Abstract
High doses of glycine have been reported to improve negative schizophrenic symptoms, suggesting that ingested glycine activates glutamatergic transmission via N-methyl-d-aspartate (NMDA) receptors. However, the pharmacokinetics of administered glycine in the brain has not been evaluated. In the present study, the time- and dose-dependent distributions of administered glycine were investigated from a pharmacokinetic viewpoint. Whole-body autoradiography of radiolabeled glycine was performed, and time–concentration curves for glycine and serine in plasma, cerebrospinal fluid (CSF), and brain tissues were obtained. Furthermore, pharmacokinetic parameters were calculated. For a more detailed analysis, the amount of glycine uptake in the brain was evaluated using the brain uptake index method. Radiolabeled glycine was distributed among periventricular organs in the brain. Oral administration of 2 g/kg of glycine significantly elevated the CSF glycine concentration above the ED50 value for NMDA receptors. The glycine levels in CSF were 100 times lower than those in plasma. Glycine levels were elevated in brain tissue, but with a slower time-course than in CSF. Serine, a major metabolite of glycine, was elevated in plasma, CSF, and brain tissue. Glycine uptake in brain tissue increased in a dose-dependent manner. Time–concentration curves revealed that glycine was most likely transported via the blood–CSF barrier and activated NMDA receptors adjacent to the ventricles. The pharmacokinetic analysis and the brain uptake index for glycine suggested that glycine was transported into brain tissue by passive diffusion. These results provide further insight into the potential therapeutic applications of glycine.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
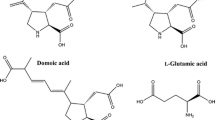
Glycine, a non-essential amino acid, plays a vital role in inhibitory and excitatory neurotransmission via the strychnine-sensitive glycine receptor and the N-methyl-d-aspartate (NMDA) receptor, respectively (Johnson and Ascher 1987; D’Souza et al. 1995). Glycine receptors and NMDA receptors are located at pre- and post-synaptic terminals, and their ED50 values for glycine are 90–100 μM and 100–300 nM, respectively (D’Souza et al. 1995).
The level of extracellular glycine in the brain is strictly regulated by the Na+/Cl−-dependent glycine transporters GlyT1 and GlyT2, which are expressed on glial cells and neurons, respectively (Betz et al. 2006; Zafra and Gimenez 2008). Extracellular glycine is recycled by reuptake into neurons (Gomeza et al. 2003), metabolized to carbon dioxide and ammonia by glycine cleavage enzymes in glial cells, or converted to l-serine by serine hydroxymethyltransferase (SHMT) in glial cells (Verleysdonk et al. 1999; dos Santos Fagundes et al. 2001). l-serine is converted to pyruvate and used as an energy source in the tricarboxylic acid cycle (Xue et al. 1999a, b).
Large doses of glycine (40–90 g/day) have beneficial effects on the negative symptoms of schizophrenia in humans (Tsai et al. 1998, 2004; Heresco-Levy et al. 1999). We recently reported that glycine ingestion before bedtime significantly improves subjective sleep quality among people with insomniac tendencies (Inagawa et al. 2006; Yamadera et al. 2007). Additionally, orally administered glycine has been shown to cross the blood–brain barrier (BBB) and accumulate in the cerebrospinal fluid (CSF) in rodents and humans (Richter and Wainer 1971; Toth and Lajtha 1981, 1986). These reports indicate that orally administered glycine may affect brain function. However, the evidence is inconclusive, and therefore, the pharmacokinetic characteristics and the mechanisms of glycine uptake in the brain remain unclear. To better understand the potential therapeutic applications of glycine, especially in the brain, the pharmacokinetic characteristics of externally administered glycine were investigated, including its distribution, its concentration–time curves, and its uptake by the brain. This study was carried out in three steps. First, we determined the distribution of administered glycine using autoradiographic imaging. Then, we measured the concentrations of glycine and serine in plasma, CSF, and cortex for 24 h following glycine administration. Finally, the brain uptake of glycine was calculated following the administration of radiolabeled glycine.
Methods
Animals
In total, 113 male Wistar rats (2 rats for experiment 1 and 111 rats for experiment 2) and 12 Sprague–Dawley rats (for experiment 3) weighing 250 g were purchased from Charles River Japan, Inc. (Yokohama, Japan). The animals were housed individually in plastic cages and allowed food and water ad libitum. The animal room was maintained at constant temperature (23 ± 3°C) and humidity (55 ± 20%) with a 12-h light–dark cycle (lights were on from 0700 hours to 1900 hours). All experimental procedures were reviewed and approved by the Animal Care Committee of Ajinomoto Co., Inc., and every effort was made to minimize both the number of animals used and their discomfort.
