Abstract
This study was conducted in an Afro-Brazilian, slave-descendant community with high (42.4%) hepatitis B virus (HBV) prevalence. Twenty (8.4%) out of the 239 subjects under study were HBsAg-positive, and HBV-DNA was detected in 59 (25%) individuals. A high rate (18.3%) of occult infection was therefore observed that was associated to low HBV loads (mean, 1.8 × 104 copies/ml) and to a specific amino acid substitution (C100Y) in the small surface antigen. Genotyping of 50 isolates showed that 43 (86%) were of subgenotype A1, one (2%) from subgenotype A2, and five (10%) from subgenotype D. Mixed genotypes A1 and E were observed in one (2%) sample. The genetic distance (0.8 ± 0.3%) among the HBV/A1 isolates from the community was smaller than the intragroup divergence among A1 isolates from Brazil as a whole, but it was similar to that found between A2 isolates from different countries, suggesting that HBV/A1 was introduced in the community through different sources. The substitution W501R (polymerase), previously reported only in Gambia, was observed in 46% of the HBV/A1 isolates. The precore/core promoter region of HBsAg-positive isolates showed several substitutions that could explain the anti-HBe phenotype found in 18 of 20 (90%) of the HBsAg-positive subjects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatitis B virus (HBV) is still a major cause of liver disease worldwide despite the introduction in the last decades of vaccination programs. It is estimated that 2 billion people have been infected with HBV and that more than 350 million are chronic carriers of the virus. HBV is an etiological agent of acute self-limited hepatitis B, asymptomatic HBV status, fulminant hepatitis and chronic hepatitis that can progress to liver cirrhosis and hepatocellular carcinoma (HCC) [22].
Based on sequence divergence of 8% or more in the entire genome, HBV isolates are classified into eight genotypes, designated A–H, with a distinct geographical distribution [31, 32]. Genotype A circulates in Europe, India, Africa, and North and South America [9, 32]. This genotype is now divided into three subgenotypes: one of African origin that was originally designated subgroup A′ [5] and renamed subgenotype Aa [39] or subtype A1 [17]. The subgenotype of European origin has been designated Ae [39] or A2 [17]. A third subgenotype, A3, has been identified in Cameroon [21]. Isolates belonging to genotypes B and C have been observed in Southeast Asia and the Far East. Genotype D is widespread, with a high prevalence in the Mediterranean area and in the Middle East region. Genotype G is infrequent and has mainly been found in Europe, Mexico, and the USA [32], while genotype E is native to West Africa [19, 28], and genotypes F and H are considered indigenous to Latin America [9]. Genotypes A, D and F are the most prevalent in Brazil [4, 24, 26, 38]. Recently, a high proportion of genotype A, subtype A1, was observed among HBV Brazilian isolates [4, 24].
Occult HBV infection is defined as the presence of HBV-DNA in blood and/or liver of patients in the absence of detectable hepatitis B surface antigen (HBsAg). Prevalence data of occult infection reported in different studies are difficult to compare due to important differences in the composition of the studied populations and the level of sensitivity of the HBV-DNA detection assay. However, high rates of occult hepatitis B have been observed in endemic areas for HBV infection [12, 43]. Occult HBV infection rates varying from 5 to 55% among subjects with chronic hepatitis, with or without HCC, have been observed [3, 6]. It has also been reported in populations without symptomatic liver disease, such as blood donors (BD), individuals with normal liver tests or general populations (rates from 0 to 17%) [6, 25].
Mutations in HBV nucleotide sequence may occur at any stage of infection, allowing the emergence of variant viruses, including mutations in the precore, basal core promoter (BCP), pre-S/S and polymerase regions [8]. The precore and BCP regions play an important role in HBV replication and HBeAg production. Thus, mutations in these regions have been detected in many HBeAg-negative patients with persistent viremia and active liver disease [2, 10].
