Abstract
Twelve nasal swabs were collected from yearling horses with respiratory distress and tested for equid herpesvirus 1 (EHV-1) and equid herpesvirus 4 (EHV-4) by real-time PCR targeting the glycoprotein B gene. All samples were negative for EHV-1; however, 3 were positive for EHV-4. When these samples were tested for EHV-2 and EHV-5 by PCR, all samples were negative for EHV-2 and 11 were positive for EHV-5. All three samples that were positive for EHV-4 were also positive for EHV-5. These three samples gave a limited CPE in ED cells reminiscent of EHV-4 CPE. EHV-4 CPE was obvious after 3 days and was characterised by syncytia. None of the samples produced cytopathic effect (CPE) on African green monkey kidney (Vero) cells or hamster kidney (BSR) cells. Four of the samples, which were positive in the EHV-5 PCR, produced CPE on rabbit kidney (RK13) cells and equine dermis (ED) cells. EHV-5 CPE on both cell lines was slow and was apparent after four 7-day passages. On RK13 cells, the CPE was characteristic of equid herpesvirus, with the formation of syncytia. However, in ED cells, the CPE was characterised by ring-shaped syncytia. For the first time, a case of equine respiratory disease involving dual infection with EHV-4 and EHV-5 has been reported in Queensland (Australia). This was shown by simultaneously isolating EHV-4 and EHV-5 from clinical samples. EHV5 was recovered from all samples except one, suggesting that EHV5 was more prevalent in young horses than EHV2.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Respiratory diseases of horses in Australia have been mainly attributed to equid herpesviruses, adenoviruses and rhinoviruses [4, 5, 16, 18, 23, 27, 40]. Among the former, only two types have demonstrated pathogenicity in susceptible horses. Equid herpesvirus 1 (EHV-1), a member of the subfamily Alphaherpesvirinae, has been isolated and characterised from respiratory and abortion cases and neurological disorders [11, 24, 33, 36, 41]. Another member of the Alphaherpesvirinae, equid herpesvirus 4 (EHV-4) has been linked with respiratory cases and rarely with abortion [2]. Equid herpesvirus 2 (EHV-2), a member of the subfamily Gammaherpesvirinae, is classified as an equid herpesvirus of unknown pathogenic role. However, there have been reports of a pathogenic role for EHV-2 as it has been isolated from cases of respiratory disease [22, 30, 39] and keratoconjunctivitis [12, 29]. Equid herpesvirus 5 (EHV-5) is also a gammaherpesvirus of unknown pathogenic role. The similarity to EHV-2 suggests a similar role for EHV-5; however, this has not been proven as yet. EHV-2 and EHV-5 are ubiquitous and have been isolated from healthy as well as diseased horses in Australia and elsewhere [3, 15, 16, 23, 38]. The prevalence of these two members of the Gammaherpesvirinae in Australia was shown to be 31% for EHV-2 and 16% for EHV-5 [35], which is low compared to figures in other parts of the world. In a study carried out in New Zealand, Dunowska et al. [15] isolated EHV-5 on numerous occasions from apparently healthy foals and concluded that the foals were harbouring either a latent or persistent infection.
Some reports have suggested that EHV-2 plays a predisposing and/or reactivating role for pathogenic members of the Alphaherpesvirinae such as EHV-1 and EHV-4 [16, 21, 34, 45] or bacterial pathogens such as Streptococcus zooepidemicus, Rhodococcus equi and Streptococcus equi [28, 31]. Banbura et al. [6] even speculated that EHV-2 had played a role in determining the severity of respiratory disease and neurological disease caused by bacterial infections in three horses. EHV-2 has been isolated in conjunction with EHV-1 [30] but not with EHV-4. In a study carried out in Western Australia in 2000, Wilcox and Raidal [46] isolated EHV-2 in conjunction with EHV-5 in some horses. They also isolated EHV-1 in combination with EHV-5; however, the EHV-1 occurred only in peripheral blood mononuclear cells (PBMC) and not in nasal swabs, from which only EHV-5 was isolated. They concluded that the presence of EHV-5 in nasal secretions was not a sign of persistent infection. They did not isolate EHV-4 in combination with EHV-5, though in a few samples they isolated EHV-1 or EHV-4 with EHV-2. There are no reports of EHV-5 isolation in conjunction with EHV-4. In a study of horses with respiratory disease conducted by Dynon et al. [19], nasal swabs were simultaneously PCR positive for EHV-2, EHV-4 and EHV-5; however, only EHV-4 was isolated.
