Abstract
Although the transition to menopause represents a period of risk for depressive symptoms, there is little research into personality or trait-like factors that may confer vulnerability to depression during the transition to menopause. This study investigated whether the personality trait of self-criticism moderated the effects of irritability on depressive symptoms in women transitioning to menopause and whether these effects were mediated by lower levels of emotional regulation. Participants were 376 women, of whom 157 had entered the transition phase to menopause. These women in the transition phase completed measures of self-criticism, irritable mood, emotional regulation, and depressive symptoms. All analyses controlled for attitudes toward menopause and somatic symptoms. Moderated mediation regression analyses showed that higher levels of irritability were associated with poorer emotional regulation in highly self-critical women, but not in less self-critical women, and poorer emotional regulation was, in turn, related to higher levels depressive symptoms. Findings suggest that the transition to menopause may represent an especially vulnerable period for women with high levels of self-criticism. Although irritability is transitory for most women, for women who are highly self-critical, irritability may tax their ability to self-regulate and lead to more encompassing symptoms of depression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Menopause is a natural occurrence that nearly all women experience during midlife. Menopause refers to the natural cessation of menstruation and marks the end of a woman’s reproductive phase. The approximately 4-year phase leading up to menopause, referred to as the menopausal transition (MT) or peri-menopause, is characterized by widely fluctuating and declining hormonal levels. A woman is considered to have entered the transition from the reproductive to the non-reproductive phase of life when rising follicle stimulating hormone (FSH) concentration results in observable changes in her menstrual cycle (Soules et al. 2001). The phase coincides with midlife, a period which may be characterized by emotional turmoil (Wilk and Kirk 1995). Thus, the transition to menopause has been portrayed as a period of great emotional vulnerability (e.g., Freeman et al. 2006). Recent investigations indicate that although there may be some women who develop depression during the menopausal transition (Avis et al. 1994; Bromberger et al. 2001; Freeman et al. 2004; Hunter 1992; Maartens et al. 2002), a much more prevalent concern among women is an increase in irritable mood (Baram 2005; Born 2004; Bromberger et al. 2003; Powell 1996). Evidence stemming from research unrelated to menopause indicates that irritability and depression are distinct mood conditions (e.g., Born and Steiner 1999). Furthermore, various researchers have proposed that irritable mood is a prodrome of full-blown depression (e.g., Fava and Tossani 2007), especially if other vulnerability factors, such as maladaptive personality traits (Blatt 2004; Blatt and Zuroff 1992), are involved. The overarching objective of this study was to examine factors that are related to higher levels of depressive symptoms and to identify women at risk for depressive symptoms during the transition to menopause.
Emotional regulation during the transition to menopause
The inability to effectively regulate mood and emotion can compromise many aspects of an individual’s life and lead to a cascade of stressors and psychological difficulties. Difficulties with mood and emotion and deficits in regulating such states have been implicated in up to 75 % of disorders listed in the Diagnostic and Statistical Manual of Mental Disorders, 4th edn. (DSM-IV, Werner and Gross 2010) including depression (Gross and Munoz 1995). Emotional regulation involves “the extrinsic and intrinsic processes responsible for monitoring, evaluating, and modifying emotional reactions, especially their intensive and temporal features, to accomplish one’s goals” (Thompson 1994, p. 27–28). However, this resource is limited and, if consumed but not replenished, it will result in ego depletion (Baumeister et al. 1998) and contribute to a type of self-regulation failure referred to as under-regulation (Baumeister and Heatherton 1996). Under-regulation is reflected in behavior (e.g., individual has difficulty staying on task and engaging in goal-directed behavior), affect (e.g., individual has difficulty modulating negative emotions), and cognitive activity (e.g., individual has difficulty concentrating or ‘resisting’ maladaptive cognitions). The limited-resource model of self-regulation has been used to explain why people succumb to temptation when feeling distressed (Tice et al. 2001), and there is a large body of research on the role of self-regulation in psychopathology including depression (Baumeister et al. 2007; Strauman 2002).
For instance, participants with a history of depression reported more difficulties in emotional regulation than a matched, never-depressed group (Ehring et al. 2008). They also showed impaired ability to access strategies deemed effective and reported more difficulties with goal-directed behavior when upset (Ehring et al. 2008). Lastly, Vujanovic et al. (2008) reported a positive association between difficulties in emotional regulation and anhedonic depressive symptoms among a sample of young adults. Emotional regulation may therefore be an important predictor of depressive symptoms during the transition to menopause.
Irritability and depression during the transition to menopause
Although evidence is somewhat mixed, and studies show that the majority of women do not develop severe mood disturbances as they traverse to menopause, research has generally confirmed that this period as a whole is associated with increased depressive symptoms. For instance, depressive symptoms increase from pre-menopause to peri-menopause and from peri-menopause to post-menopause (Maartens et al. 2002), while other data show that depressive symptoms increase during the menopausal transition (Avis et al. 1994; Bromberger et al. 2001; Freeman et al. 2004; Hunter 1992) and then improve after menopause (Freeman et al. 2004). Freeman et al. (2006) found that clinically significant depressive symptoms (CES-D scores ≥ 16) were four times more likely to occur, and a clinical diagnosis of depressive disorder was 2.5 times more likely during the period of transition than in pre-menopause. Schmidt et al. (2004) also reported that compared with pre-menopause, the 24-month period surrounding the final menstrual period (FMP, the menopause) was associated with a 14-fold increased risk of episodes of minor depression relative to the 31-year time period that preceded the onset of the transition. Furthermore, although prior depression has been reported as a significant, and even the primary, risk factor for depression during the menopausal transition (Freeman et al. 2004; Harlow et al. 2003; Hunter 1990), other data indicate that the risk for new onset of depressed mood was elevated during the transition, even in women with no history of prior depression (Freeman et al. 2006; Cohen et al. 2006; Schmidt et al. 2004).
While the transition to menopause appears to confer risk for depression, others note that irritability is a more common presenting mood complaint of women transitioning to menopause (Baram 2005; Born 2004; Bromberger et al. 2003; Powell 1996). Indeed, in the context of menopause, for up to 70 % of transitioning women, irritability rather than depression is their primary complaint (Born 2004). Although irritability is often a normal and transitory state, more prolonged or excessive levels can have a negative impact on physical and psychological health, can impair daily functioning, particularly within the home (Hylan et al. 1999), and can cause friction in interpersonal relationships (Born et al. 2002; Fava 1987; Fava and Tossani 2007). Van Praag (1996a, b) note that there is accumulating empirical evidence indicating that heightened sensitivity to environmental stressors, which manifests as irritability, may be the primary and initial experience of a mood disturbance, whereas depression is secondary to such dysregulation. For example, Fava et al. (1990) report that, compared to a non-depressed control group, depressed outpatient participants had at least one prodromal psychiatric symptom 6 months prior to the onset of depressed mood and of the full depressive syndrome. They reported that anxiety and irritable mood were the most frequent prodromes (Fava et al. 1990), with others reporting similar findings (Iacoviello et al. 2010; Mahnert et al. 1997). Fava and Tossani (2007) proposed that in the presence of other risk factors, these initial mood symptoms increase the likelihood that a full-blown depressive episode will develop.
