Abstract
Aminopeptidases represent a class of (zinc) metalloenzymes that catalyze the cleavage of amino acids nearby the N-terminus of polypeptides, resulting in hydrolysis of peptide bonds. Aminopeptidases operate downstream of the ubiquitin–proteasome pathway and are implicated in the final step of intracellular protein degradation either by trimming proteasome-generated peptides for antigen presentation or full hydrolysis into free amino acids for recycling in renewed protein synthesis. This review focuses on the function and subcellular location of five key aminopeptidases (aminopeptidase N, leucine aminopeptidase, puromycin-sensitive aminopeptidase, leukotriene A4 hydrolase and endoplasmic reticulum aminopeptidase 1/2) and their association with different diseases, in particular cancer and their current position as target for therapeutic intervention by aminopeptidase inhibitors. Historically, bestatin was the first prototypical aminopeptidase inhibitor that entered the clinic 35 years ago and is still used for the treatment of lung cancer. More recently, new generation aminopeptidase inhibitors became available, including the aminopeptidase inhibitor prodrug tosedostat, which is currently tested in phase II clinical trials for acute myeloid leukemia. Beyond bestatin and tosedostat, medicinal chemistry has emerged with additional series of potential aminopeptidases inhibitors which are still in an early phase of (pre)clinical investigations. The expanded knowledge of the unique mechanism of action of aminopeptidases has revived interest in aminopeptidase inhibitors for drug combination regimens in anti-cancer treatment. In this context, this review will discuss relevant features and mechanisms of action of aminopeptidases and will also elaborate on factors contributing to aminopeptidase inhibitor efficacy and/or loss of efficacy due to drug resistance-related phenomena. Together, a growing body of data point to aminopeptidase inhibitors as attractive tools for combination chemotherapy, hence their implementation may be a step forward in a new era of personalized treatment of cancer patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
More than 50 years ago, Rutenburg et al. (1958) and Willighagen and Planteydt (1959) were the first to report the potential relevance of aminopeptidase activity for cancer. Rutenburg et al. (1958) demonstrated that patients with pancreatic cancer had significantly increased leucine aminopeptidase (LAP) activity in serum and urine, whereas patients with a malignant lymphoma or leukemia had increased LAP activity in urine. Willighagen and Planteydt (1959) also observed higher aminopeptidase activity in tumor cells and stroma in sixty surgically removed human neoplasms. Twenty years later, Umezawa et al. (1976) discovered one of the first aminopeptidase inhibitors; bestatin, being produced by actinomycetes, a group of gram-positive bacteria.
Aminopeptidases, a class of (zinc) metalloenzymes, catalyze the cleavage of amino acids nearby the N-terminus of polypeptides, facilitating hydrolysis of the peptide bond (Taylor 1993). Binding of one or two metal ions, mostly zinc, is required for the activity of the aminopeptidases. Some of these enzymes require two metal ions for full activity, for others only one metal ion is sufficient for catalysis, while the second metal ion can modulate the activity either positively or negatively. Aminopeptidases are widely distributed throughout plants, animals, bacteria and fungi, and function in many cellular processes (Lowther and Matthews 2002). Their function is implicated in the final step of intracellular protein degradation by trimming peptides produced by the ubiquitin–proteasome pathway either for antigen presentation or for full hydrolysis into free amino acids, which can be reutilized for renewed protein synthesis (Saric et al. 2004) (Fig. 1). The critical relevance of these functions for cancer progression paved the way to explore inhibitors of aminopeptidases for application as anti-cancer therapeutic drugs. The mechanistic rationale and current status of established and experimental aminopeptidase inhibitors for next generation cancer therapy are discussed hereafter.
Protein degradation pathway; role of proteasome and aminopeptidases. aa Amino acid, TOP thimet oligopeptidases, MHC major histocompatibility complex. Modified from Saric et al. (2004)
Positioning of aminopeptidases
Mechanism of action downstream of the ubiquitin–proteasome pathway
The ubiquitin–proteasome pathway is the major proteolytic system in the cytosol of eukaryotic cells and plays an important role in protein homeostasis, degradation of specific short-lived proteins and rapid elimination of damaged or misfolded proteins. Intracellular ubiquitin-mediated protein degradation is highly selective; different proteins can have a half-life that varies from a few minutes to several days and up to a few years. This process is tightly regulated and has been implicated in numerous key processes such as DNA repair, cell-cycle progression, signal transduction, transcriptional regulation, receptor down-regulation, and gene expression. The ubiquitin system is also essential for immune response, development, and programmed cell death (Goldberg 2003; Hershko and Ciechanover 1992).
Two main steps are involved in the degradation of a protein via the ubiquitin–proteasome pathway: (1) labeling of the protein by the covalent attachment of multiple ubiquitin (Ub) molecules and (2) degradation of the labeled protein by the 26S proteasome complex. These steps require the sequential action of three enzymes; E1 (Ub-activation), E2 (Ub-conjugation) and E3 (Ub-ligation). The short peptides, ultimately generated by the ubiquitin–proteasome processes are short-lived and do not accumulate in cells, but are further degraded to free amino acids by cytosolic peptidases, such as aminopeptidases (Emmerich et al. 2000; Glickman and Ciechanover 2002; Hershko 2005; Hershko and Ciechanover 1998; Kisselev et al. 1998, 1999; Lecker et al. 2006).
Aminopeptidases directly degrade the smallest products (2–6 amino acids) released from the proteasome complex, whereas larger peptides (6–24 amino acids) are primarily cleaved by endopeptidases, such as thimet oligopeptidases (TOP) and tripeptidyl peptidase II (TPPII), into shorter peptides (2–6 amino acids), which subsequently can be fully hydrolyzed by aminopeptidases (Fig. 1; complete hydrolysis) to free amino acids being available again for new protein synthesis (Botbol and Scornik 1979; Saric et al. 2004).
A very small fraction of the proteasome products can escape the complete hydrolysis and is utilized for major histocompatibility complex (MHC) class I antigen presentation (Fig. 1; antigen presentation). These peptides are transported from the cytosol into the endoplasmic reticulum (ER) by the transporter associated with antigen processing (TAP). In addition, the N-terminal extension of peptides can be processed before transportation (cytosol) or after transportation (ER) by specific aminopeptidases. This phenomenon is also called ‘trimming’ (Glickman and Ciechanover 2002; Groettrup et al. 1996; Saric et al. 2004). Subsequently, the MHC class I molecules bind the (trimmed) peptides (8–10 amino acids) and expose them on the cell surface for recognition by cytotoxic T lymphocytes and initiating an immune response (Rock and Goldberg 1999). The role of aminopeptidase activity in antigen presentation has been subject of various reviews (Dong et al. 2000; Hattori and Tsujimoto 2004; Kim et al. 2009; Larsen et al. 1996; Reits et al. 2003; Rock et al. 2004; Yewdell and Princiotta 2004). This review will primarily focus on the role of aminopeptidases in the peptide hydrolysis to amino acids from a cancer perspective.
