Abstract
Sulfur amino acids (SAA), particularly methionine and cysteine, are critical for the gut to maintain its functions including the digestion, absorption and metabolism of nutrients, the immune surveillance of the intestinal epithelial layer and regulation of the mucosal response to foreign antigens. However, the metabolism of SAA in the gut, specifically the transmethylation of methionine, will result in a net release of homocysteine, which is shown to be associated with cardiovascular disease and stroke. Furthermore, the extensive catabolism of dietary methionine by the intestine or by luminal microbes may result in a decrease in nutritional efficiency. Therefore, the regulation of SAA metabolism in the gut is not only nutritionally relevant, but also relevant to the overall health and well-being. The superiority of dl-2-hydroxy-4-methylthiobutyrate to dl-methionine in decreasing homocysteine production, alleviating stress responses, and reducing the first-pass intestinal metabolism of dietary methionine may provide a promising implication for nutritional strategies to manipulate SAA metabolism and thus to improve the nutrition and health status of animals and perhaps humans.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There is growing evidence that sulfur amino acids (SAA), methionine and cysteine, play a metabolically and functionally important role in human health and disease (Shoveller et al. 2005). For example, methionine is a nutritionally indispensable AA for vertebrates (Wang et al. 2009), but on the other hand is also toxic to animals and humans (Garlick 2006). Cardiovascular disease in adults (Stipanuk 2004; Selhub 1999) and increased risk of stroke in infants and children (Hogeveen et al. 2002; Van Beynum et al. 1999) have been shown to be strongly associated with enhanced plasma levels of homocysteine, a key product of methionine metabolism via transmethylation pathway (Brosnan and Brosnan 2006). Recent evidence indicates that the gut is a significant site of net homocysteine release (Riedijk et al. 2007; Bauchart-Thevret et al. 2009a, b). Dietary methionine deficiency (Bauchart-Thevret et al. 2009a) or excess (Velez-Carrasco et al. 2008) directly effects on plasma homocysteine concentrations. The balance of dietary SAA (Shoveller et al. 2004), the route of feeding (enteral vs. parenteral) and the source of methionine (methionine vs. methionine hydroxy analogue) (Xie et al. 2007) were also demonstrated to affect plasma homocysteine concentrations. Thus, how to regulate the methionine metabolism with the objective of controlling the systemic homocysteine generates particular interest among researchers in clinical treatment of cardiovascular disease and stroke.
Notably, recent evidence supports the view that tissues of the intestine capture, transform, and degrade absorbed AA before their entry into portal circulation (Fang et al. 2009, 2010a; Riedijk and van Goudoever 2007; van Goudoever et al. 2006) and thus form a critical first line of defense against the vagaries of the dietary AA supply (van Goudoever et al. 2008), acting as a “gatekeeper” to defend the organism against AA toxicity (Baracos 2004). However, whether and how SAA are metabolized by the gut in the first pass remains an open question, the elucidation of which may have implications for nutritional strategies to manipulate homocysteine metabolism as a means to reduce the risk of cardiovascular disease and stroke. Furthermore, given that the intestinal epithelium obtains a substantial fraction of its metabolic energy from the catabolism of dietary AA and thereby results in decreased availability of these AA to extraintestinal tissues (Wu et al. 2005; Wu 1998; Stoll et al. 1998), the regulation of this metabolism may also have implications for nutritional efficiency of dietary AA. Therefore, the purpose of this article is to discuss the recent evidence regarding the intestinal metabolism of dietary SAA and the potential strategies to manipulate this metabolism.
New insights into intestinal metabolism of dietary SAA
Historically, it is assumed that dietary AA be absorbed from the lumen into the portal blood without degradation. However, this notion was questioned by the intriguing finding (Stegink and Besten 1972) that there was dropped plasma cysteine concentration when diets with methionine as the sole SAA were administered parenterally, whereas the concentration rose immediately when feeding switched to the oral route. Given that the parenteral feeding make the infused solution enter the circulation directly without first passing through the gut and liver, these results revealed that splanchnic tissues (mainly the gut and liver) may play an important role in the utilization of dietary methionine to cysteine synthesis. Shoveller et al. (2003a, b) also found that regardless of dietary cystine deficiency or excess, methionine requirements are ~30% lower in parenterally fed than in enterally fed piglets, further confirming the important first-pass metabolic demand of dietary methionine by splanchnic tissues. But from these studies, the relative contribution of the gastrointestinal tissues to the metabolism of dietary methionine remains unclear. With the increasing evidence that the gut may play an essential role in altering the concentrations and profiles of AA such as glutamine absorbed from the lumen before their entry into the portal blood (Windmueller 1982), the first-pass metabolism of dietary methionine in the gut generates growing interest among nutritional researchers. Stoll et al. (1998) implanted young piglets with portal and arterial catheters for determination of the portal balance of AA, and demonstrated that only 48% of dietary methionine intake was absorbed into the portal blood. On the basis of the net portal appearance, methionine rather than lysine was considered to be one of the limiting AA for young piglets. Fang et al. (2010a) used piglets implanted with arterial and portal catheters combined with the duodenal infusions of stable isotope tracer methionine (1-13C-methionine) to measure the appearance across and the use of the tracer by the portal drained viscera (PDV) (stomach, intestine, pancreas and spleen). The results confirmed that 30% of dietary methionine was metabolized by the intestine in the first pass. The earlier studies in rat (Finkelstein 2000) and recent studies in piglets (Bauchart-Thevret et al. 2009a) both demonstrate that the gastrointestinal tissues possess the significant activities of enzymes necessary to metabolize methionine to cysteine, which provided a further biochemical basis for the extensive utilization of methionine by the intestine (Bauchart-Thevret et al. 2009b; Shoveller et al. 2005).