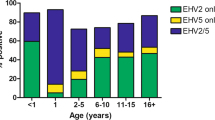
There have been reports of slowly cytopathic equine herpesviruses or equine cytomegaloviruses (ECM) in Queensland in the past, which may have involved EHV-2 or EHV-5 or both [4, 5, 23]. These reports established the infection rate of ECM in horses in Queensland at 63%. However, no relationship was established between isolation of these viruses and disease as they were present in healthy horses as well. In recent years, there has been very little research on equine respiratory disease in Queensland. Wang et al. [44] described EHV-5 as a ubiquitous virus in a horse population in Western Australia. They estimated the prevalence of EHV-5 alone in horses at 89%. Based on their findings they concluded that EHV-5 played no role in respiratory disease of horses. They also detected by PCR simultaneously EHV-5 and EHV-4 in one foal out of 141 and none in another group of 131 horses.
The objective of this study is to investigate the role of equine herpesviruses in respiratory disease in yearlings. In this paper, we describe a case of respiratory disease in which EHV-5 was isolated, either alone or in conjunction with EHV-4, from nasal discharge. Using a gel based PCR for EHV-5 described by Holloway et al. [25] and a real-time PCR for EHV-4 detection described by Diallo et al. [14], we screened 12 samples from horses with a respiratory condition, and the results are reported in this study.
Materials and methods
Samples and reference strains
Nasal swabs were collected from 12 yearling horses, of which 9 presented with nasal discharge. The swabs were then placed in 3 ml virus transport medium made of sucrose (200 mM), potassium di-hydrogen orthophosphate (4 mM), di-potassium hydrogen orthophosphate (7 mM), sodium glutamate (5 mM), bovine serum albumin (10 mg/ml), penicillin (0.1 IU/ml), streptomycin (0.1 μg/ml) and fungizone (0.002 μg/ml) and transported to the laboratory. Samples were frozen at −20°C if not transferred to the laboratory immediately; however, immediate freezing of samples was not always possible, as the veterinarian collected the samples while doing his daily rounds of stables.
Reference strains EHV-1 438/77, EHV-2 86/67, EHV-4 405/76 and EHV-5 2.141 were provided by the Centre for Equine Virology, University of Melbourne (Courtesy of Dr Carol Hartley).
Case study
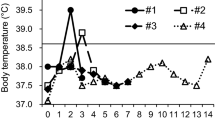
The clinical observations are presented in Table 1. The most prevalent clinical signs were respiratory distress, coughing and nasal discharge. Three horses did not exhibit any clinical signs, while the remaining nine horses presented these symptoms at the time of the study. In three horses with more severe signs, muco-purulent discharge and coughing were observed.
Samples were collected during or just after a horse event in 2006 where there was a great deal of horse movement. Six horses (#1, 2, 3, 5, 6, 7) were from the same stud, and of these, five (2, 3, 5, 6, 7) presented with clinical signs and were sampled during the event. Another horse (#10), originally from another stud, was accommodated with the six horses at the event and was sampled after the event upon return to its original stable, where it was accommodated with two other horses (#9 and 11) that presented with similar signs and were sampled at the same time. Another horse from the same region, but a different stable (horse # 12), was sampled at the same period.
Except for one horse (# 8), which was from another region and which had never been to the event, all of the horses were in contact with many other horses at the horse event.
Virus isolation
The swabs were vortexed for 15 s in the virus transport medium. The suspensions were filtered through 0.45-μm filters, and 400 μl was inoculated onto green monkey kidney (Vero) cells, rabbit kidney (RK13) cells, baby hamster kidney (BSR) cells and equine dermis (ED) cells. Cells were checked every day for cytopathic effect (CPE). Five passages were carried out for each sample, and if no CPE was visible after the fifth passage, the sample was considered negative.