Function and location of different aminopeptidases and their association with different diseases
The function and subcellular location of at least five aminopeptidases [aminopeptidase N (APN), leucine aminopeptidase (LAP), puromycin-sensitive aminopeptidase (PuSA), leukotriene A4 (LTA4) hydrolase and endoplasmic reticulum aminopeptidase 1/2 (ERAP1/2)] has been associated with the pathophysiology of different non-malignant diseases (discussed in this section) as well as with (different types of) cancer (discussed in the next section). Aminopeptidases can be subdivided into three general groups, based on their function, those that: (1) hydrolyze the first peptide bond (aminoacyl- and iminoacyl-peptide hydrolases), (2) remove dipeptides from polypeptide chains (dipeptidyl-peptide hydrolases), and (3) only act on tripeptides (tripeptidyl-peptide hydrolases) (Sanderink et al. 1988). They can also be subdivided based on structural characteristics. Four of the five aminopeptidases (APN, PuSA, LTA4 hydrolase and ERAP1/2) belong to the M1 zinc-aminopeptidases subfamily, which harbor a consensus HEXXH (18X) E motif for zinc binding. This zinc ion binding is essential for the enzymatic activity of aminopeptidases (Sato 2004). LAP is a member of the peptidase M17 family.
Aminopeptidase N (APN)
Aminopeptidase N (APN, also known as CD13) has been referred to as a ‘moonlighting ectoenzyme’, because it can fulfill a multitude of functions (Mina-Osorio 2008). Upon ligand binding, APN can operate as an enzyme, a receptor and/or signaling molecule. Each of these three functions is associated with their own mechanism of action; peptide cleavage, endocytosis and signal transduction, respectively. Subsequently, each of these three mechanisms elicited different biological effects. Generally, APN plays a role in the final digestion of peptides generated from hydrolysis of proteins and polypeptides, in particular those involved in the metabolism of various regulatory peptides that impact the function of small intestinal and tubular epithelial cells, macrophages, granulocytes and synaptic membranes from the CNS (Mina-Osorio 2008; Santos et al. 2000). Moreover, APN can cleave antigenic peptides prior to binding to MHC class II molecules of antigen presenting cells (Dong et al. 2000).
Leucine aminopeptidase (LAP)
Unlike APN, leucine aminopeptidase (LAP, also known as cytosol aminopeptidase) is less well characterized. It catalyzes the removal of unsubstituted N-terminal amino acids from various peptides and is presumably involved in the processing and regular turnover of intracellular proteins (Matsushima et al. 1991). Subsequently, it processes antigenic peptides for presentation by the MHC class I molecules (Beninga et al. 1998). LAP is located in the cytoplasm, but data on tissue specificity are scarce. LAP has been implicated in a small variety of pathophysiological states, including HIV infection (Pulido-Cejudo et al. 1997), systemic lupus erythematosus (Inokuma et al. 1999) and malaria (Lee et al. 2010).
Puromycin-sensitive aminopeptidase (PuSA)
Puromycin-sensitive aminopeptidase (PuSA) has broad substrate specificity for several peptides and is involved in proteolytic events essential for cell growth and viability (Constam et al. 1995). As for APN, PuSA is thought to act as a regulator of neuropeptide activity (Tobler et al. 1997) and plays an important role in the antigen processing pathway for MHC class I molecules (Kim et al. 2009; Stoltze et al. 2000; Towne et al. 2008). PuSA is also able to digest polyglutamine (polyQ) peptides found in many cellular proteins (Bhutani et al. 2007).
PuSA is localized in both the cytoplasm and cellular membranes, and was found in liver, epithelium of renal tubules, epithelium of small and large intestine, gastric epithelial cells, and alveoli of the lung (Yamamoto et al. 2000).
PuSA was found to be involved in the degradation of tau (Sengupta et al. 2006), which does it more efficiently in normal brain compared to brain from Alzheimer disease patients (Hui 2007).
Leukotriene A4 (LTA4) hydrolase
Leukotriene A4 (LTA4) hydrolase is involved in the removal of a single N-terminal amino acid residue and exhibits a variety of important biological functions, including the processing of cell surface antigens and involvement in tumor angiogenesis. LTA4 hydrolysis catalyzes the formation of the chemotaxin leukotriene B4 (LTB4), a key lipid mediator of the innate immune response; it stimulates adhesion of circulating neutrophils to vascular endothelium and directs their migration to sites of inflammation (Fitzpatrick et al. 1994; Radmark et al. 1984; Tholander et al. 2008).
LTA4 hydrolase is compartmentalized in lipid-rich organelles (lipid droplets) residing in the cytoplasm (Bozza et al. 2009) and is expressed in monocytes, lymphocytes, neutrophils, reticulocytes, platelets and fibroblasts (Haeggström 2004; Haeggström et al. 2002).
LTB4 plays an important role in a variety of allergic and inflammatory reactions, due to these biological activities of LTB4, LTA4 hydrolase is involved in a variety of acute and chronic inflammatory diseases, e.g., nephritis, arthritis, dermatitis, chronic obstructive pulmonary disease and asthma (Haeggström 2004; Haeggström et al. 2002; Holloway et al. 2008; De Oliveira et al. 2011; Thunnissen et al. 2001).
Endoplasmic reticulum aminopeptidase 1/2 (ERAP1/2)
The main function of endoplasmic reticulum aminopeptidase 1 and 2 [ERAP1; also known as puromycin-insensitive leucine aminopeptidase (PILSAP) and ERAP2] involves trimming of HLA class I-binding precursors in the endoplasmic reticulum (ER) for MHC class I antigen presentation. ERAP1 and 2 can act as monomer, but mostly function as heterodimers allowing them to combine their restricted specificities to remove complex N-terminal extensions. In addition, ERAP1 has a unique substrate preference; it strongly prefers peptide substrates between nine and sixteen amino acid residues long and thereby covers the formation of about one-third of peptide–MHC class I complexes. ERAP2 presents distinct specificity for the N-terminal residue of the peptide substrates. Both enzymes are also thought to play a role in the inactivation of peptide hormones (Birtley et al. 2012; Nguyen et al. 2011; Saric et al. 2002; Saveanu et al. 2005; Serwold et al. 2002; York et al. 2002). ERAP1 is also found to be involved in blood pressure regulation by inactivation of angiotensin II (Hallberg and Michaëlsson 2003).
ERAP1 and 2 are localized on the ER membrane and are ubiquitously expressed, mostly in spleen and leukocytes (Saveanu et al. 2005).
Relation between aminopeptidases and cancer
Aminopeptidases are essential for physiologically important processes such as protein maturation, degradation of peptides, and cell-cycle control. For cancer cells, the supply of cellular free amino acids, regulated by aminopeptidases, is of utmost importance for their survival and proliferation. Importantly, many tumor cells are dependent on specific amino acids and depletion of these amino acids has a greater impact on cancer cells than normal cells (Scott et al. 2000). Moore et al. (2009) indicated that myeloid leukemia and multiple myeloma cells were highly dependent on the unfolded protein response in which aminopeptidases play an important role. Consistently, this study showed that aminopeptidase inhibition resulted in marked inhibition of myeloma cell growth and survival, and thus is of potential therapeutic interest. Martínez et al. (1999) documented both up- and down-regulation of selective aminopeptidase activities in breast cancer tissue. These alterations were dependent on local hormonal status, indicating that tumor microenvironment plays a role in regulating aminopeptidase expression. Cifaldi et al. (2012) discussed the outcome of six different studies that assessed the expression and tissue distribution of endoplasmic reticulum aminopeptidase 1 and 2 (ERAP1 and ERAP2) in tumor cells of lymphoid and non-lymphoid origin compared to their normal counterparts. In one study including eleven different tumor cell lines (melanomas, leukemia-lymphomas and carcinomas of breast, colon, lung, chorion, skin, prostate, cervix, kidney and bladder), ERAP1 and 2 were expressed at highly variable levels. In a second study, the expression of ERAP1 and ERAP2 was either lost, acquired or retained in 150 surgically removed neoplastic lesions as compared to their normal histotype counterparts. Down-regulation of ERAP1 and/or ERAP2 expression was mainly found in ovarian, breast and lung carcinomas, whereas an up-regulation of these enzymes was observed in colon and thyroid carcinomas. A third study reported heterogeneous expression of ERAP1 and ERAP2, ranging from high to very low levels, in 28 melanoma cell lines as compared to primary melanocytes. Three other studies demonstrated ERAP1 expression in 64 % of endometrial carcinomas, in which ERAP1 may function to suppress angiogenesis and endothelial cell migration. Both ERAP1 and 2 are present in leukemia, lymphoma, carcinoma, and melanoma cell lines (Fruci et al. 2008; Fruci and Ferracuti 2006; Kamphausen et al. 2010; Mehta et al. 2009). Mostly ERAP1 is involved in a few types of cancer, such as endometrial carcinoma (Watanabe et al. 2003) and cervical carcinoma (Mehta et al. 2009).
