Abstract
The Postpartum Bonding Questionnaire (PBQ) was developed to assess mother-infant bonding disturbances in the postpartum period. The aim of this study was to examine the psychometric properties of the Spanish version of the PBQ in a sample of Spanish postpartum women. Eight hundred forty mothers were recruited in the postpartum visit (4–6 weeks after delivery): 513 from a gynecology unit (forming the general population sample) and 327 mothers from a perinatal psychiatry program (forming the clinical sample). All women were assessed by means of the Edinburgh Postnatal Depression Scale (EPDS) and the PBQ. Neither the original four-factor structure nor alternative structures (Reck et al. 2006; Wittkowski et al. 2010) were replicated by the confirmatory factor analyses. An exploratory factor analysis showed a four-factor solution. The Schmid-Leiman transformation found a general factor that accounted for 61 % of the variance of the PBQ. Bonding impairment showed higher associations with depressive symptomatology in both samples. The Spanish version of the PBQ showed adequate psychometric properties for use with clinical and general populations of Spanish postpartum women. The results suggest that the PBQ could be summarized by a general factor and confirm the utility of the use of the total score for detecting bonding impairment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
One of the most important processes in the postpartum period is the development of mother-infant bonding (Brockington 2004, 2011). Taylor uses the term “bonding” to describe how the mother feels towards her infant. The term refers to the unique emotional tie between the mother and her infant and is characterized by positive feelings, emotional warmth, and affection towards the child (Taylor et al. 2005); it differs from attachment, which includes the infant’s behavior towards the mother (Taylor et al. 2005; Tietz et al. 2014). This relationship is particularly relevant because much of the growth and maturation of the human brain is postponed until the postpartum period; the brain must develop in a social environment focused initially on the primary caregiver, usually the mother (Broad et al. 2006). The mother-infant bond provides an attachment figure for the baby, which will be the basis for future social ties (Yarrow 1972) and keep the baby protected and safe—a fundamental parental function for child survival (Bowlby 1982). Mäntymaa suggests that good-quality mother-infant interaction behavior facilitates the infant’s later socio-emotional, behavioral, and cognitive development and is even related to the child’s physical health (Mäntymaa 2006, cited by Korja et al. 2012). Disruption of mother-infant bonding affects the infant neurobehavioral development; in animal models, it has demonstrated long-lasting effects on socio-emotional behaviors such as anxiety-like and maternal behaviors (Mogi et al. 2011). Fonagy stressed the importance of the parent-infant relationship for the emergence of mentalizing (imaginative mental activity, namely, perceiving and interpreting human behavior), a capacity with a social-cognitive basis (Fonagy et al. 2012). Consequently, it is widely accepted that early impaired bonding is a risk factor for infant development.
In recent years, specific instruments have been developed and validated to detect and prevent bonding disorders. Among the most useful and frequently applied assessment strategies are the self-administered scales that allow an evaluation of mothers’ emotional responses to their babies (Taylor et al. 2005). These instruments include the Maternal Postpartum Attachment Scale (MPAS: Condon and Corkindale 1998), the Postpartum Bonding Questionnaire (PBQ: Brockington et al. 2001), the Mother-to-Infant Bonding Scale (MIBS) (Taylor et al. 2005), and Zeanah’s Working Model of the Child Interview (Zeanah and Benoit 1995). There are also confirmatory interviews such as The Yale Inventory of Parent Thoughts and Actions (YIPTA: Leckman et al. 1994) and The Birmingham Interview for Maternal Mental Health (BIMMH: Brockington et al. 2006b). Validation of instruments measuring mother-child bonding disorders in different countries facilitates detection and early intervention, and also the comparison of results between studies.