Virus for further testing was grown in Roux flasks and harvested when the monolayer was 90% destroyed. The cells were disrupted by three cycles of freeze-thawing. The virus suspension was centrifuged at 1,900×g for 5 min to remove cell debris. The resulting suspension was centrifuged at 20,000×g for 2 h [42]. The virus pellet was resuspended in 2 ml of TE buffer. Further purification of the virus was performed by centrifuging the viral suspension through a 25% sucrose cushion at 23,000×g for 2 h. The resulting pellet was resuspended in 2 ml Tris–EDTA buffer, pH 7.4.
Polymerase chain reaction
All samples were tested for EHV-1, EHV-2, EHV-4 and EHV-5 by PCR.
The swabs were vortexed for 15 sec in the virus transport medium, and 200 μl of the suspension was used for DNA extraction using a QIAamp DNA Mini Kit (QIAGEN, Melbourne) according to the manufacturer’s recommendations.
Virus grown on cells also was used for DNA extraction. Viral DNA was extracted from purified viral suspensions using a QIAamp DNA Mini Kit. The resulting DNA was used as template for the PCRs.
EHV-1 real-time PCR. An EHV-1 real-time PCR targeting the glycoprotein B gene was used as described previously [13].
EHV-4 real-time PCR. An EHV-4 real-time PCR targeting the glycoprotein B gene was used as described previously [14].
EHV-2 and EHV-5 PCRs. Conventional PCRs targeting the respective glycoprotein B genes were used for EHV-2 and EHV-5 detection.
The EHV-2 PCR was derived from a method described by Telford et al. [42]. This was a nested PCR; however, in order to decrease chances of contamination, the PCR was modified to be performed as a single-round PCR. In order to improve the specificity of the single-round PCR, the primers were slightly modified and were as follows:
Forward (pos 33,717 to 33,736) 5′-GCC AGT GTC TGCCAA GTT GAT A-3′
Reverse (pos 34,159 to 34,138) 5′-CAT GGT CTC GAT GTC AAA CAC G-3′
The resulting amplicon is 444-bp long (data not shown).
The EHV-5 PCR was as described by Holloway et al. [25]. The resulting amplicon has a size of 293 bp.
Results
Virus isolation
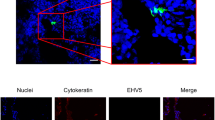
Virus isolation results are summarised in Table 1. No CPE was observed in either Vero or BSR cells. Samples NS-4, NS-5, NS-7 and NS-10 grew in RK13 cells after four passages. The CPE in RK13 cells appeared on days 2–3 of the fourth passage. The CPE was characterised by rounded cells and syncytia. The cell monolayer was fully destroyed after 3 days once the CPE had started (data not shown). These samples also grew in ED cells. CPE produced by samples NS-4, NS-5 and NS-7 on ED cells was characterised by ring-shaped syncytial formations as described by Fong and Hsiung [20]. Unlike the RK13 cells, cells were not rounded at first; however, the monolayer displayed areas of cell degeneration bordered by a ring of dead cells. The cells contained within the ringed area were rounded. These cells formed syncytia only after 2 weeks of incubation at 37°C and were destroyed after 3 weeks (data not shown). Virus isolated from RK-13 and ED was confirmed to be EHV-5 by PCR.
Reference strain EHV-5 2.141 grew only in ED cells, giving a ring-shaped CPE. It did not grow in RK13 after five passages.
Electron microscopy showed a typical herpesvirus for all supernates harvested from RK13 cells exhibiting CPE; however, there were no viral particles observed from ED cells, even when a ring-shaped CPE was observed.
Samples NS-9, NS-10 and NS-11 presented 1-2 foci of apparent CPE in ED cells. However, the progression of the CPE was limited as it did not lead to a full destruction of the monolayer. Cells became rounded and refractile within 3 days post-inoculation, but after 7 days the monolayer looked full and normal. This did not agree with the real-time PCR and gel-based PCR results, in which all three samples were positive for EHV-4 and EHV-5.