Experiment 1: in vivo whole-body autoradiography with 14C-glycine
To examine the tissue distribution of administered glycine, [2-14C]-glycine (American Radiolabeled Chemicals Inc., 2.04 GBq/mmol) was dissolved in saline, and a final concentration of 7.3 MBq/2.4 mL/kg (3.6 μmol/kg) was injected into the tail veins of rats anesthetized with diethyl ether. Two rats were killed 6 min after injection while still under anesthesia, and their entire bodies were frozen in liquid nitrogen. Most of the injected glycine was neither metabolized nor eliminated within 6 min. Twenty micron-thick sagittal cryosections of the whole body were prepared using a microtome (CRYOMACROCUT, Leica, Nussloch, Germany) and gently freeze-dried under vacuum conditions for 1 week. After lyophilization, the cryosections were exposed to X-ray film for 3 weeks at room temperature, and the film was developed to visualize the signal from the radioactive glycine. Whole-body bright-field images and autoradiograms were obtained by scanning the sections and X-ray films with an Imagio Neo 601 (Ricoh, Tokyo, Japan).
Experiment 2: amino acid analysis
Rats received 2 g/kg of glycine (Ajinomoto Co. Inc., Tokyo, Japan) or water as a vehicle control administered by gavage after 24 h of fasting. Blood, CSF and cortex samples were collected 0, 0.0833, 0.25, 0.5, 1, 2, 4, 8, 12, 16 and 24 h after the oral administration of glycine. Each recorded time point represents data from 4 to 6 rats. Blood was collected from the abdominal aorta under ether anesthesia. EDTA was used as an anticoagulant, and plasma was obtained from the blood samples by centrifugation. After blood sampling, a cannula was inserted into the cisterna magna, and 100 μL of CSF was collected. After CSF sampling, the whole brain was immediately isolated, and the cerebral cortex was removed. Blood, CSF and cortex were collected from each rat within 2 min.
Amino acid concentrations in the CSF, plasma and cerebral cortex were measured using a previously published protocol (Noguchi et al. 2006). Briefly, amino acids were separated by cation-exchange chromatography and detected spectrophotometrically after post-column reaction with a ninhydrin reagent.
Experiment 3: study of in vivo brain uptake of 3H-glycine
In vivo glycine transportation across the BBB was evaluated after glycine injection into the carotid artery, as reported previously (Oldendorf 1970; Moriki et al. 2004). [2-3H]-glycine (37 MBq/mL) was purchased from PerkinElmer (Waltham, MA, USA), and carboxyl-14C-inulin (3.7 MBq/mL) was purchased from American Radiolabeled Chemicals Inc. (St. Louis, MO, USA). Inulin was used as a reference because of its high molecular weight and inability to cross the BBB. The final concentrations of total glycine were 0.67 nmol/kg, 50 nmol/kg, 2.5 μmol/kg and 2.5 mmol/kg, and each solution contained 1.5 MBq/kg of radioactive glycine and 0.25 MBq/kg (0.67 nmol/kg) of radioactive inulin. Each dose was given to three rats. While the rats were under ether anesthesia, 1 mL/kg body weight of the injection solution was administered into the left carotid artery. Twenty seconds after the injection, which is enough to circulate glycine to whole body, blood samples were collected from the abdominal aorta and then the brain was collected.
Whole blood samples were divided into two tubes, i.e., one was for whole blood analysis and the other was for plasma analysis. 20 µL of whole blood and 2 mL of tissue solubilizer (Lumasolve, Lumac LSC, Belgium) were added to a scintillation vial. This solution was incubated at 50°C, and 0.5 mL of isopropanol and 1 mL of 30% of H2O2 were added. Plasma was obtained from the other blood tube, and 1 mL of tissue solubilizer was added to each 20 μL plasma sample. The brain was divided into separate brain regions (the tissue weights for the cerebral cortex, thalamus, cerebellum, midbrain, and medulla were 76.3 ± 4.9, 58.1 ± 4.9, 50.8 ± 2.2, 64.7 ± 6.7 and 62.5 ± 5.3 mg, respectively) and dissolved in 5 mL of 2 M NaOH. Ten to sixteen milliliters of scintillation fluid (LUMASAFE, Lumac LSC, Belgium) was added to each sample to measure radioactivity using a scintillation counter (2750TR/LL, PACKARD, Meriden, CT, USA).
