Abstract
Patients with Autism Spectrum Disorder (ASD) need to be provided with behavioral, psychological, educational, or skill-building interventions as early as possible. Cognitive Behavior Therapy has proven useful to manage such problems. There is also growing evidence on the usefulness of Virtual Reality Therapy (VRT) in treating various functional deficits in ASD. This exploratory study is aimed at assessing the changes in cognitive functions in children with ASD, and the putative subtending neurophysiological mechanisms, following the provision of rehab training using an innovative VRT system. Twenty patients with ASD, aged 6–15 years, were provided with 24 sessions of VRT by using the pediatric module of the BTS NIRVANA System. Neuropsychological and EEG evaluations were carried out before and at the end of the training. After VRT, all patients showed a significant improvement in their cognitive-behavioral problems concerning attention processes, visuospatial cognition, and anxiety. These findings were paralleled by an evident reshape of frontoparietal connectivity in the alpha and theta frequency range. Our study suggests that VRT could be a useful and promising tool to improve ASD neurorehabilitation outcomes. This improvement is likely to occur through changes in frontoparietal network connectivity following VRT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Autism spectrum disorder (ASD) (including Autistic disorder, Asperger’s syndrome, and Pervasive developmental disorder not otherwise specified) is a neurodevelopmental disorder characterized by a variety of symptoms with differing severity, such as difficulties in joint attention and visual contact, fascination with sensorial stimuli, lack of social intent to communicate, and imitative social play (Toth et al. 2006; Brentani et al. 2013; Fuentes et al. 2014; Ogundele 2018). All these symptoms account for the limited capacity in communicating and interacting with other people, restricted interests, and repetitive behaviors, thus negatively affecting functional activities, including school, work, and other areas of life (Park et al. 2019; Diagnostic and Statistical Manual of Mental Disorders 5).
Patients with ASD show often-high levels of anxiety and cognitive deficits, mainly involving attention, executive function, and praxis, negatively affecting their quality of life (Zwick 2017). Consistent with the wide range of cognitive impairments related to the disease (Toth et al. 2006; Brentani et al. 2013; Fuentes et al. 2014; Ogundele 2018), patients with ASD need to receive behavioral, psychological, educational, or skill-building interventions. These interventions include the following: (i) learning life-skills necessary to live independently; (ii) reducing challenging behaviors; (iii) increasing or building upon strengths, and (iv) learning/potentiating social, communication, and language skills.
Cognitive Behavior Therapy (CBT) is a valid strategy to mitigate mood-related symptoms and potentiate cognitive, communicative, sensorimotor, adaptive behavior, and socio-emotional reciprocity abilities (Gaus and Attwood 2018; Ben-Sasson et al. 2009; Edgington et al. 2016; Douglas 2019; Werchan et al. 2018; Sukhodolsky et al. 2013; Wood et al. 2015; Kose et al. 2018). However, there is no clear evidence of CBT’s effectiveness in cognitive domains for young ASD patients, whereas some evidence is available for anxiety reduction following CBT (Leichsenring and Steinert 2017; Hofmann et al. 2012; Walters et al. 2016; Spain et al. 2017). Therefore, innovative and multidisciplinary approaches aimed at targeting cognitive dysfunction in ASD should be welcomed.
Virtual Reality Therapy (VRT) is a new way to deliver a wide range of treatments within a multimodal approach, thus representing a tool that can be implemented within CBT. It consists of a VR environment (VRE), such as computer-based simulations of reality, designed to comprehensively or selectively stimulate different motor and cognitive domains in patients with neurologic (e.g., stroke) or psychiatric disorders, including ASD. There is some evidence of the usefulness of VRT in the treatment of both adults and children with ASD (Bernard-Opitz et al. 2001, Mitchell et al. 2007a, b; Ozonoff and Miller 1995; Wainer and Ingersoll 2011; Mesa-Gresa et al. 2018; De Luca et al. 2018, 2019; Didehbani et al. 2016; Wang and Reid 2013; Rizzo and Buckwater 2004; Kandalaft et al. 2013). The advantage of adopting VRT lies in the fact that an individual can practice difficult or personally challenging social interactions in a less-anxiety-producing platform, i.e., in a VRE (Kandalaft et al. 2013; Maskey et al. 2014; Parsons and Mitchell 2002; Wainer and Ingersoll 2011). Furthermore, VRE can offer patients simple emotion recognition tasks or role-playing scenarios. VRT can provide patients with safe, unlimited, and commonly encountered day-to-day contexts to practice social and or interactive scenarios, allowing for repeated practice in a dynamic, continually changing social context, such as identifying/finding objects, counting, and describing, chasing, or moving items (Kandalaft et al. 2013; Parsons et al. 2005; Wallace et al. 2010). Lastly, VRT is often experienced by children as highly engaging, interactive, motivating, and rewarding (Parsons and Mitchell 2002). One important detail is that the motor, cognitive, and social skills learned in the VRE can be transferred to everyday life interactions by intensive, repetitive, and task-oriented VRT practice (Bellani et al. 2011, Parsons and Cobb 2011; Tzanavari et al. 2015). This practice is also thought to cognitively rehearse the learned motor schemas to enhance motor performance beyond cognitive processes (Kitago and Krakauer 2013).