Of the existing instruments, we have focused on the PBQ (Brockington et al. 2001), for several reasons. This reliable, validated tool is widely used in a number of countries for identifying problems in the mother-infant relationship during the postpartum period. It is based on clinical experience and is very easy to apply. The PBQ was designed in the UK by Brockington and colleagues in 2001. Originally composed of 84 items, the final version of the instrument has 25. It is designed to investigate mothers’ feelings about their babies and their recent postpartum experience. The items measure the frequency of maternal feeling scored on a 6-point scale from 0 to 5 with six options: “always,” “very often,” “quite often,” “sometimes,” “rarely,” and “never”. The final 25 items were selected from a factor analysis with orthogonal varimax rotation from the combined 84 items. The four final scales were responsible for 50 % of the variance: scale 1, a general factor termed impaired bonding (34 % of the variance) consisted of 12 items; scale 2, rejection and anger (8 % of the variance) comprised seven items; scale 3, anxiety about care (3.7 % of the variance) comprised four; and scale 4, risk of abuse (3.4 % of the variance) consisted of two. Brockington and colleagues conducted two studies validating the PBQ (Brockington et al. 2001, 2006c). In 2001, 104 mothers were recruited from various sources, including general populations from maternity clinics, mothers with babies with some abnormality, high-risk pregnancies, mothers with a depressive disorder but with a normal mother-infant relationship, and mothers with a bonding disorder. Fifty-one of these mothers were interviewed using as a gold standard the third edition of the structured interview for pregnancy-associated disorders (which later became the BIMMH), in order to diagnose the existence of bonding disorders and to determine cutoff scores. The cutoff scores used for each scale were the following: scale 1 > 12, scale 2 > 16, scale 3 > 9, and scale 4 > 2. In the 2006 study, 125 mothers were recruited from other specialists and all showed some type of mother-infant bond disorder and other comorbid mental disorders (depression, anxiety, post-traumatic stress disorder, and obsessive). All mothers were interviewed using the fifth edition of the BIMMH. As a result of this second validation, the authors suggested adjusting the cutoff points of scale 2, >12, and scale 4 > 1. In addition, the total score ranged from 0 to 125. A general cutoff score of 26 was proposed to identify “any type of bonding disorder” and a cutoff ≥40 to identify severe disturbances.
Since its publication, the instrument has been used in other locations (Edhborg et al. 2005; Muzik et al. 2013) and so far has been translated and validated in Germany (Reck et al. 2006), China (Siu et al. 2010), Belgium (van Bussel et al. 2010) and used to validate other instruments related to the assessment of maternal-infant relationships (Wittkowski et al. 2007; van Bussel et al. 2010; Høivik et al. 2013). However, later validation studies have not been able to replicate its factor structure (Reck et al. 2006; Wittkowski et al. 2010). Reck et al. (2006) carried out a factor analysis obtaining a one-factor model and a new 16-item version, most of which loaded on the general factor of “Impaired bonding.” Wittkowski et al. (2010) removed items from scale 4 and found a new structure with three factors, partially related to Brockington’s first, second, and third factors, although the assignment of items to each factor was slightly different.
The PBQ has proven to be useful in several clinical populations such as mothers suffering from depression (Hornstein et al. 2006; Moehler et al. 2006; Noorlander et al. 2008) or post-traumatic stress disorder (PTSD) (Ayers et al. 2007; Parfitt and Ayers 2009). PTSD has a negative effect on parental bonding (Parfitt and Ayers 2009), and depression in the early postnatal period has shown long-term effects in the mother-infant bonding process (Moehler et al. 2006). Depressive mothers perceive their bonding to the infant more negatively than mothers suffering of psychosis (Hornstein et al. 2006; Noorlander et al. 2008). Interestingly, in contrast to women with postpartum psychosis, the subjective experience of bonding in depressed women correlates with the observation of mother-infant interaction (Noorlander et al. 2008). This finding reinforces the use of both subjective measures of bonding and objective measures of mother-infant interaction.
Due to the need to assess these disorders in Perinatal Mental Health Programs in Spain, it is essential to have valid, reliable tools to evaluate mother-infant bonding disorders in the Spanish population. At present, there is no Spanish-language instrument for identifying problems in the mother-infant relationship during postpartum which can guide early diagnosis and treatment or can be used in the investigation of the factors associated with this disorder. The present study was conducted with the aim of assessing the psychometric properties of the Spanish version of the PBQ in a sample of Spanish women during postpartum period.
Method
Participants and procedure
Participants were 840 mothers recruited in the postpartum visit (4–6 weeks postpartum), over a 5-year period (2008–2013). A sample of mothers was recruited from the general population (n = 513) attended at a gynecology unit, and a clinical sample (n = 327) comprising mothers enrolled on a perinatal psychiatry program treated for a psychiatric disorder during their pregnancy or in the postpartum period.
