Abstract
Chronic coinfection with hepatitis C virus (HCV) and human immunodeficiency virus (HIV) is among the greatest challenges facing public health worldwide. In this population, the response to hepatitis C therapy by treatment with pegylated interferon plus ribavirin (PEG-IFN+RBV) is lower than in HCV-monoinfected patients, particularly in those infected by HCV genotype 1. A PKR/eIF-2α phosphorylation homology domain (PePHD) within the E2 protein has been found to interact with PKR and inhibit PKR in vitro, suggesting a possible mechanism for HCV to evade the antiviral effects of IFN. The aim of this work was to analyze the amino acid conservation in the HCV-E2-PePHD and quasispecies diversity among HCV-HIV-coinfected patients exhibiting sustained virological response, non-response, or partial response with viral relapse to PEG-IFN+RBV by ultra-deep pyrosequencing. For this purpose, HCV-E2-PePHD PCR products were generated and sequenced directly for four patients with a sustained response, seven patients with no virological response, and four patients with viral relapse before and after treatment with PEG-IFN+RBV. HCV-E2-PePHD amino acid sequences were obtained for isolates from serum collected before and during treatment (24 h, 4 weeks, and 12 weeks). Quasispecies analysis of the HCV-E2-PePHD and flanking genomic regions was performed using 454/Roche pyrosequencing, analyzing 39,364 sequence reads in total. The HCV-E2-PePHD sequence at the amino acid and nucleotide level was highly conserved among HCV genotype 1 strains, irrespective of the PEG-IFN+RBV response. This high degree of amino acid conservation and sporadic mutations in the HCV-E2-PePHD domain do not appear to be associated with treatment outcome. The HCV-E2-PePHD sequence before or during treatment cannot be used to predict reliably the outcome of treatment in patients coinfected with HCV genotype 1 and HIV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatitis C virus (HCV) infection is a major cause of chronic hepatitis and hepatocellular carcinoma worldwide [1]. A significant proportion of patients with chronic hepatitis C in Western countries are co-infected with HIV [2]. In this population, the response to hepatitis C therapy is lower than in HCV-monoinfected patients [3, 4]. The HCV genotype appears to be a major determinant, because patients infected with HCV genotype 2 (HCV-2) or HCV-3 have a higher rate of response to pegylated interferon combined with ribavirin (PEG-IFN+RBV) than those infected with HCV-1 [5]. The mechanisms underlying the strong PEG-IFN+RBV resistance observed in patients infected with HCV-1 are unclear. A direct interaction between viral proteins and the IFN-α pathway has been suggested. The HCV envelope protein 2 (E2) of HCV-1 isolates has been shown to inhibit IFN-α-induced protein kinase (PKR) in vitro by means of a specific interaction with a 12-amino-acid domain: PePHD (PKR-eIF2alpha phosphorylation homology domain). This domain may act as a pseudosubstrate for PKR, inhibiting its kinase activity and impairing the inhibition of viral protein synthesis mediated by this enzyme [6]. The sequence of the HCV-E2-PePHD domain of HCV-1 is more similar to that of the PKR autophosphorylation site than are the sequences of the other genotypes. The relationship between HCV-E2-PePHD sequence conservation and resistance to antiviral treatments for HCV-1 infection in vivo has not been described for HIV-coinfected patients.
In this manuscript, we report that the pattern of mutations in the HCV-E2-PePHD motif and flanking genomic regions analysed by ultra-deep pyrosequencing (UDPS) are not involved in the acquisition of PEG-IFN+RBV resistance in HIV-coinfected patients, and consequently, its use as prognostic marker of therapy response appears to be inappropriate in this population.
