Abstract
Limited research has been conducted in the United Arab Emirates in relation to postpartum depression. The purpose of this study was to investigate the risk and protective factors of postpartum depression in women in Sharjah, United Arab Emirates. We carried out a prospective study in which we followed women from the second trimester of pregnancy until 4 months postpartum. Data were collected during the second and third trimesters and then at 2- and 4- months postpartum. The risk/protective factors that were investigated included: depression and anxiety during pregnancy, stressful life events, breastfeeding, employment status following delivery, religiosity, and socio-demographic variables. The Edinburgh Postnatal Depression Scale (screening) and the Mini International Neuropsychiatric Inventory (diagnostic) were used as outcome variables. Using the Mini International Neuropsychiatric Inventory (diagnostic), 10% of the 137 participants in the study were diagnosed with postpartum depression. The following variables were found to be predictive of postpartum depression: depression during pregnancy in both the second and third trimesters: number of children, religion, and use of formula for feeding. Several factors were of borderline significance including educational level of mother, lack of breastfeeding, personal stressful life events, and employment status following delivery. These risk factors are important as they indicate potential areas for early identification. Screening of pregnant women during pregnancy and in the postpartum phase would be important. This study forms the foundation for further research and development related to prevention and intervention for postpartum depression in this Arab context.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Postpartum depression is the most common complication of childbirth. The average prevalence rate based upon a large number of studies is between 10–15% of recently delivered mothers (O’Hara and Swain 1996; Robertson et al. 2004). This condition has negative health implications for the mother, child, and family (Robertson et al. 2004). A recent review of the literature found that the following risks factors are the strongest predictors of postpartum depression (in decreasing order of effect): depression during pregnancy, anxiety during pregnancy, experience of stressful life events during pregnancy, low levels of social support, and previous history of depression (Robertson et al. 2004). An earlier meta-analysis of the research had also found the following variables to be predictors of postpartum depression: self-esteem, childcare stress, marital relationship, infant temperament, marital status, socioeconomic status, and unplanned/unwanted pregnancy (Beck 2001). These results are similar to those obtained in the first meta-analysis of the subject by O’Hara and Swain (1996). Both formula feeding in place of breastfeeding and cigarette smoking have also been found to be risk factors (Breese McCoy et al. 2006).
Limited research has been conducted in the United Arab Emirates in relation to postpartum depression. Abou-Saleh and Ghubash (1997) conducted a research study of 95 women admitted to a hospital in Dubai for childbirth. The prevalence rate of postpartum depression using the Edinburgh Postnatal Depression Scale was 18%. Green et al. (2006), in their study of postpartum depression in Abu Dhabi, found that 22% of mothers fell into the Depression category and another 22% in the Borderline Depression category at 3 months. At 6 months, this fell to 12.5% in the Depression category and 19.6% in the Borderline Depression category. Risk factors that emerged from this study included: not breastfeeding, giving birth to the first child, poor body image, poor relationship with mother-in-law, and older age at marriage.
Ghubash and Eapen (2009), in a recent qualitative study, reported that lack of support from the husband and his family, as well as disagreements between the husband's and wife's families were major contributors to depression during pregnancy. Other factors that were believed by focus group members to contribute to postnatal depression included difficult delivery, unhealthy or difficult baby, poor bonding, lack of support and isolation from family of origin, and conflicts with regard to mother's role (i.e., wife, mother, or employee).
The aim of the present study was to determine the prevalence and psychosocial risk and protective factors for postpartum depression, including depression and/or anxiety during pregnancy, stressful life events during pregnancy, breastfeeding, employment status, religiosity, and socio-demographic variables. This research is important as there is a strong primary health care system in this affluent country, but very limited mental health services for pregnant and postpartum women. Demonstrating a need may provide rationale for future development of such services. Based upon research mentioned above, there may also be cultural-specific factors contributing to or protective against postpartum depression. It would be important to determine these factors in order to enhance development of cultural-specific treatment options. This research is also unique in that it includes religion and religiosity as putative protective factors which prior research has not considered.