Polymerase chain reaction
PCR results are presented in Table 1.
All nasal swabs were negative for EHV-1 real-time PCR targeting the glycoprotein B gene and EHV-2 PCR targeting the glycoprotein B gene.
EHV-4 real time. Of the 12 samples, 3 were positive for EHV-4 real-time PCR. Samples NS-9, NS-10 and NS-11 had mean C t values of 22, 32 and 25, respectively (Table 1). The positive control EHV-4 405/76 had a mean C t of 29 (Table 1). It was also of interest to note that one of the samples had C t values of 37 and 0 (the sample was tested twice in duplicate). This suggested that there were low amounts of EHV-4 DNA in the sample, as the limit of detection of the real-time PCR was set at C t = 38 [14].
EHV-5 PCR. All samples except sample NS-8 were positive for the glycoprotein B PCR of EHV-5. They all had the expected 293-bp amplicon of the glycoprotein B gene of EHV-5 (Fig. 1).
EHV-5 glycoprotein B gene PCR [25]: lane 1 and 16 molecular weight marker ΦX174 RF DNA Hae III (Fermentas); lane 2 negative control; lane 3 NS-1; lane 4 NS-2; Lane 5 NS-3; lane 6 NS-4; lane 7 NS-5; lane 8 NS-6; lane 9 NS-7; lane 10 NS-8; lane 11 NS-9; lane 12 NS-10; lane 13 NS-11; lane 14 NS-12; lane 15 EHV-5 2.141 (reference strain)
Discussion
The findings in this study support the findings of Wang et al. [43], who showed that, unlike in other countries [9, 15, 32], EHV-5 was more prevalent in horse populations in Australia than EHV-2. Of the 12 nasal swabs tested, 11 were EHV-5 PCR positive, while none were positive for EHV-2 PCR. It is also possible that these observations are due to the fact that EHV-5 is more likely to infect older horses than EHV2, as suggested by Dunowska et al. [15], Nordengrahn et al. [32] and Bell et al. [7]. However, unlike the study of Wang et al. [44], where the horses tested were healthy, in this study, EHV-5 was isolated from diseased horses, and this observation may have been biased towards diseased animals. Furthermore, EHV-5 may have played a predisposing role in the onset of respiratory disease; however, there is little evidence to assign such role to EHV-5.
This is the first time a case of equine respiratory disease involving dual infection with EHV-4 and EHV-5 has been reported in Queensland. The epidemiological data suggest that these horses may have contracted the respiratory disease during the horse event where there was a great deal of horse movement, specifically horses of different immune backgrounds were confined in the same area for an extended period of time. Samples (nasal discharges) NS-9, NS-10 and NS-11 were positive for EHV-5 PCR and EHV-4 real-time PCR as well. Moreover, EHV-4 was isolated from these samples when ED cells were inoculated. The results obtained for NS-9, and NS-11 were similar to those of Dynon et al. [19], who have managed to isolate only EHV-4 from a horse that was EHV-4, EHV-5 and EHV-2 PCR positive. They were unable to simultaneously isolate EHV-4, EHV-2 and EHV-5, even though the sample was triple positive by PCR. This once again underlines the superior sensitivity of PCR compared to conventional virus isolation from clinical samples, especially when the storage and/or transport of samples to the laboratory may have been inadequate. However, both EHV-4 and EHV-5 were isolated from NS-10 when RK13 and ED cells were inoculated. This is the first case of isolation of EHV-5 and EHV-4 from the same clinical sample. The significance of this virus isolation is uncertain, as the pathogenic role of EHV-5 is not well defined. However, the fact that EHV-4, a known respiratory pathogen of horses, and EHV-5 were isolated simultaneously in 3 out of 12 tested nasal discharges may suggest that EHV-5 was playing a predisposing role in this infection. This observation warrants further investigations to establish the role of these EHV-5 strains in pathogenicity. EHV-2, a member of the subfamily Gammaherpesvirinae that is closely-related to EHV-5, has been isolated in conjunction with other herpesviruses, in particular EHV-1 [30, 44, 46]. These authors reported cases of combined infection with members of