However, recent studies (Chen et al. 2007, 2009) in vitro with isolated enterocytes seem contradictory to the view that the gut may be quantitatively important site for conversion of dietary methionine to both homocysteine and cysteine. In the studies conducted by Chen et al. (2009), enterocytes isolated from the jejunum of 0-, 7-, 14-, and 21-day-old piglets were incubated in Krebs buffer containing plasma concentrations of AA and one of the following tracer AA plus tracers: lysine, methionine, threonine, tryptophan, histidine, phenylalanine, and branched-chain AA (BCAA) including leucine, isoleucine and valine, to test whether the mucosal cells of the neonatal small intestine could degrade nutritionally indispensable AA. The results indicated that BCAA were extensively transaminated and 15–50% of decarboxylated branched-chain a-ketoacids were oxidized to CO2 depending on the age of piglets. In contrast to BCAA, catabolism of methionine and phenylalanine was negligible and that of other indispensable AA was absent in enterocytes from all ages of piglets due to the lack of key enzymes. The authors (Chen et al. 2009) concluded that previously observed extensive in vivo catabolism of methionine, histidine, lysine, phenylalanine, threonine or tryptophan by the small intestine (Stoll et al. 1998) may result from the action of luminal microbes in the intestinal mucosa (Blachier et al. 2007). In agreement with this notion, recent evidence demonstrated that dietary and endogenous AA were the main contributors to microbial protein in the upper gut of normally nourished pigs (Libao-Mercado et al. 2009), which means that microbial protein, if subsequently not digested and absorbed, may make a net loss to the host’s AA supply. However, it is also possible that 13C-methionine oxidation reported in vivo in pigs occurs by other cell types and tissues with the PDV, such as lymphocytes, fibroblast, pancreatic tissue, spleen tissue, or stomach as they all drain into the portal vein. In support of this view, Riedijk et al. (2007) demonstrated that 20% of dietary methionine intake was metabolized by the intestine and 40% of this was oxidized to CO2. One demand for intestinal methionine oxidation may be for synthesis of cysteine-rich mucins secreted by goblet cells involved in innate immune function (Van Klinken et al. 1998). Similarly, the observation that 14C radioactivity in the pancreas was about twice that in the intestine after administration of l-1-14C-methionine (Saunderson 1985) may imply the significant role of pancreas in the metabolism of dietary methionine, which remains to be defined.
In addition, it should also be cautioned that studies in vitro with isolated enterocytes have its own limitation and thus may not always reflect the case in vivo. Firstly, because the apical and basolateral membranes of each enterocyte are chemically, biochemically, and physically distinct (Madara 1991), the enterocytes can selectively receive nutrients from two sources: the arterial blood across its basolateral membrane and the intestinal lumen across its brush border membrane (Wu et al. 2005; Stoll and Burrin 2006). There is growing evidence that the intestine may preferentially oxidize the methionine derived from the artery rather than that absorbed from the lumen (Riedijk et al. 2007), further confirming the importance of that the bi-polar nature of the gut is stimulated in vitro, in particular using chamber systems as well as some cell systems such as Caco-2. In this regard, in vitro culture of isolated primary intestinal epithelial cells (Chen et al. 2009) may limit the utilization of methionine by these cells. Secondly, recent evidence (Riedijk et al. 2007) suggests that the high rate of methionine transsulfuration in the gut is driven by cysteine needs for glutathione synthesis because of the oxidant stress associated with the high metabolic activity of proliferating epithelial cells. Thus, the potential difference in the oxidation status associated with proliferation rate of epithelial cells between in vitro and in vivo studies may also result in difference in methionine metabolism. Thirdly, previous studies (Dangin et al. 2001) in young men demonstrate that a single meal of free AA mimicking casein composition compared with a single meal of slowly digested casein induced a stronger, more rapid and transient increase of AA oxidation. Therefore, the existing status (AA vs. protein) of nutrients used in the in vitro and in vivo studies combined with the dynamic access rate (fast vs. slow) of enterocytes to these nutrients may also result in difference in methionine metabolism between in vitro and in vivo studies. Thus, the relative contribution of PDV tissues and luminal microbes to the metabolism of dietary methionine remains to be elucidated.