Methods
This prospective study was conducted in the Maternal and Child Health Center (MCHC) in the Emirate of Sharjah, United Arab Emirates, the only center of its kind in Sharjah. This governmental center provides comprehensive preventive and curative services to women and children including antenatal care, well baby care, breastfeeding clinic, nutrition clinic, and health education. The services are available free of charge for nationals and legal residents of Sharjah. The women were first assessed during the second trimester of their pregnancies and were followed during the third trimester of pregnancy and for 4 months postpartum. Data were collected from the antenatal (during pregnancy) and well baby care clinics (during postpartum phase). The study was conducted from February 2008 until March 2009 and approval was granted by the Institutional Review Board of the University of Sharjah prior to implementation.
Participants
A convenient sample of 137 pregnant women, aged 18 and above, attending the MCHC were involved in this study. Prospective participants were approached in the waiting areas in the Center. The study was explained to participants and informed consent was obtained prior to data collection. Women under 18 years of age and non-Arabic or non-English speakers were excluded from the study. Women were also excluded if they had plans to deliver the baby in their home country as they would have been lost during the follow-up phase.
Procedure
The study was of a prospective nature involving follow-up of participants during pregnancy and after delivery. Data were collected at the following points: second trimester of pregnancy (fourth, fifth, or sixth month), third trimester of pregnancy (seventh, eighth, or ninth month), 2 months postpartum and 4 months postpartum. These postpartum dates were selected as they coincided with the childhood vaccination schedule for the UAE. Interviews were organized with the mothers during the well baby care visits to the Center. Four months postpartum was selected as the final data point due to the literature which indicates that postpartum depression is likely to have appeared by that time. Participants were added to the participant pool as they were obtained and then follow-up proceeded with each one accordingly. Forms were self-administered with questions clarified by a trained, female research assistant. For illiterate participants, the forms were read to them.
During the first data point (second trimester), the following data were obtained: socio-demographic information, Beck Depression Inventory-II, Beck Anxiety Inventory, Stressful Life Events Inventory, and measure of religiosity. For the third trimester, only the Beck Depression Inventory-II and the Beck Anxiety Inventory were re-administered. At 2 and 4 months postpartum, the following measures were administered: Edinburgh Postnatal Depression Scale (EPDS) and Mini International Neuropsychiatric Interview (MINI)—Major Depression module. Only participants who scored 10 or above on the EPDS (screening tool) were administered the MINI (diagnostic tool). Only results for the 2-month postpartum phase are reported here.
Measures
Socio-demographic information
The following socio-demographic variables were assessed: age, nationality, country of birth, educational status of mother, occupational status of mother, educational status of husband, monthly family income, number of wives of the husband, number of children, and religion.
Beck Depression Inventory-II
The Beck Depression Inventory-II (BDI-II) is the most widely used inventory for depression. It is a 21-item self-rating scale with very good psychometric properties. Each item is comprised of four statements (rated 0–3) describing increasing severity of the abnormality concerned over the preceding week. It is important to note that the BDI provides an indication of the level of depressive symptomatology, but it is not a diagnostic instrument. The Arabic version of the Beck Depression Inventory was used for purposes of this study. This version has been validated and demonstrated to be culturally appropriate for this population (Hamdi et al. 1988; Rader et al. 1991; West 1985). For purposes of statistical analyses, for the BDI-II score, each subject was categorized into one of four groups: (1) 0–13 minimal depression, (2) 14–19 mild depression, (3) 20–28 moderate depression, and (4) 29–63 severe depression.
Beck anxiety inventory
The Beck Anxiety Inventory (BAI) is a 21-item scale of common anxiety symptoms. The respondent is requested to rate how much she has been bothered by each of the symptoms over the past week on a 4-point scale ranging from 0 to 3. The ratings are then summed to obtain a total score ranging from 0 to 63. The scale has high internal consistency and item-total correlations ranging from 0.30 to 0.71. Test–retest reliability correlations have been reported to be 0.75. For the BAI, four categories were formed: (1) 0–7 minimal anxiety, (2) 8–15 mild anxiety, 16–25 moderate anxiety, and (4) 26–63 severe anxiety. This scale is also available in the Arabic language.