In a previous study with 12 semi-isolated communities in Central Brazil, almost exclusively composed of descendants of African slaves, a mean overall HBV infection prevalence of 19.8% was found. Large variations in infection rates were observed from one community to another. The highest prevalences were detected in the Furnas dos Dionísios (FD) community, with 42.4% and 7.4% for hepatitis B core antibody (anti-HBc) and HBsAg, respectively [27]. In the present study, this community was chosen in order to investigate the prevalence of occult HBV infection, the HBV genotype distribution, and the occurrence of intrafamilial transmission. In addition, genetic variability of precore, BCP, and small S regions, as well as of the overlapping parts of the polymerase gene, was examined.
Materials and methods
Study population
This study was conducted in Furnas dos Dionisios (FD), a semi-isolated Afro-Brazilian community in the State of Mato Grosso do Sul (MS), Central Brazil. The FD community consists of about 80 families. Two hundred thirty-nine (88%) of the 271 individuals previously examined for HBV epidemiological status [27] were included in this study. Sera from the 32 remaining subjects were not available for molecular studies. The age range of the individuals was 2–87 years (mean, 25.7 ± 18.4 years). One hundred twenty-one (50.6%) individuals were male and 118 (49.4%) were female. This study was approved by the Human Ethics Committee of the Federal University of Mato Grosso do Sul, and informed consent was obtained from all subjects.
HBV serological tests
Detection of HBsAg, anti-HBc and anti-HBs were performed using enzyme-linked immunosorbent assay (ELISA) (Hepanostika Uni-form Organon Teknika B. V., Boxtel, Holland). HBsAg-positive samples were tested for the presence of anti-HBc IgM, HBeAg and anti-HBe (Hepanostika Uni-form Organon Teknika B. V.).
PCR amplification and genotyping
Viral DNA was extracted from all 239 serum samples as previously reported [29] and subjected to a semi-nested PCR performed with Taq polymerase (Invitrogen, San Diego, CA) to amplify the almost complete pre-S/S region. This assay uses, in the first round, sense primer PS1 and a mixture of antisense primers S2 and S22, which makes possible the amplification of all HBV genotypes. The second round of amplification was performed with 1 μl of the first-round PCR product, using primers PS1 and SR (Table 1). This two-round PCR assay, resulting in amplicons shorter than those described in our original genotyping study [4], was recently standardized to increase sensitivity (to three DNA molecules per assay) without a loss of specificity [27]. Isolates were genotyped by using a restriction fragment length polymorphism (RFLP) analysis of PCR products. For this, PCR products were digested separately with BamHI, EcoRI and StuI restriction endonucleases [4, 27].
Nucleotide sequencing
HBV-DNA-positive samples were subjected to amplification of the entire S region using a semi-nested PCR assay. The first round of amplification was carried out with sense primer PS1 and antisense primers S2 and S22. The second round of amplification was performed with sense primer S1 and antisense primers S2 and S22 (Table 1). BCP and precore regions were amplified by semi-nested PCR, using primers X4 and C2 in the first round and X4 and C3 in the second round. Nucleotide sequences of the amplified regions were determined by direct sequencing using a BigDye Terminator kit (Applied Biosystems, Foster City, CA) with specific HBV primers (S1, S2, S22, S4, S7 and C1, Table 1). Sequencing reactions were analyzed on an ABI3730 + automated sequencer (Applied Biosystems). Bioinformatics analysis of the sequences was performed using the University of Wisconsin Genetic Computer Group package. A neighbor-joining phylogenetic tree was drawn and rearranged using the Mega program version 3 [20]. Phylogenetic analysis was performed and genetic distances were determined using 37 HBV isolates from the FD community, 18 HBV/A Brazilian isolates from other places, three of which were from blood donors (BD) living in the city of Campo Grande, located at 45 km from the FD community, 33 HBV/A1 from Africa, and 44 GenBank sequences representative of HBV genotypes from other geographical regions.