The uptake amount and brain uptake index (BUI) of glycine were calculated using the method reported by Oldendorf (Oldendorf 1970; Moriki et al. 2004), as described below. Formula 1 describes the concentration of distributed glycine in blood, and formula 2 describes its concentration in tissue. The weight of blood containing in the brain tissue was calculated by formula 3. The uptake amount of glycine in tissue (mol/g; Uptakegly,tissue) was calculated by subtracting the glycine amount in blood from that in tissue. BUI was calculated using formula 5.
The terms in the above equations are defined as follows: LSC3H-Gly,blood, 3H radioactivity in blood (dpm); LSC3H-Gly,tissue, 3H radioactivity in brain tissue (dpm); LSC14C-Inulin,blood, 14C radioactivity in blood (dpm); LSC14C-Inulin,tissue, 14C radioactivity in brain tissue; weightblood, weight of blood sample; weigthttissue, weight of brain tissue; weightblood,tissue, weight of blood containing in the brain tissue; radioactivity3H-Gly, radioactivity of injected 3H glycine.
Statistical analysis
The data are presented as mean values ± SEM. Changes in the amino acid levels in plasma and CSF were analyzed using two-way analysis of variance (ANOVA) followed by the Holm-Sidak test using SigmaPlot version 11.2 (Systat Software Inc., Richmond, CA, USA). The pharmacokinetic parameters of glycine and serine were calculated from the concentration–time curves plotted for the plasma, CSF and cortex using non-compartmental analysis with WinNonlin 6.0.0 (Pharsight Corporation, Mountain View, CA, USA).
Results
Experiment 1: in vivo whole-body autoradiography of 14C-glycine
Two rats were used for autoradiography, and both showed the same distribution of glycine. Figure 1a shows whole-body autoradiographs made 6 min after intravenous injection of 14C-glycine. Localized high autoradiographic density was observed in both the liver and the pancreas. In the brain, high density was detected in the fourth ventricle, the circumventricular zone, the pineal gland and the pituitary gland (Fig. 1c).
X-ray images of 14C-glycine in whole-body and brain sections are presented in a and c, respectively. Bright-field images of the same sections are shown in b and d. The autoradiograms show a high density of 14C-glycine in the liver, pancreas (a, arrowhead), pineal gland, pituitary gland, subfornical organ, and fourth ventricle (c, arrowhead)
Experiment 2: amino acid analysis
Concentration–time curves were generated for glycine in plasma and CSF following oral administration (2 g/kg of glycine). At 0.5 h (T max), glycine in plasma reached its maximum concentration of 5,371 ± 507 μmol/L (C max), which is 13-fold higher than the level in vehicle controls (410 ± 21 μmol/L; Fig. 2a). In CSF, T max was again 0.5 h, and C max was 52.7 ± 4.4 μmol/L, which is sixfold higher than the level in the vehicle controls (8.8 ± 0.7 μmol/L; Fig. 2b). Glycine levels returned to baseline 24 h after its administration. The glycine levels in the cerebral cortex were also examined (Fig. 2c). In this region, glycine concentrations reached T max at 4 h, and C max was 1,376 ± 30 pmol/mg wet tissue, which is twofold higher than that observed in the vehicle controls (676 ± 40 pmol/mg wet tissue). Two-way ANOVA revealed significant differences between the glycine and vehicle groups [F group(1,110) = 258.172, P < 0.001 in plasma; F group(1,105) = 143.786, P < 0.001 in CSF; F group(1,104) = 49.224, P < 0.001 in the cortex].