Materials and methods
Study samples
Among 593 HIV-positive patients, >18 years old, who were attended to at our unit for their scheduled controls for HIV viral load (VL) at the Argentinean National Reference Centre for AIDS (CNRS) [7, 8], this prospective study included 15 HIV-HCV coinfected patients who were followed up prior to and during therapy with PEG-IFN-α+RBV. Individual data were collected on baseline clinical, biochemical, virological, and histological parameters (Table 1). Treatment was planned for 48 weeks in all patients. All of them received subcutaneous PEG-IFN alfa-2b (Peg-Intron-A, Schering Corp., Kenilworth, NJ) (80–150 mg, body-weight-adjusted dosing) each week plus oral ribavirin (Rebetol, Schering Corp., Kenilworth, NJ) every day. RBV dosing was body weight-adjusted in all cases.
All of the patients gave consent to participate in this study, which was evaluated and approved according to the ethical guidelines of the 1975 Declaration of Helsinki by the local ethics committee.
Blood samples were drawn at baseline (immediately before initiating the therapy), 24 h, 4, and 12 weeks. Plasma samples were frozen at −80 °C until use.
HCV-RNA (COBAS AMPLICOR® Hepatitis C Virus Test, version 2.0) and HCV-VL (Bayer VERSANT® HCV RNA 3.0 Assay, range 615–7,690,000 IU/mL) were measured at each time point (Table 2).
The 15 patients were infected with HCV-1 as determined by LiPA VERSANT® HCV Genotype Assay (Siemens Healthcare Diagnostics, Argentina). Four of these patients achieved a sustained virological response (SVR) to antiviral therapy, defined as the absence of HCV RNA detection by PCR six months after the end of treatment. Seven patients did not respond (NR) and did not achieve viral clearance at the end of treatment, and the remaining four were relapsers (BT) who experienced reappearance of serum HCV RNA after achieving an undetectable level at the end of therapy.
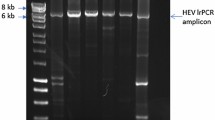
Amplification and direct sequencing of the HCV-E2-PePHD domain nucleotide sequence and its flanking regions
A previously described classical nested RT-PCR method [9] was used, including an initial RT step followed by two rounds of amplification. HCV RNA was extracted from plasma (200 μl) using TRIzol LS (GIBCO, Life Technologies, MI, USA). RNA extracts were reverse transcribed with a specific primer (5′-AGYARCATCATCCACAAGCAGG-3′; nucleotide positions 2539 to 2561 according to the numbering for HCV-J). RT was carried out at 42 °C for 60 min in the presence of 12.5 U of Moloney murine leukemia virus reverse transcriptase (Invitrogen, Argentina). The first round of PCR was carried out with the RT primer described above as the outer antisense primer (20 pmol) and with primer 5′-TCCAGCTKATMAACACCAACGGCA-3′ (nucleotide positions 1593-1596) as the outer sense primer (20 pmol). The first round of amplification consisted of 35 cycles, as follows: denaturation at 94 °C for 30 s, primer annealing at 55 °C for 50 s, and primer extension at 72 °C for 2 min, followed by a final prolonged extension step at 72 °C for 5 min. The second step was performed with the inner sense primer 5′-CGACTACCCATACAGGCTCTGG-3′ (20 pmol; nucleotide positions 2168 to 2185) and the inner antisense primer 5′-GCAGGMRCAGACCGCGCGCGTC-3′ (20 pmol; nucleotide positions 2523 to 2544). The conditions for the second round were identical to those for the first round. Negative controls, in which distilled water replaced the RNA or cDNA, were included at each of the three steps to ensure that the RT and PCR mixtures were not contaminated. HCV-negative serum samples were used to assess the specificity of the assay. Amplified products were subjected to electrophoresis in 1% agarose gels (Gibco BRL, MI, USA) and stained with ethidium bromide. A 376-bp PCR product 155 nucleotides upstream and 204 nucleotides downstream from the HCV-E2-PePHD domain was generated. The DNA obtained from the purified nested-PCR products (Quick Spin; QIAGEN, Venlo, The Netherlands) was directly subjected to double-strand sequencing with dye-labeled dideoxy terminators (ABI PRISM 3100 automated sequencer, Applied Biosystems, Foster City, CA, USA).
