladani and Tsaloglidou (2011) used the Lederman postpartum self-evaluation questionnaire (LPSQ—Lederman et al. 1981) to assess women’s psychological well-being, asserting that changes in well-being could be associated with reductions in depression and stress symptoms (Barlow and Coren 2004). Assessing changes in PND symptom scores were the primary outcomes in six studies (Montgomery et al. 2007; Ko et al. 2012; Keller et al. 2014; Albright et al. 2012; Claesson et al. 2014; Lecheminant et al. 2014).
Body composition assessment
In terms of body composition, research teams often completed assessment, and appropriate referral to clinicians was made where dual-energy X-ray absorptiometry (DXA) was used. While BMI was the standard body composition indicator, other measures were also used. Body fat percentage was assessed in four studies (Ko et al. 2012; Krummel et al. 2010; Keller et al. 2014; Lecheminant et al. 2014) using bioelectric impedance (BIA, Keller et al. 2014), body composition analyser machine (a digital scale that allows measurement of participants’ weight, fat percentage, lean body mass and total body water—Ko et al. 2012) or DXA (Lecheminant et al. 2014) methods. Three studies assessed waist, hip circumference and waist-hip ratio (Montgomery et al. 2007; Krummel et al. 2010; Keller et al. 2014).
Additional outcomes
Included studies also examined several secondary (often psychological) outcomes. Two studies examined changes in self-efficacy (Albright et al. 2012; Lecheminant et al. 2014), social support (i.e. Dritsa et al. 2009; Albright et al. 2012) and perceived stress (Dritsa et al. 2009; Krummel et al. 2010). Stress was considered as a possible mediator to body composition change (Krummel et al. 2010). Two studies examined changes in postpartum fatigue (i.e. Dritsa et al. 2009; Ko et al. 2012). Further, individual studies examined changes in anxiety symptom severity (Claesson et al. 2014), perceived barriers and benefits of PA (Albright et al. 2012) and sleep quality (Dritsa et al. 2009) via questionnaires.
Exercise or PA interventions (modality, session frequency/durations, intensity and intervention duration)
Refer to Table 2 for a summary of intervention characteristics in included studies. Exercise modality varied though walking was implemented in four studies (Montgomery et al. 2007; Krummel et al. 2010; Albright et al. 2012; Keller et al. 2014). Within walking studies, interventions differed in structure and format ranging from prescribed 30–150 min/week for 12 weeks (Keller et al. 2014) to the targeted attainment of 10,000 steps/day for 7 days/week over 18 months (Albright et al. 2012). Krummel et al. (2010) also assigned the goal of 10,000 steps/day with progression to 12,000 steps/day over a year. Meanwhile, Montgomery et al. (2007) targeted an increase in the average number of steps by 500 steps/week to reach 5000 steps across 12 weeks, while Claesson et al. (2014) implemented an unsupervised postpartum PA intervention, stipulating that any form of PA could be undertaken with the requirement of at least 30 min/day, three times per week, over 11 weeks with intensity matching that of brisk walking. To note, Claesson et al. intervention was a part of a longer-term ante-postnatal cohort tracking study.
Using other exercise and PA modalities, one study compared resistance training (RT) relative to flexibility and static stretching (Lecheminant et al. 2014) across 18 weeks. The RT intervention was progressive, including nine exercises for all main muscle groups, performed for between 1 and 3 sets, with 8–12 repetitions/set on two non-consecutive days/week. During the first month, all training sessions were supervised by a trained instructor. From 2 to 4 months, only one session per week was monitored. By contrast, Dritsa et al. (2009) implemented a home-based aerobic exercise intervention for 60–120 min/week for 12 weeks at an intensity of 60–85% of maximal heart rate, under the supervision of an exercise physiologist, adhering to ACSM guidelines (ACSM 1998). Zourladani and Tsaloglidou (2011) implemented a multi-component low impact aerobic strengthening and stretching intervention relative to a no training group for 12 weeks. In group sessions under supervision, the intervention contained 20–25 min/session of aerobic exercises (e.g. low impact exercises and dance) along with 15–20 min of muscle strengthening exercises (e.g. upper and lower back, abdominal muscles and pelvic floor) with repetitions and sets increasing progressively. Training sessions were followed by 10 min/session of yoga and stretching. Finally, Ko et al. (2012) trialled yoga and pilates. Their intervention was group based and led by an instructor with sessions delivered once per week for 60 min duration over 12 weeks.