Quantification of HBV-DNA
HBV-DNA-positive samples were quantified using the real-time PCR TaqMan technology, according to Pas and Niesters [34], with some modifications. A panel of reference sera was used for quantification by real-time PCR. This panel was tested by comparison to commercially available panels and contained known numbers of HBV-DNA molecules. Amplification assays were performed in a final volume of 25 μL of TaqMan universal Master Mix (Applied BioSystems), containing 2 μL of DNA, 1 μM each of sense S14 and antisense S17 primers (Table 1), and 0.3 μM of probe (5′-FAM-TGTTGACAARAATCCTCACAATACCRCAGA-TAMRA-3′, nucleotide position 218–247). After initial incubation steps of 2 min at 50°C and 10 min at 95°C, the PCR cycling program consisted of 50 cycles of 15 sec at 95°C and 60 sec at 60°C. Reactions were performed in a 7700 SDS system (Applied BioSystems). The assay has a limit of detection of 10 copies/reaction, i.e., 100 copies/ml of serum.
Avoiding PCR contamination
Extreme care was taken to avoid PCR contamination. Positive and negative controls were included in all runs of DNA extraction and PCR amplification reactions. No more than 10 serum samples were extracted together. In addition, water was subjected to the same steps of extraction and PCR amplification, as a negative control. All samples subjected to PCR-RFLP amplification were tested in two independent assays of DNA extraction and PCR amplification. Only samples that were positive in both independent assays were considered positive for HBV-DNA.
Results and discussion
Hepatitis B serological profile and HBV-DNA results
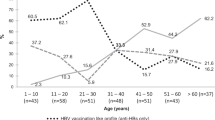
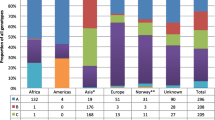
Table 2 shows that 20 out of 239 (8.4%) individuals were HBsAg-positive. An anti-HBs-positive/anti-HBc-positive/anti-HBc-IgM-negative serological pattern, corresponding to past HBV infection, was observed in 87 (36.4%) subjects. Five (2.1%) individuals were ‘anti-HBc only’. Isolated anti-HBs was detected in 68 (28.4%) subjects, probably as a result of previous vaccination. The pre-S/partial S region was successfully amplified in 59 (24.7%) samples. HBV-DNA was detected in 19 of 20 (95%) HBsAg-positive- and 40 of 219 HBsAg-negative samples, showing an overall occult infection rate of 18.3%. Such a high rate of occult HBV infection (18.3%) in an Afro-Brazilian slave-descendant community where high prevalence rates of anti-HBc (42.4%) and HBsAg (7.4%) had been detected previously [27] was in accordance with some studies which reported that occult HBV infection is frequent in regions where HBV is endemic [3, 6, 25, 43, 45]. Six HBsAg-negative samples, which gave PCR-positive, although not reproducible, results were considered HBV-DNA negative. The presence of HBV-DNA was detected in samples showing an HBsAg-negative pattern, varying from 40% (2/5 subjects) among individuals with anti-HBc alone to 10.2% (6/59) among subjects without any HBV serological marker (Table 2). HBV-DNA levels were measured by real-time PCR in 48 of 59 HBV-DNA-positive samples. HBV-DNA loads were significantly higher (p = 0.041) in the HBsAg-positive patients (mean, 1.9 × 107 copies/ml) than among those with occult infection (1.8 × 104 copies/ml). In agreement with previous reports [11, 16, 23, 30, 44], the most probable reason for occult infection is the occurrence of low HBV loads.