Ultra-deep pyrosequencing (UDPS)
UDPS was used to sequence HCV-E2-PePHD and flanking genomic regions after PCR amplification. The primers used were those previously employed for the second round, modified by 5′ Tag extensions, which provided binding sites for pyrosequencing on the genome sequence. The tags were as follows: sense-Tag 5′-CACGACGTTGTAAAACGA-3′; antisense-Tag 5′-CAGGAAACAGCTATGACC-3′.
PCR-purified amplicons were quantified using Quant-iT PicoGreen (Invitrogen, Life Technologies, MI, USA). In addition, an Agilent 2100 bioanalyzer (Agilent Life Science, Santa Clara, California, USA) was used to verify the quality and length of the amplicons. After quality controls, PCR amplicons from each patient were pooled in equimolar concentrations and sequenced in the forward direction on a 454 Life Science platform (GS-FLX, Roche Applied Science) according to the manufacturer’s instructions. This technical approach increases the probability of detecting minority variants that are poorly represented in the heterogeneous viral population existing in a patient’s circulation.
To distinguish authentic minority variants from technical artefacts, we used an estimation threshold of 1%. Mutations detected above that threshold by UDPS were unlikely to have resulted from a technical artefact based on a theoretical calculation reported previously using a statistical approach [10].
Nucleotide sequences and phylogenetic analysis
DNA sequences were edited, assembled and translated using the Sequencher software v.4.10.1 (Gene Codes). Reference sequences for the HCV genotypes 1a and 1b were obtained from GenBank [11, 12]. Multiple sequence alignments were achieved using the Mafft program [13, 14]. BioEdit 5.0 software [15] was used to detect longitudinal amino acid variations among HCV-E2-PePHD sequences characterized during each patient follow-up.
The most appropriate substitution model for our datasets was selected with hierarchical likelihood ratio testing implemented in jModelTest 3.7 [16]. The best-fitting model for our dataset was GTR+G+I. The maximum-likelihood method with heuristic searches was implemented in the PhyML version 3.0 computer program [17]. Support for individual nodes in the most likely tree topology was estimated using a non-parametric bootstrap test (1000 replicates). The tree topologies were midpoint-rooted for purposes of illustration and drawn using the Dendroscope v2.7.4 program [18].
Statistical analysis
A descriptive analysis of baseline variables was conducted looking at the central tendency and dispersion. These values were compared to ensure that the demographic, epidemiological, and clinical characteristics were similar among patients in different groups. The Mann-Whitney test was used to analyze quantitative variables. The p-values (two-tailed) <0.05 were considered statistically significant. Statistical analysis was performed using SPSS v.12.0 (SPSS Corporation, Chicago, IL)
Results
Patient characteristics
When comparing sustained virological responder, relapser and non-responder patient groups, no significant differences (p > 0.05) were found in the mean ± SD age (39.5 ± 6.8, 40.3 ± 5.6, and 40.3 ± 6.5 years, respectively), HCV viral load (5.9 ± 5.7, 6.0 ± 6.1, and 6.5 ± 6.5, log IU/ml, respectively), CD4 T cell count (721 ± 254, 473 ± 160, and 638 ± 545 cells/ml, respectively), or ALT level (62.8 ± 55.1, 105.3 ± 66.3, 75.9 ± 21.4) (Table 1). Thirteen out of the 15 patients were males.
The mean (±SD) baseline HCV viral load across the three studied groups was 6.2 (±0.54) log IU/ml. Since the 15 patients were undergoing antiretroviral therapy, the HIV viral load was undetectable (<1.7 log IU/ml) in all of them except one (NR5, 4 log IU/ml). Samples from four time points were studied from non-responder patients, including one collected prior to therapy and the other three collected during therapy. For the remaining two groups, the times at which samples were analyzed depended on the partial or complete virological response to treatment. Despite the rapid decrease in HCV plasma viral load in responders, sequence data were available for four patients undergoing therapy, who were sampled during the first month of treatment, but no consistent changes were detected in the HCV-E2-PePHD or flanking regions (Table 2).