Intervention support strategies
Six studies reported on the provision of supplementary support strategies to accompany exercise/PA interventions. Related to walking interventions, a range of strategies were apparent though phone call follow-up and counselling were common. For instance, Albright et al. (2012) provided telephone PA counselling by counsellers trained in motivational interviewing to help problem-solve and maintain PA activity in their 10,000 steps/day intervention. By comparison, the control group recived only online resources specifying the benefits of PA. In Keller et al. (2014) intervention, group walking was impliclty intended as a social support strategy alongside provision of goal-setting and social support from community health advisors. Whereas the control group received more normative social support via a weekly telephone call focusing only on mothers postpartum and newborn concerns, within Krummel et al. (2010) 1-year walking intervention, multi-facted lifestyle behaviour change counselling (psychological and dietary advice) was incorporated as part of facilitated discussion groups. Further, monthly personalised feedback on PA behaviours and dietary behaviours were provided. At the same time, controls received only one session of dietary counselling and received a monthly newsletter. To support Montgomery et al. (2007) 12-week walking study, an activity calendar for logging walking actvity was provided, alongside a prompt reminder sheet and music CD for use while walking. A motivational letter was sent in weeks 4 and 8. Researchers contacted participants by phone or e-mail bi-weekly.
In the non-walking studies, Claesson et al. (2014) intervention participants received one-one midwife educational and weight management counselling for 30-min session during pregnancy (up to potentially 22 visits) and were invited to partake in acqua-aerobic classess prior to the postpartum PA phase of the study. In the postpartum PA phase, where self-chosen PA activity occurred, participans kept a PA diary to register all activity and maintained contact with the midwife and researcher team. Finally, in Dritsa et al. (2009) aerobic exercise, several supplementary support strategies were outlined. Support included an initial fitness assessment and feedback, provision of educational infromation (i.e. benefits from exercise) and periodic supervised exercise sessions with an exercise physiologists across their 12-week intervention.
Intervention adherence
All studies—bar one (Albright et al. 2012)—reported some form of adherence related or withdrawal information. Interventions associated with higher adherence rates (in order) were Montgomery et al. (2007) 12-week walking intervention with various support strategies (i.e. 100% adherence); Claesson et al. (2014) postnatal phase self-chosen physical activity intervention (98.6% intervention vs 88.6% control); Zourladani and Tsaloglidou (2011) local community, group-based, supervised aerobic strengthning intervention (91% approx); Ko et al. (2012) outpatient clinic, supervised and structured yoga and pilate intervention (82% approx); and Dritsa et al. (2009) home-based individualised aerobic exercise interventions with periodic supervised support (76.1%). Studies associated with lower adherence were Krummel et al. (2010) 1-year daily walking (10,000/day) intervention (42.3% estimated) and Keller et al.’s (2014) social group walking (54.9% intervention vs 77.9% control) with sedentary and overweight/obese participants.
Concurrent treatment
Across all nine included studies, participants either did not receive conucrrent parrallel treatements (e.g. medication and counselling) or studies did report that such treatments were occurring concurrently alongside exercise/PA interventions. This possibly changes that a potential changes from exercise/PA were not (or less) confounded by other ongoing parrallel treatments.
Exercise and PA assessment measures
Seven studies implemented different strategies to monitor exercise or PA levels and intervention compliance. In the walking interventions, PA measures included the use of either the Lifecorder EX New Lifestyles NL-2200 or Actigraph GT1M accelerometers (Albright et al. 2012; Keller et al. 2014 Lecheminant et al. 2014) or the Yamax SW-200 or Yamax Omron HJ-720ITC pedometer (Montgomery et al. 2007; Krummel et al. 2010; Keller et al. 2014). Heart rate monitors and self-report PA questionnaires (Dritsa et al. 2009; Albright et al. 2012; Keller et al. 2014) and exercise log (Krummel et al. 2010; Albright et al. 2012) were other means of PA measurement. In Claesson et al. (2014) study, self-report measures were used with subsequent metabolic equivalent conversions applied to estimate PA intensity.
Psychological and physiological outcomes
Results from exercise and PA interventions were inconsistent and varied, indicating either a favourable change in both outcomes, a change in one outcome measure or otherwise no change. For instance, in the supervised walking interventions, Keller et al. (2014) did not identify a group × time interaction, but did identify decreases in both outcomes from baseline to 12 months with effect size estimates for PND symptoms and BMI change being, respectively, small (depression g = −0.10; BMI g = −0.10). In Claesson et al. (2014) 11-week unsupervised PA intervention, no decrease in PND was evident (−3.8 ± 3.4; p < 0.059; g could not be estimated) and neither in BMI (p = 0.21). In Montgomery et al. (2007) 12 weeks of unsupervised walking (without a control/comparison group), there were no changes in PND score (p = 0.20), but significant changes to BMI (0.82 ± 0.93 kg/m2; p < 0.001) with a small effect size (g = −0.11). In Krummel et al. (2010) 12-month RCT of nutrition and unsupervised walking, no significant changes in depression or BMI score were apparent. Finally, based on their 18-month RCT of unsupervised moderate-vigorous walking every day, Albright et al. (2012) reported no difference in PND from baseline to 12 months, and BMI change pre-post intervention was not reported.