Molecular characterization and evolutionary analysis of S and P regions
Fifty out of 59 (85%) HBV-DNA-positive samples were successfully genotyped by PCR-RFLP. Forty-four (88%) of them belonged to genotype A, 43 of which were from subgenotype A1 and one was from subgenotype A2. Subgenotype A1 has been shown to be common in both Brazilian [4, 24, 38] and African [5, 17–19, 33] populations and has also been detected at a high frequency in Afro-Venezuelan groups [35]. These results suggested an African origin for the HBV isolates circulating in the Afro-Brazilian community under study, probably as a result of the slave trade that took place during three centuries (1,551–1,857). Five (10%) isolates belonged to genotype D, which is common in Brazil [24, 38]. The presence of few genotype D isolates in the FD community may be explained by a recent entry of young black people who moved from an urban zone to the community. A mixture of genotypes A1 and E was observed in one sample (2%). Nucleotide sequencing of the small S gene was successfully performed in 37 of the 50 isolates. Phylogenetic analysis (Fig. 1) of these 37 isolates confirmed RFLP patterns, with 34 isolates belonging to subgenotype A1. One isolate (FD151) belonged to subgenotype A2 and another one (FD09) clustered with genotype D sequences. The sequence from isolate FD123 that displayed mixed A + E genotypes by PCR-RFLP analysis clustered with genotype E sequences, indicating that the major HBV population belonged to genotype E. Interestingly, the HBV genotype E carrier was born in Angola (he came to the FD community in 2000). This genotype circulates in western, sub-Saharan Africa but has never been found in people born in Brazil. The absence of genotype E is compatible with the hypothesis of Mulders et al. [28], who suggested the emergence of genotype E as a human pathogen in the mid-to-late nineteenth century, at a time when the slave trade was already over.
Phylogenetic analysis based on nucleotide sequencing of the small S region. Sequences whose names begin with FD (filled circle, isolated community) and BD (blood donors) are from this work. F1 to F13 refer to the 13 families of the FD community under study. Genotypes are indicated at the branches of the tree
The possibility of intrafamilial transmission was investigated among members of the FD community. Family was defined as father, mother and offspring. Five sequences were derived from family F1, eight from F2, five from F3, seven from F4, two from F5, two from F6, and two from F7. The remaining six sequences, namely FD191, FD123, FD09, FD174, FD97 and FD210, were the unique representatives of families F8 to F13, respectively. The phylogenetic tree (Fig. 1) shows that some HBV sequences, derived from members of the same family, were located in distinct groups. Inversely, two identical sequences (FD95-F1 and FD219-F3) were derived from members of different families. In areas that are highly endemic for HBV, different modes of horizontal transmission may occur as a consequence of close and frequent contacts between family members, especially in populations with low socioeconomic level and poor hygiene conditions [13, 40, 42]. In this study, no correlation could be established between families and HBV nucleotide sequences. This may be due to a high rate of inter-family/intra-community transmission.
To further explore the phylogenetic relatedness and genetic diversity of FD sequences, molecular genetic distances were calculated among 100 HBV sequences divided into four groups. Nucleotide sequence divergences in the small S region within (1) 18 HBV/A1 Brazilian sequences from different geographical regions, (2) 33 HBV/A1 sequences from Africa, (3) 28 HBV/A1-FD sequences, and (4) 21 HBV/A2 isolates from different continents were 1.3 ± 0.4%, 1.5 ± 0.3%, 0.8 ± 0.2% and 0.9 ± 0.4%, respectively. The sequence variation (0.8 ± 0.3%) within the group of HBV/A1-FD isolates was smaller than intragroup divergence found between HBV/A1 isolates circulating in Brazil (1.3 ± 0.4%) but similar to sequence variation between HBV/A2 isolates from different countries (0.9 ± 0.4%). Hannoun et al. [15] have speculated that the A2 subgenotype has evolved from a subgroup of A1 isolates exported from southern Africa to Europe about 500 years ago or later. In a similar way, one could argue that the HBV/A1-FD isolates were derived from a subset of A1 African isolates and may have been evolving in relative isolation.