The number of sequence reads determined for each sample was 872 on average, reaching a total of 39,364 pyrosequences reads that passed quality control. The quality control criteria [19] included (i) a perfect match to the barcode and primer sequences, (ii) >400 bases in length, and (iii) no undetermined bases.
Direct sequence analysis
HCV-E2-PePHD domain and flanking nucleotide sequences obtained by direct sequencing of the nested PCR products were aligned with the reference strands (HCV-J for genotype 1b –D90208- and HCV-1 for genotype 1a –M62321-). Figure 1 shows the amino acid composition of the amplified E2 region from viral isolates obtained during the follow-up from the three study groups of patients. In all of the groups, the HCV-E2-PePHD domain appeared to be highly conserved prior to and during HCV treatment, remaining unchanged irrespective of the therapy response.
Amplified HCV-E2 amino acid region of relapsers (BT), sustained virological responders (SVR) and non-responders (NR) to peg-IFN+RBV treatment, prior to (Basal) and during antiviral therapy (24 h, and 4 and 12 weeks). The PePHD domain is highlighted. Gen Bank M62321 (genotype 1a) and D90208 (genotype 1b) sequences were used as references
When phylogenetic analysis was carried out using the sequences of all of the HCV isolates, most of them were assigned to genotype 1a, except for two (SVR-4 and BT-4) that belonged to HCV-1b. The clustering observed among isolates grouped the sequences according to their patient origin, but they were not related with respect to their final response to PEG-IFN+RBV therapy (Fig. 2).
Maximum-likelihood tree of HCV-E2 sequences. Fifteen HCV-1 sequences from samples collected prior to (Basal) and during peg-IFN+RBV treatment (24 h, 4 and 12 weeks) were analyzed. Black circles denote reference sequences used for different genotypes and subtypes. Bootstrap values are shown at branches. Branch lengths are proportional to the number of nucleotide substitutions per aligned site (bar = 0.1 substitutions). NR: non-responders; SVR: sustained virological responders; BT: relapsers
Analysis of UDPS-derived HCV-E2-PePHD sequences and their relationship to IFN-response
The amino acid composition of the HCV-E2-PePHD was highly conserved when it was compared among all the sequences analyzed (39,364 HCV sequences). There was more than 99% amino acid conservation per site (Table 3).
The pyrosequencing-derived HCV-E2-PePHD amino acid sequences at baseline and subsequent sampling times were highly conserved among the HCV-1 isolates (from the four sustained responders, the four relapsers and the seven non-responders) by both inter- and intra-patient comparison, regardless of the treatment outcome.
However, when the HCV-E2-PePHD flanking regions were compared by UDPS, the amino acid sequences exhibited larger heterogeneity at both the inter- and intra-host level, sustaining the phylogenetic clustering described previously (Fig. 1). HCV minority variants (less than 5% relative abundance in the total viral population) appeared during the longitudinal intra-patient analysis, but no such viral quasispecies emerged as a majority variant during PEG-IFN+RBV therapy (data not shown).
Discussion
Like other RNA viruses, HCV replicates rapidly, and the RNA polymerase lacks proofreading activity, resulting in the accumulation of mutations at a rate of 0.4 × 10−3 to 1.2 × 10−3 bases substitutions per site per year [20–22]. These high substitution rates were reflected in the amino acids variability observed throughout the amplicon analyzed. Strikingly, the amino acid HCV-E2-PePHD domain was extremely conserved, showing less than 0.4% of mutations per amino acid position.
Several authors have postulated that this domain could be involved in resistance to IFN-based therapy [23, 24], although the issue is still controversial, since other authors have found no relationship between mutations in HCV-E2-PePHD and response to treatment [25, 26]. Taylor et al. [6] reported that HCV-E2-PePHD-deleted HCV-1 mutants remain capable of binding to PKR to some extent, while C-terminally truncated E2 protein loses its PKR-inhibiting activity. This finding indicates that HCV E2 regions other than PePHD within the C-terminal part of this glycoprotein could interact with PKR, possibly playing a role in suppressing PKR, a mediator of IFN-induced antiviral resistance. Thus, the HCV-E2-PePHD flanking regions could be implicated in treatment resistance, but this study shows that these regions are conserved and that no minor variants emerge during treatment. Moreover, those variants disappeared after treatment.
