Abstract
This pilot study explores the effects of a brief individual psychoanalytic therapy on perinatal depressive symptoms. This intervention is based on the Geneva’s mother–infant intervention model. A sample of 129 pregnant women was recruited in Geneva (Switzerland) and screened for depressive symptoms with two instruments: the ‘Edinburgh postnatal depression scale’ (EPDS) and the ‘Dépistage anténatal de la dépression postnatale’. A group of 40 women presenting depressive symptoms (treatment group) participated in a four-session intervention called ‘Psychotherapy centred on parenthood (PCP)’. It consists in two antenatal and two postnatal sessions and is focussed on changing problematic representations of parenthood. This treatment group was compared to a control group of 88 women without depressive symptoms and following the usual obstetrical care. The main outcome measure was EPDS at 3 and 6 months after delivery. The ‘Global assessment functioning scale’ was administered at the end of each therapeutic session. The ‘Parent–infant relationship global assessment scale’ was administered at the two postnatal sessions in order to explore if PCP was also effective in preventing the potential negative effects of depression on mother–infant relationship. Results show that in the treatment group (N = 31), EPDS scores dropped from 12.8 to 4.8; none of these women met the EPDS cut-off score of 12 at 3 and 6 months postpartum. Mother–infant relationship was well adapted for all 31 dyads at the end of the intervention. These results suggest that PCP is a promising intervention for treating perinatal depression and helping mothers engaging in parenting.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Transition to parenthood is a challenging period of life demanding important adjustments to the future parents and leading to an increased vulnerability to depression. Perinatal mental health problems are recognised as a major public health issue (Austin et al. 2008), with as many as 20 % of pregnant women presenting depressive symptoms (Marcus et al. 2003) and 10 % to 15 % of new mothers suffering from depression during the first year after delivery. Moreover, maternal mental health problems are among the leading causes of maternal death during this period (Austin et al. 2007). Even a low baseline level of depressive symptoms in the peripartum may lead to great suffering for the mother and also for the other family members, especially the offspring. Postpartum depression has well-known adverse consequences on the mother’s and her infant’s functioning, as well as on the quality of the mother–infant relationship (Stuart and Clark 2008). Mothers are less sensitive and responsive to their child, and they tend to be less affectively attuned and less responsive to their infant’s needs. Infants present less vocal, visual, and corporal interactions, more crying, feeding, and sleeping disorders (Righetti-Veltema et al. 2002). Many mothers are still depressed 1 year later (O’Hara 2009). Even when the mother’s remission occurs, infants may still be at risk of presenting disturbances such as an insecure attachment, behavioural problems, cognitive, and verbal delays and emotional dysregulations (Righetti-Veltema et al. 2003). Moreover, untreated depression presents a high risk of relapse (Beck 2003). Antenatal mood disorders are also associated with several pregnancy complications such as excessive weight gain, increased substance use, or premature birth (Marcus 2009). In addition, untreated antenatal depression may be complicated by smoking, poor antenatal care, or self-harm, all of which are serious risk factors for the foetus (Condon 2010).
Continuity between prenatal and postnatal depression suggests that they can be seen as a unique entity. According to Austin et al. (2007), 30 % to 40 % of postpartum women with depressive symptoms had elevated depressive scores already during pregnancy, suggesting there is a continuation of pre-existing symptoms into the postnatal period (Pearson et al. 2010). Moreover, prenatal depression is the major risk factor identified for future postpartum depression: 40 to 50 % of depressive pregnant women will present depressive symptoms during the first postpartum months (Righetti-Veltema et al. 1998). Therefore, the evidence-based report of the US Agency of Health-Care Research and Quality proposed the notion of perinatal depression (PD) to define an episode of major or minor depression occurring during pregnancy or the first 12 months after birth (Gaynes et al. 2005).
Despite all the knowledge about PD and its adverse health consequences, depression is one of the most underdiagnosed and untreated conditions during pregnancy (Condon 2010). The professionals caring for pregnant women do not always investigate the presence of depressive symptoms, or they tend to attribute these symptoms to pregnancy or recent delivery like the women themselves do. Recently, Marcus (2009) found that only 18 % of women who meet criteria for major depressive disorder receive a treatment during the perinatal period. Few early interventions have been validated for PD (Austin 2004; Milgrom et al. 2011). These interventions may have different theoretical frames (psychosocial, educational, cognitive–behavioural, interpersonal therapy) and use individual and/or group sessions. Pharmacological approaches are not always well accepted by pregnant or nursing women because of the risks for the foetus and the infant (Goodman and Tully 2009). More recently, Fitelson et al. (2010) pointed out long-term effects of early drug exposure on the developing brain.