Stressful life events inventory
Stressful life events were assessed by a modified Arabic version of an inventory by Kendler et al. (1999). With this assessment tool, the occurrence of “personal” events and “network” events in the past year were recorded to the nearest month. Personal events are those that occurred primarily to the subject herself and included the following general categories: marital or relationship problems, serious health problems, employment-related problems, financial or housing problems, legal problems, abuse or trauma. Four classes of network events (events occurring primarily to, or in interaction with, a person in the respondent’s social network) were also assessed. These event classes consisted of death, serious illness, or personal crisis of an individual in the network, as well as serious trouble getting along with an individual in the network. The network consisted of the respondent’s spouse, child, parent, sibling, other relative, and someone else close (friend, neighbor). Modifications to the Stressful Life Events Inventory were made by removing one item (i.e., living in a bad neighborhood) and adding others (i.e., physical abuse, emotional abuse, natural disaster, and war or terrorism) that seemed more appropriate for the population. The instrument was translated into Arabic and then back-translated into English.
Self-reported religiosity
Three items were used to assess the religiosity of participants: (1) To what extent would you define yourself as religious? (2) To what extent do you observe religious commandments? (3) To what extent do you feel a sense of affiliation to your religion? Participants were asked to respond on a scale ranging from 1 (not at all) to 6 (very much so). The Cronbach’s alpha measure of internal consistency is reported to be 0.87 (Haj-Yahia 2002). Reliability scores of 0.86 and 0.88 have also been reported (Haj-Yahia 1998a; b). Previous studies have demonstrated that these three questions successfully measure the extent of religiosity of participants from various religious groups in Arab society (i.e., Muslims, Christians, Druze) (Haj-Yahia 2002). The Arabic version of the items was provided by the author. For purposes of data analysis, scores on each of the three items were converted into a percentage (out of 100) of religiosity.
Edinburgh Postnatal Depression Scale
The EPDS is a 10-item self-report instrument that screens for postpartum depressive symptoms within the previous seven days and identifies at-risk mothers. Each item is scored on a four-point scale (from 0 to 3), with the minimum and maximum scores being 0 and 30, respectively. The EPDS is widely used in the research of postpartum depression and has been validated in the Arabic language (Ghubash et al. 1997). The authors of this validation study suggested a cutoff score of 10 for this Arabic version. With this cutoff, the sensitivity of the scale was found to be 91% and its specificity was 84%. For purposes of this study, a cutoff of 9 (10 or above) was used as suggested by Wisner et al. (2002) for community samples.
Mini International Neuropsychiatric Interview
The Major Depressive Disorder Module of the MINI was used. The MINI is a short diagnostic structured interview developed in France and the United States to explore 17 disorders according to Diagnostic and Statistical Manual-IV diagnostic criteria (Lecrubier et al. 1998; Sheehan et al. 1998a). It is fully structured to allow administration by non-specialized interviewers. For each disorder, one or two screening questions rule out the diagnosis when answered negatively. The reliability, sensitivity, and specificity have been investigated in clinical populations versus the CIDI (Lecrubier et al. 1997) and versus the SCID (Sheehan et al. 1998b). In both of these validation studies, the performance of the MINI was equivalent to the longer interviews. The MINI has been translated (and back-translated) into the Arabic language with attention to semantic rather than literal translation.
Postnatal questionnaire
The postnatal questionnaire was designed specifically for this study and included questions related to breastfeeding and returning to work. Specific breastfeeding questions were related to the following: (1) breastfeeding baby at any time during postpartum (yes or no), (2) length of breastfeeding, (3) breastfeeding at current time (yes or no), (4) frequency of breastfeeding in 1 day, and (5) use of baby formula (yes or no). Specific questions related to work included: (1) working at current time (yes or no), (2) when returned to work, (3) working part-time or full-time, (4) plans to return to work.
Statistical analyses
Data were entered into a Microsoft Excel sheet, and then transferred to the Statistical Analysis Software (SAS, version 9.1) which was used for data management and analyses. Descriptive analyses were carried out by calculating the number and percent for the categorical variables, and the mean and standard deviation for continuous variables. Risk/protective factors for depression (measured by the MINI scale, case vs. non-case) were identified by carrying out the chi-square or Fisher’s exact T test for categorical variables, and Student’s t test or Wilcoxon–Mann–Whitney test for continuous variables, as appropriate. Moreover, the risk/protective factors for depression (measured by the EPDS as a continuous variable) were identified by carrying out the Student’s t test or Wilcoxon–Mann–Whitney test for categorical variables, or Pearson correlation coefficient for continuous variables, as appropriate. A p value of 0.05 or less was considered statistically significant.