The regulation of intestinal SAA metabolism
It is established that the gut is a significant site of net homocysteine release into the circulation (Riedijk et al. 2007; Bauchart-Thevret et al. 2009a, b) and moreover, the transmethylation and transsulfuration in splanchnic tissues are manipulated by dietary SAA (Shoveller et al. 2003a; Di Buono et al. 2003). Thus, the regulation of intestinal SAA metabolism may have implications for nutrition and health.
The regulation of intestinal SAA metabolism by dietary SAA status
The pioneering studies in humans (Stegink and Besten 1972) indicated that circulating plasma total cysteine concentrations were significantly greater in enterally than in parenterally fed men administered methionine as the sole dietary SAA. Further studies in piglets (Shoveller et al. 2003a) revealed that plasma cysteine concentrations were positively associated with SAA intake in enterally but not parenterally fed piglets. These results have two implications: firstly, splanchnic tissues may play an important role in the conversion of dietary methionine to cysteine in the first pass and secondly, dietary SAA status including the component (methionine or cysteine alone, or their combinations) and intake may effect on the transmethylation and transsulfuration of methionine and thus the net cysteine release from the splanchnic tissues. In support of this view, adult humans fed methionine alone [24 mg/(kg day)] had higher rates of transmethylation and transsulfuration and lower rates of remethylation than adults fed 13 mg methionine/(kg day) and 11 mg methionine/(kg day) (Di Buono et al. 2003). The studies in humans with isotopic tracers also showed indirectly that a substantial fraction of the dietary methionine transsulfuration occurs via first-pass splanchnic metabolism (Hiramatsu et al. 1994; Raguso et al. 1997). However, on the basis of these results, the role of the gut in SAA metabolism cannot be discriminated from that of the liver which is usually considered to be the major site of methionine transmethylation and transsulfuration. Most recently, Burrin and co-workers (Riedijk et al. 2007) using duodenal and intravenous infusion of stable isotope tracer methionine in infant piglets demonstrate that the gastrointestinal tract metabolizes 20% of dietary methionine intake, which is mainly transmethylated to homocysteine and transsulfurated to cysteine during conditions of diet supply with sufficient SAA. In contrast, under SAA-deficient conditions, methionine metabolism is prioritized in a coordinate manner, such that protein synthesis is preserved over methionine transmethylation and the methionine pool is preserved by upregulation of homocysteine remethylation and suppression of transsulfuration (Bauchart-Thevret et al. 2009a). These results make it clear that the gut is also a significant site of methionine metabolism and moreover, the metabolic fate (remethylation or transsulfuration) of methionine is regulated by dietary SAA status.
The potential regulation of SAA metabolism by methionine sources
Except for glycine, all AA can have l- and d-isoforms (Wu 2009). Most d-AA, except for d-arginine, d-cystine, d-histidine, d-lysine, and d-threonine, can be converted into l-AA in animals via widespread d-AA oxidases (d-AAOX) and transaminases (Baker 2009; Fang et al. 2009). However, because the efficiency of D-AA utilization, on a molar basis of the l-isomer, may be 20–100%, depending on substrates and species (Baker 2009), not all d-isomers can be widely used for nutritional purpose. In contrast, some d-isomers such as d-methionine (d-MET) have been widely accepted as a methionine source due to its nutritional efficiency and some specific functional role in health. Evidence in rats (Campbell et al. 1996) indicates that d-MET provides excellent protection from cisplatin ototoxicity. This is considered to be associated with that the d-MET is less well-metabolized than l-methionine (l-MET) in humans, so it may remain more available for cisplatin binding, thereby protecting the l-MET for needed protein synthesis, cell activation and metabolism. In support of this view, parenteral administration of dl-methionine (dl-MET) in humans results in higher plasma levels of the d-MET than that of the l-MET (Printen et al. 1979).