Most studies support that psychological interventions are effective during the perinatal period (O’Hara et al. 2000; Horowitz and Goodman 2004). This has been confirmed by Cuijpers et al. (2011) in their recent meta-analysis. Interpersonal, cognitive–behavioural, or psychodynamic psychotherapy and other supportive interventions, such as telephone-based support and counselling by a health visitor or partner support, have proved to be more effective than usual care or a waiting list (Fitelson et al. 2010).
Even if several of these studies present methodological limitations (small sample size, high attrition rate, etc.), they all tend to show that individual treatments seem to be more beneficial than group-based interventions (Dennis 2010). Brugha et al. (2000) and Austin et al. (2008) found no benefit from their interventions in terms of rates of postnatal depression. Spinelli and Endicott (2003) focussed on the impact of treatment in reducing depressive symptoms during pregnancy and observed that interpersonal psychotherapy is an effective method for treating depression during pregnancy. Grote used a brief interpersonal psychotherapy and showed that women receiving this intervention displayed a significant reduction of depression diagnosis before childbirth and at 6 months postpartum. Women also presented significant improvement in social functioning at 6 months postpartum, indicating that antenatal interventions may also have a protective impact after birth (Grote et al. 2009).
Surprisingly, few antenatal interventions for PD have focussed specifically on preparing for parenthood or on the future mother–infant relationship. More recently, Milgrom et al. (2011) developed an intervention aimed both at reducing depression and anxiety symptoms and at improving parent–infant adjustment. The principal target of this intervention is to enhance emotional well-being and to develop the coping skills of the women and their partners in the transition to parenthood. This program, addressed to a community-based sample, is composed of a nine-unit self-guided workbook with weekly telephone support. An additional community-networking component was implemented to allow social support or contact to health professionals in order to facilitate the access to treatment of current antenatal depression or anxiety. This antenatal program was effective in reducing both postnatal depression and anxiety and parenting stress.
There is evidence that treating only PD may not be sufficient in protecting children against poor long-term outcomes. Thus interventions for this disorder should also include an approach focussed on the parenting role. Early mother–infant interventions are well adapted to this aim because they focus on mother–infant interactions and on maternal skills in order to increase sensitivity and responsiveness (Cicchetti et al. 2000). Clark et al. (2003) developed an original intervention called ‘Mother–infant therapy group’ centred not only on the mother’s depressive symptoms but also on the infant’s emotional regulation and developmental skills and on the quality of the mother–infant and family relationships. This intervention addresses mother–infant interactions because women experiencing PD are often impaired in their ability to provide sensitive responses for their infant. Women undergoing this intervention reported significantly fewer depressive symptoms and experienced their infants as more reinforcing than the depressed mothers on a waiting list. Moreover, the mothers participating in this intervention were rated as exhibiting more positive affective involvement in the interactions with their infants than the wait-list controls. These results show there is a need to develop interventions for PD focussing both on depressive symptoms and on preparing to parenthood.
In order to treat PD and to prevent its deleterious effects, an intervention based on the Geneva’s mother–infant psychotherapeutic model (Cramer 1998; Manzano et al. 1999) called ‘Psychotherapy centred on parenthood’ (PCP), was recently developed. This intervention aims at treating maternal depressio already during the antenatal period and at supporting depressive mothers in parenting during early postnatal period. PCP is a brief four-session individual intervention including two prenatal and two postnatal sessions focussing on maternal representations linked to parenthood. These representations are central, as they will assist the mother in understanding her infant’s emotional states and responding to its needs in order to allow the development of affect-regulation capacities. Maternal representations of parenting and of the foetus start to develop throughout pregnancy. During the peripartum, women are more accessible to modify their representations and skills. If maternal representations present important distortions or an overemphasis of negative emotions, they can seriously interfere with her psychological engagement into pregnancy. Psychoanalytically oriented research has shown that, during pregnancy, the woman’s representations of herself, foetus and own mother, evolve in a way that reflect her relational history (Fava Vizziello et al. 1993). These internal unconscious representations impact on the way the mother experiences her pregnancy; they are frequently associated with depression and/or anxiety, as with difficulties in engaging in parenting. The symptoms’ improvement is seen as a result of the woman gaining insight on her internal conflicting relationships and on her emotional states and behaviours. This gain of insight induces a reorganisation of her unbalanced representations as well as an improvement of her mood, allowing her to engage more appropriately in parenting.