Many authors have reported that HCV-E2-PePHD is a highly conserved region [23, 24, 27–35], but none of them described these results in patients coinfected with HIV. Gaudy et al. [26] found a high degree of conservation of HCV-E2-PePHD in monoinfected patients with genotype 1b and no association between HCV-E2-PePHD mutations and response to treatment, while Yahoo et al. [34] reported high amino acid conservation in HCV-1a at four weeks of treatment. The effect of HIV infection on PEG-IFN+RBV therapy outcome could produce changes in T-cell subsets. When increased, the PEG-IFN+RBV doses mainly affected CD4+ T-cells but failed to modify clinical outcome [36]. Also, regarding the effect of accompanying antiretroviral drugs on virological response to PEG-IFN+RBV, it has been suggested that with the exception of regimens including zidovudine, accompanying antiretroviral drugs have little effect on the virological response [37]. Bagaglio et al. [38] studied the variation of HCV-E2-PePHD among HIV-coinfected patients, but in HCV genotype 3a, and suggested that the E2-PePHD genetic variability at baseline is not associated with treatment response and that anti-HCV treatment did not influence HCV heterogeneity within the E2 domain. Similarly, among six HCV-3a-monoinfected patients, Afzal et al. [24] reported that the E2-PePHD domain was not entirely conserved and had substitutions in some isolates irrespective of the treatment response. However, they suggested that the breakthrough response in a single patient could be related to the presence of an amino acid change in the HCV-E2-PePHD sequence that made this domain more similar to that of HCV genotype 1a. Here, by ultra-deep sequencing analysis of HCV-1 isolates from HIV-coinfected patients, before treatment and at several sampling times during PEG-IFN+RBV treatment, a high degree of amino acid conservation of this region was found among responders, relapsers and non-responders. Furthermore, the ultra deep sequencing analysis allowed us to identify minority populations that have not been found by the traditional cloning method. The role of these populations and whether those sequences have an influence on PEG-IFN+RBV treatment outcome is unclear.
The high degree of amino acid conservation in the HCV-E2-PePHD domain does not appear to be associated with treatment resistance but might be involved, like other E2 domains, in specific functions such as inhibition of cellular apoptosis [39] and CD81 binding, allowing the virus to enter cells [40].
References
Thomson EC, Smith JA, Klenerman P (2011) The natural history of early hepatitis C virus evolution; lessons from a global outbreak in HIV-1 infected individuals. J Gen Virol. doi:10.1099/vir.0.033910-0
Pang PS, Planet PJ, Glenn JS (2009) The evolution of the major hepatitis C genotypes correlates with clinical response to interferon therapy. PLoS One 4(8):e6579. doi:10.1371/journal.pone.0006579
Rockstroh JK, Mocroft A, Soriano V, Tural C, Losso MH, Horban A, Kirk O, Phillips A, Ledergerber B, Lundgren J (2005) Influence of hepatitis C virus infection on HIV-1 disease progression and response to highly active antiretroviral therapy. J Infect Dis 192(6):992–1002. doi:10.1086/432762