The mean age of the mothers was 34 years (SD = 4.5; range 18–50). The majority (98 %) had a partner at the time of the evaluation. The average number of children per mother was 1.5; primiparous women represented the largest group (58.2 %), followed by mothers with two children (35.3 %) and those with three children (5.8 %). The entire range was one to five children. Some form of assisted reproduction had been required in 12.1 % of the mothers. Clinical sample mothers, when compared with the general population sample, had more children (1.7 ± 0.79 vs. 1.5 ± 0.66; t[477.6] = 4.22, p < 0.001) and had more frequently no partner at the time of the evaluation (4.7 vs. 1 %; p < 0.01, Fisher’s exact test). Mothers from the general population required some form of assisted reproduction more frequently than clinical sample mothers (15.7 vs. 4.6 %; p < 0.001, Fisher’s exact test). There were no differences between the samples in mean age.
Approval was obtained from the institutional review board, and all women provided written informed consent before entering the study. Once enrolled, at the postpartum visit (between 4 and 6 weeks postpartum), the Edinburgh Postnatal Depression Scale (EPDS) was administered to assess current depressive symptoms, and the PBQ to assess disturbances in the mother-infant bond. Sociodemographic information was also recorded.
Instruments
Postpartum Bonding Questionnaire (Brockington et al. 2001)
This instrument was used to assess mother-infant bonding. It assesses the risk of presenting disorders in the mother-infant relationship during the postpartum period and includes four subscales with a total of 25 items which are rated by the mother on a 0–5 scale. The subscales are as follows: general factor, rejection and pathological anger, infant-focused anxiety, and incipient abuse scale. The PBQ was translated to Spanish by the translation-retranslation method recommended for cross-cultural studies (Brislin 1970).
Edinburgh Postnatal Depression Scale (Cox et al. 1987)
A 10-item scale designed to assess the presence of postpartum depression. Each item is scored on a 4-point scale (from 0–3), with the total score ranging from 0 to 30. The Spanish validation obtained a cutoff point of ≥11 to identify the presence of postpartum depression (Garcia-Esteve et al. 2003).
Sociodemographic data
Mothers completed a form which records information on sociodemographic and obstetric variables and affective disorders throughout life and during pregnancy.
Statistical analyses
Analyses were performed using the SPSS (version 18.0) software program, and M-Plus 3.0 (Muthén and Muthén 1998). The latter was used to conduct the confirmatory factor analyses (CFA). A series of CFA, using the maximum likelihood procedure as the technique for parameter estimation (Hoyle 1995), was carried out to test the factor structures proposed by previous studies (Brockington et al. 2001; Reck et al. 2006; Wittkowski et al. 2010). Comparative fit index (CFI), Tucker-Lewis index (TLI), root mean square error of approximation (RMSEA), and relative chi-square (χ 2/df) were used in the present study as fit indices. As rules of thumb, CFI and TLI values ≥0.90, RMSEA values ≤0.05, and χ2/df ratios <3 are indicators of a good model fit (Hoyle and Painter 1995; Kline 1998; Byrne 2001).
A series of exploratory factor analyses (EFA) was performed using the principal components extraction method and retaining different numbers of factors (from two to five), and then rotated using the oblique promax method. The number of factors was determined by inspecting the scree plot and by considering the criteria of interpretability. The agreement between factor loadings of the two samples was analyzed with Tucker’s congruence index (Lorenzo-Seva and ten Berge 2006). Subsequently, we performed a second-order analysis. A principal component analysis of the first-order factor correlation was conducted, and Schmid-Leiman transformation was computed (Schmid and Leiman 1957), using the SPSS syntax provided by Wolff and Preising (2005).
Intercorrelations between factors were computed by means of Pearson correlations, and the agreement between factor loadings was analyzed using congruence coefficients. Cronbach’s alpha coefficients as well as the correlations of each item with their corrected scale were calculated to assess the internal consistency. The association between depressive symptomatology and impaired bonding was analyzed by means of Pearson correlation, chi-square test or Student’s t test as appropriate.
Results
Confirmatory factor analysis
Table 1 shows the fit indices corresponding to the four-factor model proposed by the original author (Brockington et al. 2001, 2006c), Wittkowski’s three-factor model (2010), and the one-factor model proposed by Reck et al. (2006). The table shows the fit indices for the total sample, the general population sample, and the clinical sample. None of the models achieved satisfactory index-of-fit indices.