the Alphaherpesvirinae (EHV-1) and Gammaherpesvirinae (EHV-2). However, they did not isolate EHV-5 from animals that had an ongoing infection due to an alphaherpesvirus. Wang et al. [44] have detected EHV-5 and EHV-4 from a nasal swab of one foal, using PCR; however, they did not attempt virus isolation. In another study, Bell et al. [7] isolated EHV-4 from nasal swabs in foals with respiratory disease, but never concomitantly with gammaherpesviruses, even though the authors have shown that EHV-2 and EHV-5 were ubiquitous in the cohort of horses studied. In our case, EHV-5 was detected in nasal discharge of horses with respiratory disease and also from 3 healthy horses. The isolation of EHV-4 in 3 out of the 12 nasal swabs, which were from the three horses presenting with respiratory distress, is significant and provides circumstantial evidence that EHV-4 may have been responsible for the respiratory disease. This is further supported by the fact that it was not recovered from the remaining eight nasal discharges that were also EHV-4 real-time PCR negative, suggesting that there was no EHV-4 DNA present in those samples, as the real-time PCR can detect as few as four copies of the target gene [14]. However, it is also possible that EHV-4 DNA was present in all samples but might have been degraded, as suggested by the results of the EHV-4 real-time PCR for sample NS-4, where one duplicate gave a C t value of 37, while the other duplicate gave a C t value of 0. This may mean that either there were very low amounts of EHV-4 DNA (fewer than four copies) or the DNA was degraded and was not detectable by real-time PCR. As the samples were collected on the veterinarian’s rounds at various stables, the conditions of storage of samples may have been inadequate, which may mean that the DNA may have been degraded by the time the sample reached the laboratory. It is also of interest to note that even though 11 nasal swabs out of 12 were EHV-5 PCR positive, virus was isolated from only four of these samples. This suggested that the virus may have been inactivated by the time the virus isolation was attempted. This is also supported by the fact that in one of the samples EHV-4 was detected by PCR but not cultured. However, this might have been the result of the gammaherpesvirus inhibitory effect on alphaherpesvirus, as was observed by Wang et al. [44], who detected EHV-1 and EHV-5 simultaneously on eight occasions by PCR but managed to isolate EHV-1 only on one occasion by co-cultivation. They suggested that the rapid replication of EHV-5 may have hindered that of EHV-1. This conclusion was based on just one observation, with the other seven attempts of co-cultivation of either virus being unsuccessful. Previous studies carried out by Dutta et al. [17] and Welch et al. [45] have highlighted the inhibitory effect of EHV-2 replication on EHV-1. These authors suggested that gammaherpesviruses may have an inhibitory effect on the recovery of other equid herpesviruses, especially EHV-1, and as a result, they were not able to recover EHV-1 from samples that were PCR positive; however, this could also be due to the virus being inactivated. In our study, we have also observed a similar phenomenon, characterised by the limited growth of EHV-4 in samples NS-9, NS-10 and NS-11 and the total inhibition of EHV-4 for sample NS-4. However, the growth of EHV-5 was slower than that of EHV-4; therefore, there may be another underlying interaction between the two viruses which affects the replication of EHV-4.
Purewal et al. [34], Welch et al. [45], Fortier et al. [21], Jolly et al. [28] and Nordengrahn et al. [31] have linked EHV-2 with Streptococcus zooepidemicus, Rhodococcus equi, and S. equi. In our study, we could not establish a link between gammaherpesvirus infection and bacterial colonization, as all swabs were transported to the laboratory in virus transport medium containing antibiotics and therefore unsuitable for bacteriology testing. Further work is required to establish the pathogenicity of these particular isolates in healthy susceptible yearlings.