Another exciting new development in SAA nutrition is the discovery of the superiority of dl-2-hydroxy-4-methylthiobutyrate (dl-HMTB), the hydroxy analogue of dl-MET, to dl-MET in decreasing homocysteine production and alleviating stress responses. There is evidence that plasma ceruloplasmin, α-1 acid glycoprotein concentration, and heterophil to lymphocyte ratio in blood after lipopolysaccharide injection were lower in chicks fed a dl-HMTB diet than in chicks fed a dl-MET diet, which suggested that dietary dl-HMTB had a potential to alleviate certain stress responses (Matsushita et al. 2007). Furthermore, recent studies in ducks (Xie et al. 2007) indicated that plasma homocysteine of birds fed dl-HMTB-supplemented diets was significantly lower than birds fed equimolar dl-MET-supplemented diets, suggesting the less toxicity of dl-HMTB relative to dl-MET. However, there is limited biochemical evidence for these differences. The original studies (Martín-Venegas et al. 2006) in vitro with isolated chicken enterocytes showed that cysteine and taurine synthesis after incubation with dl-HMTB was higher when compared with l-MET incubation, indicating that cysteine and taurine formation by chicken enterocytes could be favored when dl-HMTB was used as a methionine source. Given that the high rate of methionine transsulfuration in the gut may be driven by cysteine needs for synthesis of mucins secreted by goblet cells involved in innate immune function (Van Klinken et al. 1998), the favored cysteine production following dl-HMTB administration may account for the potential of dl-HMTB to alleviate stress responses induced by lipopolysaccharide as evidenced by Matsushita et al. (2007). Recent studies (Fang et al. 2010a) in vivo with piglets implanted with arterial, portal and mesenteric catheters found that there was increased circulating plasma taurine concentration in dl-HMTB fed than in dl-MET fed piglets, further confirming the greater potential of dl-HMTB than of dl-MET to promote the transsulfuration of dietary methionine. Given that the increased taurine concentration was mainly observed in the arterial plasma rather than in the portal plasma, the liver may play a major role in methionine transsulfuration. Thus, that dl-HMTB might be preferentially diverted to the transsulfuration pathway by splanchnic tissues may in part account for the lower circulation homocysteine in dl-HMTB fed than dl-MET fed animals such as ducks (Xie et al. 2007).
However, based on previous reports (Martín-Venegas et al. 2006) that cysteine and taurine formation by isolated enterocytes could be favored when dl-HMTB rather than l-MET was used as a methionine source, dl-HMTB fed piglets should have higher portal plasma taurine concentration than dl-MET fed piglets, which was not observed in the studies of Fang et al. (2010a). The inconsistency between the in vitro and in vivo studies may be explained by the novel evidence that dl-HMTB absorption occurred primarily in the proximal gastrointestinal tract prior to the small intestine (Richards et al. 2005). The fact that until it is converted to l-MET, dl-HMTB is an organic acid, not an amino acid (Dibner and Buttin 2002), may provide a biochemical basis for the absorption of dl-HMTB in the upper gastrointestinal tract including the stomach. Furthermore, it is established that diffusion into cells represents a major route of organic acid uptake and occurs most rapidly at low pH when more of the acid will be protonated and lipophilic (Walter and Gutknecht 1984). In this regard, the low pH (<4.3) and considerable retention time (~2 h) of digesta in the stomach of piglets (Wilson and Leibholz 1981) may facilitate the absorption of dl-HMTB by the gastric tissues. Therefore, it is likely that dl-HMTB is high efficiently absorbed in the upper gastrointestinal tract of piglets, thereby reducing the amount of methionine sources that can be accessed by the intestine or luminal microbes in the first pass, which may imply the greater potential of dl-HMTB than AA such as dl-MET to bypass the first-pass intestinal metabolism as discussed below.
dl-HMTB, a methionine source with greater potential to bypass the first-pass intestinal metabolism
In addition to health relevant SAA metabolism, the recent intriguing data show that intestinal metabolism of methionine and its precursors may also have important implications for nutritional efficiency (Fang et al. 2009, 2010a, b). Given evidence that the extensive catabolism of dietary indispensable AA by the small intestine results in a decrease in their nutritional efficiency (Wu et al. 2005; Wu 1998; Stoll et al. 1998), there is growing interest in the question whether the catabolism of AA represents a functional requirement by the intestine for purposes of growth and function or if it is driven simply by the local availability of these substrates to the mucosal enterocytes (Fang et al. 2010a). Previous evidence (van Goudoever et al. 2000) indicated that intestinal oxidation of enteral lysine contributed one-third of total body lysine oxidation in growing pigs fed a high-protein diet, but was virtually absent in pigs fed a low-protein diet. In agreement with this notion, there was a substantial suppression of AA oxidation by the intestine during a low protein intake (van der Schoor et al. 2001). Further study revealed that the first-pass utilization rate of dietary lysine by the intestine was directly increased by the enteral lysine availability (Bos et al. 2003). These results indicate adaptive regulation of intestinal protein and AA metabolism. Therefore, it is likely that the high rate of mucosal AA catabolism in the intestine is under nutritional regulation, particularly by the protein intake of the animals (Fang et al. 2010a).