Torriani FJ, Rodriguez-Torres M, Rockstroh JK, Lissen E, Gonzalez-Garcia J, Lazzarin A, Carosi G, Sasadeusz J, Katlama C, Montaner J, Sette H Jr, Passe S, De Pamphilis J, Duff F, Schrenk UM, Dieterich DT (2004) Peginterferon Alfa-2a plus ribavirin for chronic hepatitis C virus infection in HIV-infected patients. N Engl J Med 351(5):438–450. doi:10.1056/NEJMoa040842
Manns MP, McHutchison JG, Gordon SC, Rustgi VK, Shiffman M, Reindollar R, Goodman ZD, Koury K, Ling M, Albrecht JK (2001) Peginterferon alfa-2b plus ribavirin compared with interferon alfa-2b plus ribavirin for initial treatment of chronic hepatitis C: a randomised trial. Lancet 358(9286):958–965 (pii:S0140673601061025)
Taylor DR, Shi ST, Romano PR, Barber GN, Lai MM (1999) Inhibition of the interferon-inducible protein kinase PKR by HCV E2 protein. Science 285(5424):107–110 (pii:7641)
Laufer N, Bolcic F, Rolon MJ, Martinez A, Reynoso R, Perez H, Salomon H, Cahn P, Quarleri J (2011) HCV RNA decline in the first 24 h exhibits high negative predictive value of sustained virologic response in HIV/HCV genotype 1 co-infected patients treated with peginterferon and ribavirin. Antiviral Res 90(1):92–97. doi:10.1016/j.antiviral.2011.02.013
Laufer N, Quarleri J, Bouzas MB, Juncos G, Cabrini M, Moretti F, Bolcic F, Fernandez-Giuliano S, Mammana L, Salomon H, Cahn P (2010) Hepatitis B virus, hepatitis C virus and HIV coinfection among people living with HIV/AIDS in Buenos Aires, Argentina. Sex Transm Dis 37(5):342–343. doi:10.1097/OLQ.0b013e3181d73c0d
Bolcic F, Bull L, Martinez L, Reynoso R, Salomon H, Arduino R, Barnett B, Quarleri J (2008) Analysis of sequence configurations of the PKR-interacting HCV proteins from plasma and PBMC as predictors of response to interferon-alpha and ribavirin therapy in HIV-coinfected patients. Intervirology 51(4):261–264. doi:10.1159/000158523
Eriksson N, Pachter L, Mitsuya Y, Rhee SY, Wang C, Gharizadeh B, Ronaghi M, Shafer RW, Beerenwinkel N (2008) Viral population estimation using pyrosequencing. PLoS Comput Biol 4(4):e1000074. doi:10.1371/journal.pcbi.1000074
Kuiken C, Hraber P, Thurmond J, Yusim K (2008) The hepatitis C sequence database in Los Alamos. Nucleic Acids Res 36(Database issue):D512–D516. doi:10.1093/nar/gkm962
Kuiken C, Korber B, Shafer RW (2003) HIV sequence databases. AIDS Rev 5(1):52–61
Katoh K, Misawa K, Kuma K, Miyata T (2002) MAFFT: a novel method for rapid multiple sequence alignment based on fast Fourier transform. Nucleic Acids Res 30(14):3059–3066
Katoh K, Asimenos G, Toh H (2009) Multiple alignment of DNA sequences with MAFFT. Methods Mol Biol 537:39–64. doi:10.1007/978-1-59745-251-9_3
Hall T (1999) BioEdit: a user-friendly biological sequence alignment editor and analysis program for Windows 95/98/NT. Nucl Acids Symp Ser 41:95–98
Posada D (2008) jModelTest: phylogenetic model averaging. Mol Biol Evol 25(7):1253–1256. doi:10.1093/molbev/msn083
Guindon S, Gascuel O (2003) A simple, fast, and accurate algorithm to estimate large phylogenies by maximum likelihood. Syst Biol 52(5):696–704 (pii:54QHX07WB5K5XCX4)
Huson DH, Richter DC, Rausch C, Dezulian T, Franz M, Rupp R (2007) Dendroscope: an interactive viewer for large phylogenetic trees. BMC Bioinformatics 8:460. doi:10.1186/1471-2105-8-460
Huse SM, Huber JA, Morrison HG, Sogin ML, Welch DM (2007) Accuracy and quality of massively parallel DNA pyrosequencing. Genome Biol 8(7):R143. doi:10.1186/gb-2007-8-7-r143
Ogata N, Alter HJ, Miller RH, Purcell RH (1991) Nucleotide sequence and mutation rate of the H strain of hepatitis C virus. Proc Natl Acad Sci USA 88(8):3392–3396