Table 3 shows the amino acid changes observed in the S protein in comparison with a consensus of 33 African HBV/A1 (HBV/A1-AF) sequences. HBV/A1-FD sequences were also compared to a consensus (HBV/A1-BR) obtained by alignment of the 18 sequences from HBV/A1 isolates of different geographical Brazilian regions. FD isolates sharing the same S protein sequence were grouped. All positions in which amino acid variations were observed in more than one FD sequence are shown in Table 3. Most amino acid substitutions found in the S protein were linked to genotypes. All HBV/A-FD sequences displayed Lys 122 residues (Table 3) as well as Pro 127, Phe 134 Lys 160 (not shown), allowing the classification of these samples as serotype adw2. The deduced serotypes of isolates FD123 (genotype E) and FD09 (genotype D) were ayw4 and ayw3, respectively. Some variations specific for HBV/A1-FD isolates were observed when compared with amino acid residues of the consensus HBV/A1-AF and with residues typical of HBV/A1-BR. Except for one residue (aa 194), the consensus sequences from African and Brazilian sequences were identical. At position 194, most of the HBV/A1-FD isolates displayed the same amino acid, Ala 194, as in the HBV/A1 Brazilian consensus sequence, whereas African sequences showed Val 194. Fifteen FD isolates displayed the same amino acid sequence as the HBV/A1-BR consensus. The most prevalent substitution among HBV/A1-FD isolates was Y100C, observed in 8 of 37 isolates. Interestingly, all samples displaying Y100C were from cases of HBV occult infection. This mutation has been previously found in HBsAg-negative and anti-HBc-positive BD from Venezuela [14]. Further studies of in vitro HBsAg expression of HBV isolates with the Y100C substitution should be conducted to verify the association between this mutation and the HBsAg-negative phenotype.
As shown in Table 4, the deduced amino acid sequences of polymerase (aa 359–569) in FD isolates demonstrated the presence of mutations in several positions. Except for two positions (401 and 457; not shown), the consensus sequences from the African and Brazilian sequences were identical. In these positions, all but one HBV/A1-FD isolate displayed the same amino acids (Ile 401 and Ser 457) as in the HBV/A1-BR consensus. The most frequent specific mutation of the Afro-descendant community was W501R, found in 17 HBV/A1-FD isolates. This substitution in the viral polymerase was previously identified only in Gambia [15]. Interestingly, it is known that a number of slaves who came to Brazil were from Gambia [36]. This suggested that substitution W501R may be used as a marker of HBV isolates originating in Gambia.
Precore/core mutations linked to HBeAg phenotype
Several studies have emphasized the potential importance of BCP and precore mutations in viral persistence during residual infection. The most common naturally occurring variations include the precore stop codon mutation G1896A, which abolishes HBeAg production [7, 10], and the double mutation A1762T-G1764A in the BCP, which down-regulates the expression of HBeAg [37, 39]. In this study, most (18/20) of the HBsAg-positive patients were anti-HBeAg positive. The age of these 20 HBsAg-positive individuals varied from 8 to 52 years (mean, 21 years). To identify mutations in the BCP and precore gene regions that may explain the predominance of the anti-HBe phenotype, nucleotide sequence analysis was carried out. This was performed for 10/20 HBV/A1-FD HBsAg-positive samples (two HBeAg-positive and eight anti-HBe-positive). All isolates were from subgenotype A1. Independent of their HBeAg status, all samples showed C at nt 1,858 and, as expected, G at nt 1,896, which precludes the occurrence of the classical precore stop codon, HBeAg-negative mutation [10]. A high rate (60%, 6/10) of the double substitution A1762T-G1764A, located in the BCP region, was found. This mutation, which has been associated with the HBeAg suppressive phenotype, is also prevalent in isolates from HBV/A1 carriers [1, 7, 15, 41]. The G1862T substitution (in the bulge of the encapsidation signal) was found in all 10 of the HBV/A1-FD isolates that were sequenced. This mutation is commonly detected in HBV/A1 isolates and affects virus replication and production of HBeAg [15, 39, 41]. The G1888A substitution, which introduces an extra precore start codon, was found in 7 of 10 samples. All 10 HBV/A1-FD isolates showed the double G1809T-C1812T mutation, which is only found in subgenotype A1 isolates. This double mutation alters the Kozak sequence preceding the precore start codon at nt 1,814 and may impair HBeAg expression as a result of suboptimal translation initiation [17]. The triple mutations G1809T-C1810T-C1812T and G1809T-A1811C-C1812T were observed in two samples (FD56 and FD58). These changes can severely impair the expression of HBeAg [1, 17, 39]. As in black Southern-African carriers infected with subgenotype A1 [18], a high proportion of anti-HBe was observed. This association seems to be characteristic of subgenotype A1. However, in a previous study conducted with subgenotype A1 isolates from 14 HBeAg-positive children (age 7–29; median, 13 years), mutations G1809T-C1812T, G1862T and G1888A were frequently detected [15]. It was suggested that these changes may produce stable variants that, for some reason, have become prevalent in subgenotype A1, even in HBeAg-positive subjects. However, in the present study, as in other ones, those mutations were mainly detected in anti-HBe-positive individuals. The difference in HBeAg status between these populations may be related to the age of the subjects. Indeed, the median age (21 years) of the subjects studied here was higher than that in the study by Hannoun et al. [15]. One hypothesis is that the occurrence of such mutations, related to the anti-HBe phenotype, may be cumulative, increasing gradually with age. However, the low number of HBeAg-positive isolates observed here makes this conclusion uncertain. Further investigations in populations infected with subgenotype A1 and their different HBeAg status should be conducted to verify this possibility.