In other exercise modalities, only Ko et al. (2012) 12-week yoga and pilates single cohort intervention reported a significant reduction in both PND-associated scores (−5.76 ± 2.74; p = 0.021) with a small-moderate effect (intervention group g = −0.29) and BMI (0.31 ± 0.04 kg/m2; p < 0.001; intervention group g = −0.23). Meanwhile, in Zourladani and Tsaloglidou (2011) 12-week RCT of supervised aerobic strengthening and stretching, findings identified significantly improved psychological well-being pre-post intervention relative to controls (p < 0.05; g could not be estimated), but no changes in BMI (p = 0.66). Similarly, in Dritsa et al. (2009) 12-week RCT of supervised home-based exercise, depression symptoms significantly improved pre-post intervention relative to controls (−5.16 ± 3.67; p = 0.01), with a notably strong effect size (g = −0.86). Authors noted that women with higher initial PND symptoms improved more pre-post intervention. The analysis of BMI data was not reported and could not be obtained after author follow-up. Finally, in Lecheminant et al. (2014) 18-week intervention of supervised RT versus FT, significantly reduced pre-post PND scores (p = 0.01) with a small-moderate effect (g = −0.37) and body composition (p = 0.18; g = −0.04) from baseline to 4 months were identified. However, PND symptom changes were not significant between groups (p ≥ 0.05) with RT and FT groups both improving pre-post intervention (FT depression g = −0.10; BMI g = −0.16). To note, authors reported that in the RT group, 88% of participants were classified as ‘no longer depressed’ at post-intervention stage compared with 50% in the FT group.
Discussion and conclusion
The purpose of this systematic review was primarily to determine the effectiveness of exercise or PA interventions on PND and weight loss simultaneously. A secondary aim was to identify the more effective intervention approaches and accompanying support strategies that could be recommended as part of clinical treatment practice. Based on the limited number of presently available and included studies—though some with high study quality ratings containing RCT research designs—overall findings suggest inconsistency and sporadic cases of (non-)support as to whether exercise or PA were effective in simultaneously reducing both PND-associated symptoms and weight loss (as often reflected by body composition indices). Of the identified studies, two (22.2%) identified significant changes in both targeted outcomes with small effect sizes (i.e. Ko et al. 2012; Keller et al. 2014). Four studies (44.4%) reported changes in one outcome variable, typically associated with PND outcomes and with variable effect sizes, while three studies (33.3%) either reported no effect or did not report the outcome (Claesson et al. 2014; Albright et al. 2012; Krummel et al. 2010).
Related to our secondary aim, the identification of more effective interventions is constrained by several factors. These include the diversity and content or exercise/PA interventions implemented to date; the range of delivery and support strategies adopted; the measurement procedures used to assess PND (or components of) and weight (or body composition), as well as the inconsistent outcomes achieved in respective interventions. Nevertheless, insight and ‘lessons learned’ can still be extrapolated from examination of existing studies, particularly with reference to those deploying higher quality research design, who achieved PND and/or weight loss changes with higher effect magnitudes, and who maintained higher degrees of adherence relative to other studies. Supervised (1–1, group or combination), structured (i.e. with weekly frequency, scheduled durations, moderate intensity) exercise or PA interventions which adhered to specific exercise/PA guidelines over an extended postpartum period (e.g. 12 weeks +), and which were supplemented by support strategies are predictably most likely to associate with meaningful PND and/or weight loss changes (e.g. Dritsa et al. 2009; Lecheminant et al. 2014). For instance, Dritsa et al. (2009) 12-week RCT of supervised home-based exercise with one-one periodic trained supervision adhered to specific aerobic cardio-respiratory exercise guidelines and lead to a strong effect outcome in terms of PND symptom reduction (g = −0.86; post-intervention body composition data was not reported). With specific reference to weight loss, interventions were generally less successful, and where present, effect size magnitudes were small. Studies with structured supervised lower intensity exercise (Ko et al. 2012) and walking interventions with objective measurements did identify changes (e.g. Montgomery et al. 2007; Keller et al. 2014), whereas unsupervised, non-objectively tracked and lesser adherent interventions did not (e.g. Claesson et al. 2014; Krummel et al. 2010; Albright et al. 2012). Still, it remains possible that a variety of other participant, intervention and methodological reasons could also potentially account for such outcomes.