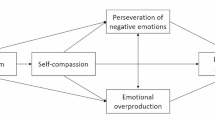
The relationship between irritability, risk factors, and depressive symptoms associated with the transition to menopause may be understood through a vulnerability or diathesis–stress model. Diathesis–stress models posit that although stress may be an important factor in precipitating and maintaining psychological disorders, it is especially potent in individuals with certain characteristics. A dual-vulnerability model (DVM), as proposed by Young and associates (1991), may be specifically applicable to the development of depression within the context of menopause. According to this model, individuals most likely to develop the full syndrome of a disorder possess two distinct vulnerabilities, each giving rise to a specific set of symptoms. The first is a biological vulnerability; in this case, the transition to menopause. This, in turn, gives rise to the first set of symptoms; in this case, irritability. These symptoms then act as stressors. In individuals who also possess the second vulnerability, which is of a psychological nature, these stressors then precipitate the second set of symptoms; in this case, depressive symptoms (Young et al. 1991). In the context of this study, the psychological vulnerability may implicate personality dispositions. The role of personality vulnerability has been widely studied in relation to depression (see Blatt 2004), but not as a factor that moderates the relation between irritability, which has been shown to be prevalent in the transition to menopause, emotional regulation, and depressive outcomes. According to the DVM model, women at increased risk for depression as they transition to menopause should be those who possess both vulnerabilities.
Although several personality or cognitive factors have been posited as risk factors for depression, one widely studied such factor is the personality trait of self-criticism (Blatt 1974; Blatt et al. 1997; Blatt and Shichman 1983; Blatt and Zuroff 1992). According to this model, self-critical individuals “strive for excessive achievement and perfection, are often highly competitive and work hard” (Blatt and Zuroff 1992, p. 528), and they “possess the basic wish to be acknowledged and respected” (Vettese and Mongrain 2000, p. 610). Evidence has generally confirmed that self-criticism confers risk for the development of depression, both in the absence of and following stressors (for an extensive review, see Blatt 2004). However, no research has examined whether it may increase risk for depression during the transition to menopause, or whether they may moderate the effects of irritability on depression during this transition.
There is good reason to expect self-criticism to moderate the effects of irritability on depression during the transition to menopause. Self-criticism is associated with aspects of affective experience that underlie depressive disorders and dysphoria. For example, individuals high in self-criticism experience high levels of negative affect (Kopala-Sibley and Santor 2009; Kopala-Sibley et al. 2012) and low levels of positive affect (Kopala-Sibley and Santor 2009). They experience more persistent and frequent episodes of mood disturbances, and their affective states are also more intense (Zuroff et al. 1999). Self-critical individuals experience ambivalence over the expression of negative emotions (Mongrain and Zuroff 1994), which may then inhibit women’s emotional regulation abilities when they become irritated.
Moreover, women high in self-criticism tend to react aggressively and with overt manifestations of hostility in response to conflict with others (Mongrain et al. 1998). As Mongrain et al. (1998) note, although self-criticism is associated with the ability to express negative emotions, it also seems to be associated with a greater sense of submissiveness, which suggests that such individuals may feel incompetent and disempowered. Such secondary negative emotions tend to perpetuate and intensify emotional states. Taken together, these characteristics suggest that emotional regulation abilities may be impaired in these individuals and that self-criticism may moderate the effects of irritability on depression in women during the transition to menopause.
Overview and hypotheses
This study examined predictors, moderators, and mediators of depressive symptoms during the transition to menopause in a sample of women who were classified as transitioning to menopause (Sowers et al. 2000). Analyses also controlled for the confounding effects of stress, women’s attitudes toward menopause, and their levels of menopausal symptoms and complaints, as these factors may impact depression during the transition to menopause. First, we expected that irritability would be associated with depressive symptoms during the transition to menopause. Second, we expected the relationship between irritability and depression to be stronger in highly self-critical women. Third, we expected emotional regulation to mediate the association between irritability and severity of depressive symptoms in the context of the personality vulnerability factor of self-criticism. That is, we tested a mediated-moderation model such that self-criticism moderated the relationship between irritability and emotional regulation, which, in turn, was associated with depressive symptoms.
Methods
Participants
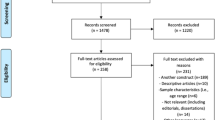
Participants were recruited through Craigslist and through Interactive Tracking Systems Inc. (Itracks), which recruits and supplies participants for online research. The study was advertised as an examination of the role of personality on health and well-being in adulthood. They were entered into a lottery to win one of four cash prizes of $50 or $100 each. Participants were 391 women. The sample was predominantly Caucasian (90.6 %), and approximately 25 % of the sample had a university degree. To be eligible, women had to be fluent in English and have an intact uterus with at least one ovary. Exclusionary criteria included current use of psychotropic or hormonal medications including hormonal contraceptives and hormone replacement therapy, pregnancy, or breastfeeding, alcohol or drug abuse, and serious or chronic medical or psychiatric conditions (e.g., cancer, diabetes, hypothyroidism, and schizophrenia). Pre-screening questions were administered to select women who met either of the following two age and menopausal status combinations: (1) aged between 35 and 40 years, and meeting criteria for pre-menopause (as defined below), or (2) aged between 47 and 60 years, and meeting criteria for any of the remaining three menopausal stages.
There are no objective biological markers or indicators with widely accepted cut-offs that can be used to define the transition to menopause (NAMS 2010). According to Harsh et al. (2009), the most reliable method combines plasma gonadotropin levels, chronologic age, and menstrual cycle characteristics. The present study used the most cost-effective method for assessing stages of reproductive aging which is based on menstrual bleeding patterns (Soules et al. 2001) and chronologic age (Bastian et al. 2003). Chronologic age, though not a good marker of menopausal status, is important to consider because cycle irregularity is not restricted to the transitioning period (Harsh et al. 2009) and, in women younger than 40 years, may reflect a lifetime pattern of variability rather than a changing endocrine environment (Harlow et al. 2007). Also, as indicated by Bastian and colleagues (2003), staging menopausal status in early to mid-40s is challenging. Thus, in the present study, age was used in conjunction with staging criteria (described below) to categorize women into four groups.