Concentration–time curves of glycine in plasma (a), CSF (b), and the cerebral cortex (c) following oral administration of vehicle (empty circles) or 2 g/kg of glycine (filled circles). Each symbol represents the mean ± SEM (N = 4–6). Asterisks indicate a statistical difference between the vehicle-treated group and the glycine-treated group at a given time point (P < 0.01)
A concentration–time curve was also generated for serine. The T max of the serine concentration in plasma was 2 h, and the C max was 497 ± 58 μmol/L, which is 1.9-fold higher than the level in the vehicle controls (267 ± 4.8 μmol/L; Fig. 3a). In the CSF, T max was 8 h, and C max was 136.7 ± 0.8 μmol/L, which is twofold higher than the level in the vehicle controls (66.9 ± 3.3 μmol/L; Fig. 3b). Serine levels returned to baseline 24 h after glycine administration. In the cerebral cortex, T max was 8 h, and C max was 1,521 ± 16 pmol/mg wet tissue, which is 1.5-fold higher than the level in the vehicle controls (1,052 ± 22 pmol/mg of wet tissue; Fig. 3c). Two-way ANOVA showed significant differences between the groups [F group(1,110) = 182.280, P < 0.001 in plasma; F group(1,105) = 178.835, P < 0.001 in CSF; F group(1,104) = 20.245, P < 0.001 in the cortex].
Concentration–time curves of serine in plasma (a), CSF (b), and the cerebral cortex (c) following oral administration of vehicle (empty circles) or 2 g/kg of glycine (filled circles). Each symbol represents the mean ± SEM (N = 4–6). Asterisks indicate a statistical difference between the vehicle-treated group and the glycine-treated group at a given time point (P < 0.01)
Table 1 shows the difference between the peak and baseline concentrations (ΔC max), T max, the difference in the area under the curve (ΔAUC), and the pharmacokinetic distribution parameters (T-lag, T 1/2, MRT, VRT, CLtot, and V dss) obtained by subtracting the values obtained for the glycine administration group from those determined for the vehicle administration group using non-compartmental analysis. In plasma, the ΔC max of serine was approximately 1/21 that of glycine, whereas in the CSF and cortex, the ΔC max values for serine were about 1.75 times and 0.67 times those of glycine, respectively. ΔAUC exhibited the same pattern as ΔC max. The T max of serine occurred later than that of glycine in plasma, CSF and cortex.
Experiment 3: brain uptake of 3H-glycine in vivo
Glycine uptake in the brain varied with respect to the injected quantity of glycine (Fig. 4). Figure 5 shows the BUI values of glycine (from this study) and other amino acids (Pardridge and Oldendorf 1975) at several different concentrations. As shown in the figure, the BUI of glycine were stable in the injection concentration range, whereas those of the other amino acids in the figure were decreased dose-dependently.
Brain uptake indices (BUIs) of glycine and other amino acids as reported by Pardridge and Oldendorf (1975). BUI of glycine was calculated from the results of experiment 3. Each symbol represents the mean ± SEM (N = 3–6)
Discussion
Glycine has been recently utilized as an activator of the NMDA receptor, especially in schizophrenic patients. The therapeutic administration of glycine to patients has been explored since the 1990s; however, the distribution of externally administered glycine and its metabolites in various organs and body fluids has remained unclear. In the present study, we followed the fate of administered glycine in rats to evaluate its pharmacokinetic characteristics, including distribution, uptake into brain tissues, BUI for glycine, and the time–concentration curves of both glycine and its metabolite, serine.
Glycine transport to the brain
Detailed concentration–time curves for orally administered glycine were obtained (Fig. 2). Glycine concentrations were found to increase in plasma, CSF and cortex. It has previously been reported that 0.2 g/kg of intravenous glycine infused over 45 min in humans increases the plasma glycine concentration to 5,093 ± 823 μmol/L, which is 20-fold greater than the baseline concentration. CSF was collected 135 min after injection, and the glycine level in the CSF was 21.2 ± 6.989 μmol/L, which is fourfold greater than the baseline concentration (D’Souza et al. 2000). Glycine levels increased more rapidly in plasma than in CSF in both the human infusion study and our study.
In our experiments, glycine levels increased more slowly in cortex than in plasma or CSF, potentially indicating the presence of distinct delivery mechanisms at the blood–CSF barrier (BCB) and the BBB. T max was 4 h in the cortex, whereas T max was 30 min in both plasma and CSF. These results suggest that glycine transport occurs much more quickly across the BCB than across the BBB (Table 1). Both the BCB and the BBB consist of tight junctions between epithelial cells in the choroid plexus and endothelial cells (Saunders et al. 1999), and a carrier for glycine may exist in the choroid plexus (Preston et al. 1989). Thus, it is possible that glycine is primarily transported into the CSF from the blood via the BCB and passively diffuses into the brain parenchyma from the CSF and/or directly crosses the BBB. Glycine was not detected in brain tissue 6 min after radiolabeled glycine injection; however, glycine was detected in the fourth ventricle at this time point (Fig. 1c). Moreover, as shown in Fig. 2, the glycine concentration in the cortex was not elevated at this time. These results indicate that a detectable amount of glycine reaches the CSF, but not the brain tissue, 6 min after injection.