Most studies on aminopeptidase activity in correlation with cancer are focused on aminopeptidase N (APN), a zinc-dependent membrane-bound ectopeptidase that degrades preferentially proteins and peptides with a N-terminal neutral amino acid. Tokuhara et al. (2006) investigated the clinical significance of aminopeptidase N in non-small cell lung cancer (NSCLC) and were the first to show a relationship between APN expression and poor prognosis of patients with NSCLC. Van Hensbergen et al. (2002) found elevated soluble APN activity in plasma and effusions of cancer patients, which was strongly correlated with tumor load. APN also appeared to be involved in cell motility of thyroid carcinoma cells (Kehlen et al. 2003), of which undifferentiated anaplastic thyroid carcinomas had a higher APN expression than differentiated thyroid carcinomas. Increased APN expression was associated in the pathophysiology of additional types of cancer; head and neck squamous-cell carcinoma (Pérez et al. 2009), acute myeloid leukemia (Lee et al. 2003; Piedfer et al. 2011), prostate cancer (Ishii et al. 2001) and colon cancer (Hashida et al. 2002). Beyond this, APN was also found to be selectively expressed in the vasculature of tissues that undergo angiogenesis, e.g., in malignant gliomas and lymph node metastases from multiple tumor types, but not in blood vessels of normal tissues (Pasqualini et al. 2000). In line with these observations, APN serves as a receptor for a specific motif (NGR), which is expressed on endothelial cells of angiogenic vasculature (Wickström et al. 2011). Collectively, it can be concluded that an increased APN expression was related to a more malignant phenotype.
Other than for APN and ERAP, cancer-related involvement of additional aminopeptidases is less well documented. Notwithstanding this fact, LAP activity appeared to play a role in prostate carcinoma (Rackley et al. 1991) and head and neck cancer (Garg et al. 1994), PuSA activity in clear cell renal cancer (Varona et al. 2007) and prostate adenocarcinoma (Lee 2009), and LTA4 hydrolase in lung cancer (Abe et al. 1996), esophageal adenocarcinoma (Chen et al. 2003), colon cancer (Jeong et al. 2009) and pancreatic cancer (Oi et al. 2010).
In conclusion, there is a growing body of evidence that pinpoint aminopeptidase activity, especially APN and ERAP1/2, to a great variety of cancer types and their progressive and proliferative state.
Mechanism of action of aminopeptidase inhibitors
The first clinically approved aminopeptidase inhibitor bestatin (Ubenimex), discovered by Umezawa et al. (1976), was originally designed as an immune-modulating agent. Follow-up research demonstrated that bestatin also harbored anti-proliferative effects and displayed activity as an anti-cancer drug, corroborating the relevance of aminopeptidases in cancer tissue (Rutenburg et al. 1958; Sawafuji et al. 2003; Scornik and Botbol 2001; Willighagen and Planteydt 1959). As a mechanism of action, Taylor (1993) revealed that bestatin was tightly bound to the aminopeptidases LAP and APN. Each subunit of LAP was capable of bestatin binding, but the binding of one bestatin molecule was already sufficient to exert an inhibitory effect. In addition, Botbol and Scornik (1991) noted that bestatin induced the accumulation of di- and tripeptide intermediates, again indicating aminopeptidase inhibition as a mechanism of action. Almost two decades later, Krige et al. (2008) provided evidence that for the aminopeptidase inhibitor prodrug tosedostat (CHR2797), its main mechanism of action was to provoke a depletion of intracellular amino acids, which suppressed cell growth. Consistent with earlier studies, also tosedostat exposure introduced intracellular accumulation of small peptides. Intracellular amino acid depletion triggers the so-called amino acid deprivation response (AADR), which is involved in transcriptional and post-transcriptional regulatory mechanisms, such as up-regulation of amino acid synthetic genes, amino acid transporters, and tRNA synthetases (Fig. 2). Lastly, Krige et al. (2008) observed that aminopeptidase inhibition reduced the phosphorylation of mammalian target of rapamycin (mTOR) substrates to suppress rates of protein synthesis. mTOR is a protein kinase known as the master regulator of protein synthesis, cell growth and proliferation (Laplante and Sabatini 2012). The mTOR protein consists of two distinct multi-protein complexes; mTOR complex 1 (mTORC1) and mTOR complex 2 (mTORC2). mTORC1 stimulates protein synthesis by phosphorylating the eukaryotic initiation factor 4E-binding protein 1 (4E-BP1) and the p70 ribosomal 6S kinase 1 (S6K1). Phosphorylation of 4E-BP1 prevents its binding to eukaryotic initiation factor 4E (eIF4E), enabling eIF4E to promote cap-dependent translation. The induction of S6K1 activity by mTORC1 leads to an increase in mRNA biogenesis, cap-dependent translation and elongation, and the translation of ribosomal proteins through regulation of the activity of many proteins. Amino acids can strongly regulate mTORC1 activity, but the mechanism by which intracellular amino acids signal to mTORC1 is still largely unresolved. Recent evidence suggested that the amino acid leucine is essential for mTORC1 activation, levels of which rely on transport into cells in a glutamine-dependent fashion (Laplante and Sabatini 2009). Next, the rag proteins, a family of four related small GTPases, also interact with mTORC1 in an amino acid-sensitive manner and are also necessary for the activation of the mTORC1 pathway (Sancak et al. 2008). In contrast to mTORC1, mTORC2 activity is less directly affected by amino acid depletion, though through facilitating phosphorylation of Akt, it can promote mTORC1 activity as a compensatory mechanism. As such, mTORC2 plays key roles in cell survival, metabolism, proliferation and cytoskeleton organization (Goberdhan 2010; Hay and Sonenberg 2004; Laplante and Sabatini 2009).
Mechanism of action of aminopeptidase inhibitors bestatin and tosedostat. Aminopeptidase inhibitors elicit two main effects: (1) amino acid deprivation response (AADR) and (2) inhibition of mTOR. Modified from Löwenberg et al. (2010)
Collectively, aminopeptidase inhibitors elicit their effect mainly by induction of AADR and reduction of mTOR activity, which ultimately results in the inhibition of cell growth, cell proliferation, cell motility, cell survival, protein synthesis and transcription (Guertin and Sabatini 2007; Laplante and Sabatini 2012; Löwenberg et al. 2010). This unique mechanism of action merits further clinical exploitation and implementation in current cancer chemotherapy.