Okamoto H, Kojima M, Okada S, Yoshizawa H, Iizuka H, Tanaka T, Muchmore EE, Peterson DA, Ito Y, Mishiro S (1992) Genetic drift of hepatitis C virus during an 8.2-year infection in a chimpanzee: variability and stability. Virology 190(2):894–899
Smith DB, Pathirana S, Davidson F, Lawlor E, Power J, Yap PL, Simmonds P (1997) The origin of hepatitis C virus genotypes. J Gen Virol 78(Pt 2):321–328
Ukai K, Ishigami M, Yoshioka K, Kawabe N, Katano Y, Hayashi K, Honda T, Yano M, Goto H (2006) Mutations in carboxy-terminal part of E2 including PKR/eIF2alpha phosphorylation homology domain and interferon sensitivity determining region of nonstructural 5A of hepatitis C virus 1b: their correlation with response to interferon monotherapy and viral load. World J Gastroenterol 12(23):3722–3728
Afzal S, Idrees M, Akram M, Awan Z, Khubaib B, Aftab M, Fatima Z, Badar S, Hussain A (2010) Mutations in the E2-PePHD region of hepatitis C virus genotype-3a and correlation with response to interferon and ribavirin combination therapy in Pakistani patients. Virol J 7:377. doi:10.1186/1743-422X-7-377
Munoz de Rueda P, Casado J, Paton R, Quintero D, Palacios A, Gila A, Quiles R, Leon J, Ruiz-Extremera A, Salmeron J (2008) Mutations in E2-PePHD, NS5A-PKRBD, NS5A-ISDR, and NS5A-V3 of hepatitis C virus genotype 1 and their relationships to pegylated interferon-ribavirin treatment responses. J Virol 82(13):6644–6653. doi:10.1128/JVI.02231-07
Gaudy C, Lambele M, Moreau A, Veillon P, Lunel F, Goudeau A (2005) Mutations within the hepatitis C virus genotype 1b E2-PePHD domain do not correlate with treatment outcome. J Clin Microbiol 43(2):750–754. doi:10.1128/JCM.43.2.750-754.2005
Berg T, Mas Marques A, Hohne M, Wiedenmann B, Hopf U, Schreier E (2000) Mutations in the E2-PePHD and NS5A region of hepatitis C virus type 1 and the dynamics of hepatitis C viremia decline during interferon alfa treatment. Hepatology 32(6):1386–1395. doi:10.1053/jhep.2000.20527
Chayama K, Suzuki F, Tsubota A, Kobayashi M, Arase Y, Saitoh S, Suzuki Y, Murashima N, Ikeda K, Takahashi N, Kinoshita M, Kumada H (2000) Association of amino acid sequence in the PKR-eIF2 phosphorylation homology domain and response to interferon therapy. Hepatology 32(5):1138–1144. doi:10.1053/jhep.2000.19364
Gerotto M, Dal Pero F, Pontisso P, Noventa F, Gatta A, Alberti A (2000) Two PKR inhibitor HCV proteins correlate with early but not sustained response to interferon. Gastroenterology 119(6):1649–1655 (pii:S0016508500186731)
Hung CH, Lee CM, Lu SN, Lee JF, Wang JH, Tung HD, Chen TM, Hu TH, Chen WJ, Changchien CS (2003) Mutations in the NS5A and E2-PePHD region of hepatitis C virus type 1b and correlation with the response to combination therapy with interferon and ribavirin. J Viral Hepat 10(2):87–94 (pii:414)
Sarrazin C, Bruckner M, Herrmann E, Ruster B, Bruch K, Roth WK, Zeuzem S (2001) Quasispecies heterogeneity of the carboxy-terminal part of the E2 gene including the PePHD and sensitivity of hepatitis C virus 1b isolates to antiviral therapy. Virology 289(1):150–163. doi:10.1006/viro.2001.1092
Jenke AC, Moser S, Orth V, Zilbauer M, Gerner P, Wirth S (2009) Mutation frequency of NS5A in patients vertically infected with HCV genotype 1 predicts sustained virological response to peginterferon alfa-2b and ribavirin combination therapy. J Viral Hepat 16(12):853–859. doi:10.1111/j.1365-2893.2009.01140.x