Results
Demographic characteristics
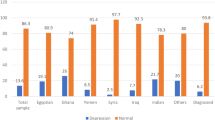
Approximately 180 women were approached in the Center to participate in the study. Some women did not plan to be in the vicinity through 4 months postpartum and thus were not recruited. Others had small children with them, felt that the questionnaire was too long, or had no specific reason for declining. One hundred and fifty women participated in the first phase of the study. Thirteen of these were lost during the follow-up phase or had incomplete data and thus the data analyses were conducted for 137. Socio-demographic characteristics of the sample, along with other variables, are shown in Table 1, stratified by results on the MINI. Of the sample, 53.3% were from the Arabian Peninsula (i.e., United Arab Emirates, Saudi Arabia, Kuwait, Yemen) and Levant Countries (i.e., Syria, Palestine, Jordan, Iraq, Lebanon) and 46.7% were from North Africa (i.e., Egypt, Sudan, Algeria, Morocco, Libya, Tunisia) and other countries (i.e., India, Pakistan). The majority of the participants were younger with 73.7% in the 18–29 range and 26.3 in the 30+ range. All of the participants were married as pregnancy outside of marriage is very rare in this part of the world. Approximately, 70.8% had a college or university education, 29.2% had secondary school or below. The majority, 67.2%, were not working, while 25.6% were working full-time and 7.3% were working part-time. About 67.9% of the husbands were college or university educated and 32.1% had secondary or below education. Ninety-nine percent had only one wife. In regard to family income, 24.1% had monthly income below AED 5,000 ($1,360), 47.5% had income between AED 5,000 and 10,000 ($2700) and 28.5% income of more than AED 10,000. The majority at 92.0% were of the Islamic faith, while 8.0% were other religions (5.1% Christian and 2.9% Hindu or Sikh).
Beck Depression Inventory-2 and Beck Anxiety Inventory
Frequencies of scores for the BDI-2 and BAI are also presented in Table 1. The mean of the scores for the BDI-2 during the second trimester was 16.1 (SD = 7.5), while the mean score for BAI was 16.0 (SD = 10.1). For the third trimester, the mean score of the BDI-2 was 16.1 (SD = 6.3) and the mean score of the BAI was 10.0 (SD = 6.9). It is interesting to note that there was no change in the mean for the BDI-2, but there was a change of 6 points in the mean of the BAI.
Edinburgh Postnatal Depression Inventory and Mini International Neuropsychiatric Interview (2-months postpartum)
The mean score of the EPDS for the sample at 2-months postpartum was 5.9 (SD = 4.9). Approximately 83.2% scored below 10 and 16.8% scored 10 or above. For the MINI, 10.1% were diagnosed with Major Depressive Disorder, while 89.9% were not. There was an obvious strong correlation between the EPDS and the MINI (p < 0.0001).
Correlation of MINI with predictive variables
Cross-tabulations of the MINI (2-months postpartum) with socio-demographic variables, BDI, BAI, stressful life events, religiosity, breastfeeding, and returning to work variables are presented in Table 1. The following socio-demographic variables were found to be correlated with scores on the MINI (p < .05): number of children (having more than one child), and religion (non-Muslim). It should be noted that monthly family income trended in the direction of significance (p < 0.14) and, in fact, it was significant when the analysis was run with EPDS as a continuous variable (p < 0.03).
Scores on the BDI during both the second and third trimesters were significantly correlated with the MINI, (p < 0.01 and p < 0.002, respectively). The number of stressful life events (either personal or network) that a woman had experienced in the past year was not found to be correlated with depression, nor was religiosity. For the BAI, neither of the scores during the second or third trimester was found to be significantly correlated with the MINI.
In relation to feeding of the infant, use of formula was found to be significantly related (p < 0.001) to the MINI, with women using formula more likely to be diagnosed with PPD. Breastfeeding at all was not found to be significantly correlated with the MINI, but it had borderline significance (p < 0.07). When the correlation was run with EPDS as a continuous variable, there was significance. In this case, women who had breastfed at all (p < 0.05) and were breastfeeding at the time of data collection (p < 0.004) had lower scores on the EPDS than women who had not breastfeed or breastfeed for a shorter period of time. The frequency of breastfeeding was also correlated with EPDS scores (p < 0.04), with greater frequency related to lower scores.