Menopausal status was determined using a questionnaire, adapted from the 22-item questionnaire used by Schleifer (2003), that collected information on reproductive characteristics (e.g., menstrual history and bleeding patterns, use of hormonal preparations) and medical history. Items asked participants about cycle regularity, date of last cycle, and four mutually exclusive questions regarding participants’ menstrual bleeding pattern in the preceding 12 months. Classification was based on a widely used system established by the Study of Women’s Health Across the Nation (SWAN, Sowers et al. 2000). Women were classified as follows: (1) pre-menopause: menstrual cycles have been regular with no change in cycle length; (2) early transition: menstruated in previous 3 months, but experienced a change in frequency (more or less frequent periods); (3) late transition: had a period in last 12 months, but not in past 3 months; and (4) post-menopause: did not have a menstrual period in the previous 12 months. Women were included in the pre-menopause group if they met the relevant criteria and were between the ages of 35 and 40 years. Based on evidence that the median age of onset of the transition is 47.5 years (McKinlay et al. 1992), the age range for sampling women in the menopause transition (early and late) and post-menopause was restricted to those between the ages of 47 and 60 years.
The number of participants included in each of the groups were as follows: (1) pre-menopause: 106, (2) early transition: 96, (3) late transition: 68, and (4) post-menopause: 121. As the focus of this paper is on the transition to menopause, only women in the early transition and late transition groups were included in regression analyses, although differences in irritability, self-criticism, and depressive symptoms are examined across all four groups. It is noted that, of the participants who were still menstruating, the majority reported their periods as being regular (96 % of pre-menopause group), or that they had been regular prior to entering the transition (92 % of transition group).
Procedure
Measures
Demographics
A total of nine items were used to collect information on demographic variables such as age, education, occupational status, marital status, ethnicity, and annual household income.
Self-criticism
The depressive experiences questionnaire (DEQ, Blatt et al. 1976) is a widely used instrument designed to measure individual differences in self-criticism. The McGill revision (Santor et al. 1997a) is a unit-weighted revision of the original DEQ. It consists of 48 of the original 66 items. Participants respond by indicating their degree of agreement to each item using a seven-point Likert scale from 1 (strongly disagree) to 7 (strongly agree). Example items include “I set my personal goals and standards as high as possible” and “I have a difficult time accepting weakness in myself.” The self-criticism scale of the McGill version was highly correlated with the original DEQ self-criticism scale in a nonclinical student sample (Santor et al. 1997b). The self-criticism scale of the DEQ has shown retest reliability of 0.75 and 0.80 at 3 and 12 months, respectively (Zuroff et al. 1983; Zuroff et al. 1990), and displays retest stability even following stressful life events (Zuroff et al. 1990). This scale also shows good internal consistency and construct validity (Blatt et al. 1976; Mongrain and Zuroff 1989; Zuroff and Mongrain 1987; Zuroff et al. 1990) and has been widely used as measures of personality–vulnerability factors to depression and psychopathology (e.g., Abela et al. 2007; Abela and Taylor 2003; Abela et al. 2006; for reviews, see Blatt 2004; Blatt and Zuroff 1992). The revised scale shows adequate internal consistencies, with Cronbach’s α ranging from 0.69 to 0.76 for self-criticism. The revised version has been validated in clinical and nonclinical populations (Santor et al. 1997b). In the present study, the self-criticism scale showed a Cronbach’s alpha of 0.80 for the combined sample and 0.76 for the transition sample.
Irritability
Irritability was assessed using the self-rating version of the Born–Steiner irritability scale (BSIS; Born et al. 2008). The BSIS is a self-report measure designed to assess severity of state irritability specific to women. The scale measures irritable mood as a unidimensional construct with 14 items that assess the following core symptoms of irritability: (1) annoyance (e.g., “It took very little for things to bother me”); (2) anger (e.g., “I have been feeling mad”); (3) tension (e.g., “I have been feeling ready to explode”); (4) hostile behavior (e.g., “I have yelled at others”); and (5) sensitivity (e.g., “I have been irritable when someone touched me”). Participants use a four-point Likert scale from 1 (not at all) to 4 (most or all of the time) to rate the extent to which the item was experienced during a specified time frame. This scale shows good internal consistency (α = 0.93) and test–retest reliability (r = 0.70) over 21 days (Born et al. 2008). The measure has good convergent validity as evidenced by the significant correlations of the self-rated with observer-rated ratings (Born et al. 2008). In the present study, Cronbach’s alpha was 0.96 for both samples. In order to keep the time frame consistent among all measures used in the study, participants were required to indicate how they felt in the past week.
Emotional regulation
Emotional regulation was assessed with the difficulties in emotional regulation scale (DERS; Gratz and Roemer 2004) by summing the goals (e.g., “When I’m upset, I have difficulty concentrating”), impulse (e.g., “When I’m upset, I lose control over my behaviors”), and strategy (e.g., “When I’m upset, I believe that wallowing in it is all I can do”) subscales. The DERS is a 36-item self-report measure designed to assess difficulties in emotional regulation. These three subscales were combined based on their substantial correlations as reported by Gratz and Roemer (r = 0.61 and 0.62 for strategies with impulse and with goals, respectively, and 0.50 between goals and impulse). Most statements begin with the stem “When I’m upset…” Participants rate the degree to which each statement provided applies to them using a five-point Likert scale from 1 (almost never 0 to 10 %) to 5 (almost always 91 to 100 %). Ratings are summed to yield subscores and, across subscores, to obtain a global score, with higher scores indicating a greater degree of difficulty in regulating emotion. The overall scale shows high internal consistency (α = 0.93) as well as test–retest reliability (α = 0.88) over a period of between 4 and 8 weeks (Gratz and Roemer 2004). The DERS correlates with various measures of emotion dysregulation and avoidance, as well as various behavioral outcomes related to emotional regulation deficits (Gratz and Roemer 2004). In the present study, Cronbach’s α was 0.90 for both samples.
Depressive symptoms
Depressive symptoms were assessed using the beck depression inventory-II (BDI-II; Beck et al. 1996). The BDI-II is a widely used 21-item measure of the severity of depressive symptoms in adolescents and adults. Items are rated on a 0–3 point scale (0 = not present to 3 = severe symptom manifestation). The BDI has strong psychometric properties (Beck et al. 1996; Steer et al. 1997). The item assessing the symptom irritability was omitted so as to remove redundancy with the construct irritable mood, which was measured with the BSIS. Also, due to the sensitive nature of item that assesses suicidal intent and our inability to provide clinical support to any participant who endorses the option indicating high risk of self-harm, this item was omitted. Internal consistency was 0.87 for the combined sample and 0.89 for the transition sample. In the present study, participants were asked to indicate how they felt in the past week.