Glycine uptake into the brain increased in a dose-dependent manner (Fig. 4), maintaining a BUI between 2.6 and 9.0% (Fig. 5). This value is consistent with previous reports using a dose of 15 nmol/kg (Oldendorf 1971; Pardridge and Oldendorf 1975). The BUIs of other amino acids such as phenylalanine, leucine, tyrosine, and methionine, that are transported by specific transporters (Uchino et al. 2002), have been shown to decrease dose-dependently (Fig. 5; (Pardridge and Oldendorf 1975). If glycine is transported by a specific transporter, the highest dose would saturate the transporter at V max, resulting in a lower BUI. However, we found a linear relationship between the injected and detected glycine levels in the injection concentration range from 0.67 nmol/kg to 2.5 mmol/kg. Thus, the BUI data suggest that glycine passively diffuses across the BBB by means of nonspecific transport at the concentrations tested.
Metabolism
Oral administration of glycine elevated serine levels in the plasma, CSF, and cerebral cortex (Fig. 3). l-Serine and glycine can be interconverted by SHMT (Verleysdonk et al. 1999). In this study, the T max values for serine in plasma, CSF and cortex were 2, 8 and 8 h, respectively, whereas those of glycine were 0.5, 0.5 and 4 h, respectively. Although the concentrations of l-serine and d-serine were not determined individually by our method, the time courses indicated an enzymatic reaction biased toward l-serine production, which might last for several hours after oral administration of glycine. To assess the conversion rate, pharmacokinetic parameters including ΔAUC and T 1/2 were calculated (Table 1). The ΔAUC of glycine can be used as an index of glycine uptake, and the ΔAUC of serine can be used as an index of the conversion of glycine to l-serine. In plasma, the glycine ΔAUC was greater than the serine ΔAUC, which suggests two possibilities. The first possibility is that plasma glycine was partially converted to l-serine, and the remainder was taken up into tissues or metabolized by a system other than SHMT, such as the glycine cleavage system (GCS). The other possibility is that this imbalance is due to the elimination of serine, which occurs faster than that of glycine and is limited by the rate of serine formation. Consistent with this hypothesis, the T 1/2 of serine and glycine were dissimilar. By contrast, the difference between the glycine and serine ΔAUC values was virtually zero in the cortex, suggesting that most of the glycine was converted to l-serine by SHMT. Glycine in the brain is thought to be metabolized by both SHMT and GCS (Petzke et al. 1986; Lamers et al. 2007). Our results suggest that SHMT is dominant in the cortex. Unlike glycine metabolism by GCS, metabolism by SHMT does not lead to the production of toxic ammonia (Bachmann et al. 2004). Moreover, the T 1/2 of serine in CSF was shorter than that of glycine, suggesting that l-serine is easily metabolized or discharged into plasma.
Putative mechanism for the activity of glycine against negative symptoms of schizophrenia
The pathology of schizophrenia has been attributed to NMDA receptor malfunction (Javitt and Zukin 1991; Tsai and Coyle 2002; Lin et al. 2011; Gilmour et al. 2011). Continuous administration of a large amount of glycine or d-serine has been reported to improve negative schizophrenic symptoms (Javitt et al. 1994; Tsai et al. 1998; Tuominen et al. 2005). The ED50 of glycine for the glycine receptor and the NMDA receptor is 90–100 μM and 100–300 nM, respectively (D’Souza et al. 1995). In this study, the glycine levels after administration were higher than the ED50 of NMDA receptors and lower than the ED50 of glycine receptors. Furthermore, the concentration of d-serine in the neocortex has been shown to increase following the administration of glycine (Takahashi et al. 1997), suggesting that the elevated glycine concentration in the CSF may activate neurotransmission via NMDA receptors. Because the baseline glycine levels in CSF are higher than the ED50 of NMDA receptors, NMDA receptors might be activated by endogenous glycine. When the glycine levels in CSF are higher than baseline, the probability of glycine binding to NMDA receptors should increase, resulting in the activation of NMDA receptors.