The classic brief psychoanalytic intervention developed by Cramer focussing both on maternal representations and on the emerging mother–infant relationship has shown to have a significant effect both on postpartum depression (Cramer 1993) and on the infant’s symptoms (Cramer et al. 1996) when it is proposed during the first years of life. Our pilot study explores the effects of the intervention when proposed throughout antenatal and early postnatal period on the women’s depressive symptoms and on the quality of her relationship with the infant.
Method
Design
In a longitudinal study, we evaluate women with depressive symptoms from pregnancy to 6 months postpartum and early mother–infant relationships in order to assess the effects of a brief psychoanalytic intervention both on the mother’s emotional state and on the mother–infant interactions. The pregnant women were enrolled between July 2006 and July 2007; they were referred by health professionals (gynaecologists, paediatricians, midwives) of the city of Geneva (Switzerland). All French-speaking pregnant women were included, except those with a known severe psychiatric pathology (substance abuse, bipolar disorder, schizophrenia, or mental retardation). The Ethic Committee of the Geneva University Hospital approved the study protocol in May 2006.
The study included an initial screening interview (T1) during which participants provided written informed consent and were screened for depressive symptoms using two questionnaires, the ‘Edinburgh postnatal depression scale’ (EPDS) developed by Cox et al. (1996) and the ‘Dépistage anténatal de la dépression postnatale’ (DADP; Nanzer and Righetti-Veltema 2009). Women presenting a positive score on one or both of the questionnaires (i.e., EPDS ≥ 12 and DADP ≥ 3) were assigned to the treatment group and participated in the four-session PCP intervention: two prenatal (S1–S2) and two postnatal sessions (S3–S4). Women presenting no criteria for PD continued to receive outpatient usual antenatal and postnatal care and were assigned to the control group. The outcome measure (EPDS) was administered to the two groups at baseline (T1) and at 3 (T2) and 6 months (T3) after birth. Measures requiring an in-depth clinical investigation were assessed by the therapists at the end of each clinical session (the ‘Global assessment functioning scale’, GAF) or at the end of the two postnatal sessions (the ‘Parent–infant relationship global assessment scale’, PIRGAS). Assessment and intervention schedule is summarised in Fig. 1.
Assessment and intervention schedule. T1: first assessment interview (screening measures), T2 second assessment interview (outcome measures at 3 months), T3 third assessment interview (outcome measures at 6 months), S1 first intervention session, S2 second intervention session, S3 third tintervention session, S4 fourth intervention session
Sample
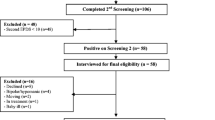
Of the 128 pregnant women who participated at the first screening interview, 40 presented depressive symptoms and were assigned to the treatment group and 88 had no criteria for PD and were assigned to a control group (see Fig. 2). Of the 40 pregnant women assigned to the treatment group, 31 (77.5 %) attended the follow-up 3 months after birth (T2). Four women never came to the first treatment session and 5 left the treatment after the first or the second session. At the 6 months follow-up (T3), 25 women (62.5 %) accepted to participate and 6 could not be joined. In the control group, 52 of the 88 women participated at the 3 months follow-up (T2) and 41 were present at the 6 months follow-up (T3). Women of the treatment group had a mean gestational age of 29 weeks (SD = 4.05) at the first treatment session (S1) and a gestational age of 33 weeks (SD = 4.4) at the second session (S2). The two postnatal sessions (S3–S4) occurred at 4.9 weeks (SD = 1.9) and 9.4 weeks (SD = 3.3) after birth. The sociodemographic characteristics of the population are summarised in Table 1. Social and educational level were medium to high. Both groups were similar in age, gestational age, and parity. Within the treatment group, we found slightly more women living alone and more women with a lower educational level or with a non-European origin.
Measures
Edinburgh postnatal depression scale
The EPDS is a questionnaire widely used to measure depressive symptoms during the perinatal period. According to Murray and Carothers (1990), the EPDS is a reliable method to identify depressive mothers (sensitivity 81.1 % with a limit at 12.5). It has also been validated during pregnancy (Murray and Cox 1990). We used the French version validated by Guedeney and Fermanian (1998). A cut-off score of 12 points was used to screen women presenting depressive symptoms.