References
Ahn S, Kramvis A, Kawai S, Spangenberg H, Li J, Kimbi G, Kew MC, Wands J, Tong S (2003) Sequence variation upstream of the precore AUG start codon of hepatitis B virus reduces HBe-antigen production. Gastroenterology 125:1370–1378
Akahane Y, Yamanaka T, Suzuki H, Sugai Y, Tsuda F, Yotsumoto S, Omi S (1990) Chronic active hepatitis with hepatitis B virus DNA and antibody against e antigen in the serum. Disturbed synthesis and secretion of e antigen from hepatocytes due to a point mutation in the precore region. Gastroenterology 99:1113–1119
Allain J-P (2004) Occult hepatitis B virus infection. Transfus Clin Biol 11:18–25
Araujo NM, Mello FCA, Yoshida CFT, Niel C, Gomes SA (2004) High proportion of subgenotype A’ (genotype A) among Brazilian isolates of hepatitis B virus. Arch Virol 149:1383–1395
Bowyer SM, van Staden L, Kew MC, Sim JGM (1997) A unique segment of the hepatitis B virus group A genotype identified in isolates from South Africa. J Gen Virol 78:1719–1729
Brechot C, Thiers V, Kremsdori D, Nalpas B, Pol S, Paterlini-Brechot P (2001) Persistent hepatitis B virus infection in subjects without hepatitis B surface antigen: clinically significant or purely “occult”? Hepatology 34:194–203
Buckwold VE, Xu Z, Yen TS, Ou JH (1997) Effects of a frequent double-nucleotide basal core promoter mutation and its putative single nucleotide precursor mutation on hepatitis B virus gene expression and replication. J Gen Virol 78:2055–2065
Buti M, Rodriguez-Frias F, Rosendo J, Esteban R (2005) Hepatitis B virus genome variability and disease progression: the impact of pre-core mutants and genotypes. J Clin Virol 34:S79–S82
Campos RH, Mbayed VA, Pinero Y, Leone FG (2005) Molecular epidemiology of hepatitis B virus in Latin America. J Clin Virol 34(2):S8–S13
Carman WF, Jacyna MR, Hadziyannis P, McGarvey MJ, Markis A, Thomas HC (1989) Mutation prevention formation of hepatitis B e antigen in patients with chronic hepatitis B infection. Lancet 2:588–591
Chaudhuri CJ, Nanu A, Panda SK, Chand P (2003) Evaluation of serologic screening of blood donors in India reveals a lack of correlation between anti-HBc and PCR-amplified HBV DNA. Transfusion 43:1442–1448
Chemin C, Trepo C (2005) Clinical impact of HBV infections. J Clin Virol 34(1):S15–S21
Dumpis U, Holmes EC, Mendy M, Hill A, Thusz M, Hall A, Whittle H, Karayiannis P (2001) Transmission of hepatitis B virus infection in Gambian families revealed by phylogenetic analysis. J Hepatol 35:99–104
Gutierrez C, Devesa M, Loureiro CL, Leon G, Liprandi F, Pujol FH (2004) Molecular and serological evaluation of surface antigen negative hepatitis B virus infection in blood donors from Venezuela. J Med Virol 1:1–8
Hannoun C, Soderstrom A, Norkrans G, Lindh M (2005) Phylogeny of African complete genome reveals a West African genotype A subtype of hepatitis B virus and relatedness between Somali and Asian A1 sequences. J Gen Virol 86:2163–2167
Hennig H, Puchta I, Luhm J, Schlenke P, Goerg S, Kirchner H (2002) Frequency and load of hepatitis B virus DNA in first-time blood donors with antibodies to hepatitis B core antigen. Blood 100:2637–2641