Attitudes toward menopause and aging (ATMA; Sommer et al. 1999)
This seven-item measure was developed by the SWAN to assess the participant’s attitude toward aging and menopause in their multiethnic community-based studies. Participants use a three-point Likert scale to rate the degree of agreement with each statement, from 1 (disagree) to 3 (agree). Ratings are summed across the seven items, with higher scores indicative of a more positive attitude toward menopause and aging. In the present study, Cronbach’s alpha was 0.70 in the combined sample and 0.71 in the transition sample.
Menopause rating scale (MRS; Schneider et al. 2002)
The MRS is a self-report measure composed of 11 items designed to assess symptoms and complaints in women who are still menstruating or transitioning to menopause. The current study focused on the somatic symptoms subscale as it assesses symptoms of hot flashes and sleep disturbance. Using a five-point Likert scale, participants rate their perceived severity of symptoms from 0 (none) to 4 (very severe). Cronbach’s alpha for the somatic subscale factor was 0.68 in the combined sample and 0.71 in the transition sample. Participants were asked to indicate severity of symptoms experienced in the past week.
Data analyses
Initial analyses consisted of ANOVAs with planned comparisons in order to determine whether depressive symptoms and irritability varied as a function of menopausal status. Zero-order correlations then determined whether our hypothesized independent, dependent, and mediator variables were significantly related. All subsequent analyses were performed within the combined early and late transition menopausal groups (combined N = 164). Mediational analyses consisted of a series of hierarchical multiple regression models. As measures of effect size, we report R 2 and Cohen’s d values. All analyses controlled for attitudes toward menopause and somatic symptoms, as these variables are known to predict mood and depressive symptoms during the transition to menopause (Avise et al. 2001; Baker et al. 1997; Bosworth et al. 2001; Brown et al. 2009). All predictors were standardized. Our approach to testing mediation and moderation followed Baron and Kenny (1986), and our approach to testing-mediated moderation followed Muller et al. (2005). In all models, depression was the criterion variable. Accordingly, block one contained our control variables. Block two contained the main effects of self-criticism and irritability. Block three contained the interaction term between self-criticism and irritability. Following a significant interaction term, emotional self-regulation was then added as a control variable, and the reduction in the effect of our interaction term was examined. Sobel tests were computed in order to examine the significance of the indirect paths from the interaction of self-criticism and irritability to depression via self-regulation. Significant interaction terms were examined by testing the effects of irritability at high (+1 SD), moderate (mean), and low (−1 SD) levels of self-criticism.
Results
Descriptive statistics and bivariate correlations
Means, standard deviations, and bivariate correlations are presented in Table 1. In support of our hypotheses, severity of depressive symptoms was significantly correlated, within the combined sample, with self-criticism, irritable mood, severity of somatic symptoms, and with difficulties in self-regulation. Severity of depressive symptoms was also related to having a negative attitude toward aging and menopause. Lastly, one-way ANOVAs showed that mean levels of self-criticism did not differ between the four menopause groups, F(3,334) = 0.40, p = 0.75 and F(3,330) = 0.61, p = 0.61, respectively, suggesting these variables are stable across the four menopausal stages.
Stage-related differences in depression and irritability
A significant main effect of menopause status on irritability was obtained [F(3,365) = 4.34, p = 0.005, and ω2 = 0.027]. Specifically, contrast tests indicate that, relative to pre-menopause, irritability was higher in women in the early transition stage [F(1,365) = 6.64, p = 0.01, and d = 0.35]. Women in the early transition phase also showed a trend toward higher levels of irritability than women in the early transition [F(1,365) = 0.69, p = 0.41] and showed higher levels of irritability than post-menopausal women [F(1,365) = 12.03, p < 0.001, and d = 0.48].
Results also revealed a significant main effect for menopause status on level of depressive symptoms [F(3,349) = 2.62, p = 0.05, and ω2 = 0.013]. The effect size was slightly larger for irritability than for depressive symptoms, but both are considered small effects. Contrast analyses indicate that, compared to pre-menopause levels, depressive symptoms were higher in the early transition [F(1,349) = 4.63, p = 0.03, and d = 0.32], late transition [F(1,349) = 3.82, p = 0.05, and d = 0.36], and post-menopause, [F(1,349) = 6.40, p = 0.01, and d = 0.37].
Initial model predicting depressive symptoms
Because the primary goal of this study was to examine the effect of personality on managing the mood symptoms found to be more pronounced and persistent during the menopausal transition, these hypotheses were tested in transitioning women. The overall model predicting depressive symptoms was significant [F(6,94) = 23.44, p < 0.0001] and explained 60 % of the variance in depressive symptoms. Main effects were obtained for menopause-related somatic symptoms (β = 0.28, p < 0.001) and negative attitudes toward menopause and ageing (β = −0.50, p < 0.0001). Main effects were also obtained for self-criticism (β = 0.38, p < 0.0001) and irritability (β = 0.03, p = 0.68). There was a significant interaction between self-criticism and irritability (β = 0.22, sr 2 = 0.05, and p = 0.002). Higher levels of irritability were related to higher levels of depression at high [β = 0.42, t(99) = 4.20, and p < 0.0001] and moderate [β = 0.20, t(99) = 2.58, and p < 0.01] levels of self-criticism, but not at low levels of self-criticism [β = −0.02, t(99) = −0.15, and p = 0.88]. The difference between the slopes at high and moderate levels of self-criticism approached significance [t(99) = 1.75, p = 0.08; Fig. 1].
Self-regulation as a mediator
Finally, the preceding analyses were repeated, but with self-regulation included prior to the interaction of self-criticism and irritability. Emotional self-regulation showed a significant effect on depressive symptoms [β = 0.26, t(93) = 3.08, and p = 0.003]. Crucially, the moderated effect of irritability by self-criticism on depressive symptoms was weaker after entering the mediator in the regression [β = 0.17, t(93) = 2.54, and p = 0.013 vs. β = 0.22, t(94) = 3.37, and p < 0.001], but still significant. At low levels of self-criticism, the effect of Irritability on emotional regulation was not significant [β = 0.13, t(94) = 1.16, and p = 0.25], and neither was the total indirect effect on depression [β = 0.034 (SE = 0.035), Z = 0.97, and p = 0.33]. At the mean of self-criticism, the slope [β 51 = 0.34, t(94) = 3.58, and p < 0.0001] and the total indirect effect were both significant [β = 0.088 (SE = 0.038), Z = 2.32, and p = 0.02]. At high levels of self-criticism, the slope became steeper [β 51 = 0.55, t(94) = 4.70, and p < 0.0001] and contributed to a stronger indirect effect on depression [β = 0.143 (SE = 0.058), Z = 2.46, and p = 0.014]. In sum, higher levels of irritability were related to higher levels of difficulties in emotional regulation in women who were moderately or highly self-critical, which, in turn, were related higher levels of depressive symptoms.