Dépistage antenatal de la dépression postnatale
The DADP questionnaire is an instrument developed in Switzerland during an epidemiologic prospective study on PD. In this study, 570 pregnant women were interviewed during the last trimester of pregnancy and at 3 and 18 months postpartum (Righetti-Veltema et al. 1998). It contains six items: four concern psychological aspects (blaming oneself, difficulty in falling asleep or staying asleep, feeling lonely, feeling that others do not understand you or are unsympathetic); two items refer to somatic issues (itching and lower back pain). In its final version, the DADP (Nanzer and Righetti-Veltema 2009) contains the same six items enhanced with a better presentation in order to allow an easier implementation. This questionnaire enables a rapid detection of pregnant women presenting mild, non-identified depressive symptoms and recognises the importance of somatic issues during pregnancy, an aspect not covered by the EPDS.
Global assessment functioning
The GAF is a numeric scale included in the DSM-IV generally used by mental health clinicians and physicians to rate the social, occupational, and psychological functioning of adults. This scale rates the person’s functioning during a specified period on a continuum from psychiatric illness to health. The scale value ranges from 1 (hypothetically sickest person) to 100 (hypothetically healthiest person).
Parent–infant relationship global assessment scale
The PIR-GAS is a 90 point scale used to assess the quality of infant–parent relationship based on a continuum from well adapted to grossly impaired. This scale is to be completed only after a thorough clinical evaluation of the infant’s problems. It is designed to help clinicians recognise individual differences in ways infants and young children relate to their primary care. This scale is frequently used to assess the level of the relationship at the time of the evaluation and at the end of the treatment. The PIR-GAS is a supplement to the DC-03 diagnostic classification (Zero to three 2005).
PCP protocol
The treatment group women participated in a four-session individual psychotherapy based on Cramer and Palacio Espasa’s manual (Cramer 1995) of mother–infant therapy which focusses on parental representations. We adapted this protocol to the prenatal period and developed a PCP. It consists of two antenatal sessions (during the second or third trimester of pregnancy, depending on the moment of referral and on the clinical needs) and two postnatal sessions (1 and 2 months after delivery). The treatment goal is to identify and modify the nature of the core conflicting themes concerning motherhood which are responsible for the woman’s feelings of guilt and mood disturbances. The psychiatrists involved in this study followed a procedure described in detail in a manual actually in press (Nanzer et al. 2012). They met on a monthly basis in order to specify the main steps of each session and to analyse the difficulties found during the sessions. They are all well experienced psychoanalytic psychiatrists with more than 10-year experience in parent–infant psychotherapy in a university hospital.
In this intervention, the therapist is active in creating an alliance and in remaining centred on the identified focus. The identification of the focus allows the mother to recognise and elaborate the distortions of her representations concerning herself and/or her future baby. These unbalanced representations are frequently related to the woman’s past history and to her relationship with her own mother. Free associations and dream narratives are encouraged in order to identify the unconscious representations in connection with the emerging parenthood: what parent am I going to be? What child am I going to have? What kind of parents did I have? What kind of a child was I? What was my attitude toward siblings?
Clinical practice of brief mother–infant psychotherapy shows that the main psychic themes observed during pregnancy and early motherhood are: (1) the fear of not being a good mother, (2) the fear to reproduce the patterns that the mother suffered during her childhood, (3) the existence of a too high maternal ideal. These conflicts are connected to unconscious or non-elaborated bereavements of the woman’s past, with more or less conscious reproaches addressed to her parents, which are returned against herself when she becomes a mother. The intervention leads to an improvement of the mother’s mood by relieving the anxiety and guilt, allowing her to engage in an active psychological process and to be emotionally ready for motherhood. The four main steps in the therapy’s process are described in Table 2.
During the first session, the therapist explores with the mother the themes and representations concerning parenthood. The woman is free to associate while the therapist listens in an analytic, nondirective way. The therapist’s aim is to establish the main focus of the psychic conflicts. During the end of the first session and during the second session, the therapist is more active and helps the woman to elaborate her conflicting representations and the repetitions of past schemes. Sessions 3 and 4 occur after birth and allow the therapist to work not only on maternal representations but also on the actual interactions between the mother and her infant. At that period, the antenatal internal conflicts are frequently externalised and acted out in the mother–baby relationship. In these sessions, the therapist’s work is centred on helping the mother recognise these aspects. Sometimes, new preoccupations appear after the baby’s birth and the third session frequently enables the new mother to express them. Finally, the last session permits the mother to better elaborate these themes and to prepare to separation.