For employment status at the time of interview, women who had returned to work were more likely to be diagnosed with postpartum depression than those who had not, although this result was not significant (p < 0.10). In the analysis with the Edinburgh, working women had higher scores than non-working women and this was significant (p < 0.0025). Women who planned to return to work were less likely to be diagnosed with postpartum depression (p < 0.15) and had lower scores on the Edinburgh (p < 0.03).
Stressful life events
The frequencies of stressful life events are presented in Tables 2 and 3 for both personal events and network events. The two most common stressful personal events were separation from a loved one or close friend (14.2%) and serious housing problem (14.2%), followed by other serious marital problem (13.5%), war or terrorism (9.2%), major financial problems (7.9%), difficulties at work (7.1%), and emotional abuse (6.4%). The most common stressful network events were death of other relative (17.7%), difficulty getting along with in-laws (11.4%), serious or life-threatening illness or injury of parent (9.2%) or other relative (8.5%), serious personal crisis of sibling (7.8%), and death of parent (7.1%).
Cutoff differences for EPDS
Using a cutoff score of 11 or above on the EPDS resulted in 85.6% falling in this category and 14.4% in the below 11 range. Approximately 89.2% of the participants scored in the 12 and above range, using this cutoff, while 10.8% scored below 12. It is worth noting that using the cutoff score of 10 or above on the EPDS resulted in 9 false positive cases which were subsequently classified as non-cases with the MINI. None of the patients with a score of less than 10 on the EPDS were later classified as cases, indicating 0 false negatives. Raising the cutoff to 11 and above resulted in seven false positives and one false negative. With a cutoff of 12 and above, there were four false positives and three false negatives. While this last cutoff provides a closer percentage to the MINI in terms of cases, it also results in more false negatives.
Conclusions and discussion
The uniqueness of this study is that it is prospective in design and examines some of the risk and protective factors of postpartum depression that have been established in Western literature in an Arab context. Ten percent of this sample was found to have a diagnosis of postpartum depression using the Mini International Neuropsychiatric Interview. Variables that were found to be correlated with scores on the MINI (p < 0.05) included number of children (having more than one child), religion (non-Muslim), scores on the Beck Depression Inventory during both the second and third trimesters of pregnancy, and use of formula for feeding of the infant.
The prevalence of postpartum depression for women in this study (10%) was lower than that found in previous studies in the UAE (approximately 18%). This discrepancy may be related to the differences in assessment devices utilized. A diagnostic scale was used in this present study, while previous researchers employed a screening tool. It is likely that this present statistic is more accurate, at least for women in Sharjah. It also more closely approximates international norms. There may also be differences due to cutoffs that are used which may have an influence upon the outcome (see discussion below).
In their validity study of the Arabic version of the Edinburgh Postnatal Depression Scale, Ghubash et al. (1997) suggested the use of 10 as a cutoff score. They found that by lowering the cutoff score from 12 to 10, the sensitivity of the scale increased from 73% to 91% with limited effect upon specificity (90% versus 84%). As mentioned, a cutoff of 9 (10 or above) was used in this study. The rationale for lowering the cutoff is that it is better to have false positives rather than false negatives in a two-stage assessment procedure. The results of this study are consistent with this notion. With a cutoff of 10 or above, there were no false negatives, but there were nine false positives. Those nine false positives would simply be eliminated in the diagnostic phase of the process. Raising the cutoff to 12 and above resulted in fewer false positives (4), but more false negatives (3). It is more important to catch the false negatives, so a lower cutoff is more beneficial for purposes of community screening.
One of the most significant predictive variables in this present study was depressive symptoms during pregnancy. This is likely due to the fact that depression during pregnancy may carry over into the postnatal phase. As noted earlier, this variable has been found to be a risk factor for postpartum depression in Western populations (Robertson et al. 2004). The importance of this variable is that it indicates the need to conduct screening of women in the prenatal phase as well as the postnatal phase. Women who are identified as depressed during pregnancy and then treated prior to delivery are less likely to have problems during the postnatal phase.