Kimbi GC, Kramvis A, Kew MC (2004) Distinctive sequence characteristics of subgenotype A1 isolates of hepatitis B virus from South Africa. J Gen Virol 85:1211–1220
Kramvis A, Weitzmann L, Owiredu WKBA, Kew MC (2002) Analysis of the complete genome of subgenotype A’ hepatitis B virus isolates from South Africa. J Gen Virol 83:835–839
Kramvis A, Restorp K, Norder H, Botha JF, Magnius LO, Kew MC (2005) Full genome analysis of hepatitis B virus genotype E strains from South-Western Africa and Madagascar reveals low genetic variability. J Med Virol 77(1):47–52
Kumar S, Tamura K, Nei W (2004) Mega 3: integrated software for molecular evolutionary genetics analysis and sequence alignment. Brief Bioinform 5:150–163
Kurbanov F, Tanaka Y, Fujiwara K, Sugauchi F, Mbanya D, Zekeng L, Ndembi N, Ngansop C, Kaptue L et al (2005) A new subtype (subgenotype) Ac (A3) of hepatitis B virus and recombination between genotypes A and E in Cameroon. J Gen Virol 86(7):2047–2056
Lavanchy D (2005) Worldwide epidemiology of HBV infection, disease burden, and vaccine prevention. J Clin Virol 34:S1–S3
Liu CJ, Lo SC, Kao JH (2006) Transmission of occult hepatitis B virus by transfusion to adult and pediatric recipients in Taiwan. J Hepatol 44:39–46
Mello FC, Souto FJ, Nabuco LC, Villela-Nogueira CA, Coelho HS, Franz HC, Saraiva JC, Virgolino HA, Motta-Castro AR, Melo MM, Martins RM, Gomes SA (2007) Hepatitis B virus genotypes circulating in Brazil: molecular characterization of genotype F isolates. BMC Microbiol 7:103
Minuk GY, Sun D-F, Uhanova J, Zhang M, Caouette S, Nicolle LE, Gutkin A, Doucette K, Martin B, Giulivi A (2005) Occult hepatitis B virus infection in a North American community-based population. J Hepatol 42:480–485
Moraes MT, Gomes SA, Niel C (1996) Sequences analysis of pre-S/S gene of hepatitis B virus strain of genotypes A, D, and F isolated in Brazil. Arch Virol 14:1767–1773
Motta-Castro ARC, Martins RMB, Yoshida CFT, Teles SA, Paniago AM, Lima KMB, Gomes SA (2005) Hepatitis B virus infection in isolated Afro-Brazilian communities. J Med Virol 77:188–193
Mulders MN, Venard M, Njayou M, Edorth AP, Bola AO, Muller CP (2004) Low genetic diversity despite hyperendemicity of hepatitis B virus genotype E throughout West Africa. J Infect Dis 190:400–408
Niel C, Moraes MTB, Gaspar AMC, Yoshida CFT, Gomes SA (1994) Genetic diversity of hepatitis B virus strains isolated in Rio de Janeiro, Brazil. J Med Virol 44:180–186
Noborg U, Gusdal A, Horal P, Linh M (2000) Levels of viremia in subjects with serological markers of past or chronic hepatitis B virus infection. Scand J Infect Dis 32:249–252
Norder H, Courouce AM, Magnius LO (1994) Complete genomes, phylogenetic relatedness, and structural proteins of six strains of the hepatitis B virus, four of which represent two new genotypes. Virology 198:489–503
Norder H, Courouce A-M, Coursaget P, Echevarria JM, Lee S-D, Mushahwar IK, Robertson BH, Locarnini S, Magnius LO (2004) Genetic diversity of hepatitis B virus strains derived worldwide: genotypes, subgenotypes, and HBsAg subtypes. Intervirology 47:289–309