Based on available evidence, alternative regimens of intervention content such as moderate-lower intensity interventions may also be beneficial, feasible and preferential. For instance for women with lesser exercise/PA experience, those whose PND symptoms are more severe and affecting cognitive functioning, women with sedentary, overweight and obese characteristics or those whose movement capabilities may be constrained in the immediate weeks postpartum, alternate modalities and intensities could prove helpful in exercise/PA initiation stages. Such a proposition is supported when considering findings from Zourladani and Tsaloglidou (2011) 12-week RCT of supervised group-based aerobic strengthening and stretching (50–60 min × 3 days/week) as well as Ko et al. (2012) 12-week instructed yoga and pilates classes. In both cases, self-reported psychological health and PND symptoms improved, respectively, with BMI also improving from Ko et al. (2012) yoga and pilates. Whether more or less intensive exercise is deployed, the accompanying support strategies to promote adherence and increase the likelihood of health benefits remain important. Guided by present studies, local community provision, opportunities for peer or group social interaction as well as frequent tracking and follow-up by researchers and practitioners (e.g. community nurse, midwife, counsellors, exercise instructors, physiologists and psychologists) in a supportive psycho-social environments can be recommended as accompanying intervention support strategies.
Linked to our observations in more effective interventions, existing literature and public health organisation do specifically recommend exercise programs, particularly to promote positive changes in body composition and associated cardio-metabolic benefits for at risk overweight and obese adults. For instance, the current American College of Sports Medicine (ACSM) recommendations (Donnelly et al. 2009) state that aerobic exercise programs need to exceed 225 min/week to induce clinically significant weight loss (≥5% of baseline body weight) (Lavie et al. 2009). Further, by increasing PA to ≥10,000 steps/day is indicative of an active lifestyle (Swift et al. 2014). However, in general, these tend to result in very modest weight loss (<2 kg) (Tudor-Locke and Bassett 2004). Therefore, the varied and small effect size results for weight loss from our included studies are likely most explained by differences in volumes and intensities in aerobic exercise/PA and objectively measured adherence to these schedules. For psychological benefits, including depression, a similar volume of aerobic exercise is recommended ≥150 min/week (Stanton and Reaburn 2014). Also, on this basis, it is difficult at present to discern whether weight loss following an exercise intervention plays a beneficial role toward treating PND. It has been reported that approximately 14–25% of women are at least 5 kg heavier 1 year following delivery (Gunderson and Abrams 1999; Schauberger et al. 1992), increasing their risk of cardio metabolic disease, mental health disease and premature mortality (Dye et al. 1997; Santos et al. 2007). Therefore, it is plausible that weight loss induced from an exercise intervention may positively affect depression symptoms via the improvement in self-perception, self-efficacy, body-image, and improved perceived quality of life/health (Clark et al. 2009; Xie et al. 2010). Driving these psychological changes via physiological change and capacity development may also be a helpful process in women’s postpartum health.
Limitations and future directions
Findings from the present review are limited by several study design, intervention characteristic, measurement and study reported features. These include the identification of few studies examining psychological and physiological outcomes simultaneously; the application of higher quality research designs; the inconsistency in application of diagnostic cut-off criteria to define PND severity; the variability in exercise/PA intervention content (including intensity management across intervention durations); the use of subjective exercise/PA for intervention tracking; variability in adherence and compliance; and potential confounding from participant characteristics (e.g. prior history of PND; baseline body weight, BMI and PA behaviour status); and potential parallel treatments or behaviour changes (e.g. medication, counselling, changes in dietary intake or behaviours). To accurately establish whether exercise or PA interventions do hold consistent simultaneous effects for PND and body weight specifically and women’s postpartum health more broadly, review findings highlight the need for high-quality well-controlled studies with consistent pre-post intervention reporting on targeted psychological and physiological indices. Studies examining supervised, structured, progressive aerobic and/or low-intensity exercise style modalities, with frequent sessions over an extended period (e.g. 10–12 weeks +), seem most pertinent and feasible based on current data.