Analysis
Longitudinal data were submitted for statistical elaboration using a 2 (group: treatment versus non-treatment) × 3 (time: T1, T2, T3) repeated measures analysis of variance for the outcome measure (EPDS) in order to investigate the interaction between time and group. Time effect was evaluated in order to investigate changes within groups. In case of a significant group by time or time effect, a two-tailed t-test (probability level p < .05) was performed to investigate significance of between group differences or significance within group changes over time.
To assess clinical impact of treatment, we evaluated the degree to which the means of both groups shifted from dysfunctional to functional cut-off EPDS scores. Significant differences between groups in the ratio of cases moving from clinical to nonclinical range were calculated using a χ² test. To check if significant differences were observed in GAF and PIRGAS scores during and after treatment, a two-tailed t-test (probability level p < .05) was performed. The evolution of the quality of parent–infant relationship between S2 and S3 was investigated by a two-tailed t-test (probability level p < .05) performed on the PIRGAS score. Data were analysed with SPSS 15.0 for Windows.
A power analysis for t-tests was conducted a priori. For T1, with a probability of finding an effect size of d = 2, the probability of finding a significant difference between the two groups is 99 %. Between T1 and T2, for the treatment group, with a probability of an effect size of d = 2 (assuming correlation of 0.5 and slightly lower than observed mean), the probability of finding a significant effect is above 99 %. These calculations were made with G-Power 3.12.
Results
Changes on EPDS scores
Means, standard deviations, and values of significance of the outcome measure (EPDS score) concerning maternal depression are presented in Table 3. The analysis of longitudinal data (Table 3) shows there are significant group by time and time effects. Regarding the significant interaction between time and group, t-tests between groups show significant differences between T1 and T2 as a consequence of major improvement of the EPDS scores of the women assigned to the treatment group: the mean EPDS scores of women with depressive symptoms joined the baseline represented by the EPDS score of the control group (who showed no significant changes between T1 and T2). From T2 to T3, no significant differences were found between the two groups indicating there was no major change between the 3 and 6 months’ examination. The mean score of the treated women continues to slightly decrease several months after the end of the treatment.
Concerning time effect, the t-test within groups shows a significant change from T1 to T2 and between T1 and T3 only for the treatment group. From T2 to T3, no significant changes of EPDS scores were observed. These results demonstrate that major changes of depressive symptoms occurred between the beginning and the end of the treatment. Moreover, this improvement is maintained 3 months later (T2).
Evolution of clinical EPDS scores
The treatment group shows a statistically significant change in clinical EPDS scores (EPDS > 12) between T1 and T2: whereas before treatment 78 % of the women presented a clinical score, after the intervention all the women present a nonclinical score (EPDS ≤ 12). This result is maintained with no clinical EPDS score observed at the 6-month interview. No significant shift is observed in the control group, although three control mothers presented a clinical EPDS score at T2 or T3.
Changes in GAF scores
Table 4 presents the mean scores of the GAF at each of the four treatment sessions. They slightly improve between sessions 2 and 3 changing from a moderate (GAF < 70) to a good level of functioning (GAF ≥ 70) after delivery. These changes are statistically significant and indicate that the treatment had a positive impact on the women’s global functioning despite the important adaptation required by maternal role during the early postpartum period.
Changes in PIRGAS scores 3 and 6 months
Table 5 presents the mean scores of the PIRGAS at each postpartum session. The mean scores of the two postpartum sessions are 80.5 (SD 6.3) and 79.7 (SD 14.1; ANOVA .07 NS).
In the majority of the mother–infant dyads, the relationship is considered as well adapted (PIR-GAS ≥ 70) at the last session, indicating that mothers participating in the intervention were able to engage in parenthood in a satisfying way: they were able to establish an adjusted relationship with their infants, despite the depressive symptoms presented during the antenatal period.
Discussion
The importance of early detection and referral of PD is actually well documented, but these practices are still missing in clinical settings. In our study, 50 % of the 129 women never heard about the existence of postpartum depression before their participation in the study, even if they had already suffered from depression. These facts indicate the urgent need for more information concerning PD and its treatment, addressed not only to future parents but also to their caregivers in perinatal services.