Aminopeptidase inhibitors in cancer therapy
Currently, neither the European Medicines Agency (EMA) nor the Food and Drug Administration (FDA) has approved any aminopeptidase inhibitor in an anti-cancer treatment setting. However, some clinical trials are ongoing or completed, being most advanced for bestatin (Ubenimex) and tosedostat (CHR2797). Whereas bestatin is a direct aminopeptidase inhibitor, Tosedostat is a hydrophobic aminopeptidase inhibitor prodrug that is rapidly taken up by cells and then intracellular activated by de-esterification into a hydrophilic pharmacologically active acid product (CHR79888). This hydrophilic metabolite is efficiently retained in cells to exert an inhibitory effect to multiple aminopeptidases, with preference for LTA4 hydrolase, APN and LAP (Krige et al. 2008). Below, different aminopeptidases will be discussed in the context of clinical cancer therapy and the development of next generation experimental aminopeptidase inhibitors.
Aminopeptidase inhibitors tested in the clinic
Bestatin was used in Japan as an immunomodulator and antitumor drug (lung cancer and acute myeloid leukemia), under the trademark Ubenimex (Nippon Kayaku Co, Tokyo) (Scornik and Botbol 2001). Its broader clinical development proceeds at a low scale. The outcome of recent clinical studies in solid tumors and leukemia with single agent bestatin and tosedostat is shown in Table 1.
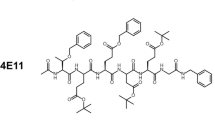
New compounds in development
There are two main approaches for aminopeptidase targeting; by direct inhibition or via prodrugs, which are enzymatically metabolized into pharmacologically active acid products (Wickström et al. 2011). To improve on selectivity, pharmacokinetics/dynamics, most rationally designed novel aminopeptidase inhibitors build on bestatin as prototypical compound. Remarkably, most of newly generated compounds came out as inhibitors of APN rather than of other aminopeptidases. A selection of recently identified experimental aminopeptidase inhibitors; their chemical structure and activity profile are listed in Table 2.
Aminopeptidase inhibitory profiles of classical and novel experimental aminopeptidase inhibitors
Following medicinal chemistry, preclinical evaluation of classical and novel experimental aminopeptidase inhibitors includes assessment of their inhibitory potency against one or multiple crude/purified aminopeptidases from human and rodent sources. Table 3 provides an overview of inhibitory potency of bestatin, tosedostat and selected novel aminopeptidase inhibitors against APN (most commonly tested), LAP, PuSA, LTA4-hydrolase and ERAP1. With bestatin and tosedostat/CHR79888 as a reference, displaying potent inhibitory effects against APN, LAP, LTA4 hydrolase and PuSA, most novel inhibitors displayed APN inhibitory capacity, with the 4cc compound being more potent than bestatin and tosedostat. Overall, natural inhibitors showed lower toxicity, broad spectrum activity and poor tissue specificity as compared to synthetic inhibitors (Mina-Osorio 2008). It remains a challenge to design inhibitors that could selectively target specific aminopeptidases, which can be implicated in cancer or chronic inflammatory diseases (e.g., LTA4 hydrolase).
Resistance modalities for aminopeptidase inhibitors
Prolonged drug administration often comes along with the onset of acquired drug resistance. Also for aminopeptidase inhibitors, therapy resistance may occur as observed in a phase I/II clinical study with tosedostat (Löwenberg et al. 2010). However, the molecular basis for resistance remains elusive. Some mechanisms that may confer resistance are briefly discussed below just as options to overcome resistance.
Possible mechanisms of resistance
One general mechanism of drug resistance relates to cellular extrusion of drugs, mediated by ATP-dependent drug efflux pumps (Gottesman et al. 2002). In fact, Grujić and Renko (2002) showed that inhibition of multidrug resistance-associated protein (MRP) and P-glycoprotein (P-gp) enhanced the activity of both bestatin and actinonin, suggesting that these compounds may be substrates for these efflux pumps. In addition, activation of mTOR by free amino acids can induce resistance as part of overcoming the amino acid deprivation response (Laplante and Sabatini 2009). These amino acids may be delivered through upregulated expression of amino acid transporters. Consistently, Fan et al. (2010) showed that l-amino acid transporter (LAT1) was upregulated in human ovarian cancer cells and that the inhibition of LAT1 sensitized cells for bestatin. Conceivably, for aminopeptidase inhibitor prodrugs like tosedostat, it may be anticipated that down-regulation of carboxylesterases, implicated in the conversion of tosedostat to the active metabolite CHR79888 (Krige et al. 2008), could be a contributing factor in loss of activity of tosedostat. These mechanisms warrant further exploration and confirmation in preclinal model systems and in a clinical setting.
Combination therapy to bypass resistance
Personalized medicine has received considerable attention in current cancer chemotherapeutic approaches. Aminopeptidase inhibitors can either be used in combination with other drugs to enhance their own activity and reduce toxicity, or could constitute synergistic interactions with other chemotherapeutic or therapies. Table 4 depicts an overview of completed and ongoing clinical studies of combination therapies with aminopeptidase inhibitors. As an example, Fan et al. (2010) showed that the combination of bestatin and a LAT1 inhibitor significantly increased bestatin activity in human ovarian cancer cells, which may thus be considered as an improved treatment option for ovarian cancer patients. Tsukamoto et al. (2008) demonstrated that inhibition of APN by Ubenimex enhanced radiosensitivity of cervical cancer cells in vitro as well as in vivo (mouse models). In the clinical setting, tosedostat is combined with standard chemotherapy regimens to determine whether this would improve their efficacy. Moreover, inhibition of aminopeptidases leading to amino acid deprivation has a clear scientific rationale for these combinations. e.g., for the synthesis of RNA and DNA precursors amino acids are essential, so that combination with antimetabolites, such as with cytarabine in AML is likely to be beneficial (Peters and Jansen 2001). Moreover, inhibition of either aminopeptidases or the proteasome will prevent degradation of enzymes involved in DNA repair, apoptosis and signaling. Therefore, interaction with drugs such as anthracyclines, also used in the treatment of AML is likely to be synergistic. All these options need further investigations. Together, the unique mechanism of action of aminopeptidase inhibitors has attractive options to further explore synergistic drug/therapeutic combinations.
Concluding remarks
A growing body of data has underscored the critical role of aminopeptidases in various types of cancer tissues. One role involves protein/peptidase degradation to free amino acid which is required for renewed protein biosynthesis, while the other role involves trimming of antigenic peptides for MHC class I presentation. Although aminopeptidases represent attractive candidates for therapeutic intervention, development of aminopeptidase inhibitors is in a relatively early stage, compared to the development of inhibitors of the proteasome, which functions upstream of aminopeptidases in protein degradation. This may be related to the broad spectrum of functions regulated by individual aminopeptidases preventing a specific inhibition. Moreover, aminopeptidase inhibition may affect various physiological processes (e.g., cell adhesion, enzymatic regulation of peptides, differentiation, proliferation, chemotaxis, antigen presentation, cholesterol metabolism, phagocytosis and angiogenesis). However, in a cancer therapeutic setting, two of the most advanced studied aminopeptidase inhibitors (i.e., bestatin and tosedostat) were generally well tolerated with most of the patients only experiencing mild adverse events (grade 1–2). Another unresolved issue relates to the fact that aminopeptidases have a broad and overlapping substrate specificity, and therefore inhibition may not always be specific. It is a challenge for medicinal chemists to rationally design selective inhibitors for individual aminopeptidases and explore whether this could elicit differential effects against specific types of cancer, or even non-malignant diseases (e.g., HIV, malaria, Alzheimer disease, chronic inflammatory diseases). Expanded knowledge of the mechanism of action and putative resistance modalities may also help to define optimal application of aminopeptidase inhibitors in future cancer chemotherapy. Lessons learned from (pre)clinical investigations with tosedostat highlighted the impact of the amino acid depletion and inability to deal with the associated amino acid deprivation response as a critical factor in suppressing cancer cell growth (Krige et al. 2008). Hence, promoting compensatory effects for amino acid depletion could dictate the efficacy of aminopeptidase inhibitors as stand-alone drugs. However, given their unique mechanism of action, it is anticipated that the most successful application will adhere to combinations with other chemotherapeutic drugs. As such, aminopeptidases and their inhibitors hold promise for future rationally designed chemotherapeutic applications.