In implementation, establishing consistent inclusion criteria, valid and reliable PND assessment and objective measurement instruments (e.g. PA tracking devices), and postpartum starting points (i.e. weeks post-birth) for intervention need to be considered. As depression and PND are associated with pre-existing depression episodes and severity along with multiple social and demographic risk factors, careful consideration of these potentially confounding factors is required. Related to confounding factors, it will be important to consider and incorporate the potential effects of concurrent treatments (e.g. exercise + counselling relative to a counselling alone group) to better isolate exercise/PA-associated effects. Likewise, screening for other related changes (e.g. dietary advice and social support) will need to be considered. Similarly, and specific to body composition characteristics (e.g. normative pre-birth weight, weight gain and loss across pregnancy and postpartum) need to be considered prior to intervention. Being able to delineate normative postnatal (pregnancy associated) weight loss from exercise/PA-induced weight will be important in determining the postpartum effect of exercise/PA. Finally, exercise or PA intervention adherence and compliance with exercise/PA session content also need to be reported to determine (i) whether exercise or PA can simultaneously effects women’s holistic health and (ii) whether the most effective, preferred and adherent approaches can be identified for clinincal practice.
Implications
Taken together, review findings suggest that a list of intricate (inter-relating) factors need to be carefully considered if generic exercise or PA interventions can be effectively utilised either as an adjunct treatment for postnatal depression or as a distinct stand-alone lifestyle behaviour for psychological and physiological health improvement in postpartum women. Exercise or PA interventions with supervision (1–1, group), structure (weekly frequency, scheduled durations, moderate intensity), which adhered to specific exercise/PA guidelines over an extended postpartum period (e.g. 12 weeks +) and were supplemented by several psycho-social support strategies (e.g. educational information, exercise/PA advice and counselling) could potentially provide most benefit. However, such targeting needs to be carefully balanced against physical mobility capabilities and health indicators at respective postpartum stages. Similarly, patient previous experience, psychological self-efficacy, perceived mobility capability and exercise/PA modality preferences are all factors that will affect exercise or PA uptake. Thus, striking a balance between these needs and implementing psycho-social strategies to support exercise/PA uptake and compliance remain important in practice when assisting women affect by PND and/or have body composition (e.g. weight) concerns.
Conclusion
Findings from this systematic review identify that exercise/PA interventions can positively effect PND symptoms and body composition (weight)-related indices. Change and higher effect size estimates were more associated with PND symptom reduction, while weight-loss was less consistent and only associated with small effect sizes (where evident). However, present evidence is limited and inconsistent. Supported by parallel evidence, exercise or PA interventions with supervision (i.e. 1–1, group or combination), structure (weekly frequency, scheduled durations, moderate intensity), which adhered to specific exercise/PA guidelines over an extended postpartum period (e.g. 12 weeks +) and were supplemented by several psycho-social support strategies (e.g. educational information, exercise/PA advice and counselling) are more likely to be more effective. To determine a more clear position, study weaknesses need to be addressed. Future studies need to consider inconsistencies in study inclusion criteria, participant characteristics and outcome measurement; examine exercise and PA interventions recommended (and more likely to benefit); implement known psycho-socail support strategies to support adherence and compliance; and assess potentially confounding factors (e.g. pregnancy associated weight gain, parallel treatments and potential dietary change). Likewise, considering how best exercise (or PA) can be delivered alongside existing clinical or local community provision (e.g. community midwife, nurse or health advisors) will evaluate whether exercise/PA interventions can be integrated into clinical practice to benefit women’s postpartum health.
References
Albright C, Steffen A, Novotny R, Nigg C, Wilkens L, Saiki K, Brown W (2012) Baseline results from Hawaii’s Na Mikimiki project: a physical activity intervention tailored to multi-ethnic postpartum women. Women Health 52:265–291