In these reported cases, EHV-5 was isolated from nasal discharge, which might suggest that the virus was replicating in the upper respiratory tract. Similar observations were made by Wilks and Studdert [47] where the buffy coat of a horse with respiratory disease yielded strain EHV-5 M2BO and on another occasion where EHV-5 strain 253/72 was isolated from imported horses [1]. This may support the predisposing role of EHV-5, which has already been suggested by other authors for EHV-2 a closely related herpesvirus [6, 8, 30, 31, 37]. These observations warrant further characterisation of these EHV-5 isolates.
In our hands, EHV-5 grew readily in RK13 cells, while in equine cells (ED), virus growth was muted and showed an atypical CPE. Even though the CPE observed was reminiscent of the CPE described by Fong and Hsiung [20] in ED and RK13 cells, the CPE we observed was more marked in RK13 cells, where the monolayer was destroyed within 3 days, while in ED cells, even after five passages, the cell monolayer was not destroyed, and the monolayer showed signs of rounded cells surrounded by a ring of dead cells. Similar observations were made by Hsiung et al. [26], who described a ring-shaped CPE in ED cells due to an equine herpesvirus. They compared the virus to other herpesviruses, with specific reference to cytomegalovirus, a gammaherpesvirus of humans. It was also of interest to note that when the supernatant from inoculated ED cells with ring-shaped CPE was examined by electron microscopy, no viral particles were observed, suggesting that the virus might be cell associated. In fact, when DNA from such cells was extracted and subjected to PCR, EHV-5 DNA was detected (results not shown).
Reference strain EHV-5 2.141 was different from field isolates. It did not grow in RK13 cells, while all four field strains grew readily in RK13 cells. However, in ED cells, all four isolates and the reference strain gave the same type of CPE: a ring-shaped CPE. The difference in growth in different cell types may be due to differences in virus cell entry and replication, which may be determined by the difference in glycoprotein B of these isolates. It has been shown that glycoprotein B of alphaherpesviruses is essential for entry of the virus into the cell. In an elegant experiment using a glycoprotein B mutant of herpes simplex virus (HSV), Cai et al. [10] showed that the role of glycoprotein B lies principally in fusion, not in the binding of the virus to the cell.
This is the first report of dual equine herpes viral infection in yearlings due to EHV-4 and EHV-5 in Queensland. It is also the first time that EHV-4 and EHV-5 were simultaneously isolated from clinical samples. Furthermore, this study has added some more insight into the potential role of EHV-5 as a predisposing factor for herpesvirus infection due to EHV-4. Further characterisation of these isolates will help answer questions relating to the potential of EHV-5 to cause respiratory disease.
References
Agius CT, Nagesha HS, Studdert MJ (1992) Equine herpesvirus 5: comparisons with EHV-2 (equine cytomegalovirus), cloning, and mapping of a new equine herpesvirus with a novel genome structure. Virology 191:176–186
Allen GP, Bryans JT (1986) Molecular epizootiology, pathogenesis and prophylaxis of equine herpesvirus 1 infections. Progr Vet Microbiol Immunol 2:78–144
Bagust TJ (1971) The equine herpesviruses. Vet Bull 41:79–82
Bagust TJ (1972) A review of viral infections in horses. Aust Vet J 48:520–523
Bagust TJ, Pascoe RR (1972) Studies on equine herpesviruses 3. The incidence in Queensland of three different equine herpesvirus infections. Aust Vet J 48:47–53