Exploratory factor analysis
Since no model confirmed the original structure of the PBQ, we conducted a series of exploratory factor analyses, extracting a different number of factors. The Kaiser-Meyer-Olkin coefficient was 0.92, suggesting a good fit of the data to the factor analysis; the Bartlett’s test of sphericity was significant (p < 0.001), which indicates that there were significant relationships between the items. The factor analysis revealed five factors with eigenvalues higher than 1, while the inspection of the scree plot suggested the extraction of two to five factors. Consequently, careful analysis of factor solutions (between two and five factors) resulted in the selection of the four-factor solution based on psychological interpretability. The four-factor solution accounted for 52.9 % of common variability in the total sample (factor 1 33.2 %, factor 2 9.4 %; factor 3 5.7 %; factor 4 4.6 %) (Table 2). The scale loading pattern of each factor was different from Brockington’s model. The first factor, which described signs of impaired bonding, included eight items (Q1, Q2, Q3, Q15, Q16, Q17, Q22, and Q23) which reflected topics such as emotional distance, regret about having the baby, unavailability to take care of the baby, or nostalgia for earlier times when the baby was not yet born. The second factor, related to anxiety about care, comprised eight items (Q7, Q10, Q12, Q13, Q19, Q20, Q21, and Q25) referring to maternal distress (“My baby cries too much,” “My baby makes me feel anxious,” “I am afraid of my baby,” or “My baby irritates me”). The third factor included items which identify a lack of enjoyment and affection for the baby (inversely scored: “I love to cuddle my baby,” “I love my baby to bits,” “My baby is the most beautiful in the world,” “I enjoy playing with my baby,” and “I feel happy when my baby smiles or laughs”). This third factor includes five items, of which three belong to the first original factor (Q4, Q8, Q9, Q11, and Q16). The fourth and last factor describes rejection and risk of abuse and includes four items related to negative feelings regarding their babies and behaviors that put the baby’s welfare at risk (Q14, Q15, Q18, and Q24) (“I feel angry with my baby,” “I resent my baby,” “I have done harmful things to my baby,” and “I feel like hurting my baby”).
Congruence coefficients between sample pairs of factors were as follows: factor 1 (0.75), factor 2 (0.98), factor 3 (0.43), and factor 4 (0.62). The congruence coefficients were low for all factors with the exception of factor 2, related to anxiety about care.
Intercorrelations among the factors
The intercorrelations between the four new factors obtained in the exploratory factor analysis in the total sample, general population, and clinical sample are displayed in Table 3. In general, we observed a high correlation between the factors, obtaining values from 0.43 to 0.67 in the total sample. In the clinical sample, intercorrelations between factors were higher than those observed in the general population sample.
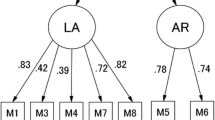
Schmid-Leiman transformation
To test the possibility of a general factor (already suggested by Reck et al. 2006) due to the high correlations between the four new factors identified by the exploratory analysis, we conducted a Schmid-Leiman transformation (1957), a procedure which estimates the percentage of variance explained by the general factor. The results are shown in Table 4, where a general factor is reflected with 22 items of the 25 that reported saturations higher than 0.41. In the total sample, a second-order general factor (GF) accounted for 61 % of the variance, and the four primary factors accounted for the remaining 39 %. These results support the idea that the best solution is to consider one general factor which explains most of the variance of the PBQ.
Reliability
Table 5 displays the reliability results of the PBQ’s Spanish version. Cronbach’s alpha coefficients in the total sample were 0.90 for the general factor (PBQ total score), and ranged from 0.56 to 0.85 for the four new primary factors. In the total sample, all corrected item-scale correlations were ≥0.30, with the exception of item 18, “I have done harmful things to my baby.”
Frequency and characteristics of bonding disorder
Taking into consideration the cutoff values for the total PBQ score suggested by Brockington et al. (2006c), 2.9 % of mothers in the general population group reported a bonding disorder and 0.6 % a severe bonding disorder; in the clinical group, the figures were 15.9 and 6.4 %, respectively, and in the total sample 8 and 2.8 % of mothers, respectively.
Relationship between bonding disorder and depressive symptomatology
EPDS scores in the total sample showed significant associations with general factor (GF) (r = 0.59; p < 0.001), as well as the PBQ factors impaired bonding (r = 0.53; p < 0.001), anxiety about care (r = 0.51; p < 0.001), lack of enjoyment (r = 0.40; p < 0.001), and rejection and risk of abuse (r = 0.32; p < 0.001). The clinical sample presented higher scores than the general population sample on depressive symptomatology (12.1 ± 7.5 vs. 4.9 ± 3.8; t[363.1] = 14.9, p < 0.001).