American College of Sports Medicine (1998) American college of sports medicine position stand. The recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness, and flexibility in healthy adults. Med Sci Sports Exerc 30:975–91
American Psychiatric Association (2013a) Cautionary statement for forensic use of DSM-5 in Diagnostic and Statistical Manual of Mental Disorders Washington, DC: America
American Psychiatric Association (2013b) Diagnostic and statistical manual of mental disorders. In: DSM-5, 5th edn. American Psychiatric Publishing, Arlington, p 2013
Asbee S, Jenkins T, Butler J, White J, Elliot M, Rutledge A (2009) Preventing excessive weight gain during pregnancy through dietary and lifestyle counseling: a randomized controlled trial. Obstet Gynecol 113(2):305–311
Barlow J, Coren E (2004) Parent-training programs for improving maternal psychosocial health. Cochrane Database Syst Rev 1:CD002020
Beck C (2001) Predictors of postpartum depression: an update. Nurs Res 50:275–285
Beck A, Steer R, Brown G (1996) Manual for the Beck depression Inventory-II. Psychological Corporation, San Antonio
Bridle C, Spanjers K, Patel S, Atherton N, Lamb S (2012) Effect of exercise on depression severity in older people: systematic review and meta-analysis of randomized controlled trials. Br J Psychiatry 201:180–185
Brüne M (2015) Textbook of evolutionary psychiatry and psychosomatic medicine, 2nd edn. Oxford University Press, Oxford
Caspersen C, Powell K, Christenson G (1985) Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep 100(2):126–131
Claesson M, Klein S, Sydsjö G, Josefsson A (2014) Physical activity and psychological well-being in obese pregnant and postpartum women attending a weight-gain restriction program. Midwifery 30(1):11–16
Clark A, Skouteris H, Wertheim E, Paxton S, Milgrom J (2009) The relationship between depression and body dissatisfaction across pregnancy and the postpartum: a prospective study. J Health Psychol 14:27–35
Cohen J (2013) Statistical power analysis for the behavioral Sciences. Book, whole. Elsevier, Burlington
Cooper P, Murray L (1995) Course and recurrence of postnatal depression. Evidence for the specificity of the diagnostic concept. Br J Psychiatry 166:191–195
Cox J, Holden J, Sagovsky R (1987) Detection of postnatal depression. Development of the 10-item Edinburgh postnatal depression scale. Br J Psychiatry 150:782–786
Craft L, Perna F (2004) The benefits of exercise for the clinically depressed. Prim Care Companion J Clin Psychiatry 6:104–111
Currie J, Develin E (2002) Stroll your way to well-being: a survey of the perceived benefits, barriers, community support and stigma associated with pram walking groups designed for new mothers Sydney. Health Care Women Int 23:882–893
Dennis C, Ross L (2005) Relationships among infant sleep patterns, maternal fatigue, and development of depressive symptomatology. Birth 32:187–193
Dennise C, Ross L, Grigoriadis S (2007) Psychosocial and psychological interventions for treating antenatal depression. Cochrane Database of Syst Rev 18(3):CD006309
Dietz P, Callaghan W, Morrow B (2005) Population-based assessment of the risk of primary cesarean delivery due to excess prepregnancy weight among nulliparous women delivering term infants. Matern Child Health J 9:237–244
Donnelly J, Blair S, Jakicic J, Manore M, Rankin J, Smith B (2009) American College of Sports Medicine position stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc 41(2):459–471
Doran F, Davis K (2011) Factors that influence physical activity for pregnant and postpartum women and implications for primary care. Aust J Prim Health 17(1):79–85
Downs S, Black N (1998) The feasibility of creating a checklist for the assessment of the methodological quality both of randomized and non-randomized studies of health care interventions. J Epidemiol Community Health 52:377–384
Dritsa M, Dupuis G, Lowensteyn I, Da Costa D (2009) Effects of home-based exercise on fatigue in postpartum depressed women: who is more likely to benefit and why? J Psychosom Res 67:159–163
Dye T, Knox K, Artal R, Aubry R, Wojtowycz M (1997) Physical activity, obesity, and diabetes in pregnancy. Am J Epidemiol 146(11):961–965
Endres LSH, Mckinney C, Plunkett B, Minkovitz C, Schetter C, Shalowitz M (2015) Postpartum weight retention risk factors and relationship to obesity at one year. Obstet Gynecol 125(1):144–152
Eninarson A (2009) Antidepressants and pregnancy: complexities of producing evidence-based information. CMAJ 182:1017–1018
Evenson K, Savitz D, Huston S (2004) Leisure-time physical activity among pregnant women in the US. Pediatr Perinat Epidemiol 18:400–407
Fjeldsoe B, Marshall A, Miller Y (2009) Behavior change interventions delivered by mobile telephone short-message service. Am J Prev Med 36:165–173
Grace S, Evindar A, Stewart D (2003) The effect of postpartum depression on child cognitive development and behavior: a review and critical analysis of literature. Arch Womens Ment Health 6:263–274