Banbura MW, Chmielewska A, Tucholska A, Sendecka H, Rzewuska M, Dzieciatkowski T (2004) Outbreak of equine herpesvirus type 2 (EHV–2) infections in relation to respiratory or neurological symptoms. Med Weter 60:496–499
Bell SA, Balasuriya UBR, Gardner IA, Barry PA, Wilson WD, Ferraro GL, MacLachlan NJ (2006) Temporal detection of equine herpesvirus infections of a cohort of mares and their foals. Vet Microbiol 116:249–257
Borchers K, Wolfinger U, Goltz M, Broll H, Ludwig H (1997) Distribution and relevance of equine herpesvirus 2 (EHV-2) infections. Arch Virol 142:917–928
Borchers K, Frölich K, Ludwig H (1999) Detection of equine herpesvirus types 2 and 5 (EHV-2 and EHV-5) in Przewalski’s wild horses. Arch Virol 144:771–780
Cai W, Gu B, Person S (1988) Role of glycoprotein B of herpes simplex virus type 1 in viral entry and cell fusion. J Virol 62:2596–2604
Campbell TM, Studdert MJ (1983) Equine herpesvirus type 1 (EHV-1). Vet Bull 53:135–146
Collinson PN (1994) Isolation of equine herpesvirus type 2 (equine gamma herpesvirus 2) from foals with keratoconjonctivitis. J Am Vet Med Assoc 205:329–331
Diallo IS, Hewitson G, Wright L, Rodwell BJ, Corney BG (2006) Detection of equine herpesvirus type 1 using a real-time polymerase chain reaction. J Virol Methods 131:92–98
Diallo IS, Hewitson G, Wright L, Rodwell BJ, Corney BG (2007) Multiplex real-time PCR for differentiation of Equid Herpesvirus type 1 and Equid Herpesvirus type 4. Vet Microbiol 123:93–103
Dunowska M, Meers J, Wilks CR (1999) Isolation of equine herpesvirus type 5 in New Zealand. NZ Vet J 47:44–46
Dunowska M, Wilks CR, Studdert MJ, Meers J (2002) Equine respiratory viruses in foals in New Zealand. N Z Vet J 50:140–147
Dutta SK, Myrup AC, Thaker SR (1986) In vitro interference between equine herpesvirus types 1 and 2. Am J Vet Res 47:747–750
Duxbury AE, Oxer DT (1968) Isolation of equine rhinopneumonitis from an epidemic of acute respiratory disease in horses. Aust Vet J 44:58–63
Dynon K, Black WD, Ficorelli N, Hartley CA, Studdert MJ (2007) Detection of viruses in nasal swabs samples from horses with acute, febrile, respiratory disease using virus isolation, polymerase chain reaction and serology. Aust Vet J 85:46–50
Fong CKY, Hsiung GD (1972) Development of an equine herpesvirus in two cell culture systems: light and electron microscopy. Infect Immun 6:865–876
Fortier G, Pitel PH, Maillard K, Pronost S (2003) Herpes virus en pathologie equine: connaissances actuelles et perspectives. Bull Acad Vet France 156:13–24
Fu ZF, Robinson AJ, Horner GW et al (1986) Respiratory disease in foals and epizootiology of equine herpesvirus type 2 infection. N Z Vet J 34:152–155
Harden TJ, Bagust TJ, Pascoe RR, Spradbrow PB. Studies on equine herpesviruses 5: (1974) Isolation and characterisation of slowly cytopathic equine herpesviruses in Queensland. Aust Vet J 50: 483–488
Hartley WJ, Dixon RJ (1979) An outbreak of foal perinatal mortality due to equine herpesvirus type1: pathological observations. Equine Vet J 11:215–218
Holloway SA, Lindquester GJ, Studdert MJ, Drummer HE (1999) Identification and characterisation of equine herpesvirus 5 glycoprotein B. Arch Virol 144:287–307
Hsiung GD, Fischman FR, Fong CKY, Green RH (1969) Characterisation of a cytomegalovirus-like virus isolated from spontaneously degenerated equine kidney culture. Proc Soc Exp Biol Med 130:80–84
Johnston KG, Hutchins DR (1967) Suspected adenovirus bronchitis in Arab foals. Aust Vet J 43:600
Jolly PD, Fu ZF, Robinson AJ (1986) Viruses associated with respiratory disease of horses in New Zealand. N Z Vet J 34:46–50
Kershaw O, von Oppen T, Glitz F, Deegen E, Ludwig H, Borchers K (2001) Detection of equine herpesvirus type 2 (EHV–2) in horses with keratoconjonctivitis. Virus Res 80:93–99