It is surprising that neither anxiety during depression nor number of stressful life events were found to be risk factors in this study, although personal stressful life events approached significance with the MINI. These variables have also been identified in the Western literature to be important and Hamdan et al. (2008) found stressful life events to be significantly related to depressive symptoms in a study of Arab women in primary health care. Future research studies will be required to determine the reason for this discrepancy.
The results of this study point to the importance of breastfeeding for the new mother. Breastfeeding was found to be a protective factor against postpartum depression, while formula feeding is a risk factor. These results have also been reported in previous literature. It is important to note that these results are correlational in nature and that the direction of the influence may be in the opposite direction. Green et al. (2006) noted that another possible explanation could be that depression affects a mother's decision to wean the baby (i.e., they would be more likely to wean the baby due to the depression). They also highlight the role of religious factors in that if a woman decides not to breastfeed, thus going against religious and cultural expectations, this may lead to increased stress and amplify the likelihood of depressive symptoms. It would be interesting to investigate these variables further, as well as the role of employment status in this relationship.
The influence of low socioeconomic status (SES) was reported by Hamdan et al. (2008) in their study of depression in the primary health care centers of Sharjah. While the average per capita income in the UAE is one of the highest in the world, there are families who are of a lower SES. In this study, women in the low SES group were more likely to experience postpartum depression than those in higher income groups.
Ghubash and Eapen (2009) reported that employed women felt that a balance between family and work would be optimal, but the majority felt that family should take precedence over work. In this present study, difficulty at work was one of the most commonly occurring stressful life events during the prenatal phase. Also, those who were employed outside of the home were more likely to have higher postpartum depression scores than women who were not employed. It is of interest to note that women who planned to return to work had lower scores on the Edinburgh and were less likely to be diagnosed with PPD. It may be that the idealistic notion of returning to work and being freed from the stress of motherhood provided some solace to these new mothers. This does not seem to be beneficial in reality, however, as evidenced by the employment status variable. Due to the fact that an increasing number of women are entering the labor force in this context, it would be important to study this factor in more detail to determine its impact upon the health and well-being of both the mother and the baby.
Although possessing a strong primary health care system and focusing on the development of health systems, the UAE currently has very limited services in the area of mental health for pregnant women and new mothers. Health professionals in this area have recognized the need for policy change to incorporate mental health services within maternal/child health care (Ghubash and Eapen 2009). These changes could easily be done by adding a screening component during neonatal checkups. The Edinburgh Scale is short and would not require a significant amount of time. Mental health professionals could be added to the team for women in need of more extensive services. Steps could also be taken to increase general awareness of perinatal mental health problems (e.g., informing women of the signs and symptoms during pregnancy) and to train health care workers in early detection and diagnosis (Ghubash and Eapen 2009).
There are several limitations of the study that should be taken into consideration. One is the use of a convenient sample due to practical limitations in utilizing a random sampling process. For this reason, the sample may or may not represent the population under study. The outcomes of this research, however, do seem valid, particularly since they match previous research in the area. Another related limitation may be the small sample size. It may be that correlations that neared significance in this study would have been significant with a larger sample size.
In spite of these limitations, this research contributes to the general body of knowledge on postpartum depression and provides unique insight into the prevalence and risk factors of postpartum depression in this Arab context. As a result, it forms the foundation for further research and development related to prevention and intervention for postpartum depression.