The results of this pilot study indicate that our brief PCP leads to a decrease of the mothers’ depressive symptoms and to an improvement of their global functioning. It corroborates the results obtained by Milgrom et al. (2011) with a different method, described in ‘Introduction’. Their focus also concerned parenthood. In the same way, it confirms the results obtained by Spinelli and Endicott (2003) and Grote et al. (2009) concerning the beneficial impact after childbirth on the mother and her infant of interpersonal psychotherapy during pregnancy. In our study, none of the women with prior depressive symptoms met criteria for PD after the intervention and their mean score joined the level of the nonclinical control group. Furthermore, the EPDS scores of the clinical mothers continued to decrease after the end of the intervention, confirming previous findings on the long term effect of psychodynamic psychotherapy (Leichsenring et al. 2004). The well-adapted mother–infant relationship observed in the treatment dyads at the end of the intervention suggests that the frequent deleterious effects of depression on mother–infant interactions have been prevented by the intervention which focusses on relational concerns. Its briefness (four sessions) has shown to be appropriate to protect mothers and their infant from psychological distress during the early perinatal period. In a qualitative questionnaire, at the end of the intervention, most women established that four sessions were enough even when they presented serious depressive symptoms before the intervention. Nevertheless, the number of sessions of PCP can be adapted to the mothers’ psychological distress. Further studies with larger samples should be conducted to provide more solid results concerning the benefits of PCP.
This intervention has proved to be well adapted to the perinatal period because it is centred on parenthood and on the difficulties changing identity when becoming a mother. By questioning and changing distorted maternal representations, PCP reduces maternal feelings of guilt and the associated anxiety and depressive symptoms. It focusses on representations linked to motherhood, which is of particular concern to the future mothers. This entails they are more disposed to investigate their inner world and representations during this particular period.
PCP presents the advantage of beginning during pregnancy, when the future mothers are particularly receptive to a personal psychotherapeutic work. The continuation of therapy during the postnatal period allows the therapist to work not only on maternal representations but also on the actual interactions between the mothers and their infant. The birth of a baby may induce the arousal of new maternal preoccupations and symptoms that can be specifically addressed in the postnatal sessions. Although this intervention requires experimented psychotherapists, PCP can also be implemented as a service-learning model with experienced clinicians providing supervisions. This could be a good opportunity for young child and adult psychotherapists to learn about infant development, parent–infant relationship, and parenthood as a crucial adult developmental phase.
Many authors have emphasised the problem of the high attrition rate during perinatal period and have pointed out the necessity to evaluate the women’s acceptation of this type of intervention. In our study, PCP was well accepted by all women who underwent the four sessions of the intervention. We noted a low attrition rate (10 %) compared to those generally observed during this period. This could be explained by the time-limited design of the intervention, its focus on motherhood, and the participation of the infant in the postnatal sessions. All these aspects are particularly important for the mothers.
However, this study has several methodological limitations derived in part from its clinical setting. The principal limitation is the lack of a control group including depressive women who did not undergo the intervention. For ethical reasons, PCP was proposed to all identified depressed pregnant women in order to minimise the effects of depression on the developing foetus and to avoid future disturbances of the mother–infant relationship. Moreover, the GAF and the PIRGAS have been completed by the therapist after the intervention sessions; in this way, these outcomes were not available for the nontreatment group.
Another limitation concerns the sociodemographic characteristics of the sample which include an important percentage of women with a mean/high socioeconomic status. A future randomised trial should enroll more socially and financially disadvantaged women in order to assess the feasibility of PCP with these women, known to be more difficult to engage in psychoanalytic interventions. Another aspect not covered here is the assessment of the mothers’ anxiety symptoms. During this study, we observed that mothers presenting depressive symptoms also presented a high level of anxiety; this important comorbidity during the perinatal period has also been identified in other studies. Future researches on PD should also include an assessment of maternal anxiety as recent evidence indicates that maternal anxiety may have an important impact on the foetus’ developing brain. They should also investigate the impact of PCP on anxiety symptoms. A 1-year follow-up of the mother–infant relationship and of the mother’s symptoms can be proposed to future studies in order to investigate the long-term maintenance of this intervention’s benefits. Although the mother–infant relationship was assessed, another aspect that can be evaluated is the infant’s global development in order to investigate the deleterious implications of PD on the infant’s cognitive and emotional functioning.
