Abstract
Data are scarce regarding the prevalence and risk factors for antenatal suicidal ideation because systematic screening for suicidal ideation during pregnancy is rare. This study reports the prevalence and correlates of suicidal ideation during pregnancy. We performed cross-sectional analysis of data from an ongoing registry. Study participants were 2,159 women receiving prenatal care at a university obstetric clinic from January 2004 through March 2010. Multiple logistic regression identified factors associated with antenatal suicidal ideation as measured by the Patient Health Questionnaire. Overall, 2.7% of the sample reported antenatal suicidal ideation. Over 50% of women who reported antenatal suicidal ideation also reported major depression. In the fully adjusted model antenatal major depression (OR = 11.50; 95% CI 5.40, 24.48) and antenatal psychosocial stress (OR = 3.19; 95% CI 1.44, 7.05) were positively associated with an increased risk of antenatal suicidal ideation. We found that being non-Hispanic White was associated with a decreased risk of antenatal suicidal ideation (OR = 0.51; 95% CI 0.26–0.99). The prevalence of antenatal suicidal ideation in the present study was similar to rates reported in nationally representative non-pregnant samples. In other words, pregnancy is not a protective factor against suicidal ideation. Given the high comorbidity of antenatal suicidal ideation with major depression, efforts should be made to identify those women at risk for antenatal suicidal ideation through universal screening.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Suicide is a leading cause of death among pregnant and postpartum women in the USA. (Chang et al. 2005). Despite our growing recognition of the prevalence and consequences of antenatal major depression, our understanding of suicidal ideation—a common aspect of major depressive disorder (Nock et al. 2009)—during the perinatal period is lacking. The precursor to suicide in most cases—suicidal ideation or thoughts of self-harm—among perinatal women is similar to those in the general population. In a review article, Lindahl and colleagues reported that 5–14% of women had expressed suicidal ideation during the perinatal period (Lindahl et al. 2005). Similarly, Nock and colleagues reported that 5.6–14.3% of adults reported a lifetime prevalence of suicidal ideation (Nock et al. 2009). Although screening for suicidal ideation during the perinatal period is rare, there are a few studies that have examined the prevalence and associated risk factors (Lindahl et al. 2005). One study found women were less likely to screen positive for suicidal ideation during pregnancy (Stallones et al. 2007). However, in most cases, studies found women who endorsed suicidal ideation during pregnancy, and the postpartum period experienced a myriad of adverse outcomes (Stallones et al. 2007; Paris et al. 2009; Gausia et al. 2009; Copersino et al. 2005; Newport et al. 2007; Bowen et al. 2009; Eggleston et al. 2009; Chaurdon et al. 2001). For example, suicidal ideation in pregnancy was a strong predictor of postpartum depression (Chaurdon et al. 2001), and postpartum women with psychiatric disorders reported a higher prevalence of suicidal ideation than their counterparts without psychiatric illnesses (Paris et al. 2009; Copersino et al. 2005; Newport et al. 2007; Eggleston et al. 2009).
However, the findings from earlier studies were primarily conducted within specific samples of women; thus, it is unknown whether prevalence estimates and risk factors identified in these studies are generalizable to the larger perinatal population. Recent perinatal suicidal ideation studies recruited samples comprised of those seeking treatment for perinatal mental illness (Paris et al. 2009; Copersino et al. 2005; Newport et al. 2007), women from rural areas in developing countries (Gausia et al. 2009), those seeking treatment for perinatal medical conditions (Newport et al. 2007), those in socially high-risk groups (Stallones et al. 2007; Bowen et al. 2009), pregnant active-duty soldiers (O'Boyle et al. 2005), and substance-dependent women seeking perinatal drug treatment (Eggleston et al. 2009). Findings from some studies also lack generalizability because of methodological limitations such as retrospective study designs (Copersino et al. 2005; Eggleston et al. 2009).