On the basis of that the small intestinal capacity to digest and absorb protein and AA is substantially greater than possible dietary inputs (Burrin et al. 1999), much of this organ’s demand for AA for maintenance may be an unnecessary burden (Bertolo et al. 2005). This raises a possibility that lowering intestinal AA metabolism without compromising gut absorptive capacity or protective functions may be promising for improving AA nutritional efficiency (Fang et al. 2010a). To test this hypothesis, Peng and co-workers (Fang et al. 2009, 2010a, b) conducted a series of studies with piglets implanted with arterial, portal and mesenteric catheters as the animal model and with dl-HMTB and dl-MET taken as the potential paradigms for “more” and “less” bypass-the-intestine AA, respectively. The results indicated that despite the difference in methionine sources, the first-pass utilization of dietary methionine by the intestine remained at ~30% of intake (Fang et al. 2010a). Similar results in piglets fed milk protein have been obtained in a previous study (Bos et al. 2003), in which dietary methionine intake is about 1.5-fold that administered by Fang et al. (2010a). These results suggested that the fraction of methionine might be more constant than the absolute amount of methionine that extracted by the intestine in its first-pass. It would appear that the more the local availability of dietary methionine absorbed into enterocytes, the more the absolute amount of methionine that metabolized by the intestine.
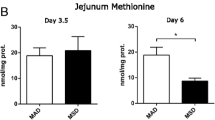
The distribution of activity of oxidation enzymes for conversion of dl-HMTB and d-MET may provide a biological basis for the difference in metabolism between sources (Fang et al. 2010b). Firstly, it was noteworthy that both D- and L-HMTB compared with only d-MET (comprising 50% of dl-MET) must be converted to l-MET before they can be used by the intestine (Dibner and Ivey 1992), such that the methionine precursor that needs converting in dl-HMTB diet was twice that in dl-MET diet (Fig. 1). Secondly, the rate-limiting enzymes for conversion of d-MET, d-HMTB and l-HMTB to l-MET are d-AAOX, d-2-hydroxy acid dehydrogenase (d-HADH) and l-2-hydroxy acid oxidase (l-HAOX), respectively (Dibner and Knight 1984) (Fig. 1). Studies in broilers (Dibner and Ivey 1992; Brachet and Puigserver 1992), piglets (Fang et al. 2010b) and ruminants (Lobley et al. 2006; McCollum et al. 2000) indicate that the intestine possesses considerable capacity to convert d-MET and d-HMTB to l-MET. In contrast, the enzyme activity values for d-AAOX were about fourfold that for l-HAOX and twofold that for d-HADH in both the duodenum and jejunum where dl-MET was mainly absorbed (Fig. 2). These results suggested that the intestine might possess a relatively higher capacity of d-MET utilization than of dl-HMTB utilization to l-MET synthesis. Thus, the more methionine precursor that needs converting in dl-HMTB than in dl-MET combined with the relatively lower oxidative activity the intestine possesses toward dl-HMTB may provide a biochemical evidence for that dl-HMTB might produce less l-MET than dl-MET when they were transported across the enterocytes, thereby reducing the first-pass metabolism of dietary methionine by the intestine (Fang et al. 2010b). In this regard, it is not surprised that there was no difference in the net portal balance of l-MET between piglets fed diets with 30% of the total methionine supplied by dl-MET or dl-HMTB (Fang et al. 2009), although the directly available l-MET in dl-MET diet was about 1.2-fold (85 vs. 70% of the total dietary methionine) that in dl-HMTB diet. Among the tissues evaluated, the liver and kidney possessing the highest l-HAOX and d-HADH activities indicates the sufficient capacity of methionine source utilization by the piglets (Fang et al. 2010b), although a major amount of these sources may be absorbed into the portal blood with few conversion occurring during the transport process (Lobley et al. 2006).
Activity values for d-AAOX, d-HADH and l-HAOX in the duodenum and jejunum of piglets fed diets with 30% of the total methionine supplied by dl-HMTB or dl-MET. Data were adapted from Fang et al. (2010b)
Conclusion and perspectives
The gut plays a key role not only in the digestion, absorption and metabolism of nutrients, but also in the immune surveillance of the intestinal epithelial layer and regulation of the mucosal response to foreign antigens. SAA, particularly methionine and cysteine, are critical for the gut to maintain these functions. However, the metabolism of SAA, specifically the transmethylation of methionine, will result in a net release of homocysteine, which is shown to be associated with cardiovascular disease and stroke. Furthermore, the extensive catabolism of dietary methionine by the intestine or by luminal microbes may result in a decrease in nutritional efficiency. Therefore, the regulation of SAA metabolism in the gut is not only nutritionally relevant, but also relevant to the overall health and well-being. The superiority of dl-HMTB to dl-MET in decreasing homocysteine production, alleviating stress responses, and reducing the first-pass intestinal metabolism of dietary methionine may provide a promising implication for nutritional strategies to manipulate SAA metabolism and thus to improve the nutrition and health status of animals and perhaps humans.