Gressier F, Guillard V, Cazas O, Falissard B, Glangeaud-Freudenthal NM-C, Sutter-Dallay A-L (2016) Risk factors for suicide attempt in pregnancy and the post-partum period in women with serious mental illnesses. J Psychiatr Res 84:284–291
Gunderson E, Abrams B (1999) Epidemiology of gestational weight gain and body weight changes after pregnancy. Epidemiol Rev 21(2):261–275
Haas J, Jackson R, Fuentes-Afflick E, Stewart A, Dean M, Brawarsky P, Escobar G (2005) Changes in the health status of women during and after pregnancy. J Gen Intern Med 20(1):41–45
Hagen E (1999) The functions of post-partum depression. Evol Hum Behav 20:325–359
Hay DF, Pawlby S, Angold A, Harold GT, & Sharp D (2003) Pathways to violence in the children of mothers who were depressed postpartum. Dev Psychol 39(6):1083–1094
Hedges L, Olkin I (1985) Statistical methods for data analysis. Academic Press, Orlando
Herring S, Rich-Edwards J, Oken E (2008) Association of postpartum depression with weight retention 1 year after childbirth. Obesity 16:1296–1301
Howard LM, Flach C, Mehay A, Sharp D, Tylee A (2011) The prevalence of suicidal ideation identified by the Edinburgh postnatal depression scale in postpartum women in primary care: findings from the RESPOND trial. BMC Pregnancy Childbirth 11(1):57
Jenkin W, Tiggermann M (1997) Psychological effects of weight retained after pregnancy. Women Health 25:89–98
Josefsson T, Lindwall M, Archer T (2014) Physical exercise intervention in depressive disorders: meta-analysis and systematic review. Scand J Med Sci Sports
Keller C, Ainsworth B, Records K, Todd M, Belyea M, Vega-López S, Nagle-Williams A (2014) A comparison of a social support physical activity intervention in weight management among post-partum Latinas. BMC Public Health 14:971
Kim D, O'Reardon J, Epperson C (2010) Guidelines for the management of depression during pregnancy. Curr Psychiatry Rep 12:279–281
Kim-Cohen J, Moffitt TE, Taylor A, Pawlby SJ, Caspi A (2005) Maternal depression and children’s antisocial behavior: nature and nurture effects. Arch Gen Psychiatry 62(2):173–181
Kirsch I, Deacon B, Huedo-Medina T, Scoboria A, Moore T, Johnson B (2008) Initial severity and antidepressant benefits: a meta-analysis of data submitted to the Food and Drug Administration. PLoS Med 5(2):e45
Ko Y, Yang C, Fang C, Lee M, Lin P (2012) Community-based postpartum exercise program. J Clin Nurs 22:2122–2131
Krummel D, Semmens E, MacBride A, Fisher B (2010) Lessons learned from the Mothers’ overweight management study in 4 West Virginia WIC offices. J Nutr Educ Behav 42:S52–S58
LaCoursiere Y, Baksh L, Bloebaum L, Vamer M (2006) Maternal body mass index and self-reported postpartum depressive symptoms. Matern Child Health J 10:385–390
Lavie C, Milani R, Ventura H (2009) Obesity and cardiovascular disease: risk factor, paradox, and impact of weight loss. J Am Coll Cardiol 53(21):1925–1932
Lecheminant J, Hinman T, Pratt K, Earl N, Bailey B, Thackeray R (2014) Effect of resistance training on body composition, self-efficacy, depression, and activity in postpartum women. Scand J Med Sci Sports 24(4):414–421
Lederman R, Toussie-Weingarten C, Lederman E (1981) Postpartum self-evaluation questionnaire: measures of maternal adaptation. Birth Defects Orig Artic Ser 17:201–231
Lindahl V, Pearson J, Colpe L (2005) Prevalence of suicidality during pregnancy and the postpartum. Arch Womens Ment Health 8(2):77–78
Luoto R, Kinnunen T, Aittasalo M, Ojala K, Mansikkamäki K, Toropainen E, Vasankari T (2010) Prevention of gestational diabetes: design of a cluster-randomized controlled trial and one-year follow-up. BMC Pregnancy Childbirth 10(1):39
Luppino F, De Wit L, Bouvy P, Stijnen T, Cuijpers P, Penninx B, Zitman F (2010) Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry 67(3):220–229
Marcus S, Flynn H, Blow F, Barry K (2003) Depressive symptoms among pregnant women screened in obestetrics settings. J Women's Health 12(4):373–380
May A (1995) Using exercise to tackle postnatal depression. Health Visit 68:146–147
Meades R, Ayers S (2011) Anxiety measures validated in perinatal populations: a systematic review. J Affect Disord 133:1–15
Milgrom J, Schembri C, Ericksen J, Ross J, Gemmill A (2011) Towards parenthood: an antenatal intervention to reduce depression, anxiety and parenting difficulties. J Affect Disord 138:385–394
Moher D, Liberati A, Tetzlaff J, Altman D, The PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097
Moncrieff J, Kirsch I (2005) Efficacy of antidepressants in adults. Brit Med J 331:155–157
Montgomery V, Grandjean P, Jackson E, Chapple B, Blessing D, Williford H, Flowers G (2007) The influence of increased physical activity on weight retention, body composition, psychological profiles, and cardiovascular function in postpartum African American women (doctor of philosophy). Auburn University, Auburn