Another limitation of earlier studies is the assessment of suicidal ideation in the presence of maternal depression during pregnancy. It is well known that major depression is an important risk factor for suicidal ideation (Perez-Rodriguez et al. 2008). The population at greatest risk for depressive disorder is women of childbearing age because the onset and course of depression (as well as comorbid disorders) are often intertwined with reproductive events. A recent study that included a nationally representative sample of 14,549 women revealed that 12-month prevalence of depressive disorder was 9.3% among past-year postpartum women, 8.4% among past-year pregnant women, and 8.1% in non-pregnant women (Vesga-Lopez et al. 2008). Despite the similar rates across pregnant and non-pregnant women, pregnant women with depressive disorders are less likely than non-pregnant women to receive treatment (Vesga-Lopez et al. 2008). This is a function of the diagnosis of depressive disorders being largely under-detected in women who receive prenatal care in obstetric clinics (Kelly et al. 2001) because the majority of women seeking prenatal care are not screened for perinatal depression. Given the negative outcomes associated with untreated maternal major depression during and beyond the perinatal period (Brand and Brennan 2009), identifying women at risk for antenatal major depression is vital for detecting those women with comorbid suicidal ideation. However, to our knowledge, there are no recent studies that have investigated the comorbid nature of antenatal suicidal ideation and major depression. If depression and suicidal ideation are overlapping but distinct phenomena, it is important to examine suicidal ideation separately to best determine the magnitude of the risk of suicidal ideation during pregnancy. Given the risks associated with antenatal suicidal ideation to women and their offspring, identifying effective methods of detecting women with antenatal suicidal ideation is a paramount challenge.
To our knowledge, this is the largest US-based study that examines the prevalence and correlates of suicidal ideation in a community-based sample of pregnant women. The objectives of the present study were to: (1) examine the prevalence of suicidal ideation and comorbid psychiatric disorders during pregnancy; (2) identify the risk factors for suicidal ideation during pregnancy.
Methods
Sample
We used data from a longitudinal study of women who received prenatal care at a single university-based delivery hospital from January 2004 to March 2010. The clinic serves a diverse group of women with respect to race, socioeconomic status (SES), and medical risk, with 46.5% reporting private health insurance coverage and 51.6% reporting publically funded health insurance (Bentley et al. 2007).
During the study period, 3,347 women completed an antenatal psychosocial questionnaire as part of their routine antenatal care. Staff was present in clinic to consent 2,577 women (77%) for participation in the study. The total number of women who declined to participate in the study was 227 (6.8%). Due to Health Insurance Portability and Accountability Act regulations, it was not possible to compare characteristics of participants with those who declined enrollment or were not approached by clinic staff to participate in the study.
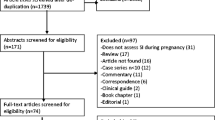
For the present analysis, we included only those women who received ongoing obstetrical care and completed one clinical questionnaire during the antenatal period. The final sample for the present analysis includes 2,159 women who had complete information on all study variables (Fig. 1). The mean gestational age when the questionnaire was completed was 27.37 weeks.
Procedures
Questionnaires measuring antenatal psychiatric disorders, including degree of suicidal ideation, as well as sociodemographic and psychosocial factors were introduced in January 2004 and designed to be distributed by clinical staff as part of routine clinical care. The screening protocol mandates that all patients must receive at least one questionnaire during pregnancy with the goal of two times: first during the early second trimester (approximately 16 weeks) and again in the third trimester (approximately 36 weeks). Questionnaires were self-administered and patients could complete them in either English or Spanish. Interpreters were also available to patients who spoke neither language. Clinic staff were asked to contact and consent potentially eligible respondents to participate in the study at the time of the questionnaire completion. Written consent was obtained in order to examine questionnaire data as well as automated medical records. Exclusion criteria for the study included age less than 15 years at the time of delivery, those who did not receive ongoing prenatal care, and inability to complete the clinical questionnaire due to mental incapacitation or language difficulties (i.e., no interpreter available). All study procedures were approved by the University of Washington Institutional Review Board prior to the beginning of the study with initial approval on September 12, 2003. The following clinic protocol was followed for women who screened positive for antenatal depression or endorsed suicidal ideation. Clinicians evaluated and managed depression during the course of antenatal care (i.e., referral to social work, therapy or specialty mental health, initiation of antidepressant medication, watchful waiting). Women reporting suicidal ideation were evaluated, followed, and referred to mental health services based on their level of suicide risk.