Abbreviations
- AA:
-
Amino acids
- BCAA:
-
Branched-chain amino acids
- d-AAOX:
-
d-Amino acid oxidase
- d-HADH:
-
d-2-Hydroxy acid dehydrogenase
- dl-HMTB:
-
dl-2-Hydroxy-4-methylthiobutyrate
- dl-MET:
-
dl-Methionine
- l-HAOX:
-
l-2-Hydroxy acid oxidase
- PDV:
-
Portal drained viscera
- SAA:
-
Sulfur amino acids
References
Baker DH (2009) Advances in protein–amino acid nutrition of poultry. Amino Acids 37:29–41
Baracos VE (2004) Animal models of amino acid metabolism: a focus on the intestine. J Nutr 134:1656S–1659S
Bauchart-Thevret C, Stoll B, Chacko S, Burrin DG (2009a) Sulfur amino acid deficiency upregulates intestinal methionine cycle activity and suppresses epithelial growth in neonatal pigs. Am J Physiol Endocrinol Metab 296:E1239–E1250
Bauchart-Thevret C, Stoll B, Burrin DG (2009b) Intestinal metabolism of sulfur amino acids. Nutr Res Rev 22:175–187
Bertolo RFP, Pencharz PB, Ball RO (2005) Role of intestinal first-pass metabolism on whole-body amino acid requirements. In: Burrin DG, Mersmann HJ (eds) Biology of metabolism in growing animals. Elsevier, London, pp 127–156
Blachier F, Mariotti F, Huneau JF, Tome D (2007) Effects of amino acid-derived luminal metabolites on the colonic epithelium and physiopathological consequences. Amino Acids 33:547–562
Bos C, Stoll B, Fouillet H, Gaudichon C, Guan X, Grusak MA, Reeds PJ, Tome D, Burrin DG (2003) Intestinal lysine metabolism is driven by the enteral availability of dietary lysine in piglets fed a bolus meal. Am J Physiol Endocrinol Metab 285:E1246–E1257
Brachet P, Puigserver A (1992) Regional differences for the d-amino acid oxidase-catalysed oxidation of d-methionine in chicken small intestine. Comp Biochem Physiol B 101:509–511
Brosnan JT, Brosnan ME (2006) The sulfur-containing amino acids: an overview. J Nutr 136:1636S–1640S
Burrin D, Stoll B, Chang X, Yu H, Reeds P (1999) Total parenteral nutrition does not compromise digestion or absorption of dietary protein in neonatal pigs. FASEB J 13:A1024
Campbell KCM, Rybak LP, Meech RP, Hughes L (1996) d-Methionine provides excellent protection from cisplatin ototoxicity in the rat. Hear Res 102:90–98
Chen LX, Yin YL, Jobgen WS, Jobgen SC, Knabe DA, Hu WX, Wu G (2007) In vitro oxidation of essential amino acids by intestinal mucosal cells of growing pigs. Livest Sci 109:19–23
Chen L, Li P, Wang J, Li X, Gao H, Yin Y, Hou Y, Wu G (2009) Catabolism of nutritionally essential amino acids in developing porcine enterocytes. Amino Acids 37:143–152
Dangin M, Boirie Y, Garcia-Rodenas C, Gachon P, Fauquant J, Callier P, Ballèvre O, Beaufrère B (2001) The digestion rate of protein is an independent regulating factor of postprandial protein retention. Am J Physiol 280:E340–E348
Di Buono M, Wykes LJ, Cole DE, Ball RO, Pencharz PB (2003) Regulation of sulfur amino acid metabolism in men in response to changes in sulfur amino acid intakes. J Nutr 133:733–739
Dibner JJ, Buttin P (2002) Use of organic acids as a model to study the impact of gut microflora on nutrition and metabolism. J Appl Poult Res 11:453–463
Dibner JJ, Ivey FJ (1992) Capacity in the liver of the broiler chick for conversion of supplemental methionine activity to l-methionine. Poult Sci 71:1695–1699
Dibner JJ, Knight CD (1984) Conversion of 2-hydroxy-4-(methylthio)butanoic acid to l-methionine in the chick: a stereospecific pathway. J Nutr 114:1716–1723
Fang ZF, Luo J, Qi ZL, Huang FR, Zhao SJ, Liu MY, Jiang SW, Peng J (2009) Effects of 2-hydroxy-4-methylthiobutyrate on portal plasma flow and net portal appearance of amino acids in piglets. Amino Acids 36:501–509
Fang ZF, Huang FR, Luo J, Wei HK, Ma LB, Jiang SW, Peng J (2010a) Effects of dl-2-hydroxy-4-methylthiobutyrate on the first-pass intestinal metabolism of dietary methionine and its extraintestinal availability. Br J Nutr. doi:10.1017/S0007114509992169