References
Abe M, Matsuki H, Domae M, Kuwata H, Kudo I, Nakanishi Y, Hara N, Mitsuyama T, Furukawa T (1996) Lung cancer cell lines inhibit leukotriene B4 production by human polymorphonuclear leukocytes at the level of phospholipase A2. Am J Respir Cell Mol Biol 15:565–573
Aoyagi T, Tobe H, Kojima F, Hamada M (1978) Amastatin, an inhibitor of aminopeptidase A, produced by actinomycetes. J Antibiot 31:636–638
Beninga J, Rock KL, Goldberg A (1998) Interferon-gamma can stimulate post-proteasomal trimming of the N terminus of an antigenic peptide by inducing leucine aminopeptidase. J Biol Chem 273:18734–18742
Bhutani N, Venkatraman P, Goldberg A (2007) Puromycin-sensitive aminopeptidase is the major peptidase responsible for digesting polyglutamine sequences released by proteasomes during protein degradation. EMBO J 26:1385–1396. doi:10.1038/sj.emboj.7601592
Birtley JR, Saridakis E, Stratikos E, Mavridis IM (2012) The crystal structure of human endoplasmic reticulum aminopeptidase 2 reveals the atomic basis for distinct roles in antigen processing. Biochemistry 51:286–295. doi:10.1021/bi201230p
Botbol V, Scornik O (1979) Degradation of abnormal proteins in intact mouse reticulocytes: accumulation of intermediates in the presence of bestatin. Proc Natl Acad Sci USA 76:703–710
Botbol V, Scornik O (1991) Measurement of instant rates of protein degradation in the livers of intact mice by the accumulation of bestatin-induced peptides. J Biol Chem 266:2151–2157
Bozza PT, Magalhães KG, Weller PF (2009) Leukocyte lipid bodies––biogenesis and functions in inflammation. Biochim Biophys Acta 1791:540–551. doi:10.1016/j.bbalip.2009.01.005
Chen X, Li N, Wang S, Wu N, Hong J, Jiao X, Krasna MJ, Beer DG, Yang CS (2003) Leukotriene A4 hydrolase in rat and human esophageal adenocarcinomas and inhibitory effects of bestatin. J Natl Cancer Inst 95:1053–1061
Cifaldi L, Romania P, Lorenzi S, Locatelli F, Fruci D (2012) Role of endoplasmic reticulum aminopeptidases in health and disease: from infection to cancer. Int J Mol Sci 13:8338–8352. doi:10.3390/ijms13078338
Constam DB, Tobler AR, Rensing-ehl A, Kemler I, Hersh LB, Fontana A (1995) Puromycin-sensitive aminopeptidase. Sequence analysis, expression, and functional characterization. J Biol Chem 270:26931–26939
De Oliveira E, Wang K, Kong H (2011) Effect of the leukotriene A4 hydrolase aminopeptidase augmentor 4-methoxydiphenylmethane in a pre-clinical model of pulmonary emphysema. Bioorg Med Chem Lett 21:6746–6750. doi:10.1016/j.bmcl.2011.09.048.Effect
Dong X, An B, Salvucci Kierstead L, Storkus WJ, Amoscato AA, Salter RD (2000) Modification of the amino terminus of a class II epitope confers resistance to degradation by CD13 on dendritic cells and enhances presentation to T cells. J Immunol 164:129–135
Emmerich NP, Nussbaum AK, Stevanovic S, Priemer M, Toes RE, Rammensee HG, Schild H (2000) The human 26 S and 20 S proteasomes generate overlapping but different sets of peptide fragments from a model protein substrate. J Biol Chem 275:21140–21148. doi:10.1074/jbc.M000740200
Fan X, Ross DD, Arakawa H, Ganapathy V, Tamai I, Nakanishi T (2010) Impact of system L amino acid transporter 1 (LAT1) on proliferation of human ovarian cancer cells: a possible target for combination therapy with anti-proliferative aminopeptidase inhibitors. Biochem Pharmacol 80:811–818. doi:10.1016/j.bcp.2010.05.021
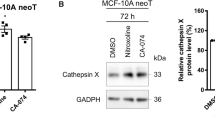
Feng J, Jin K, Zhu H, Zhang X, Zhang L, Liu J, Xu W (2012) A novel aminopeptidase N inhibitor developed by virtual screening approach. Bioorg Med Chem Lett 22:5863–5869. doi:10.1016/j.bmcl.2012.07.086
Fitzpatrick F, Lepley R, Orning L, Duffin K (1994) Suicide inactivation of leukotriene A4 hydrolase/aminopeptidase. Ann N Y Acad Sci 744:31–38
Fruci D, Ferracuti S (2006) Expression of endoplasmic reticulum aminopeptidases in EBV-B cell lines from healthy donors and leukemia/lymphoma, carcinoma, and melanoma cell lines. J Immunol 176:4869–4879
Fruci D, Giacomini P, Nicotra MR, Forloni M, Fraioli R, Saveanu L, Van Endert P, Natali PG (2008) Altered expression of endoplasmic reticulum aminopeptidases ERAP1 and ERAP2 in transformed non-lymphoid human tissues. J Cell Physiol 216:742–749. doi:10.1002/jcp.21454
Gao J-J, Gao Z-H, Zhao C-R, Yuan Y, Cui S-X, Zhang X-F, Cheng Y-N, Xu W-F, Tang W, Qu X-J (2011) LYP, a novel bestatin derivative, inhibits cell growth and suppresses APN/CD13 activity in human ovarian carcinoma cells more potently than bestatin. Invest New Drugs 29:574–582. doi:10.1007/s10637-010-9391-9
Garg LN, Yadav SP, Lal H (1994) Serum leucine aminopeptidase in head and neck cancer. J Laryngol Otol 108:660–662
Glickman MH, Ciechanover A (2002) The ubiquitin-proteasome proteolytic pathway: destruction for the sake of construction. Physiol Rev 82:373–428. doi:10.1152/physrev.00027.2001
Goberdhan D (2010) Intracellular amino acid sensing and mTORC1-regulated growth: new ways to block an old target? Curr Opin Investig Drugs 11:1360–1367
Goldberg AL (2003) Protein degradation and protection against misfolded or damaged proteins. Nature 426:895–899. doi:10.1038/nature02263
Gottesman MM, Fojo T, Bates SE (2002) Multidrug resistance in cancer: role of ATP-dependent transporters. Nat Rev Cancer 2:48–58. doi:10.1038/nrc706
Groettrup M, Soza A, Kuckelkorn U, Kloetzel P (1996) Peptide antigen production by the proteasome: complexity provides efficiency. Immunol Today 17:429–435
Grujić M, Renko M (2002) Aminopeptidase inhibitors bestatin and actinonin inhibit cell proliferation of myeloma cells predominantly by intracellular interactions. Cancer Lett 182:113–119
Guertin DA, Sabatini DM (2007) Defining the role of mTOR in cancer. Cancer Cell 12:9–22. doi:10.1016/j.ccr.2007.05.008
Haeggström JZ (2004) Leukotriene A4 hydrolase/aminopeptidase, the gatekeeper of chemotactic leukotriene B4 biosynthesis. J Biol Chem 279:50639–50642. doi:10.1074/jbc.R400027200
Haeggström JZ, Nordlund P, Thunnissen MMGM (2002) Functional properties and molecular architecture of leukotriene A4 hydrolase, a pivotal catalyst of chemotactic leukotriene formation. Sci World J 2:1734–1749. doi:10.1100/tsw.2002.810