Measures
The questionnaire inquired about sociodemographic characteristics, general health history, and past obstetrical complications, as well as validated measures assessing major depression and panic disorder (Spitzer et al. 1999), psychosocial stress (Curry et al. 1994; Curry et al. 1998), tobacco use (Melvin and Tucker 2000), alcohol use (Sokol et al. 1989), drug use (Midanik et al. 1998), and domestic violence (Mcfarlane et al. 1992). Maternal age and parity were obtained from the automated medical record.
Suicidal ideation
Suicidal ideation was assessed using the Patient Health Questionnaire (PHQ) short form (15 items) (Spitzer et al. 1999). In our study, suicidal ideation was assessed based on item 9 of the PHQ, which asks “over the last 2 weeks how often have you been bothered by… thoughts that you would be better off dead or of hurting yourself in some way.” Response options included: 0 = “not at all”, 1 = “several days”, 2 = “more than half the days”, and 3 = “nearly every day”. Respondents were considered positive for suicidal ideation if they gave a response of “several days”, “more than half the days”, or “nearly every day”. Previous studies have used item 9 from the PHQ to assess suicidal ideation in clinical populations (Schulberg et al. 2005). The need for this screen is supported by findings that only a small number of patients inform their physicians of their suicidal plans or attempts (Isometsä et al. 1994).
Antenatal depression and panic disorder
In our study, antenatal depression and panic disorder was measured by the PHQ short form. The DSM-IV criteria for major depression on the PHQ require the subject to have, for at least 2 weeks, five or more depressive symptoms present for more than half the days, with at least one of these symptoms being depressed mood or anhedonia. The criteria for panic disorder require affirmative answers to five panic symptoms and follow the DSM-IV. In a study of 3,000 OB/GYN patients, the PHQ demonstrated high sensitivity (73%) and specificity (98%) for a diagnosis of major depression based on the Structured Clinical Interview for DSM-IV, as well as for a diagnosis of panic disorder (sensitivity 81%, specificity 99%) (Spitzer et al. 2000). In the present study, structured psychiatric interviews were not conducted to confirm clinical diagnoses. Therefore, antenatal depression is reported as “probable antenatal major depression.” Additionally, women who met the DSM-IV criteria for panic disorder were classified as having “probable antenatal panic disorder.”
Behavioral and clinical characteristics
Potential confounding factors for antenatal suicidal ideation were defined from findings from previous studies (Boden et al. 2008; Bonomi et al. 2006; Goodwin et al. 2003; Golding 1999; Kessler et al. 1999; Vilhjalmsson et al. 1998). Self-reported data on potential confounders included validated measures that assessed tobacco use and psychosocial stress during the antenatal period. Data collected from the questionnaire also included information on physical/sexual abuse, prepregnancy medical conditions, and history of pregnancy-related complications. Tobacco use was assessed using the Smoke-Free Families prenatal screen, which was specifically developed to maximize disclosure of smoking status during pregnancy (Melvin and Tucker 2000). On this screen, any current smoking is classified as tobacco use.
Psychosocial stress was measured using the Prenatal Psychosocial Profile, which has demonstrated validity and reliability for use in diverse pregnant populations (Curry et al. 1994; Curry et al. 1998). It is an 11-question survey using a Likert response scale with possible scores ranging from 11 to 44; high stress in our population has previously been established as a score of ≥23 (Woods et al. 2010). The three-question abuse assessment screen assesses physical and sexual violence during the past year and during pregnancy (Mcfarlane et al. 1992). This screen has been used both as a clinical screening tool with established validity and test–retest reliability, and for research purposes as a dichotomous measure of abuse (Bullock et al. 2006). Consistent with previous research studies, we classified women as positive for domestic violence if they answered “yes” to any of the three abuse questions.
Women who reported two or more chronic health conditions in the year prior to their pregnancy were determined to have a high number of medical conditions (e.g., asthma, hypertension, diabetes, or cardiovascular problems). History of pregnancy-related complications was recorded for patients who self reported one or more significant pregnancy complications (e.g., gestational diabetes, pre-eclampsia, eclampsia, preterm delivery, or placental abruption) in a prior pregnancy.