Mottola M (2002) Exercise in the postpartum period: practical applications. Curr Sports Med Rep 1:362–368
Murray L, Sinclair D, Cooper P, Ducournau P, Turner P, Stein A (1999) The socioemotional development of 5-year-old children of postnatally depressed mothers. J Child Psychol Psychiatry 40(8):1259–1271
Muzik M, Marcus S, Heringhausen J, Flynn H (2009) When depression complicates childbearing: guidelines for screening and treatment during antenatal and postpartum obstetric care. Obstet Gynecol Clin N Am 36:771–788
Nagl M (2015) Obesity and anxiety during pregnancy and postpartum: a systematic review. J Affect Disord 186:293–305
Norman E, Sherburn M, Osborne R, Galea M (2010) An exercise and education program improves well-being of new mothers: a randomized controlled trial. Phys Ther 90(3):348–355
O'Hara M, Swain A (1996) Rates and risk of postpartum depression-a meta-analysis. Int Rev Psychiatry 8(1):37–54
Peterson K, Sorensen G, Pearson M, Hebert J, Gottlieb B, McCormick M (2002) Design of an intervention addressing multiple levels of influence on dietary and activity patterns of low-income, postpartum women. Health Educ Res 17:531–540
Radloff L (1997) The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1:385–401
Robertson ESG, Wallington T, Stewart D (2004) Antenatal risk factors for postpartum depression: a synthesis of recent literature. Gen Hosp Psychiatry 26:289–295
Rooney B, Schauberger C (2002) Excess pregnancy weight gain and long-term obesity: one decade later. Obstet Gynecol 100(2):245–252
Santos M, Steven Richards C, Kathryn Bleckley M (2007) Comorbidity between depression and disordered eating in adolescents. Eat Behav 8(4):440–449
Schauberger C, Rooney B, Brimer L (1992) Factors that influence weight loss in the puerperium. Obstet Gynecol 79(3):424–429
Schmitt N, Nicholson W, Schmitt J (2007) The association of pregnancy and the development of obesity - results of a systematic review and meta-analysis on the natural history of postpartum weight retention. Int J Obes 31:1642–1651
Schoenborn C, Adams P, Peregoy J (2013) Health behaviors of adults: United States, 2008–2010. National Center for Health Statistics. Vital Health Stat 10(257)
Silveira M, Ertel K, Dole N, Chasan-Taber L (2015) The role of body image in prenatal and postpartum depression: a critical review of the literature. Arch Womens Ment Health 18(3):409–421
Stanton R, Reaburn P (2014) Exercise and the treatment of depression: a review of the exercise program variables. J Sci Med Sport 17(2):177–182
Swift D, Johannsen N, Lavie C, Earnest C, Church T (2014) The role of exercise and physical activity in weight loss and maintenance. Prog Cardiovasc Dis 56(4):441–447
Thornhill R, Furlow B (1998) Stress and human reproductive behavior: attractiveness, women's sexual development, postpartum depression and baby's cry. Adv Study Behav 27(319–369)
Tracey M (2005) Evolutionary perspective. Nebraska Anthropologist 20
Tudor-Locke C, Bassett DR (2004) How many steps/day are enough? Preliminary pedometer indices for public health. Sports Med 34:1–8
Vernon M, Young-Hyman D, Looney S (2010) Maternal stress, physical activity, and body mass index during new mothers’ first year postpartum. Women Health 50:544–562
Walker L (2007) Managing excessive weight gain during pregnancy and the postpartum period. Obstet Gynecol Neonatal Nurs 36:490–500
Wilkinson J, Philips S, Jackson J, Walker K (2003) “mad for fitness”: an exercise group of combat a high incidence of postnatal depression. J Fam Health Care 13:44–48
Xie B, Unger J, Gallaher C, Johnson C, Wu Q, Chou C (2010) Overweight, body image, and depression in asian and hispanic adolescents. Am J Health Behav 34(4):466–478
Zourladani A, Tsaloglidou A (2011) Low impact exercise and well-being in Greek postpartum women international. Sport Med J 12:30–38
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study did not receive any funding.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors.
Informed consent: not Applicable to this study due to being a systematic review.
Conflict of interest
There are no potential conflicts of interest with respect to the research conducted, authorship and/or potential publication of this article. The authors also declare no receipt of financial support in conducting the study. Maryam Saligheh declares that she has no conflict of interest. Daniel Hackett declares that he has no conflict of interest. Philip Boyce declares that he has no conflict of interest. Stephen Cobley declares that he has no conflict of interest.
Rights and permissions
About this article
Cite this article
Saligheh, M., Hackett, D., Boyce, P. et al. Can exercise or physical activity help improve postnatal depression and weight loss? A systematic review. Arch Womens Ment Health 20, 595–611 (2017). https://doi.org/10.1007/s00737-017-0750-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00737-017-0750-9