Table 6 shows the association between the presence of depressive symptomatology (EPDS ≥11) and a bonding disorder according to the PBQ. Depressive symptomatology was significantly associated with bonding disorder regardless of the type of group of mothers analyzed in both groups, and with all subscales.
Discussion
In this assessment of the Spanish version of the PBQ, good psychometric properties were identified for its use in Spanish clinical and general populations of postpartum women. The Spanish PBQ showed adequate reliability and a factorial validity in which a general factor of bonding disorder emerged as the best solution.
Neither the original four-factor solution (Brockington et al. 2001, 2006c) nor the alternative models proposed by Wittkowski et al. (2010) and Reck et al. (2006) were confirmed in our sample. The construction of the test and the characteristics of the original factor analysis (Brockington et al. 2001) might shed light on the diversity in the factor solutions found in PBQ. Brockington et al. (2001) performed a factor analysis including 84 items, which was used to select 25 items that were representative of the four main factors. As a result, subsequent factor analyses did not exactly replicate the conditions of the original one. In our study, we identified a four-factor solution related to impaired bonding, anxiety about care, lack of enjoyment, and rejection and risk of abuse. Factor 3, lack of enjoyment, represents the main change to the original PBQ and includes items that reflect the mother’s lack of affection or enjoyment; whereas factor 4, related to rejection and risk of abuse, includes the two risk of abuse items (18 and 24) as well as items 14 “I feel angry with my baby” and 15 “I resent my baby,” suggesting that in the Spanish population, these items could be considered more severe than in previous validations. The congruence of factor solutions between samples (clinical and general population) was poor in three factors (factors 1, 3, and 4) and was only good in factor 2, related to anxiety about care. For example, items Q14 and Q15 loaded on factor 4 in the general population sample, but on factor 3 in the clinical population. Consequently, the results of our factor solution must be considered with caution and need to be replicated in other Spanish samples. Furthermore, these results may suggest the need to adapt the PBQ to specific populations (i.e., clinical vs. general population).
In contrast, the Spanish PBQ was consistently summarized by a general factor in both the clinical and the general population samples. In 2006, Brockington suggested considering a PBQ total score of 26 or higher as identifying some type of bonding disorder, and a score of 40 or higher as identifying severe bonding disorder or maternal rejection. We recommend the use of the PBQ total score for detecting the presence of bonding disorder. Several reasons could be given to support this proposal. In our study, we conducted a second-order analysis in which a general factor of impaired bonding explained 61 % of the variance in the total sample, 61 % of the variance in the clinical sample, and 51 % in the general population sample. In the German validation, Reck et al. (2006) found a general factor that explained 23.9 % of the variance in which nine items had no significant loadings, leading to the creation of the shorter 16-item version of the PBQ. In Wittkowski’s study (2010), intercorrelations between factors were between 0.67 and 0.92.
Three items did not load meaningfully on this general factor: Q7 “My baby winds me up,” Q18 “I have done harmful things to my baby,” Q24 “I feel like hurting my baby.” Item Q7 loaded on factor 1 impaired bonding in Brockington’s study (2001), on factor 2 rejection and anger in Wittkowski’s study (2010), and was not removed in Reck’s study (2006). In contrast, items Q18 and Q24 constitute the factor 4 risk of abuse in Brockington’s study (2001), were omitted in Wittkowski’s study (2010), and also showed lower loadings with the general factor in Reck’s study (2006). These items were therefore removed in the German validation of PBQ. In the original study, this factor accounted for only 3.4 % of the total variance (Brockington et al. 2001). Some authors recommend omitting these items due to its low validity and diagnostic accuracy, and because mothers with obsessional thoughts would tend to score positively (Wittkowski et al. 2007). However, these items could help to detect a proportion of mothers at high risk of abusing their infants (Brockington et al. 2001). In light of this, we opted to maintain all the items from the original version.
Bonding impairment showed higher associations with depressive symptomatology, with correlations ranging from 0.30 to 0.60. The clinical sample showed higher scores on the PBQ than the general population sample, but these differences were mainly explained by differences in EPDS scores. Other studies also found significant associations between PBQ and depressive symptomatology, though of smaller magnitude (Reck et al. 2006). Depressive symptoms are related to reduced parenting responsiveness, affection and reciprocity, increased intrusive behaviors, and less positive descriptions of their children (Wan and Green 2009). Nevertheless, Brockington et al. (2006a)) postulates that mother-infant bonding impairment and postpartum depression represents two distinctive entities. Clinical observations of postnatal depressive mothers with normal bonding and of mothers without depressive symptomatology but impaired bonding also support this distinction (Brockington et al. 2006a). Further studies in mothers with clinical diagnoses of postnatal depression are needed to examine the nature of the association between the two entities.