Sociodemographic characteristics
Available demographic data included self-reported race/ethnicity, partner status, educational attainment, and current employment status. Self-reported race/ethnicity in the study was categorized as follows: non-Hispanic White, Asian, Black, Latina, American Indian, Pacific Islander, and multi-racial. Partner status was analyzed as a binary variable (married or living with partner vs. single/separated/divorced or not living with partner). Educational attainment was measured as a binary variable (≤12 years vs. >12 years) from self-reported data regarding the highest level of formal education received. Current employment status was assessed as a binary variable (employed vs. not employed/not in labor force).
Statistical analyses
Cross-tabulations were used to describe characteristics of the sample. Chi-square tests for categorical variables and t tests for continuous variables were conducted to determine whether there were statistically significant differences in the association between sociodemographic, psychosocial, behavioral and clinical characteristics, and antenatal suicidal ideation. A series of logistic regression models were developed to account for the independent and confounding effects of each covariate with antenatal suicidal ideation. The inclusion of variables in the models was based on previous psychiatric epidemiological evidence. Odds ratios (OR) and 95% confidence intervals (CI) were generated for individual associations between each covariate and suicidal ideation during the antenatal period using STATA version 10 (STATA version 10, College Station, TX: Stata Corporation). Questionnaire data for each subject were entered and stored using Filemaker Pro (Filemaker Pro Version 9 for Windows @ 1994).
Results
Table 1 shows the clinical, sociodemographic, and behavioral characteristics of the sample, stratified by the presence or absence of antenatal suicidal ideation. Among the 2,159 respondents, mean age was 30.6 (±6.1) years, with a range of 15–51 years. The majority of women reported living with a partner (86.8%) and had completed more than 12 years of education (79.7%). The majority of women in the sample were White (66.3%) followed by Asian (11.2%), Latina (9.8%), Black (7.6%), multi-racial (3.9%), American Indian (2.6%), and Pacific Islander (1.3%).
Overall, 2.7% (n = 59) of respondents reported suicidal ideation during pregnancy. Among the women who screened positive for suicidal ideation, 78.0% reported thoughts of suicidal ideation “several days” in the last 2 weeks, 15.3% reported thoughts of suicidal ideation “more than half the days” in the last 2 weeks, and 6.7% reported thoughts of suicidal ideation “nearly every day”. The prevalence of probable antenatal major depression was 5.3% and 3.4% for probable antenatal panic disorder. Among those who were positive for suicidal ideation, 52.5% reported comorbid antenatal depression, and 15.7% experienced comorbid antenatal panic disorder.
Women who reported antenatal suicidal ideation were more likely to experience comorbid antenatal major depression and antenatal panic disorder, have 12 or less years of education, living without a spouse or cohabitating partner, report a high level of psychosocial stress, be a current smoker, be at risk for drug use, report high number of chronic health conditions, and report domestic violence (current or within the last year). Significant differences in the prevalence of suicidal ideation were present among Black and White women.
Table 2 shows the models used to examine the antenatal characteristics statistically associated with antenatal suicidal ideation. Given the prevalence and comorbidity of antenatal suicidal ideation and major antenatal depression in our sample, our basic model (model 1) included only antenatal major depression (OR = 28.33; 95% CI 16.39–48.94). Model 2 adjusted for psychosocial stress (OR = 4.06, 95% CI 2.05–8.04) and antenatal major depression (OR = 13.58, 95% CI 6.99–26.38) was still found to be significant. In model 3, we included the basic model as well as sociodemographic characteristics including educational attainment, partner status, and race (e.g., Black and White). Again, we found antenatal major depression (OR = 11.87; 95% CI 5.78–24.37) and psychosocial stress (OR = 3.84; 95% CI 1.83–8.05) to be significant risk factors for antenatal suicidal ideation. Finally, in model 4, we included the basic model, sociodemographic, behavioral, and clinical characteristics. Results were strikingly similar to those reported in model 3, except that White women were at decreased risk for antenatal suicidal ideation (OR = 0.51; 95% CI 0.26–0.99).