Fang ZF, Luo HF, Wei HK, Huang FR, Qi ZL, Jiang SW, Peng J (2010b) Methionine metabolism in piglets fed DL-methionine or its hydroxy analogue was affected by distribution of enzymes oxidizing these sources to keto-methionine. J Agric Food Chem. doi:10.1021/jf903317x
Finkelstein JD (2000) Pathways and regulation of homocysteine metabolism in mammals. Semin Thromb Hemost 26:219–225
Garlick PT (2006) Toxicity of methionine in humans. J Nutr 136:1722S–1725S
Hiramatsu T, Fukagawa NK, Marchini JS, Cortiella J, Yu YM, Chapman TE, Young VR (1994) Methionine and cysteine kinetics at different intakes of cystine in healthy adult men. Am J Clin Nutr 60:525–533
Hogeveen M, Blom HJ, Van Amerongen M, Boogmans B, Van Beynum IM, Van De Bor M (2002) Hyperhomocysteinemia as risk factor for ischemic and hemorrhagic stroke in newborn infants. J Pediatr 141:429–431
Libao-Mercado AJ, Zhu CL, Cant JP, Lapierre H, Thibault JN, Sève B, Fuller MF, de Lange CF (2009) Dietary and endogenous amino acids are the main contributors to microbial protein in the upper gut of normally nourished pigs. J Nutr 139:1088–1094
Lobley GE, Wester TJ, Calder AG, Parker DS, Dibner JJ, Vázquez-Añón (2006) Absorption of 2-hydroxy-4-methylthiobutyrate and conversion to methionine in lambs. J Dairy Sci 89:1072–1080
Madara JL (1991) Functional morphology of epithelium of the small intestine. In: Shultz SG (ed) Handbook of physiology: the gastrointestinal system. American Physiological Society, Bethesda, MD, pp 83–120
Martín-Venegas R, Geraert PA, Ferrer R (2006) Conversion of the methionine hydroxy analogue dl-2-hydroxy-(4-methylthio) butanoic acid to sulfur-containing amino acids in the chicken small intestine. Poult Sci 85:1932–1938
Matsushita K, Takahashi K, Akiba Y (2007) Effects of adequate or marginal excess of dietary methionine hydroxy analogue free acid on growth performance, edible meat yields and inflammatory response in female broiler chickens. Poult Sci 44:265–272
McCollum MQ, Vázquez-Añón M, Dibner JJ, Webb KE Jr (2000) Absorption of 2-hydroxy-4-(methylthio)butanoic acid by isolated sheep ruminal and omasal epithelia. J Anim Sci 78:1078–1083
Printen KJ, Brummel MC, Ei Soon Cho MS, Stegink LD (1979) Utilization of d-methionine during total parenteral nutrition in postsurgical patients. Am J Clin Nutr 32:1200–1205
Raguso CA, Ajami AM, Gleason R, Young VR (1997) Effect of cystine intake on methionine kinetics and oxidation determined with oral tracers of methionine and cysteine in healthy adults. Am J Clin Nutr 66:283–292
Richards JD, Atwell CA, Vázquez-Añón M, Dibner JJ (2005) Comparative in vitro and in vivo absorption of 2-hydroxy-4(methylthio) butanoic acid and methionine in the broiler chicken. Poult Sci 84:1397–1405
Riedijk MA, van Goudoever JB (2007) Splanchnic metabolism of ingested amino acids in neonates. Curr Opin Clin Nutr Metab Care 10:58–62
Riedijk MA, Stoll B, Chacko S, Schierbeek H, Sunehag AL, van Goudoever JB, Burrin DG (2007) Methionine transmethylation and transsulfuration in the piglet gastrointestinal tract. Proc Natl Acad Sci USA 104:3408–3413
Saunderson CL (1985) Comparative metabolism of l-methionine, dl-methionine and dl-2-hydroxy-4-methylthiobutanoic acid by broiler chicks. Br J Nutr 54:621–633
Selhub J (1999) Homocysteine metabolism. Annu Rev Nutr 19:217–246
Shoveller AK, Brunton JA, Pencharz PB, Ball RO (2003a) The methionine requirement is lower in neonatal piglets fed parenterally than in those fed enterally. J Nutr 133:1390–1397
Shoveller AK, Brunton JA, House JD, Pencharz PB, Ball RO (2003b) Dietary cysteine reduces the methionine requirement by an equal proportion in both parenterally and enterally fed piglets. J Nutr 133:4215–4224
Shoveller AK, House JD, Brunton JA, Pencharz PB, Ball RO (2004) The balance of dietary sulfur amino acids and the route of feeding affect plasma homocysteine concentrations in neonatal piglets. J Nutr 134:609–612