Yokozaki S, Katano Y, Hayashi K, Ishigami M, Itoh A, Hirooka Y, Nakano I, Goto H (2011) Mutations in two PKR-binding domains in chronic hepatitis C of genotype 3a and correlation with viral loads and interferon responsiveness. J Med Virol 83(10):1727–1732. doi:10.1002/jmv.21959
Yahoo N, Sabahi F, Shahzamani K, Malboobi MA, Jabbari H, Sharifi H, Mousavi-Fard SH, Merat S (2011) Mutations in the E2 and NS5A regions in patients infected with hepatitis C virus genotype 1a and their correlation with response to treatment. J Med Virol 83(8):1332–1337. doi:10.1002/jmv.22144
Bagaglio S, De Mitri MS, Lodrini S, Paties C, Cassini R, Bianchi G, Bernardi M, Lazzarin A, Morsica G (2005) Mutations in the E2-PePHD region of hepatitis C virus type 1b in patients with hepatocellular carcinoma. J Viral Hepat 12(3):243–250. doi:10.1111/j.1365-2893.2005.00589.x
Massanella M, Tural C, Papagno L, Garcia E, Jou A, Bofill M, Autran B, Clotet B, Blanco J (2010) Changes in T-cell subsets in HIV-HCV-coinfected patients during pegylated interferon-alpha2a plus ribavirin treatment. Antivir Ther 15(3):333–342. doi:10.3851/IMP1531
Berenguer J, von Wichmann MA, Quereda C, Miralles P, Mallolas J, Lopez-Aldeguer J, Alvarez-Pellicer J, De Miguel J, Crespo M, Guardiola JM, Tellez MJ, Galindo MJ, Arponen S, Barquilla E, Bellon JM, Gonzalez-Garcia J (2011) Effect of accompanying antiretroviral drugs on virological response to pegylated interferon and ribavirin in patients co-infected with HIV and hepatitis C virus. J Antimicrob Chemother 66(12):2843–2849. doi:10.1093/jac/dkr362
Bagaglio S, Bruno R, Lodrini S, De Mitri MS, Andreone P, Loggi E, Galli L, Lazzarin A, Morsica G (2003) Genetic heterogeneity of hepatitis C virus (HCV) in clinical strains of HIV positive and HIV negative patients chronically infected with HCV genotype 3a. J Biol Regul Homeost Agents 17(2):153–161
Lee SH, Kim YK, Kim CS, Seol SK, Kim J, Cho S, Song YL, Bartenschlager R, Jang SK (2005) E2 of hepatitis C virus inhibits apoptosis. J Immunol 175(12):8226–8235 (pii:175/12/8226)
Owsianka AM, Timms JM, Tarr AW, Brown RJ, Hickling TP, Szwejk A, Bienkowska-Szewczyk K, Thomson BJ, Patel AH, Ball JK (2006) Identification of conserved residues in the E2 envelope glycoprotein of the hepatitis C virus that are critical for CD81 binding. J Virol 80(17):8695–8704. doi:10.1128/JVI.00271-06
Acknowledgments
This study was supported partially by grants from the University of Buenos Aires (SECYT-UBA 2010-2012) and the Consejo Nacional de Investigaciones Científicas y Técnicas (CONICET-PIP112 200801 01773). The authors thank Sergio Mazzini (Centro Nacional de Referencia para el SIDA, Departamento de Microbiología, Facultad de Medicina, Universidad de Buenos Aires, Argentina) for his assistance during the manuscript preparation.
Conflict of interest
The authors declare that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bolcic, F., Sede, M., Moretti, F. et al. Analysis of the PKR-eIF2alpha phosphorylation homology domain (PePHD) of hepatitis C virus genotype 1 in HIV-coinfected patients by ultra-deep pyrosequencing and its relationship to responses to pegylated interferon-ribavirin treatment. Arch Virol 157, 703–711 (2012). https://doi.org/10.1007/s00705-012-1230-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00705-012-1230-1