Olinger CM, Venard V, Njayou M, Oyefolu AOB, Maiga I, Kemp AJ, Omilabu SA, Faou A, Muller CP (2006) Phylogenetic analysis of the precore/core gene of hepatitis B virus genotypes E and A in West Africa: new subtypes, mixed infections and recombinations. J Gen Virol 87:1163–1173
Pas SD, Niesters HG (2002) Detection of HBV DNA using real time analysis. J Clin Virol 25(1):93–94
Quintero A, Dm Martinez, Alarcon de Noya B, Costaglioga A, Urbina L, Gonzalez N, Liprandi F, Castro de Guerra D, Pujo FH (2002) Molecular epidemiology of hepatitis B virus in Afro-Venezuelan populations. Arch Virol 147:1829–1836
Salas A, Richards M, Lareu M-V, Scozzari R, Coppa A, Torroni A, Macaulay V, Carracedo A (2004) The African diaspora: mitochondrial DNA and the Atlantic slave trade. Am J Hum Genet 74:454–465
Scaglioni PP, Melegari M, Wands JR (1997) Biologic properties of hepatitis B viral genomes with mutations in the precore promoter and precore open reading frame. Virology 233:374–381
Sitnik R, Rebello PJR, Bertolini DA, Bernardini AP, da Silva LC, Carrilho FJ (2004) Hepatitis B virus genotypes and precore and core mutants in Brazilian patients. J Clin Microbiol 42:2455–2460
Sugauchi F, Kumada H, Acharya SA, Shrestha SM, Gamutan MTA, Khan M, Gish RG, Tanaka Y et al (2004) Epidemiological and sequence differences between two subtypes (Ae and Aa) of hepatitis B virus genotype A. J Gen Virol 85:811–820
Tabor E, Bayeley AC, Caims J, Pelleu L, Gerety RJ (1985) Horizontal transmission of hepatitis B virus among children and adults in five rural villages in Zambia. J Med Virol 15:113–120
Tanaka Y, Hasegawa I, Kato T, Orito E, Hirashima N, Acharya SK, Gish RG, Kramvis A, Kew MC et al (2004) A case-control study for differences among hepatitis B virus infections of genotype A (subtypes Aa and Ae) and D. Hepatology 40(3):747–755
Thakur V, Kazim SN, Guptan RC, Malhotra V, Sarin SK (2003) Molecular epidemiology and transmission of hepatitis B virus in close family contacts of HBV-related chronic liver disease patients. J Med Virol 70:520–528
Torbenson M, Thomas DL (2002) Occult hepatitis B. Lancet 2:479–486
Wang JT, Wang TH, Sheu JC (1991) Detection of hepatitis B virus DNA by polymerase chain reaction in plasma of volunteer blood donors negative for hepatitis B surface antigen. J Infect Dis 163:397–399
Yoshikawa A, Gotanda Y, Minegishi K, Taira R, Hino S, Tadokoro K, Mizoguchi H (2007) Lengths of hepatitis B viremia and antigenemia in blood donors: preliminary evidence of occult (hepatitis B surface antigen-negative) infection in the acute stage. Transfusion 47:1162–1171
Acknowledgments
The authors thank the nucleotide sequencing platform of the PDTIS program from FIOCRUZ. Dr. Alan Kay is acknowledged for critical reading of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Nucleotide sequence data reported are available in the DDBJ/EMBL/GenBank databases under the accession numbers EF547828 to EF547858 and FJ174794 to FJ174800.
Rights and permissions
About this article
Cite this article
Motta-Castro, A.R.C., Martins, R.M.B., Araujo, N.M. et al. Molecular epidemiology of hepatitis B virus in an isolated Afro-Brazilian community. Arch Virol 153, 2197–2205 (2008). https://doi.org/10.1007/s00705-008-0237-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00705-008-0237-0