Murray MJ, Eichorn ES, Dubovi EJ, Ley WB, Cavey DM (1996) Equine herpesvirus type 2: prevalence and seroepidemiology in foals. Equine Vet J 28:432–436
Nordengrahn A, Rusvai M, Merza M, Ekstrom J, Morein B, Belák S (1996) Equine herpesvirus type 2 (EHV-2) as a predisposing factor for Rhodococcus equi pneumonia in foals: prevention of the bifactorial disease with EHV2 immunostimulating complexes. Vet Microbiol 51:55–68
Nordengrahn A, Merza M, Ros C, Lindholm A, Pálfi V, Hannant D, Belák S (2002) Prevalence of equine herpesvirus type 2 and 5 in horse populations by using type-specific PCR assays. Vet Res 33:251–259
O’Callaghan DJ, Gentry GA, Randall CC (1983) The equine herpesviruses. In: Roizman B (ed) The herpesviruses. Plenum Press, New York, pp 215–318
Purewal AS, Smallwood AV, Kaushal A, Adegboye D, Edington N (1992) Identification and control of the cis-acting elements of the immediate early gene of equid herpesvirus type 1. J Gen Virol 73:513–519
Reubel GH, Crabb BS, Studdert MJ (1995) Diagnosis of equine gammaherpesvirus 2 and 5 infections by polymerase chain reaction. Arch Virol 140:1049–1060
Sabine M, Feilen C, Herbert L, Jones RF, Lomas SW, Love DN, Wild J (1983) Equine herpesvirus abortion in Australia 1977 to 1982. Equine Vet J 15:366–370
Schlocker N, Gerber-Bretscher R, Fellenberg R (1995) Equine herpesvirus 2 in pulmonary macrophages of horses. Am J Vet Res 56:749–754
Studdert MJ, Turner AJ, Peterson JE (1970) Isolation and characterisation of equine rhinopneumonitis virus and other equine herpesviruses from horses. Aust Vet J 46:83–89
Studdert MJ (1974) Comparative aspects of equine herpesviruses. Cornell Vet 64:94–122
Studdert MJ (1996) Virus infections of equines. In: Studdert MJ (ed) Virus infections of vertebrates, 6th edn. Elsevier, Amsterdam, pp 47–60
Studdert MJ, Hartley CA, Dynon K, Sandy JR, Slocombe RF, Charles JA, Milne ME, Clarke AF, El-Hage C (2003) Outbreak of equine herpesvirus type 1 myeloencephalitis: new insights from virus identification by PCR and the application of an EHV-1-specific antibody detection ELISA. Vet Record 153:417–423
Szilagyi JF, Cunnigham C (1991) Identification and characterisation of a novel non-infectious herpes simplex virus-related particle. J Gen Virol 72:661–668
Telford EA, Studdert MJ, Agius CT, Watson MS, Aird HC, Davison AJ (1993) Equine herpesviruses 2 and 5 are gamma-herpesviruses. Virology 195: 492–499
Wang L, Raidal SL, Pizzirani A, Wilcox GE (2007) Detection of respiratory herpesvirus in foals and adult horses determined by nested multiplex PCR. Vet Microbiol 121:18–28
Welch HM, Bridges CG, Lyon AM, Griffiths L, Edington N (1992) Latent equid herpesvirus 1 and 4: detection and distinction using the polymerase chain reaction and co-cultivation from lymphoid tissues. J Gen Virol 73:261–268
Wilcox GE, Raidal S (2000) Role of viruses in respiratory disease. A Rural Industries Research and Development Corporation report
Wilks CR, Studdert MJ (1974) Equine herpesviruses. 5. Epizootiology of slowly cytopathic viruses in foals. Aust Vet J 50:438–442
Acknowledgments
The authors wish to thank Dr. C. Hartley (Centre for Equine Virology) for providing them with EHV-2, EHV-4 and EHV-5 reference strains. The authors would also like to thank Dr. T. Mahony, J. Taylor and N. Moody (DPI&F) for their critical comments on the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Diallo, I.S., Hewitson, G.R., de Jong, A. et al. Equine herpesvirus infections in yearlings in South-East Queensland. Arch Virol 153, 1643–1649 (2008). https://doi.org/10.1007/s00705-008-0158-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00705-008-0158-y