Hallberg L, Michaëlsson K (2003) Adipocyte-derived leucine aminopeptidase genotype and response to antihypertensive therapy. BMC cardiovasc Disord 6:7–12
Hashida H, Takabayashi A, Kanai M, Adachi M, Kondo K, Kohno N, Yamaoka Y, Miyake M (2002) Aminopeptidase N is involved in cell motility and angiogenesis: its clinical significance in human colon cancer. Gastroenterology 122:376–386. doi:10.1053/gast.2002.31095
Hattori A, Tsujimoto M (2004) Processing of antigenic peptides by aminopeptidases. Biol Pharm Bull 27:777–780
Hay N, Sonenberg N (2004) Upstream and downstream of mTOR. Genes Dev 18:1926–1945. doi:10.1101/gad.1212704
Hershko A (2005) The ubiquitin system for protein degradation and some of its roles in the control of the cell division cycle. Cell Death Differ 12:1191–1197. doi:10.1038/sj.cdd.4401702
Hershko A, Ciechanover A (1992) The ubiquitin system for protein degradation. Annu Rev Biochem 61:761–807. doi:10.1146/annurev.bi.61.070192.003553
Hershko A, Ciechanover A (1998) The ubiquitin system. Annu Rev Biochem 67:425–479. doi:10.1146/annurev.biochem.67.1.425
Holloway JW, Barton SJ, Holgate ST, Rose-Zerilli MJ, Sayers I (2008) The role of LTA4H and ALOX5AP polymorphism in asthma and allergy susceptibility. Allergy 63:1046–1053. doi:10.1111/j.1398-9995.2008.01667.x
Hui K-S (2007) Brain-specific aminopeptidase: from enkephalinase to protector against neurodegeneration. Neurochem Res 32:2062–2071. doi:10.1007/s11064-007-9356-3
Ichinose Y, Genka K, Koike T, Kato H, Watanabe Y, Mori T, Iioka S, Sakuma A, Ohta M (2003) Randomized double-blind placebo-controlled trial of bestatin in patients with resected stage I squamous-cell lung carcinoma. J Natl Cancer Inst 95:605–610
Inokuma S, Setoguchi K, Ohta T, Matsuzaki Y, Yoshida A (1999) Serum leucine aminopeptidase as an activity indicator in systemic lupus erythematosus: a study of 46 consecutive cases. Rheumatology 38:705–708
Ishii K, Usui S, Sugimura Y, Yoshida S, Hioki T, Tatematsu M, Yamamoto H, Hirano K (2001) Aminopeptidase N regulated by zinc in human prostate participates in tumor cell invasion. Int J Cancer 92:49–54
Jeong C-H, Bode AM, Pugliese A, Cho Y-Y, Kim H-G, Shim J-H, Jeon Y-J, Li H, Jiang H, Dong Z (2009) [6]-Gingerol suppresses colon cancer growth by targeting leukotriene A4 hydrolase. Cancer Res 69:5584–5591. doi:10.1158/0008-5472.CAN-09-0491
Kakuta H, Tanatani A, Nagasawa K, Hashimoto Y (2003) Specific nonpeptide inhibitors of puromycin-sensitive aminopeptidase with a 2,4(1H,3H)-quinazolinedione skeleton. Chem Pharm Bull 51:1273–1282
Kamphausen E, Kellert C, Abbas T, Akkad N, Tenzer S, Pawelec G, Schild H, Van Endert P, Seliger B (2010) Distinct molecular mechanisms leading to deficient expression of ER-resident aminopeptidases in melanoma. Cancer Immunol Immunother 59:1273–1284. doi:10.1007/s00262-010-0856-7
Kehlen A, Lendeckel U, Dralle H (2003) Biological significance of aminopeptidase N/CD13 in thyroid carcinomas. Cancer Res 63:8500–8506
Kim E, Kwak H, Ahn K (2009) Cytosolic aminopeptidases influence MHC class I-mediated antigen presentation in an allele-dependent manner. J Immunol 183:7379–7387. doi:10.4049/jimmunol.0901489
Kisselev A, Akopian T, Goldberg A (1998) Range of sizes of peptide products generated during degradation of different proteins by archaeal proteasomes. J Biol Chem 273:1982–1989
Kisselev A, Akopian T, Woo K, AL G (1999) The sizes of peptides generated from protein by mammalian 26 and 20 S proteasomes. J Biol Chem 274:3363–3371
Krige D, Needham LA, Bawden LJ, Flores N, Farmer H, Miles LEC, Stone E, Callaghan J, Chandler S, Clark VL, Kirwin-Jones P, Legris V, Owen J, Patel T, Wood S, Box G, Laber D, Odedra R, Wright A, Wood LM, Eccles SA, Bone EA, Ayscough A, Drummond AH (2008) CHR-2797: an antiproliferative aminopeptidase inhibitor that leads to amino acid deprivation in human leukemic cells. Cancer Res 68:6669–6679. doi:10.1158/0008-5472.CAN-07-6627
Laplante M, Sabatini DM (2009) mTOR signaling at a glance. J Cell Sci 122:3589–3594. doi:10.1242/jcs.051011
Laplante M, Sabatini DM (2012) mTOR signaling in growth control and disease. Cell 149:274–293. doi:10.1016/j.cell.2012.03.017
Larsen SL, Pedersen LO, Buus S, Stryhn A (1996) T cell responses affected by aminopeptidase N (CD13)-mediated trimming of major histocompatibility complex class II-bound peptides. J Exp Med 184:183–189
Lecker SH, Goldberg AL, Mitch WE (2006) Protein degradation by the ubiquitin-proteasome pathway in normal and disease states. J Am Soc Nephrol 17:1807–1819. doi:10.1681/ASN.2006010083
Lee S (2009) Cobalt chloride-induced downregulation of puromycin-sensitive aminopeptidase suppresses the migration and invasion of PC-3 Cells. J Microbiol Biotechnol 19:530–536. doi:10.4014/jmb.0807.438
Lee P, Lin C, Liu C (2003) Acute leukemia with myeloid, B-, and natural killer cell differentiation. Arch Pathol Lab Med 127:93–95
Lee J, Song S, Seok J, Jha B, Han E, Song H-O, Yu H-S, Hong Y, Kong H-H, Chung D (2010) M17 leucine aminopeptidase of the human malaria parasite Plasmodium vivax. Mol Biochem Parasitol 170:45–48. doi:10.1016/j.molbiopara.2009.11.003
Löwenberg B, Morgan G, Ossenkoppele GJ, Burnett AK, Zachée P, Dührsen U, Dierickx D, Müller-Tidow C, Sonneveld P, Krug U, Bone E, Flores N, Richardson AF, Hooftman L, Jenkins C, Zweegman S, Davies F (2010) Phase I/II clinical study of tosedostat, an inhibitor of aminopeptidases, in patients with acute myeloid leukemia and myelodysplasia. J Clin Oncol 28:4333–4338. doi:10.1200/JCO.2009.27.6295
Lowther WT, Matthews BW (2002) Metalloaminopeptidases: common functional themes in disparate structural surroundings. Chem Rev 102:4581–4608
Luan Y, Ma C, Sui Z, Wang X, Feng J, Liu N, Jing F, Wang Y, Li M, Fang H, Xu W (2011) LYP3, a new bestatin derivative for aminopeptidase N inhibition. Med Chem 7:32–36
Martínez JM, Prieto I, Ramírez MJ, Cueva C, Alba F, Ramírez M (1999) Aminopeptidase activities in breast cancer tissue. Clin Chem 45:1797–1802