Discussion
The present study sought to examine factors that are related to symptoms of depression in women, as they transition from the reproductive to the non-reproductive phases of life. Results showed that irritability was significantly higher in transitioning women, compared to those who were pre-menopausal or post-menopausal. Depressive symptoms were significantly higher in transitioning and post-menopausal women. Moreover, results showed that the association between irritability and depressive symptoms in women transitioning to menopause was more marked as their level of self-criticism increased. Finally, deficits in emotional regulation partially mediated the effects of the interaction between self-criticism and irritability on depressive symptoms.
Irritability and depressive symptoms during the transition to menopause
Consistent with evidence that many women experience emotional and mood changes in the years surrounding menopause (e.g., Avis et al. 1994; Freeman et al. 2004, 2006; Schmidt et al. 2004), results showed that women who were in the early stage of the transition had significantly higher levels of irritability than women in pre-menopause. Women who were in the early and late stages of the transition reported the highest level of irritable mood. Post-menopausal women reported levels that were low and comparable to levels reported by women in pre-menopause. Depressive symptoms showed a similar phase-related pattern, such that women in the early stage of the transition reported significantly higher levels of depressive symptoms than pre-menopausal women. However, unlike irritability, levels of depressive symptoms in the late transition and post-menopause were comparable to those of the early transition. As these analyses suggest, while both mood conditions are elevated in women in the early transition as compared to levels reported by women in pre-menopause, irritability appears to be lower post-menopause, whereas depressive symptoms appear similar across the transition phase and post-menopause.
These differential patterns of association with reproductive status suggest that different mechanisms may underlie these two conditions. The finding that mean levels of irritability vary across women in different reproductive stages may implicate hormonal factors. Reproductive stages have been defined clinically by changes in menstrual bleeding patterns. These changes reflect the endocrinological events of the ageing reproductive system. Irritability could be another such manifestation. It may be that neuroendocrine activity has an indirect effect on the affective system and the physiological state affects one’s state of arousal or threshold for reactivity, rendering some women more responsive to the external environment (Buchanan et al. 1992; Hyde et al. 2008). Although irritability has not been widely studied in relation to menopause, it is reported as a prominent dimension of mood disorders related to reproductive events and cyclicity (Born and Steiner 1999; Halbreich 2010). For example, irritability is a predominant mood symptom of pre-menstrual dysphoric disorder (PMDD, American Psychiatric Association 2000). Indeed, women with PMDD report feeling irritable, but not depressed (Angst et al. 2001), and a cardinal feature of PMDD is the cyclical onset and remission of symptoms (American Psychiatric Association 2000).
Personality vulnerability, irritability, and depressive symptoms in the transition to menopause
Consistent with diathesis–stress models (Luyten et al. 2007; Mongrain and Zuroff 1994; Nietzel and Harris 1990), the effect of irritability on depressive symptoms in women who were in the transition phase to menopause was strongest for those who were highly self-critical. Importantly, this result held after controlling for factors which have previously been associated with depression such as hot flashes, sleep disturbance, and negative attitudes toward ageing and menopause.
Results are consistent with the dual-vulnerability model (DVM) of Young et al. (1991), which suggests that individuals at risk for psychopathology possess both a biological and a psychological vulnerability. In the current study, transitioning to menopause represents a biological vulnerability, while high levels of self-criticism represent a psychological vulnerability which interacts with irritability, the mood manifestation of the biological vulnerability of transitioning to menopause. Irritability acts as a stressor in and of itself. As Alexander et al. (2007) indicated, “being symptomatic in the transition is in and of itself a unique stressor of the midlife woman” (p. S100), and there is evidence that menopausal symptoms predict a decline in physical and social functioning (Kumari et al. 2005). Our results suggest that in highly self-critical women, irritable mood may be particularly disrupting and noxious as the self-critical woman’s concern to maintain self-control is challenged.
It should be noted that the menopausal transition occurs during the midlife, and many of the psychological concerns of midlife are central to issues of the self-critical personality. For example, having a strong sense of autonomy, accomplishment, and environmental mastery are important concerns in midlife (Ryff 1989, 1991) and predict well-being in middle-aged adults (Ryff 1995). However, for highly self-critical women, because of their excessively high standards and insecurities of “not being good enough,” a sense of accomplishment and of mastery may be more difficult for them to achieve. These concerns and struggles are not particular to their functioning in midlife. But at midlife, when such concerns become more central for people, in general, the self-critical woman’s sense of self-worth may be even more compromised. Personality vulnerability factors, such as self-criticism, may explain findings in the menopause literature that, for many women, the first episode of depression is experienced during the transition (Cohen et al. 2006; Freeman et al. 2006; Reed et al. 2009; Schmidt et al. 2004).
Difficulties in self-regulation during the transition to menopause
Although our cross-sectional design cannot speak to within-subject processes that unfold overtime, the current findings may contribute to the growing literature on self-criticism as they indicate that, in addition to the various mechanisms that have been proposed and tested, self-criticism in women during the transition to menopause is associated with emotional dysregulation when they are in a negative (i.e., irritable) mood state. This finding also extends research that links negative mood to depressive symptoms (Kopala-Sibley and Zuroff 2010; Fava et al. 1990; Fava and Tossani 2007) by providing evidence that self-regulation is implicated as one process that accounts for this relationship. Although self-regulation as assessed in the current study pertained to impaired concentration and disrupted performance of short-term tasks, these lower-level activities lead to the attainment of higher-level goals. Self-critical women set high standards for themselves in all domains of activity and have an incessant need not only for control and to maintain a positive sense of self but also to gain the approval and respect of others. Therefore, difficulties in self-regulation encountered in the more immediate term may be especially detrimental to them if their larger, longer-term achievements are jeopardized due to their inability to successfully engage in the tasks that lead to such accomplishments.
Furthermore, the menopause transition coincides with the midlife, and for many women, this is a time of increased responsibilities, especially if a woman is caring for aging parents, parenting adolescents or young adult children into healthy adulthood, maintaining a household, or maintaining her place in the in the workforce. For highly self-critical women, all these tasks require that they be accomplished to the best of standards. Their incessant struggles to maintain a positive sense of self and to ward off disapproval, all the while coping with internal emotional arousal (e.g., irritability), may burden their self-regulatory resources. However, we should acknowledge that these possibilities are speculative and would be best tested using longitudinal repeated-measures designs that follow women through the transition to menopause and that take into account both the various roles and responsibilities women often take on during this period of life and factors such as goal accomplishment and perceived approval from others.