Regarding clinical implications, as suggested by Klier (2006), the Spanish PBQ could be used to detect bonding disorders between mother and baby, as well as to assess the severity of the disorder. Cutoffs for the PBQ total score proposed by Brockington et al. (2006c) (26 or higher for some type of bonding disorder, and 40 or higher for severe bonding disorder) could be used for detecting bonding disorders until the Spanish version of PBQ is validated against a gold standard (interview). Furthermore, the PBQ can be useful to assess the evolution of the disorder and the progression of the therapy (Brockington et al. 2001), assessing the status of a bonding impairment beyond the recovery from the maternal depression (Klier 2006).
The main limitation of the study is the lack of a clinical interview for mother-infant bonding disorder. It is necessary to establish cutoff scores for detecting bonding disorders validated in Spanish population.
In conclusion, this study provides a Spanish version of the PBQ, an easy-to-use, reliable instrument for detecting and assessing mother-infant bonding alterations in the postpartum period. This tool has demonstrated its utility in detecting early bonding alterations in clinical and general populations.
References
Ayers S, Wright DB, Wells N (2007) Post-traumatic stress in couples after birth: association with the couple’s relationship and parent-baby bond. J Reprod Infant Psychol 25:40–50. doi:10.1080/02646830601117175
Bowlby J (1982) Attachment and loss: vol 1. Attachment. Basic Books, New York
Brislin RW (1970) Back-translation for cross-cultural research. J Cross-Cult Psychol 1:185–216. doi:10.1177/135910457000100301
Broad KD, Keverne EB, Curley LP (2006) Mother-infant bonding and the evolution of mammalian social relationships. Philos Trans R Soc Lond B Biol Sci 361:2199–2214. doi:10.1098/rstb.2006.1940
Brockington I (2004) Diagnosis and management of post-partum disorders: a review. World Psychiatry 3:89–95
Brockington I (2011) Maternal rejection of the young child: present status of the clinical syndrome. Psychopathology 44:329–336. doi:10.1159/000325058
Brockington IF, Oates J, George S et al (2001) A screening questionnaire for mother-infant bonding disorders. Arch Womens Ment Health 3:133–140. doi:10.1007/s007370170010
Brockington IF, Aucamp HM, Fraser C (2006a) Severe disorders of the mother-infant relationship: definitions and frequency. Arch Womens Ment Health 9:243–251. doi:10.1007/s00737-006-0133-0
Brockington IF, Chandra P, George S et al (2006b) The Birmingham Interview for Maternal Mental Health, 5th edn. Eyre Press, Birmingham
Brockington IF, Fraser C, Wilson D (2006c) The Postpartum Bonding Questionnaire: a validation. Arch Womens Ment Health 9:233–242. doi:10.1007/s00737-006-0132-1
Byrne BM (2001) Structural equation modeling with AMOS: basic concepts, applications, and programming. Lawrence Erlbaum, Mahwah
Condon JT, Corkindale CJ (1998) The assessment of parent-to-infant attachment: development of a self-report questionnaire instrument. J Reprod Infant Psychol 16:57–76. doi:10.1080/02646839808404558
Cox JL, Holden JM, Sagovsky R (1987) Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry 150:782–786. doi:10.1192/bjp.150.6.782
Edhborg M, Matthiesen A-S, Lundh W, Widström A-M (2005) Some early indicators for depressive symptoms and bonding 2 months postpartum—a study of new mothers and fathers. Arch Womens Ment Health 8:221–231. doi:10.1007/s00737-005-0097-5
Fonagy P, Gergely G, Target M (2012) The parent-infant dyad and the construction of the subjective self. J Child Psychol Psychiatry 48:288–328. doi:10.1111/j.1469-7610.2007.01727.x
Garcia-Esteve L, Ascaso C, Ojuel J, Navarro P (2003) Validation of the Edinburgh Postnatal Depression Scale (EPDS) in Spanish mothers. J Affect Disord 75:71–76. doi:10.1016/S0165-0327(02)00020-4