Matsushima M, Takahashi T, Ichinose M, Miki K, Kurokawa K, Takahashi K (1991) Structural and immunological evidence fort he identity of prolyl aminopeptidase with leucyl aminopeptidase. Biochem Biophys Res Cummun 178:1459–1464
Mehta A, Jordanova E, Corver W, Van Wezel T, Uh H, Kenter G, Fleuren GJ (2009) Single nucleotide polymorphisms in antigen processing machinery component ERAP1 significantly associate with clinical outcome in cervical carcinoma. Genes Chromosom Cancer 48:410–418. doi:10.1002/gcc
Menrad A, Speicher D, Wacker J, Herlyn M (1993) Biochemical and functional characterization of aminopeptidase N expressed by human melanoma cells. Cancer Res 53:1450–1455
Mina-Osorio P (2008) The moonlighting enzyme CD13: old and new functions to target. Trends Mol Med 14:361–371. doi:10.1016/j.molmed.2008.06.003
Moore HE, Davenport EL, Smith EM, Muralikrishnan S, Dunlop AS, Walker BA, Krige D, Drummond AH, Hooftman L, Morgan GJ, Davies FE (2009) Aminopeptidase inhibition as a targeted treatment strategy in myeloma. Mol Cancer Ther 8:762–770. doi:10.1158/1535-7163.MCT-08-0735
Nguyen TT, Chang S-C, Evnouchidou I, York IA, Zikos C, Rock KL, Goldberg AL, Stratikos E, Stern LJ (2011) Structural basis for antigenic peptide precursor processing by the endoplasmic reticulum aminopeptidase ERAP1. Nat Struct Mol Biol 18:604–613. doi:10.1038/nsmb.2021
Oi N, Jeong C-H, Nadas J, Cho Y-Y, Pugliese A, Bode AM, Dong Z (2010) Resveratrol, a red wine polyphenol, suppresses pancreatic cancer by inhibiting leukotriene ahydrolase. Cancer Res 70:9755–9764. doi:10.1158/0008-5472.CAN-10-2858
Pasqualini R, Koivunen E, Kain R (2000) Aminopeptidase N Is a receptor for tumor-homing peptides and a target for inhibiting angiogenesis. Cancer Res 60:722–727
Pei K-L, Yuan Y, Qin S-H, Wang Y, Zhou L, Zhang H-L, Qu X-J, Cui S-X (2012) CIP-13F, a novel aminopeptidase N (APN/CD13) inhibitor, inhibits Lewis lung carcinoma growth and metastasis in mice. Cancer Chemother Pharmacol 69:1029–1038. doi:10.1007/s00280-011-1799-1
Pérez I, Varona A, Blanco L, Gil J (2009) Increased APN/CD13 and acid aminopeptidase activities in head and neck squamous cell carcinoma. Head Neck 10:1335–1340. doi:10.1002/h
Peters GJ, Jansen G (2001) Antimetabolites. In: Souhami RL, Tannock I, Hohenberger P, Horiot JC (eds) Oxford textbook of oncology, vol 1, chapter 4.16, 2nd edn. Oxford University Press, Oxford, pp 663–713
Piedfer M, Dauzonne D, Tang R, N’Guyen J, Billard C, Bauvois B (2011) Aminopeptidase-N/CD13 is a potential proapoptotic target in human myeloid tumor cells. FASEB J 25:2831–2842. doi:10.1096/fj.11-181396
Pulido-Cejudo G, Conway B, Proulx P, Brown R, Izaguirre C (1997) Bestatin-mediated inhibition of leucine aminopeptidase may hinder HIV infection. Antiviral Res 36:167–177
Rackley RR, Yang B, Pretlow TG, Abdul-Karim FW, Lewis TJ, McNamara N, Delmoro CM, Bradley EL, Kursh E, Resnick MI (1991) Differences in the leucine aminopeptidase activity in extracts from human prostatic carcinoma and benign prostatic hyperplasia. Cancer 68:587–593
Radmark O, Shimizus T, Jornvall H, Samuelsson B (1984) Leukotriene A4 hydrolase in human leukocytes. Purification and properties. J Biol Chem 259:12339–12345
Rao M, Li Q, Feng L, Xia X, Ruan L, Sheng X, Ge M (2011) A new aminopeptidase inhibitor from streptomyces strain HCCB10043 found by UPLC-MS. Anal Bioanal Chem 401:699–706. doi:10.1007/s00216-011-5093-1
Reid AHM, Protheroe A, Attard G, Hayward N, Vidal L, Spicer J, Shaw HM, Bone EA, Carter J, Hooftman L, Harris A, De Bono JS (2009) A first-in-man phase I and pharmacokinetic study on CHR-2797 (Tosedostat), an inhibitor of M1 aminopeptidases, in patients with advanced solid tumors. Clin Cancer Res 15:4978–4985. doi:10.1158/1078-0432.CCR-09-0306
Reits E, Griekspoor A, Neijssen J, Groothuis T, Jalink K, Van Veelen P, Janssen H, Calafat J, Drijfhout JW, Neefjes J (2003) Peptide diffusion, protection, and degradation in nuclear and cytoplasmic compartments before antigen presentation by MHC class I. Immunity 18:97–108
Rock K, Goldberg A (1999) Degradation of cell proteins and the generation of MHC class I-presented peptides. Annu Rev Immunol 17:739–779. doi:10.1146/annurev.immunol.17.1.739
Rock K, York I, Goldberg A (2004) Post-proteasomal antigen processing for major histocompatibility complex class I presentation. Nat Immunol 5:670–677. doi:10.1038/ni1089
Rutenburg A, Goldbarg J, Pineda E (1958) Leucine aminopeptidase activity; observations in patients with cancer of the pancreas and other diseases. N Engl J Med 259:469–472
Sancak Y, Peterson TR, Shaul YD, Lindquist RA, Thoreen CC, Bar-Peled L, Sabatini DM (2008) The rag GTPases bind raptor and mediate amino acid signaling to mTORC1. Science 320(5882):1496–1501. doi:10.1126/science.1157535
Sanderink GJ, Artur Y, Siest G (1988) Human aminopeptidases: a review of the literature. J Clin Chem Clin Biochem 26:795–807
Santos A, Langner J, Herrmann M, Riemann D (2000) Aminopeptidase N/CD13 is directly linked to signal transduction pathways in monocytes. Cell Immunol 201:22–32. doi:10.1006/cimm.2000.1629
Saric T, Chang S-C, Hattori A, York IA, Markant S, Rock KL, Tsujimoto M, Goldberg AL (2002) An IFN-gamma-induced aminopeptidase in the ER, ERAP1, trims precursors to MHC class I-presented peptides. Nat Immunol 3:1169–1176. doi:10.1038/ni859
Saric T, Graef CI, Goldberg AL (2004) Pathway for degradation of peptides generated by proteasomes: a key role for thimet oligopeptidase and other metallopeptidases. J Biol Chem 279:46723–46732. doi:10.1074/jbc.M406537200
Sato Y (2004) Role of aminopeptidase in angiogenesis. Biol Pharm Bull 27:772–776
Saveanu L, Carroll O, Lindo V, Del Val M, Lopez D, Lepelletier Y, Greer F, Schomburg L, Fruci D, Niedermann G, Van Endert PM (2005) Concerted peptide trimming by human ERAP1 and ERAP2 aminopeptidase complexes in the endoplasmic reticulum. Nat Immunol 6:689–697. doi:10.1038/ni1208