Improved sleep following glycine ingestion
We recently reported that the ingestion of 3 g of glycine before bedtime significantly improves subjective sleep quality among individuals with insomniac tendencies (Inagawa et al. 2006; Yamadera et al. 2007), suggesting that a transient elevation in glycine levels in plasma and CSF can affect the sleep–wake cycle. Oral administration of glycine increases prefrontal serotonin levels (Bannai et al. 2011). Systemic injection of the NMDA receptor antagonist NPC12626 during the light period has been shown to prevent sleep (Stone et al. 1992), and in the basal forebrain, perfusion of NMDA via microdialysis probes has been shown to increase the sleep-associated elevation of extracellular adenosine in rats (Wigren et al. 2007; Bannai et al. 2011). Furthermore, intracerebroventricular injections of quinolinic acid, an endogenous ligand of the NMDA receptor, increases deep slow-wave sleep (dSWS) in rabbits (Milasius et al. 1990). Based on these reports and the data from this study, we hypothesize that the NMDA receptor is the primary target of glycine, which mediates these effects on sleep.
In contrast, previous studies have demonstrated that oral administration of riluzole, which inhibits the release of glutamate and antagonizes ionotropic glutamate receptors, increases slow-wave sleep in rats in a dose-dependent manner (Stutzmann et al. 1988) and thalamic injection of dl-2-amino-5-phosphonopentanoic acid (APV), an NMDA receptor antagonist, increases dSWS and paradoxical sleep in cats (Juhasz et al. 1990). Moreover, NMDA injection into the basal forebrain has been shown to increase wakefulness (Cape and Jones 2000). However, there have been no reports demonstrating that glycine alone has insomniac effects. The effect of glycine on sleep remains unclear, and the region-specific contributions of glycine to the sleep–wake cycle through NMDA receptors require further investigation.
In conclusion, the present study characterized the pharmacokinetic profile of orally administered glycine and its potential effects on NMDA receptor activation. Although the BBB strictly limited amino acid transport into the brain, glycine was taken up into brain tissue in a dose-dependent manner by passive diffusion, and long-lasting elevated glycine concentrations were observed in the CSF and cortex, suggesting potential effects of externally administered glycine.
References
Bachmann C, Braissant O, Villard AM, Boulat O, Henry H (2004) Ammonia toxicity to the brain and creatine. Mol Genet Metab 81 Suppl 1:S52–S57. doi:10.1016/j.ymgme.2003.10.014
Bannai M, Kawai N, Nagao K, Nakano S, Matsuzawa D, Shimizu E (2011) Oral administration of glycine increases extracellular serotonin but not dopamine in the prefrontal cortex of rats. Psychiatry Clin Neurosci 65(2):142–149. doi:10.1111/j.1440-1819.2010.02181.x
Betz H, Gomeza J, Armsen W, Scholze P, Eulenburg V (2006) Glycine transporters: essential regulators of synaptic transmission. Biochem Soc Trans 34(Pt 1):55–58. doi:10.1042/BST0340055
Cape EG, Jones BE (2000) Effects of glutamate agonist versus procaine microinjections into the basal forebrain cholinergic cell area upon gamma and theta EEG activity and sleep–wake state. Eur J Neurosci 12(6):2166–2184. pii:ejn099
dos Santos Fagundes I, Rotta LN, Schweigert ID, Valle SC, de Oliveira KR, Huth Kruger A, Souza KB, Souza DO, Perr ML (2001) Glycine, serine, and leucine metabolism in different regions of rat central nervous system. Neurochem Res 26(3):245–249
D’Souza DC, Charney DS, Krystal JH (1995) Glycine site agonists of the NMDA receptor: a review. CNS Drug Rev 1(2):227–260. doi:10.1111/j.1527-3458.1995.tb00285.x
D’Souza DC, Gil R, Cassello K, Morrissey K, Abi-Saab D, White J, Sturwold R, Bennett A, Karper LP, Zuzarte E, Charney DS, Krystal JH (2000) IV glycine and oral d-cycloserine effects on plasma and CSF amino acids in healthy humans. Biol Psychiatry 47(5):450–462. pii:S0006-3223(99)00133-X