The noninclusion of fathers is also a limitation given the importance of the psychological changes occurring in the process of fatherhood. Fathers were not included in the present study because of the difficulty to obtain their collaboration during the perinatal period. PCP can still be addressed to fathers encountering difficulties with parenting. Recent studies tend to show that the prevalence of depression in new fathers is higher when their wives are also depressed. There is a sort of ‘contagion’ effect of the depressive symptoms between mothers and fathers especially during the postnatal period, with a peak between 3 and 6 months after birth (Paulson and Bazemore 2010). The mechanism of this possible contagion is not yet well understood, but it could be partially explained by the increase of the tasks and responsibilities assigned to the fathers, when the mothers are depressed and fear they would harm themselves or their babies. The fathers’ depression and anxiety symptoms should thus be better screened in order to identify and treat paternal distress and avoid its serious consequences for the other family members. Future interventions for PD need to integrate fathers given the important interdependence between maternal and paternal mental health during this period.
In conclusion, this study shows that our brief psychoanalytic intervention leads to a significant decrease of depressive maternal symptoms during the perinatal period. PCP is a perinatal intervention that has the advantage of being brief, specifically focussed on mother–infant relationship and administrable already during pregnancy. During this period, women are more open to therapy than after delivery when a large part of their attention is focussed on infant care. Starting interventions during the prenatal period is an important issue because it improves maternal well-being during pregnancy and helps to prevent the foetus from the potential negative effects of maternal depression. Unlike most interventions addressed to the perinatal period, PCP allows continuity between prenatal and postnatal periods and can include both parents according to their needs. This intervention also focusses on early parent–infant interactions in order to improve the developmental course of infants of depressed mothers. Its effectiveness concerns not only the improvement of the mother’s symptoms but also the quality of the parent–infant relationship.
References
Austin MP (2004) Antenatal screening and early intervention for ‘perinatal’ distress, depression and anxiety: where to from here? Arch Womens Ment Health 7(1):1–6
Austin MP, Tully L et al (2007) Examining the relationship between antenatal anxiety and postnatal depression. J Affect Disord 101(1–3):169–174
Austin MP, Priest SR et al (2008) Antenatal psychosocial assessment for reducing perinatal mental health morbidity. Cochrane Database Syst Rev 4:CD005124
Beck CT (2003) Postpartum depression predictors inventory—revised. Adv Neonatal Care 3(1):47–48
Brugha TS, Wheatley S et al (2000) Pragmatic randomized trial of antenatal intervention to prevent post-natal depression by reducing psychosocial risk factors. Psychol Med 30(6):1273–1281
Cicchetti D, Rogosch FA et al (2000) The efficacy of toddler–parent psychotherapy for fostering cognitive development in offspring of depressed mothers. J Abnorm Child Psychol 28(2):135–148
Clark R, Tluczek A et al (2003) Psychotherapy for postpartum depression: a preliminary report. Am J Orthopsychiatry 73(4):441–454
Condon J (2010) Women’s mental health: a ‘wish-list’ for the DSM V. Arch Womens Ment Health 13(1):5–10
Cox JL, Chapman G et al (1996) Validation of the Edinburgh postnatal depression scale (EPDS) in non-postnatal women. J Affect Disord 39(3):185–189
Cramer B (1993) Are postpartum depressions a mother–Infant relationship disorder? Infant Ment Health J 14(4):283–297
Cramer B (1995) Short-term dynamic psychotherapy for infant and their parents. Child Adolesc Psychiatr Clin N Am 4:649–659
Cramer B (1998) Mother–infant psychotherapies: a widening scope in technique. Infant Ment Health J 19(2):151–167
Cramer B, Robert-Tissot C, Stern D, Rusconi Serpa S, De Muralt M, Besson G, Palacio Espasa F, Bachmann J-P, Knauer D, Berney C, d’Arcis U (1996) Outcome evaluation in brief mother–infant psychotherapy: a preliminary report. Infant Ment Health J 11(3):278–300
Cuijpers P, Geraedts AS et al (2011) Interpersonal psychotherapy for depression: a meta-analysis. Am J Psychiatry 168(6):581–592