Høivik MS, Burkeland NA, Linaker OM, Berg-Nielsen TS (2013) The Mother and Baby Interaction Scale: a valid broadband instrument for efficient screening of postpartum interaction? A preliminary validation in a Norwegian community sample. Scand J Caring Sci 27:733–739. doi:10.1111/j.1471-6712.2012.01060.x
Hornstein C, Trautmann-Villalba P, Hohm E, Rave E, Wortmann-Fleischer S, Schwarz M (2006) Maternal bond and mother–child interaction in severe postpartum psychiatric disorders: is there a link? Arch Womens Ment Health 9:279–284. doi:10.1007/s00737-006-0148-6
Hoyle RH (1995) The structural equation modeling approach. Basic concepts and fundamental issues. In: Hoyle RH (ed) Structural equation modeling: concepts, issues, and applications. Sage Publications, Thousand Oaks, pp 1–15
Hoyle RH, Painter AT (1995) Writing about structural equation model. In: Hoyle RH (ed) Structural equation modeling: concepts, issues, and applications. Sage Publications, Thousand Oaks, pp 158–176
Klier CM (2006) Mother-infant bonding disorders in patients with postnatal depression: the Postpartum Bonding Questionnaire in clinical practice. Arch Womens Ment Health 9:289–291. doi:10.1007/s00737-006-0150-z
Kline RB (1998) Principles and practice of structural equation modeling. Guilford Press, New York
Korja R, Latva R, Lehtonen L (2012) The effects of preterm birth on mother-infant interaction and attachment during the infant’s first two years. Acta Obstet Gynecol Scand 91:164–173. doi:10.1111/j.1600-0412.2011.01304.x
Leckman JF, Mayes LC, Feldman R et al (1994) Yale Inventory of Parental Thoughts and Actions. Yale University, New Haven
Lorenzo-Seva U, ten Berge JMF (2006) Tucker’s congruence coefficient as a meaningful index of factor similarity. Methodology 2:57–64. doi:10.1027/1614-2241.2.2.57
Mäntymaa M (2006) Early mother-infant interaction. Determinants and predictivity. Printed dissertation, Acta Universitatis Tamperensis.
Moehler E, Brunner R, Wiebel A, Reck C, Resch F (2006) Maternal depressive symptoms in the postnatal period are associated with long-term impairment of mother–child bonding. Arch Womens Ment Health 9:273–278. doi:10.1007/s00737-006-0149-5
Mogi K, Nagasawa M, Kikusui T (2011) Developmental consequences and biological significance of mother-infant bonding. Prog Neuropsychopharmacol Biol Psychiatry 35:1232–1241. doi:10.1016/j.pnpbp.2010.08.024
Muthén L, Muthén B (1998) Mplus user’s guide, 3rd edn. Muthen & Muthen, Los Angeles
Muzik M, Bocknek EL, Broderick A et al (2013) Mother-infant bonding impairment across the first 6 months postpartum: the primacy of psychopathology in women with childhood abuse and neglect histories. Arch Womens Ment Health 16:29–38. doi:10.1007/s00737-012-0312-0
Noorlander Y, Bergink V, van den Berg MP (2008) Perceived and observed mother–child interaction at time of hospitalization and release in postpartum depression and psychosis. Arch Womens Ment Health 11:49–56. doi:10.1007/s00737-008-0217-0
Parfitt Y, Ayers S (2009) The effect of postnatal symptoms of post-traumatic stress and depression on the couple’s relationship and parent-baby bond. J Reprod Infant Psychol 27:127–142. doi:10.1080/02646830802350831
Reck C, Klier CM, Pabst K et al (2006) The German version of the Postpartum Bonding Instrument: psychometric properties and association with postpartum depression. Arch Womens Ment Health 9:265–271. doi:10.1007/s00737-006-0144-x
Schmid J, Leiman JM (1957) The development of hierarchical factor solutions. Psychometrika 22:53–61. doi:10.1007/BF02289209
Siu BW-M, Ip P, Chow HM-T et al (2010) Impairment of mother-infant relationship: validation of the Chinese version of Postpartum Bonding Questionnaire. J Nerv Ment Dis 198:174–179. doi:10.1097/NMD.0b013e3181d14154
Taylor A, Atkins R, Kumar R et al (2005) A new Mother-to-Infant Bonding Scale: links with early maternal mood. Arch Womens Ment Health 8:45–51. doi:10.1007/s00737-005-0074-z