Discussion
In an economically and racially diverse sample of pregnant women attending a university-based clinic, the prevalence of antenatal suicidal ideation was 2.7%, which is similar to the 12-month prevalence of suicidal ideation reported in nationally representative non-pregnant samples of adults. Using data from the 1990–1992 National Comorbidity Survey (NCS) and the 2001–2003 National Comorbidity Survey Replication (NCS-R), the authors asked a cohort of adults about past year occurrence of suicidal ideation. The authors found the 12-month prevalence of suicidal ideation was 2.8% in the NCS and 3.3% NCS-R (Kessler et al. 2005). Another study using NCS-R data reported the 12-month prevalence of suicidal ideation was 2.6% (Borges et al. 2006). It should be noted that the prevalence of antenatal suicidal ideation in our study is well below the prevalence reported in previous studies of pregnant and postpartum women. In these studies, suicidal ideation has been noted to be present in 35% of women seeking antenatal neuropsychiatric or epileptic treatment (Newport et al. 2007), 35% of women with PTSD and substance abuse seeking perinatal drug treatment (Eggleston et al. 2009), and 4–40% of women from low socioeconomic groups (Stallones et al. 2007; Bowen et al. 2009). A potential explanation for the differences in prevalence of antenatal suicidal ideation in the present study compared to previous studies may be a function of the reliance of earlier studies on small sample sizes and the recruitment of women from distinct subject populations.
Our results also revealed a high prevalence of comorbidity with major depression. Over half of the sample who reported antenatal suicidal ideation also reported antenatal major depression. Not surprisingly, we also found antenatal major depression to be the strongest independent risk factor of antenatal suicidal ideation. The presence of a psychiatric disorder is among the most consistently reported risk factors for suicidal behavior. Specifically, major depressive disorder conveys one of the highest risks for suicidal ideation (Nock et al. 2008). Our study in a sample of over 2,100 pregnant women further supports the finding of the comorbid nature of suicidal ideation with major depression.
In our study, we found women with high levels of psychosocial stress to be at increased risk for antenatal suicidal ideation. Perceived stress has been shown to increase the prevalence of suicidal ideation among non-pregnant samples (Vilhjalmsson et al. 1998). However, to our knowledge, the present study is the first to show the link between high levels of psychosocial stress and antenatal suicidal ideation. Given the association between psychosocial stress (e.g., negative life events) and suicide (Feskanich et al. 2002), it is plausible that psychosocial stress is a risk factor for antenatal suicidal ideation.
An interesting finding from our study was White women were at decreased risk for antenatal suicidal ideation compared to their non-White counterparts. This finding is surprising considering studies using data from US-based nationally representative non-pregnant samples have found no racial differences in the risk associated with suicide ideation (Perez-Rodriguez et al. 2008; Kessler et al. 2005). A potential explanation for the finding may be that non-Hispanic White compared to non-White women in our sample were more likely to report ≥16 years of education (63.8% vs. 41.6%, χ 2 = 100.37, p < 0.001). Previous studies have also reported those with less education (<16 years) experienced a higher prevalence of suicide ideation (Kessler et al. 2005).
Our study has several limitations. First, suicidal ideation was captured using a single item that measures active and passive suicidal ideation. It is possible that using a single item to assess suicidal ideation may have excluded important dimensions of suicidal ideation (Lindahl et al. 2005). Second, the majority of our data were self-reported, which could lead to over identification or under reporting of some sensitive or stigmatized behaviors. Third, we examined the association between antenatal risk factors for antenatal suicidal ideation using cross-sectional data, which limit our ability to establish the causal nature of the association. Fourth, we lacked detailed information on prior mental health disorders and medications. Finally, although we have a very high rate of participation, information on non-participants was not available.
Despite these limitations, our study had a number of strengths, including the large sample size, use of a routine screening protocol with a high level of subject participation, utilization of strict DSM-IV diagnostic criteria for depressive and panic disorders, accurate assessment of multiple covariates, and adjustment for biomedical, demographic, psychosocial, and behavioral factors in our models. Among prior studies, our study is unique in accurately assessing a large number of potential confounders to establish a more complete model for antenatal suicidal ideation.