Shoveller AK, Stoll B, Ball RO, Burrin DG (2005) Nutritional and functional importance of intestinal sulfur amino acid metabolism. J Nutr 135:1609–1612
Stegink LD, Besten LD (1972) Synthesis of cysteine from methionine in normal adult subjects: effect of route of alimentation. Science 178:514–516
Stipanuk MH (2004) Sulfur amino acid metabolism: pathways for production and removal of homocysteine and cysteine. Annu Rev Nutr 24:539–577
Stoll B, Burrin DG (2006) Measuring splanchnic amino acid metabolism in vivo using stable isotope tracers. J Anim Sci 84:E60–E72
Stoll B, Henry J, Reeds PJ, Yu H, Jahoor F, Burrin DG (1998) Catabolism dominates the first-pass intestinal metabolism of dietary essential amino acids in milk protein-fed piglets. J Nutr 128:606–614
Van Beynum IM, Smeitink JA, den Heijer M, te Poele Pothoff MT, Blom HJ (1999) Hyperhomocysteinemia: a risk factor for ischemic stroke in children. Circulation 99:2070–2072
van der Schoor SR, van Goudoever JB, Stoll B, Henry JF, Rosenberger JR, Burrin DG, Reeds PJ (2001) The pattern of intestinal substrate oxidation is altered by protein restriction in pigs. Gastroenterology 121:1167–1175
Van Goudoever JB, Stoll B, Henry JF, Burrin DG, Reeds PJ (2000) Adaptive regulation of intestinal lysine metabolism. Proc Natl Acad Sci USA 97:11620–11625
van Goudoever JB, van der Schoor SR, Stoll B, Burrin DG, Wattimena D, Schierbeek H, Schaart MW, Riedijk MA, van der Lugt J (2006) Intestinal amino acid metabolism in neonates. Nestle Nutr Workshop Ser Pediatr Program 58:95–102, discussion 102–108
van Goudoever JB, Corpeleijn W, Riedijk M, Schaart M, Renes I, van der Schoor S (2008) The impact of enteral insulin-like growth factor 1 and nutrition on gut permeability and amino acid utilization. J Nutr 138:1829S–1833S
Van Klinken BJ, Einerhand AW, Buller HA, Dekker J (1998) Strategic biochemical analysis of mucins. Anal Biochem 265:103–116
Velez-Carrasco W, Merkel M, Twiss CO, Smith JD (2008) Dietary methionine effects on plasma homocysteine and HDL metabolism in mice. J Nutr Biochem 19:362–370
Walter A, Gutknecht J (1984) Monocarboxylic acid permeation through lipid bilayer membranes. J Membr Biol 77:255–264
Wang WW, Qiao SY, Li DF (2009) Amino acids and gut function. Amino Acids 37:105–110
Wilson RH, Leibholz J (1981) Digestion in the pig between 7 and 35 d of age. 2. The digestion of dry matter and the pH of digesta in pigs given milk and soya-bean proteins. Br J Nutr 45:321–336
Windmueller HG (1982) Glutamine utilization by the small intestine. Adv Enzymol 53:201–237
Wu G (1998) Intestinal mucosa amino acid metabolism. J Nutr 128:1249–1252
Wu G (2009) Amino acids: metabolism, functions, and nutrition. Amino Acids 37:1–17
Wu G, Knabe DA, Flynn NE (2005) Amino acid metabolism in the small intestine: biochemical bases and nutritional significance. In: Burrin DG, Mersmann HJ (eds) Biology of metabolism in growing animals. Elsevier, London, pp 107–126
Xie M, Hou SS, Huang W, Fan HP (2007) Effect of excess methionine and methionine hydroxy analogue on growth performance and plasma homocysteine of growing Pekin ducks. Poult Sci 86:1995–1999
Acknowledgments
This work was supported by the National Natural Science Foundation of China (30901042), the Program for Changjiang Scholars and Innovative Research Team in the University (IRTO555), and the Key Project of Sichuan Provincial Education Department (00924100). The authors thank graduate students, technicians, and colleagues for their important contributions to the work described in this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fang, Z., Yao, K., Zhang, X. et al. Nutrition and health relevant regulation of intestinal sulfur amino acid metabolism. Amino Acids 39, 633–640 (2010). https://doi.org/10.1007/s00726-010-0502-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00726-010-0502-x