Tietz A, Zietlow A-L, Reck C (2014) Maternal bonding in mothers with postpartum anxiety disorder: the crucial role of subclinical depressive symptoms and maternal avoidance behaviour. Arch Womens Ment Health 17:433–442. doi:10.1007/s00737-014-0423-x
Van Bussel JCH, Spitz B, Demyttenaere K (2010) Three self-report questionnaires of the early mother-to-infant bond: reliability and validity of the Dutch version of the MPAS, PBQ and MIBS. Arch Womens Ment Health 13:373–384. doi:10.1007/s00737-009-0140-z
Wan MW, Green J (2009) The impact of maternal psychopathology on child-mother attachment. Arch Womens Ment Health 12:123–134. doi:10.1007/s00737-009-0066-5
Wittkowski A, Wieck A, Mann S (2007) An evaluation of two bonding questionnaires: a comparison of the Mother-to-Infant Bonding Scale with the Postpartum Bonding Questionnaire in a sample of primiparous mothers. Arch Womens Ment Health 10:171–175. doi:10.1007/s00737-007-0191-y
Wittkowski A, Williams J, Wieck A (2010) An examination of the psychometric properties and factor structure of the Post-partum Bonding Questionnaire in a clinical inpatient sample. Br J Clin Psychol 49:163–172. doi:10.1348/014466509X445589
Wolff H-G, Preising K (2005) Exploring item and higher order factor structure with the Schmid-Leiman solution: syntax codes for SPSS and SAS. Behav Res Methods 37:48–58. doi:10.3758/BF03206397
Yarrow L (1972) Attachment and dependency: a developmental perspective. In: Gewirtz J (ed) Attachment and dependency. Winston, Washington, pp 81–95
Zeanah CH, Benoit D (1995) Clinical applications of a parent perception interview in infant mental health. Child Adolesc Psychiatr Clin N Am 4:539–554
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Approval was obtained from the institutional review board, and all women provided written informed consent before entering the study.
Appendix 1. The Spanish version of the Postpartum Bonding Questionnaire
Appendix 1. The Spanish version of the Postpartum Bonding Questionnaire
TEST DEL VÍNCULO EN EL POSPARTO (Postpartum Bonding Questionnaire, Brockington et al. 2001).
Traducido y Adaptado por Ll. García Esteve, P. Navarro, S. Diez.
Programa de Psiquiatría Perinatal Barcelona-CLINIC.
Por favor indique con qué frecuencia le ocurre lo que se detalla a continuación.
No hay respuestas “buenas” o “malas”. Escoja la respuesta más adecuada a su experiencia reciente.
¿Cómo se siente respecto a su bebé? | Siempre | Muy a menudo | Bastante a menudo | A veces | Raramente | Nunca | |
1. | Me siento cercana. | ||||||
2. | Desearía que volvieran los días en que no lo tenía. | ||||||
3. | Me siento distante. | ||||||
4. | Me encanta abrazarlo. | ||||||
5. | Lamento haberlo tenido. | ||||||
6. | Siento como si no fuera mío. | ||||||
7. | Siento que me toma el pelo. | ||||||
8. | Lo quiero con locura. | ||||||
9. | Me siento feliz cuando ríe. | ||||||
10. | Me irrita. | ||||||
11. | Disfruto jugando con él. | ||||||
12. | Llora demasiado. | ||||||
13. | Me siento atrapada como madre. | ||||||
14. | Me siento enfadada con mi bebé. | ||||||
15. | Siento resentimiento hacia él. | ||||||
16. | Es el más guapo del mundo. | ||||||
17. | Desearía que de alguna manera desapareciera. | ||||||
18. | He hecho cosas que son perjudiciales para él. | ||||||
19. | Me pone nerviosa. | ||||||
20. | Me asusta. | ||||||
21. | Me fastidia. | ||||||
22. | Me siento segura cuando lo estoy cuidando. | ||||||
23. | Siento que la única solución es que otra persona lo cuide. | ||||||
24. | Tengo ganas de hacerle daño. | ||||||
25. | Se consuela fácilmente. | ||||||
Rights and permissions
About this article
Cite this article
Garcia-Esteve, L., Torres, A., Lasheras, G. et al. Assessment of psychometric properties of the Postpartum Bonding Questionnaire (PBQ) in Spanish mothers. Arch Womens Ment Health 19, 385–394 (2016). https://doi.org/10.1007/s00737-015-0589-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00737-015-0589-x