What is known on this topic
Although our understanding of the prevalence and consequences of antenatal major depression has improved, our understanding of suicidal ideation—a common aspect of major depression—during pregnancy is limited.
What this paper adds
To our knowledge, this is the largest community-based study of the prevalence and correlates of antenatal suicidal ideation among pregnant women. Our findings confirm that the prevalence of suicidal ideation in the present study is similar to that in nationally representative samples of non-pregnant adults. Antenatal major depression and psychosocial stress are significantly associated with antenatal suicidal ideation.
References
Bentley SM, Melville JL, Berry BD et al (2007) Implementing a clinical and research registry in obstetrics: overcoming the barriers. Gen Hosp Psychiatry 29:192–198
Boden J, Fergusson D, Horwood L (2008) Cigarette smoking and suicidal behaviour: results from a 25-year longitudinal study. Psychol Med 38:433–440
Bonomi A, Thompson R, Anderson M et al (2006) Intimate partner violence and women's physical, mental, and social functioning. Am J Prev Med 30:458–466
Borges G, Angst J, Nock M, Ruscio AM, Walters EE, Kessler RC (2006) A risk index for 12-month suicide attempts in the National Comorbidity Survey Replication (NCS-R). Psychol Med 36:1747–1757
Bowen A, Stewart N, Baetz M et al (2009) Antenatal depression in socially high-risk women in Canada. J Epidemiol Community Health 63:414–416
Brand S, Brennan P (2009) Impact of antenatal and postpartum maternal mental illness: how are the children? Clin Obstet Gynecol 51:441–455
Bullock L, Bloom T, Davis J et al (2006) Abuse disclosure in privately and medicaid-funded pregnant women. J Midwifery Womens Health 51:361
Chang J, Berg C, Saltzman L et al (2005) Homicide: a leading cause of injury deaths among pregnant and postpartum women in the United States, 1991–1999. Am J Public Health 95:471–477
Chaurdon L, Klein M, Remington P et al (2001) Predictors, prodromes and incidence of postpartum depression. Psychosom Obstet Gynecol 22:103–112
Copersino M, Jones H, Tuten M et al (2005) Suicidal ideation among drug-dependent treatment-seeking inner-city women. J Maint Addict 3:53–64
Curry M, Campbell R, Christian M (1994) Validity and reliability testing of the prenatal psychosocial profile. Res Nurs Health 17:127–135
Curry MA, Burton D, Fields J (1998) The prenatal psychosocial profile: a research and clinical tool. Res Nurs Health 21:211–219
Eggleston A, Calhoun P, Svikis D et al (2009) Suicidality, aggression, and other treatment considerations among pregnant, substance-dependent women with posttraumatic stress disorder. Compr Psychiatry 50:415–423
Feskanich D, Jastrup JL, Marshall JR et al (2002) Stress and suicide in the nurses' health study. J Epidemiol Community Health 56:95–98
Filemaker Pro Version 9 for Windows @ 1994-2008, Santa Clara, California: FileMaker, Inc.