Gilmour G, Dix S, Fellini L, Gastambide F, Plath N, Steckler T, Talpos J, Tricklebank M (2011) NMDA receptors, cognition and schizophrenia—testing the validity of the NMDA receptor hypofunction hypothesis. Neuropharmacology. doi:10.1016/j.neuropharm.2011.03.015
Gomeza J, Hulsmann S, Ohno K, Eulenburg V, Szoke K, Richter D, Betz H (2003) Inactivation of the glycine transporter 1 gene discloses vital role of glial glycine uptake in glycinergic inhibition. Neuron 40(4):785–796
Heresco-Levy U, Javitt DC, Ermilov M, Mordel C, Silipo G, Lichtenstein M (1999) Efficacy of high-dose glycine in the treatment of enduring negative symptoms of schizophrenia. Arch Gen Psychiatry 56(1):29–36. doi:10.1001/archpsyc.56.1.29
Inagawa K, Hiraoka T, Kohda T, Yamadera W, Takahashi M (2006) Subjective effects of glycine ingestion before bedtime on sleep quality. Sleep and Biological Rhythms 4:75–77. doi:10.1111/j.1479-8425.2006.00193.x
Javitt DC, Zukin SR (1991) Recent advances in the phencyclidine model of schizophrenia. Am J Psychiatry 148(10):1301–1308
Javitt DC, Zylberman I, Zukin SR, Heresco-Levy U, Lindenmayer JP (1994) Amelioration of negative symptoms in schizophrenia by glycine. Am J Psychiatry 151(8):1234–1236
Johnson JW, Ascher P (1987) Glycine potentiates the NMDA response in cultured mouse brain neurons. Nature 325(6104):529–531. doi:10.1038/325529a0
Juhasz G, Kekesi K, Emri Z, Soltesz I, Crunelli V (1990) Sleep-promoting action of excitatory amino acid antagonists: a different role for thalamic NMDA and non-NMDA receptors. Neurosci Lett 114(3):333–338
Lamers Y, Williamson J, Gilbert LR, Stacpoole PW, Gregory JF 3rd (2007) Glycine turnover and decarboxylation rate quantified in healthy men and women using primed, constant infusions of [1, 2-(13)C2]glycine and [(2)H3]leucine. J Nutr 137(12):2647–2652. pii:137/12/2647
Lin CH, Lane HY, Tsai GE (2011) Glutamate signaling in the pathophysiology and therapy of schizophrenia. Pharmacol Biochem Behav. doi:10.1016/j.pbb.2011.03.023
Milasius AM, Grinevicius KK, Lapin IP (1990) Effect of quinolinic acid on wakefulness and sleep in the rabbit. J Neural Transm Gen Sect 82(1):67–73
Moriki Y, Suzuki T, Fukami T, Hanano M, Tomono K, Watanabe J (2004) Involvement of P-glycoprotein in blood–brain barrier transport of pentazocine in rats using brain uptake index method. Biol Pharm Bull 27(6):932–935. doi:10.1248/bpb.27.932
Noguchi Y, Zhang QW, Sugimoto T, Furuhata Y, Sakai R, Mori M, Takahashi M, Kimura T (2006) Network analysis of plasma and tissue amino acids and the generation of an amino index for potential diagnostic use. Am J Clin Nutr 83(2):513S–519S. pii:83/2/513S
Oldendorf WH (1970) Measurement of brain uptake of radiolabeled substances using a tritiated water internal standard. Brain Res 24(2):372–376. pii:0006-8993(70)90123-X
Oldendorf WH (1971) Brain uptake of radiolabeled amino acids, amines, and hexoses after arterial injection. Am J Physiol 221(6):1629–1639
Pardridge WM, Oldendorf WH (1975) Kinetic analysis of blood–brain barrier transport of amino acids. Biochim Biophys Acta 401(1):128–136. pii:0005-2736(75)90347-8
Petzke KJ, Albrecht V, Przybilski H (1986) The influence of high glycine diets on the activity of glycine-catabolizing enzymes and on glycine catabolism in rats. J Nutr 116(5):742–750
Preston JE, Segal MB, Walley GJ, Zlokovic BV (1989) Neutral amino acid uptake by the isolated perfused sheep choroid plexus. J Physiol 408:31–43
Richter JJ, Wainer A (1971) Evidence for separate systems for the transport of neutral and basic amino acids across the blood–brain barrier. J Neurochem 18(4):613–620
Saunders NR, Habgood MD, Dziegielewska KM (1999) Barrier mechanisms in the brain, I. Adult brain. Clin Exp Pharmacol Physiol 26(1):11–19