Dennis CL (2010) Postpartum depression peer support: maternal perceptions from a randomized controlled trial. Int J Nurs Stud 47(5):560–568
Fava Vizziello G, Antonioli ME et al (1993) From pregnancy to motherhood: the structure of representative and narrative change. Infant Ment Health J 14:4–16
Fitelson E, Kim S et al (2010) Treatment of postpartum depression: clinical, psychological and pharmacological options. Int J Womens Health 3:1–14
Gaynes BN, Gavin N et al (2005) Perinatal depression: prevalence, screening accuracy, and screening outcomes. Evid Rep Technol Assess (Summ) 119:1–8
Goodman SH, Tully EC (2009) Recurrence of depression during pregnancy: psychosocial and personal functioning correlates. Depress Anxiety 26(6):557–567
Grote NK, Swartz HA et al (2009) A randomized controlled trial of culturally relevant, brief interpersonal psychotherapy for perinatal depression. Psychiatr Serv 60(3):313–321
Guedeney A, Fermanian J (1998) Validation of a study of the French version of the Edinburgh post natal depression scale (EPDS): new results about use and psychometric properties. Eur Psychiatry 13:83–89
Horowitz JA, Goodman J (2004) A longitudinal study of maternal postpartum depression symptoms. Res Theory Nurs Pract 18(2–3):149–163
Leichsenring F, Rabung S et al (2004) The efficacy of short-term psychodynamic psychotherapy in specific psychiatric disorders: a meta-analysis. Arch Gen Psychiatry 61(12):1208–1216
Manzano J, Palacio Espasa F et al (1999) The narcissistic scenarios of parenthood. Int J Psychoanal 80(Pt 3):465–476
Marcus SM (2009) Depression during pregnancy: rates, risks and consequences—motherisk update 2008. Can J Clin Pharmacol 16(1):e15–e22
Marcus SM, Flynn HA et al (2003) Depressive symptoms among pregnant women screened in obstetrics settings. J Womens Health (Larchmt) 12(4):373–380
Milgrom J, Schembri C et al (2011) Towards parenthood: an antenatal intervention to reduce depression, anxiety and parenting difficulties. J Affect Disord 130(3):385–394
Murray L, Carothers AD (1990) The validation of the Edinburgh Postnatal Depression Scale on a community sample. Br J Psychiatry 157:288–290
Murray L, Cox JL (1990) Screening for depression during pregnancy with the EPDS. J Reprod Infant Psychol 8:99–109
Nanzer N, Righetti-Veltema M (2009) Use of an easily administered instrument to detect the risk of postpartum depression. Rev Med Suisse 5(191):395–401
Nanzer N, Knauer D, Palacio Espasa P et al (2012) Manuel de Psychothérapie centrée sur la parentalité. PUF, Paris
O’Hara MW (2009) Postpartum depression: what we know. J Clin Psychol 65(12):1258–1269
O’Hara MW, Stuart S et al (2000) Efficacy of interpersonal psychotherapy for postpartum depression. Arch Gen Psychiatry 57(11):1039–1045
Paulson JF, Bazemore SD (2010) Prenatal and postpartum depression in fathers and its association with maternal depression: a meta-analysis. JAMA 303(19):1961–1969
Pearson RM, Cooper RM et al (2010) Depressive symptoms in early pregnancy disrupt attentional processing of infant emotion. Psychol Med 40(4):621–631
Righetti-Veltema M, Conne-Perreard E et al (1998) Risk factors and predictive signs of postpartum depression. J Affect Disord 49(3):167–180
Righetti-Veltema M, Conne-Perreard E et al (2002) Postpartum depression and mother–infant relationship at 3 months old. J Affect Disord 70(3):291–306
Righetti-Veltema M, Bousquet A et al (2003) Impact of postpartum depressive symptoms on mother and her 18-month-old infant. Eur Child Adolesc Psychiatry 12(2):75–83
Spinelli MG, Endicott J (2003) Controlled clinical trial of interpersonal psychotherapy versus parenting education program for depressed pregnant women. Am J Psychiatry 160(3):555–562
Stuart S, Clark E (2008) The treatment of postpartum depression with interpersonal psychotherapy and interpersonal counseling. Sante Ment Que 33(2):87–104
Zero to three (2005) Diagnostic classification, 0–3 R: diagnostic classification of mental health and developmental disorders of infancy and early childhood. Zero to three, National Center for Clinical Infant Programs, Arlington
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nanzer, N., Sancho Rossignol, A., Righetti-Veltema, M. et al. Effects of a brief psychoanalytic intervention for perinatal depression. Arch Womens Ment Health 15, 259–268 (2012). https://doi.org/10.1007/s00737-012-0285-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00737-012-0285-z