Limitations and future directions
Several limitations to this study should be noted. First and foremost, the hypotheses and models of mediated-moderation test imply causation; however, the current study used a cross-sectional design in which all variables were assessed concurrently. Hence, any statement or interpretation of causation should be interpreted with caution. Indeed, our model rests on the assumption of a certain temporal order in the relationships of our variables. Longitudinal research would be better able to assess the temporal order of irritability, emotional regulation, and depressive symptoms. We also assessed depressive symptoms rather than diagnoses of Major Depressive Disorder, so it is not clear that results would extend to diagnoses of depression. Ideally, future research would follow a sample of women over time as they transition through menopause, which would permit stronger conclusions about the temporal order of effects and would assess diagnoses of depression as well as self-reported symptoms.
Next, reproductive status was based solely on self-report and relied on women’s recollection of when their last menstrual cycle occurred. Misclassification could have occurred between the early and late stages of the menopause if, for example, a participant mistakenly remembered her last cycle as having been within the previous 3 months (early transition) when it was within the past 4 months (late transition). However, based on results which showed no difference between these two groups in level of irritability and of depressive symptoms, the two groups were combined. It is acknowledged that endocrine activity may differ between these two phases of the transition; however, the focus of this study was not to uncover the particular effects of hormonal dynamics. Measures of irritability, emotional regulation, and depressive symptoms were also assessed via self-report, which may result in artificially inflated associations between variables due to shared method variance. Future research may benefit from including ratings of mood and emotional regulation from others such as family members.
Finally, this study was administered over the internet. This may introduce a self-selection bias and, furthermore, although use of internet technology is now quite ubiquitous in psychological research, the possibility remains that access to technology may be limited in certain segments of the population (e.g., low SES, older women). In this regard, women who participated in this study were predominantly Caucasian and middle class. As such, results of this study may not generalize to the entire population of mid-aged women. Accordingly, future research would benefit from longitudinal designs with more diverse samples, multiple-informant measures of irritability, and neuroendocrinological data to assess menopausal status.
Conclusion
This is the first study, to our knowledge, to examine whether self-criticism in women could potentially place them at increased risk of developing depressive symptoms as they transition to menopause and to test models of mediated moderation to examine the factors and mechanisms that underlie the relationship. Findings from this study make several significant contributions to the current literature. First, they show that different processes may underlie irritable mood and depressive symptoms, as levels of both irritability and depressive symptoms seem to increase with the onset of the transition, but only irritability abates at post-menopause. Importantly, results suggest that the transition to menopause, which is associated with an increase in irritable mood, may be more challenging for women with high levels of self-criticism. Findings suggest that, for highly self-critical women, irritability impairs these women’s ability to self-regulate and partially accounts for the increase in depressive symptoms.
References
Abela JRZ, Sakellaropoulo M, Taxel E (2007) Integrating two subtypes of depression: Psychodynamic theory and its relation to hopelessness depression in early adolescents. Journal of Early Adolescence 27:363–385. doi:10.1177/0272431607302004
Abela JRZ, Taylor G (2003) Specific vulnerability to depressive mood reactions in schoolchildren: the moderating role of self-esteem. Journal of Clinical Child and Adolescent Psychology 32:408–418. doi:10.1586/14737175.7.11s.S93
Abela JRZ, Webb CA, Wagner C, Ho MHR, Adams P (2006) The role of self-criticism, dependency, and hassles in the course of depressive illness: a multiwave longitudinal study. Personality and Social Psychology Bulletin (32)328–338. doi:10.1177/0146167205280911
Alexander JL, Dennerstein L, Woods NF, McEwen BS, Halbreich U, Kotz K, Richardson G (2007) Role of stressful life events and menopausal stage in wellbeing and health. Expert Rev Neurother 7:S93–S113. doi:10.1586/14737175.7.11s.S93
American Psychiatric Association (2000) Diagnostic and statistical manual of mental disorders, 4th edn. American Psychiatric Association, Washington, DC
Angst J, Sellaro R, Stolar M, Merikangas KR, Endicott J (2001) The epidemiology of perimenstrual psychological symptoms. Acta Psychiatr Scand 104:110–116
Avis NE, Brambilla D, McKinlay SM, Vass K (1994) A longitudinal analysis of the association between menopause and depression results from the Massachusetts women’s health study. Ann Epidemiol 4:214–220. doi:10.1016/1047-2797(94)90099-X
Avis NE, Crawford S, Stellato R, Longcope C (2001) Longitudinal study of hormone levels and depression among women transitioning through menopause. Climacteric 4:243–249
Baker A, Simpson S, Dawson D (1997) Sleep disruption and mood changes associated with menopause. J Psychosom Res 43:359–369. doi:10.1016/S0022-3999(97)00126-8
Baram DA (2005) Physiology and symptoms of menopause menopause: a mental health practitioner’s guide. American Psychiatric Publishing, Inc., Arlington, pp 15–32
Baron RM, Kenny DA (1986) The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol 51:1173–1182
Bastian LA, Smith CM, Nanda K (2003) Is this woman perimenopausal? J Am Med Assoc 289:895–902. doi:10.1001/jama.289.7.895
Baumeister RF, Heatherton TF (1996) Self-regulation failure: an overview. Psychoanal Inq 7:1
Baumeister RF, Bratslavsky E, Muraven M, Tice DM (1998) Ego depletion: is the active self a limited resource? J Pers Soc Psychol 74:1252–1265. doi:10.1037/0022-3514.74.5.1252
Baumeister RF, Zell AL, Tice DM (2007) How emotions facilitate and impair self-regulation? Handbook of emotion regulation. Guilford Press, New York, pp 408–426
Beck AT, Steer RA, Brown GK (1996) Manual for the Beck depression inventory-II. Psychological Corporation, San Antonio
Blatt SJ (1974) Levels of object representation in anaclitic and introjective depression. Psychoanal Study Child 29:7–157
Blatt SJ (2004) Experiences of depression: theoretical, clinical, and research perspectives, vol XIII. American Psychological Association, Washington, DC, 359 pp
Blatt SJ, D’Afflitti JP, Quinlan DM (1976) Depressive experiences questionnaire. New Haven, CT: Yale University Press.
Blatt SJ, Shichman S (1983) Two primary configurations of psychopathology. Psychoanal Contemp Thought 6:187–254
Blatt SJ, Zuroff DC (1992) Interpersonal relatedness and self-definition: two prototypes for depression. Clin Psychol Rev 12:527–562
Blatt SJ, Auerbach JS, Levy KN (1997) Mental representations in personality development, psychopathology, and the therapeutic process. Rev Gen Psychol 1:351–374
Blatt SJ, D’Afflitti JP, Quinlan DM (1976) Depressive experiences questionnaire. New Haven, CT: Yale University Press.