Stone WS, Walker DL, Gold PE (1992) Sleep deficits in rats after NMDA receptor blockade. Physiol Behav 52(3):609–612. pii:0031-9384(92)90355-6
Stutzmann JM, Lucas M, Blanchard JC, Laduron PM (1988) Riluzole, a glutamate antagonist, enhances slow wave and REM sleep in rats. Neurosci Lett 88(2):195–200
Takahashi K, Hayashi F, Nishikawa T (1997) In vivo evidence for the link between L- and D-serine metabolism in rat cerebral cortex. J Neurochem 69(3):1286–1290
Toth E, Lajtha A (1981) Elevation of cerebral levels of nonessential amino acids in vivo by administration of large doses. Neurochem Res 6(12):1309–1317
Toth E, Lajtha A (1986) Antagonism of phencyclidine-induced hyperactivity by glycine in mice. Neurochem Res 11(3):393–400
Tsai G, Coyle JT (2002) Glutamatergic mechanisms in schizophrenia. Annu Rev Pharmacol Toxicol 42:165–179. doi:10.1146/annurev.pharmtox.42.082701.160735
Tsai G, Yang P, Chung LC, Lange N, Coyle JT (1998) d-serine added to antipsychotics for the treatment of schizophrenia. Biol Psychiatry 44(11):1081–1089. pii:S0006-3223(98)00279-0
Tsai G, Lane HY, Yang P, Chong MY, Lange N (2004) Glycine transporter I inhibitor, N-methylglycine (sarcosine), added to antipsychotics for the treatment of schizophrenia. Biol Psychiatry 55(5):452–456. doi:10.1016/j.biopsych.2003.09.012
Tuominen HJ, Tiihonen J, Wahlbeck K (2005) Glutamatergic drugs for schizophrenia: a systematic review and meta-analysis. Schizophr Res 72(2–3):225–234. doi:10.1016/j.schres.2004.05.005
Uchino H, Kanai Y, Kim DK, Wempe MF, Chairoungdua A, Morimoto E, Anders MW, Endou H (2002) Transport of amino acid-related compounds mediated by L-type amino acid transporter 1 (LAT1): insights into the mechanisms of substrate recognition. Mol Pharmacol 61(4):729–737
Verleysdonk S, Martin H, Willker W, Leibfritz D, Hamprecht B (1999) Rapid uptake and degradation of glycine by astroglial cells in culture: synthesis and release of serine and lactate. Glia 27(3):239–248. doi:10.1002/(SICI)1098-1136(199909)27:3<239:AID-GLIA5>3.0.CO;2-K
Wigren HK, Schepens M, Matto V, Stenberg D, Porkka-Heiskanen T (2007) Glutamatergic stimulation of the basal forebrain elevates extracellular adenosine and increases the subsequent sleep. Neuroscience 147(3):811–823. doi:10.1016/j.neuroscience.2007.04.046
Xue HH, Fujie M, Sakaguchi T, Oda T, Ogawa H, Kneer NM, Lardy HA, Ichiyama A (1999a) Flux of the l-serine metabolism in rat liver. The predominant contribution of serine dehydratase. J Biol Chem 274(23):16020–16027. doi:10.1074/jbc.274.23.16020
Xue HH, Sakaguchi T, Fujie M, Ogawa H, Ichiyama A (1999b) Flux of the l-serine metabolism in rabbit, human, and dog livers. Substantial contributions of both mitochondrial and peroxisomal serine:pyruvate/alanine:glyoxylate aminotransferase. J Biol Chem 274 (23):16028–16033. doi:10.1074/jbc.274.23.16028
Yamadera W, Inagawa K, Chiba S, Bannai M, Takahashi M, Namagawa K (2007) Glycine ingestion improves subjective sleep quality in human volunteers, correlating with polysomnographic changes. Sleep Biol Rhythms 5:126–131. doi:10.1111/j.1479-8425.2007.00262.x
Zafra F, Gimenez C (2008) Glycine transporters and synaptic function. IUBMB Life 60(12):810–817. doi:10.1002/iub.128
Acknowledgments
The authors express their gratitude to Drs. Y. Urade and Z. Huang from Osaka Bioscience Institute for their valuable input.
Conflict of interest
Nobuhiro Kawai, Makoto Bannai, Shinobu Seki, Kenji Nagao and Michio Takahashi are employees of Ajinomoto Co., Inc. Tomonori Koizumi and Kenji Shinkai are employees of Ajinomoto Pharmaceuticals Co., Ltd.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kawai, N., Bannai, M., Seki, S. et al. Pharmacokinetics and cerebral distribution of glycine administered to rats. Amino Acids 42, 2129–2137 (2012). https://doi.org/10.1007/s00726-011-0950-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00726-011-0950-y