Sawafuji K, Miyakawa Y, Weisberg E, Griffin JD, Ikeda Y, Kizaki M (2003) Aminopeptidase inhibitors inhibit proliferation and induce apoptosis of K562 and STI571-resistant K562 cell lines through the MAPK and GSK-3beta pathways. Leuk Lymphoma 44:1987–1996. doi:10.1080/1042819031000122033
Scornik O, Botbol V (2001) Bestatin as an experimental tool in mammals. Curr Drug Metab 2:67–85
Scott L, Lamb J, Smith S, Wheatley DN (2000) Single amino acid (arginine) deprivation: rapid and selective death of cultured transformed and malignant cells. Br J Cancer 83:800–810. doi:10.1054/bjoc.2000.1353
Sengupta S, Horowitz PM, Karsten SL, Jackson GR, Geschwind DH, Fu Y, Berry RW, Binder LI (2006) Degradation of tau protein by puromycin-sensitive aminopeptidase in vitro. Biochemistry 45:15111–15119. doi:10.1021/bi061830d
Serwold T, Gonzalez F, Kim J, Jacob R, Shastri N (2002) ERAAP customizes peptides for MHC class I molecules in the endoplasmic reticulum. Nature 419:480–483. doi:10.1038/nature01074
Stoltze L, Schirle M, Schwarz G, Schröter C, Thompson MW, Hersh LB, Kalbacher H, Stevanovic S, Rammensee HG, Schild H (2000) Two new proteases in the MHC class I processing pathway. Nat Immunol 1:413–818. doi:10.1038/80852
Su L, Cao J, Jia Y, Zhang X, Fang H, Xu W (2012a) Development of synthetic aminopeptidase N/CD13 inhibitors to overcome cancer metastasis and angiogenesis. ACS Med Chem Lett 3:959–964. doi:10.1021/ml3000758
Su L, Jia Y, Zhang L, Xu Y, Fang H, Xu W (2012b) Design, synthesis and biological evaluation of novel amino acid ureido derivatives as aminopeptidase N/CD13 inhibitors. Bioorg Med Chem 20:3807–3815. doi:10.1016/j.bmc.2012.04.035
Taylor A (1993) Aminopeptidases: structure and function. FASEB J 32:290–298
Tholander F, Muroya A, Roques B-P, Fournié-Zaluski M-C, Thunnissen MMGM, Haeggström JZ (2008) Structure-based dissection of the active site chemistry of leukotriene A4 hydrolase: implications for M1 aminopeptidases and inhibitor design. Chem Biol 15:920–929. doi:10.1016/j.chembiol.2008.07.018
Thunnissen M, Nordlund P, Haeggström JZ (2001) Crystal structure of human leukotriene A 4 hydrolase, a bifunctional enzyme in inflammation. Nat Struct Biol 8:131–135
Tobler A, Constam DB, Schmitt-Gräff A, Malipiero U, Schlapbach R, Fontana A (1997) Cloning of the human puromycin-sensitive aminopeptidase and evidence for expression in neurons. J Neurochem 68:889–897
Tokuhara T, Hattori N, Ishida H, Hirai T, Higashiyama M, Kodama K, Miyake M (2006) Clinical significance of aminopeptidase N in non-small cell lung cancer. Clin Cancer Res 12:3971–3978. doi:10.1158/1078-0432.CCR-06-0338
Towne C, York I, Neijssen J (2008) Puromycin-sensitive aminopeptidase limits MHC class I presentation in dendritic cells but does not affect CD8 T cell responses during viral infections. J Immunol 180:1704–1712
Tsukamoto H, Shibata K, Kajiyama H, Terauchi M, Nawa A, Kikkawa F (2008) Aminopeptidase N (APN)/CD13 inhibitor, Ubenimex, enhances radiation sensitivity in human cervical cancer. BMC Cancer 8:74. doi:10.1186/1471-2407-8-74
Umezawa H, Aoyagi T, Suda H (1976) Bestatin, an inhibitor of aminopeptidase B, produced by actinomycetes. J Antibiot XXIX:97–99
van Hensbergen Y, Broxterman H, Hanemaaijer R, Jorna AS, Van Lent NA, Verheul HM, Pinedo HM, Hoekman K (2002) Soluble aminopeptidase N/CD13 in malignant and nonmalignant effusions and intratumoral fluid. Clin Cancer Res 8:3747–3754
van Herpen CM, Eskens FA, De Jonge M, Desar I, Hooftman L, Bone EA, Timmer-Bonte JN, Verweij J (2010) A phase Ib dose-escalation study to evaluate safety and tolerability of the addition of the aminopeptidase inhibitor tosedostat (CHR-2797) to paclitaxel in patients with advanced solid tumours. Br J Cancer 103:1362–1368. doi:10.1038/sj.bjc.6605917
Varona A, Blanco L, López JI, Gil J, Agirregoitia E, Irazusta J, Larrinaga G (2007) Altered levels of acid, basic, and neutral peptidase activity and expression in human clear cell renal cell carcinoma. Am J Physiol Renal Physiol 292:F780–F788. doi:10.1152/ajprenal.00148.2006
Wakita A, Ohtake S, Takada S, Yagasaki F, Komatsu H, Miyazaki Y, Kubo K, Kimura Y, Takeshita A, Adachi Y, Kiyoi H, Yamaguchi T, Yoshida M, Ohnishi K, Miyawaki S, Naoe T, Ueda R, Ohno R (2012) Randomized comparison of fixed-schedule versus response-oriented individualized induction therapy and use of ubenimex during and after consolidation therapy for elderly patients with acute myeloid leukemia: the JALSG GML200 Study. Int J Hematol 96:84–93. doi:10.1007/s12185-012-1105-y
Watanabe Y, Shibata K, Kikkawa F (2003) Adipocyte-derived leucine aminopeptidase suppresses angiogenesis in human endometrial carcinoma via renin-angiotensin system. Clin Cancer Res 9:6497–6503
Wickström M, Larsson R, Nygren P, Gullbo J (2011) Aminopeptidase N (CD13) as a target for cancer chemotherapy. Cancer Sci 102:501–508. doi:10.1111/j.1349-7006.2010.01826.x
Willighagen R, Planteydt H (1959) Aminopeptidase activity in cancer cells. Nature 183:263–264
Xu Y, Lai LT, Gabrilove JL, Scheinberg DA (1998) Antitumor activity of actinonin in vitro and in vivo. Clin Cancer Res 4:171–176
Yamamoto Y, Li YH, Ushiyama I, Nishimura A, Ohkubo I, Nishi K (2000) Puromycin-sensitive alanyl aminopeptidase from human liver cytosol: purification and characterization. Forensic Sci Int 113:143–146
Yewdell J, Princiotta M (2004) Proteasomes get by with lots of help from their friends. Immunity 20:362–363
York IA, Chang S-C, Saric T, Keys JA, Favreau JM, Goldberg AL, Rock KL (2002) The ER aminopeptidase ERAP1 enhances or limits antigen presentation by trimming epitopes to 8–9 residues. Nat Immunol 3:1177–1184. doi:10.1038/ni860
Acknowledgments
This study was supported by grants CCA/VICI-07/36 to GJ, and CCA2012-1-08 to GJ, GO and GJP.
Conflict of interest
The authors do not have a conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hitzerd, S.M., Verbrugge, S.E., Ossenkoppele, G. et al. Positioning of aminopeptidase inhibitors in next generation cancer therapy. Amino Acids 46, 793–808 (2014). https://doi.org/10.1007/s00726-013-1648-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00726-013-1648-0