References
Abou-Saleh MT, Ghubash R (1997) The prevalence of early postpartum psychiatric morbidity in Dubai: A transcultural perspective. Acta Psychiatr Scand 95:428–432
Beck CT (2001) Predictors of postpartum depression: an update. Nurs Res 50:275–285
Breese McCoy SJ, Martin JM, Miller Shipman SB, Payton ME, Watson GH (2006) Risk factors for postpartum depression: a retrospective investigation at 4-weeks postnatal and a review of the literature. J Amer Osteopath Assoc 106:193–198
Green K, Broome H, Mirabella J (2006) Postnatal depression among mothers in the United Arab Emirates: socio-cultural and physical factors. Psychol Health Med 11(4):425–431
Ghubash R, Abou-Saleh MT, Daradkeh TK (1997) The validity of the Arabic Edinburgh Postnatal Depression Scale. Soc Psychiatry and Psychiatr Epidemiol 32:474–476
Ghubash R, Eapen V (2009) Postpartum mental illness: perspectives from an Arabian Gulf population. Psychol Rep 105:127–136
Haj-Yahia MM (2002) Attitudes of Arab women toward different patterns of coping with wife abuse. J Interpers Violence 17(7):721–745
Haj-Yahia MM (1998a) Beliefs about wife-beating among Palestinian women: the influence of their patriarchal ideology. Violence Against Women 4(5):533–558
Haj-Yahia MM (1998b) A patriarchal perspective of beliefs about wife beating among Palestinian men from the West Bank and Gaza Strip. J Fam Issues 19(5):595–621
Hamdan A, Hawamdeh S, Hussein A (2008) The prevalence and correlates of depressive symptoms among Arab women in a primary healthcare setting. Int J Psychiatry Med 38(4):453–467
Hamdi N, Abu-Hijleh N, Abu Taleb S (1988) Reliability and validity study of an Arabic version of Beck’s Inventory for Depression. Dirasat 15:30–40
Kendler KS, Karkowski LM, Prescott CA (1999) Causal relationship between stressful life events and the onset of major depression. Am J Psychiatry 156(6):837–841
Lecrubier Y, Sheehan D, Hergueta T, Weiller E (1998) The Mini International Neuropsychiatric Interview. Eur Psychiatry 13(supp 4):198
Lecrubier Y, Sheehan D, Weiller E, Amorim P, Bonora I, Harnett Sheehan K et al (1997) The Mini International Neuropsychiatric Interview (MINI). A short diagnostic structured interview: reliability and validity according to the CIDI. Eur Psychiatry 12(5):224–231
O’Hara MW, Swain AM (1996) Rates and risk of postpartum depression: a meta-analysis. Int Rev Psychiatry 8(1):37–54
Rader KK, Adler L, Schwibbe MH, Sultan AS (1991) Validity of the Beck Depression Inventory for cross-cultural comparisons: a study of German and Egyptian patients. Nervenarzt 62:697–703
Robertson E, Grace S, Wallington T (2004) Antenatal risk factors for postpartum depression: a synthesis of recent literature. Gen Hosp Psychiatry 26:289–295
Sheehan DV, Lecrubier Y, Harnett Sheehan K, Amorim P, Janavs J, Weiller E et al (1998a) The Mini International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview. J Clin Psychiatry 59(supp 20):22–33
Sheehan DV, Lecrubier Y, Harnett Sheehan K, Janavs J, Weiller E, Keskiner A et al (1998b) The validity of the Mini International Neuropsychiatric Interview (MINI) according to the SCID-P and its reliability. Eur Psychiatry 12(5):232–241
West J (1985) An Arabic validation of a depression inventory. Int J Soc Psychiatry 31:282–289
Wisner KL, Barbara L, Parry MD, Piontek CM (2002) Postpartum depression. N Eng J Med 347(3):194–199
Acknowledgments
This project was funded by grant #060909 from the College of Graduate Studies and Research, University of Sharjah, United Arab Emirates. The authors would like to thank the Ministry of Health in Sharjah for granting permission to conduct the study, Dr. Sanaa Z. Mustafa at the Maternal and Child Health Center for her feedback and assistance in arranging for data collection, Asma Habbal for her committed efforts in translation and data collection and all of the participants who gave of their time for the study.
Ethical standards
This study has been approved by the Institutional Review Board of the University of Sharjah and has been performed in accordance with the ethical standards of the 1964 Declaration of Helsinki. All participants provided their informed consent prior to inclusion in the study. Details of participants that might disclose their identity have been omitted.
Conflict of interest
Aisha Hamdan was employed as an Assistant Professor in the University of Sharjah, (sponsor of the study) at the time of the study. There is no relationship with the Maternal and Child Health Center in which the study was conducted. Hani Tamim has no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hamdan, A., Tamim, H. Psychosocial risk and protective factors for postpartum depression in the United Arab Emirates. Arch Womens Ment Health 14, 125–133 (2011). https://doi.org/10.1007/s00737-010-0189-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00737-010-0189-8