Born LE (2004) A new gender-specific measure of irritability. U Toronto, Canada
Born L, Steiner M (1999) Irritability: the forgotten dimension of female-specific mood disorders. Arch Women’s Ment Health 2:153–167
Born L, Steiner M, Koren G (2002) 30th annual meeting of north american society for psychosocial obstetrics and gynecology, february 20–23, 2002 Cancun, Mexico. Arch Women’s Ment Health 4:37–65
Born L, Koren G, Lin E, Steiner M (2008) A new, female-specific irritability rating scale. J Psychiatry Neurosci 33:344–354
Bosworth HB, Bastian LA, Kuchibhatla MN, Steffens DC, McBride CM, Skinner CS, Rimer BK, Siegler IC (2001) Depressive symptoms, menopausal status, and climacteric symptoms in women at midlife. Psychosom Med 63:603–608
Bromberger JT, Meyer PM, Kravitz HM, Sommer B, Cordal A, Powell L, Ganz PA, Sutton-Tyrrell K (2001) Psychologic distress and natural menopause: a multiethnic community study. Am J Public Health 91:1435–1442
Bromberger JT, Assmann SF, Avis NE, Schocken M, Kravitz HM, Cordal A (2003) Persistent mood symptoms in a multiethnic community cohort of pre- and perimenopausal women. Am J Epidemiol 158:347–356
Brown JP, Gallicchio L, Flaws JA, Tracy JK (2009) Relations among menopausal symptoms, sleep disturbance and depressive symptoms in midlife. Maturitas 62:184–189
Buchanan CM, Eccles JS, Becker JB (1992) Are adolescents the victims of raging hormones? Evidence for activational effects of hormones on moods and behavior at adolescence. Psychiatr Bull 111:62–107
Cohen LS, Soares CN, Vitonis AF, Otto MW, Harlow BL (2006) Risk for new onset of depression during the menopausal transition. Arch Gen Psychiatry 63:385–390
Ehring T, Fischer S, Schnulle J, Bosterling A, Tuschen-Caffier B (2008) Characteristics of emotion regulation in recovered depressed versus never depressed individuals. Personal Individ Differ 44:1574–1584. doi:10.1016/j.paid.2008.01.013
Fava GA (1987) Irritable mood and physical illness. Stress Med 3:293–299
Fava GA, Tossani E (2007) Prodromal stage of major depression. Early Interv Psychol 1:9–18. doi:10.1111/j.1751-7893.2007.00005.x
Fava GA, Grandi S, Canestrari R, Molnar G (1990) Prodromal symptoms in primary major depressive disorder. J Affect Disord 19:149–152
Freeman EW, Sammel MD, Liu L, Gracia CR, Nelson DB, Hollander L (2004) Hormones and menopausal status as predictors of depression in women in transition to menopause. Arch Gen Psychiatry 61:62–70
Freeman EW, Sammel MD, Lin H, Nelson DB (2006) Associations of hormones and menopausal status with depressed mood in women with no history of depression. Arch Gen Psychiatry 63:375–382
Gratz KL, Roemer L (2004) Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. J Psychopathol Behav Assess 26:41–54
Gross JJ, Munoz RF (1995) Emotion regulation and mental health. Clin Psychol Sci Pract 2:151–164
Halbreich U (2010) Women’s reproductive related disorders (RRDs). J Affect Disord 122(1–2):10–13
Harlow BL, Wise LA, Otto MW, Soares CN, Cohen LS (2003) Depression and its influence on reproductive endocrine and menstrual cycle markers associated with perimenopause: the Harvard study of moods and cycles. Arch Gen Psychiatry 60:29–36
Harlow SD, Crawford S, Dennerstein L, Burger HG, Mitchell ES, Sowers MF (2007) Recommendations from a multi-study evaluation of proposed criteria for staging reproductive aging. Climacteric 10:112–119
Harsh V, Meltzer-Brody S, Rubinow DR, Schmidt PJ (2009) Reproductive aging, sex steroids, and mood disorders. Harv Rev Psychiatry 17:87–102
Hunter MS (1990) Psychological and somatic experience of the menopause: a prospective study. Psychosom Med 52:357–367
Hunter MS (1992) The women’s health questionnaire: a measure of mid-aged women’s perceptions of their emotional and physical health. Psychol Health 7:45–54
Hyde JS, Mezulis AH, Abramson LY (2008) The ABCs of depression: integrating affective, biological, and cognitive models to explain the emergence of the gender difference in depression. Psychol Rev 115:291–313
Hylan TR, Sundell K, Judge R (1999) The impact of pre-menstrual symptomatology on functioning and treatment-seeking behavior: experience from the United States, United Kingdom, and France. J Women’s Health Gend Based Med 8:1043
Iacoviello BM, Alloy LB, Abramson LY, Choi JY (2010) The early course of depression: a longitudinal investigation of prodromal symptoms and their relation to the symptomatic course of depressive episodes. J Abnorm Psychol 119:459–467. doi:10.1037/a0020114
Kopala-Sibley DC, Santor DA (2009) The mediating role of automatic thoughts in the personality–event–affect relationship. Cogn Behav Ther 38(3):153–161. doi::10.1080/16506070802694644
Kopala-Sibley DC, Zuroff DC (2010) Proximal predictors of depressive symptomatology: perceived losses in self-worth and interpersonal domains and introjective and anaclitic mood states. Cogn Behav Ther 39:270–282. doi:10.1080/16506073.2010.501810
Kopala-Sibley DC, Zuroff DC, Russell JJ, Moskowitz DS, Paris J (2012) Understanding heterogeneity in borderline personality disorder: differences in affective reactivity explained by the traits of dependency and self-criticism. J Abnorm Psychol 121(3):680. doi:10.1037/a0028513
Kumari M, Stafford M, Marmot M (2005) The menopausal transition was associated in a prospective study with decreased health functioning in women who report menopausal symptoms. J Clin Epidemiol 58:719–727
Luyten P, Sabbe B, Blatt SJ, Meganck S, Jansen B, De Grave C, Maes F, Corveleyn J (2007) Dependency and self-criticism: relationship with major depressive disorder, severity of depression, and clinical presentation. Depress Anxiety 24:586–596
Maartens LWF, Knottnerus JA, Pop VJ (2002) Menopausal transition and increased depressive symptomatology: a community based prospective study. Maturitas 42:195–200
Mahnert FA, Reicher H, Zalaudek K, Zapotoczky HG (1997) P.1.078 Prodromal and residual symptoms in recurrent depression: preliminary data of a long-term study under prophylactic treatment condition. Eur Neuropsychopharmacol 7:S159–S160
McKinlay SJ, Brambilla DJ, Posner JG (1992) The normal menopause transition. Am J Hum Biol 4:37–46