Gausia K, Fisher C, Ali M et al (2009) Antenatal depression and suicidal ideation among rural Bangladeshi women: a community-based study. Arch Womens Ment Health 12:351–358
Golding J (1999) Intimate partner violence as a risk factor for mental disorders: a meta-analysis. J Fam Violence 14:99–132
Goodwin R, Kroenke K, Hoven C, Spitzer R (2003) Major depression, physical illness, and suicidal ideation in primary care. Psychosom Med 65:501
Isometsä ET, Henriksson MM, Aro HM, Heikkinen et al (1994) Suicide in major depression. Am J Psychiatry 151:530–536
Kelly R, Zatzick D, Anders T (2001) The detection and treatment of psychiatric disorders and substance use among pregnant women cared for in obstetrics. Am J Psychiatry 158:213–219
Kessler R, Borges G, Walters E (1999) Prevalence of and risk factors for lifetime suicide attempts in the national comorbidity survey. Arch Gen Psychiatry 56:617–626
Kessler R, Berglund P, Borges G et al (2005) Trends in suicide ideation, plans, gestures, and attempts in the United States, 1990–1992 to 2001–2003. Journal of American Medical Association 293:2487
Lindahl V, Pearson J, Colpe L (2005) Prevalence of suicidality during pregnancy and the postpartum. Arch Womens Ment Health 8:77–87
Mcfarlane J, Parker B, Soeken K, Bullock L (1992) Assessing for abuse during pregnancy. Severity and frequency of injuries and associated entry into prenatal care. Journal of the American Medical Association 267:3176–3178
Melvin C, Tucker P (2000) Measurement and definition for smoking cessation intervention research: the smoke-free families experience. Smoke-free families common evaluation measures for pregnancy and smoking cessation projects working group. Tob Control 9(Suppl 3):III87–III90
Midanik LT, Zahnd EG, Klein D (1998) Alcohol and drug CAGE screeners for pregnant. Low-income Women: the California perinatal needs assessment. Alcohol Clin Exp Res 22:121
Newport D, Levey L, Pennell P et al (2007) Suicidal ideation in pregnancy: assessment and clinical implications. Arch Womens Ment Health 10:181–187
Nock MK, Boges G, Bromet EJ et al (2008) Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry 192:98–105
Nock M, Hwang I, Sampson N et al (2009) Cross-national analysis of the associations among mental disorders and suicidal behavior: findings from the WHO World Mental Health Surveys. PLoS Med 6:e1–e16
O'Boyle A, Magann E, Ricks R et al (2005) Depression screening in the pregnant soldier wellness program. South Med J 98(4):416–418
Paris R, Bolton R, Weinberg M (2009) Postpartum depression, suicidality, and mother-infant interactions. Arch Womens Ment Health 12:309–321
Perez-Rodriguez M, Baca-Garcia E, Oquendo M et al (2008) Ethnic differences in suicidal ideation and attempts. Prim Psychiatry 15:44–58
Schulberg H, Lee P, Bruce M et al (2005) Suicidal ideation and risk levels among primary care patients with uncomplicated depression. Ann Fam Med 3:523–528
Sokol R, Martier S, Ager J (1989) The T-ACE questions: practical prenatal detection of risk-drinking. Am J Obstet Gynecol 160:863–868, discussion 868-70
Spitzer R, Kroenke K, Williams J (1999) Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. primary care evaluation of mental disorders. Patient health questionnaire. Journal of the American Medical Association 282:1737–1744
Spitzer R, Williams J, Kroenke K et al (2000) Validity and utility of the PRIME-MD patient health questionnaire in assessment of 3000 obstetric-gynecologic patients: the PRIME-MD patient health questionnaire obstetrics-gynecology study. Am J Obstet Gynecol 183:759–769
Stallones L, Leff M, Canetto S et al (2007) Suicidal ideation among low-income women on family assistance programs. Women Health 45:65–83
STATA version 10, College Station, TX: Stata Corporation
Vesga-Lopez O, Blanco C, Keyes K et al (2008) Psychiatric disorders in pregnant and postpartum women in the United States. Arch Gen Psychiatry 65:805–815
Vilhjalmsson R, Kristjansdottir G, Sveinbjarnardottir E (1998) Factors associated with suicide ideation in adults. Soc Psychiatry Psychiatr Epidemiol 33:97–103
Woods SM, Melville JL, Guo Y et al (2010) Psychosocial stress during pregnancy. Am J Obstet Gynecol 202:1–7
Funding
This research is supported by Grant Numbers 1KL2RR025015-01 and TL1 RR025016 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH) and NIH Roadmap for Medical Research.
Competing interest
None
Human participant protection
This study was approved by the University of Washington's Institutional Review Board.
The Corresponding Author has the right to grant on behalf of all authors and does grant on behalf of all authors, an exclusive licence (or non exclusive for government employees) on a worldwide basis to the BMJ Publishing Group Ltd to permit this article (if accepted) to be published in JECH and any other BMJPGL products and sublicences such use and exploit all subsidiary rights, as set out in our licence (http://jech.bmj.com/site/about/licence.pdf).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gavin, A.R., Tabb, K.M., Melville, J.L. et al. Prevalence and correlates of suicidal ideation during pregnancy. Arch Womens Ment Health 14, 239–246 (2011). https://doi.org/10.1007/s00737-011-0207-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00737-011-0207-5