Mongrain M, Zuroff C (1989) Cognitive vulnerability to depressed affect in dependent and self-critical college women. Journal of Personality Disorders, 3, 240–251. doi:10.1521/pedi.1989.3.3.240
Mongrain M, Zuroff DC (1994) Ambivalence over emotional expression and negative life events: mediators of depressive symptoms in dependent and self-critical individuals. Personal Individ Differ 16:447–458
Mongrain M, Vettese LC, Shuster B, Kendal N (1998) Perceptual biases, affect, and behavior in the relationships of dependents and self-critics. J Pers Soc Psychol 75:230–241
Muller D, Judd CM, Yzerbyt VY (2005) When moderation is mediated and mediation is moderated. J Pers Soc Psychol 89:852–863
NAMS (2010) Menopause practice: a clinician’s guide, 4th edn. The North American Menopause Society, Ohio
Nietzel MT, Harris MJ (1990) Relationship of dependency and achievement/autonomy to depression. Clin Psychol Rev 10:279–297
Powell L (1996) Psychological changes in the perimenopausal transition. Maturitas 25:77–77
Reed S, Ludman E, Newton K, Grothaus L, Nekhlyudov L, Spangler L, LaCroix A (2009) Depressive symptoms and menopausal burden in the midlife. Maturitas 63:S34–S34
Ryff CD (1989) Happiness is everything, or is it? Explorations on the meaning of psychological well-being. J Pers Soc Psychol 57:1069–1081
Ryff CD (1991) Possible selves in adulthood and old age: a tale of shifting horizons. Psychol Aging 6:286–295. doi:10.1037/0882-7974.6.2.286
Ryff CD (1995) Psychological well-being in adult life. Curr Dir Psychol Sci 4:99–104
Santor DA, Zuroff DC, Fielding A (1997a) Analysis and revision of the depressive experiences questionnaire: examining scale performance as a function of scale length. J Personal Assess 69:145–163
Santor DA, Zuroff DC, Mongrain M, Fielding A (1997b) Validating the McGill revision of the depressive experiences questionnaire. J Personal Assess 69:164–182
Schleifer LA (2003) The role of estrogen in the mood-lowering effects of acute tryptophan depletion in postmenopausal women. McGill U, Canada
Schmidt PJ, Murphy J, Haq N, Rubinow D, Danaceau M (2004) Stressful life events, personal losses, and perimenopause-related depression. Arch Women’s Ment Health 7:19–26
Schneider HPG, Heinemann LAJ, Thiele K (2002) The menopause rating scale (MRS): cultural and linguistic translation into English. Life Med Sci. doi:10.1072/LO0305326
Sommer B, Avis N, Meyer P, Ory M, Madden T, Kagawa-Singer M, Mouton C, Rasor NON, Adler S (1999) Attitudes toward menopause and aging across ethnic/racial groups. Psychosom Med 61:868–875
Soules MR, Sherman S, Parrott E, Rebar R, Santoro N, Utian W, Woods N (2001) Executive summary: stages of reproductive aging workshop (STRAW). Fertil Steril 76:874–878
Sowers MF, Crawford SL, Sternfeld B, Morganstein D, Gold EB, Greendale GA, Evans D, Neer R, Matthews K, Sherman S, Lo A, Weiss G, Kelsey J (2000) SWAN: a multicenter, multiethnic, community-based cohort study of women and the menopausal transition. In: Lobo RA, Kelsey J, Markus R (eds) Menopause: biology and pathobiology. Academic Press, San Diego, pp 175–188
Steer RA, Ball R, Ranieri WF, Beck AT (1997) Further evidence for the construct validity of the Beck depression inventory-II with psychiatric outpatients. Psychol Rep 80:443–446
Strauman TJ (2002) Self-regulation and depression. Self Identity 1:151–157
Thompson RA (1994) Emotion regulation: A theme in search of definition. Monographs of the society for research in child development, 59(2-3), 25–52
Tice DM, Bratslavsky E, Baumeister RF (2001) Emotional distress regulation takes precedence over impulse control: if you feel bad, do it! J Pers Soc Psychol 80:53–67
van Praag HM (1996a) Faulty cortisol/serotonin interplay. Psychopathological and biological characterisation of a new, hypothetical depression subtype (SeCA depression). Psychiatry Res 65:143–157
van Praag HM (1996b) Serotonin-related, anxiety/aggression-driven, stressor-precipitated depression. A psychobiological hypothesis. Eur Psychiatry 11:57–67
Vettese LC, Mongrain M (2000) Communication about the self and partner in the relationships of dependents and self-critics. Cogn Ther Res 24:609–626. doi:10.1023/A:1005587009681
Vujanovic A, Zvolensky M, Bernstein A (2008) The interactive effects of anxiety sensitivity and emotion dysregulation in predicting anxiety-related cognitive and affective symptoms. Cogn Ther Res 32:803–817. doi:10.1007/s10608-007-9148-8
Werner K, Gross JJ (2010) Emotion regulation and psychopathology: a conceptual framework emotion regulation and psychopathology: a transdiagnostic approach to etiology and treatment. Guilford Press, New York, pp 13–37
Wilk CA, Kirk MA (1995) Menopause: a developmental stage, not a deficiency disease. Psychother Theory Res Pract Train 32:233–241
Young MA, Watel LG, Lahmeyer HW, Eastman CI (1991) The temporal onset of individual symptoms in winter depression: differentiating underlying mechanisms. J Affect Disord 22:191–197
Zuroff DC, Mongrain, M. (1987). Dependency and self-criticism: Vulnerability factors for depressive affective states. J Abnorm Psychol 96:14–22. doi:10.1037/0021-843X.96.1.14
Zuroff DC, Igreja I, Mongrain M (1990) Dysfunctional attitudes, Dependency and Self-Criticism as predictors of depressive mood states: A 12-month longitudinal study. J Cogn Ther & Res 14:315–326
Zuroff DC, Moskowitz DS, Wielgus MS, Powers TA, Franko DL (1983) Construct validation of the dependency and self-criticism scales of the depressive experiences questionnaire. J Res Personal 17:226–241
Zuroff DC, Mongrain M, Santor DA (2004) Conceptualizing and measuring personality vulnerability to depression: comment on Coyne and Whiffen (1995). Psychol Bull 130:489–511
Zuroff DC, Blatt SJ, Sanislow CA III, Bondi CM, Pilkonis PA (1999) Vulnerability to depression: reexamining state dependence and relative stability. J Abnorm Psychol 108:76–89
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mauas, V., Kopala-Sibley, D.C. & Zuroff, D.C. Depressive symptoms in the transition to menopause: the roles of irritability, personality vulnerability, and self-regulation. Arch Womens Ment Health 17, 279–289 (2014). https://doi.org/10.1007/s00737-014-0434-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00737-014-0434-7