Despite these premises, there are only a few VRT-based studies focused on reducing anxiety symptoms (Conaughton et al. 2017), improving sensory processing difficulties (Edgington et al. 2016), and ameliorating cognition, affective communication, social skills, and facial emotion perception in young patients with ASD (Weston et al. 2016). Furthermore, the neurophysiological underpinnings of VRT remain only partially elucidated, although a selective effect of VRT has been hypothesized on the brain network activity sustaining cognitive processes (Faria et al. 2016; Petzinger et al. 2013; Fan et al. 2005; Doniger et al. 2018; Wang et al. 2013; Boutros et al. 2015; De Luca et al. 2019).
The present pilot study was aimed at assessing the changes in some aspects of cognitive functioning (including non-verbal fluid intelligence, attention processes, and sensorimotor integration) and anxiety symptoms in children with ASD following a rehab training using an innovative VRT system, i.e., the pediatric module of the BTS NIRVANA System v.2.0 (BTSN) (BTS Bioengineering; Garbagnate Milanese, Italy). Using this device, we provided patients with a semi-immersive VRE in which children had to carry out different motor exercises involving their trunks and limbs and stimulating different cognitive domains.
Furthermore, we aimed at assessing the putative neurophysiological mechanisms subtending the abovementioned changes. We hypothesized that BTSN might target the detrimental long-range networks that are strategic to sustain the above-mentioned cognitive functions.
Materials and methods
Study population and setting
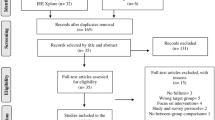
Forty-seven school-aged children affected by ASD and attending the child neuropsychiatry outpatient ambulatory of the IRCCS Centro Neurolesi (Messina, Italy) were screened for study inclusion from January to June 2018.
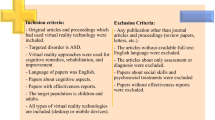
The inclusion criteria were (i) diagnosis of ASD, according to the DSM-V (American Psychological Association 2015); (ii) age range 5–18 years; and (iii) no cognitive therapy within the last six months before enrollment. Exclusion criteria included: (i) severe aggressive, self-directed, and/or hetero-directed behaviors; (ii) severe intellectual disability according to the IQ score ranges on the Wechsler Abbreviated Scale of Intelligence (WASI), so that only children with ASD having a mild to moderate intellectual disability were included in the study; (iii) acute psychiatric condition or a history of neurologic disorders; and (iv) epileptic seizure induced by light stimuli.
Thirty patients met the inclusion/exclusion criteria, and 20 of them (aged 6–15 years; mean ± sd 11 ± 3 years; 13 females and seven males) received the experimental protocol. Indeed, parents of ten children with ASD refused to give informed consent for different personal and work-related reasons.
The local Ethics Committee approved the study (IRCCSME 39/2017), and all patients' caregivers provided their written informed consent to study participation and data publication.
Outcome measures
All patients were assessed before (baseline, T0), immediately after (T1), and one month after (T2) the completion of the VRT training using a specific psychometric battery. This included the Raven’s Colored (RSPM) and Standard Progressive Matrices (RSPM) (Raven et al. 1998) to measure the non-verbal fluid intelligence; the Modified little bell test (MTCM) (Biancardi 1997) to evaluate the attention processes; the Developmental Test of Visual-Motor Integration (VMI) (Beery and Beery 2004) to assess the visual-spatial functions; and the Beck Anxiety Inventory for Youth (BAI-Y), which belongs to the self-report multi-assessment instrument Beck Youth Inventories (Beck et al. 2005) to rate anxiety symptoms. EEG recording in resting conditions at T0 and T1 was also carried out to investigate the neurophysiological changes following the training.
VRT was delivered once daily, three times a week, for eight consecutive weeks (24 sessions, each session lasting about 30–45 min).
Device and procedures
BTSN is a VRE-based medical device specifically designed to rehabilitate patients with neurological disorders complaining of motor and cognitive difficulties. The tool is a movement-based system that provides the patients with interactive VRE, where different audio/video stimuli are presented in different parts of the screen. Indeed, the system is connected to a large projector or screen (i.e., a 2D flat-panel projection system), which reproduces an interactive series of exercises involving trunk and limbs and stimulating different cognitive domains. Moreover, an infrared video camera records the patient’s movements, so he/she can interact with the screen on which a scenario is displayed and perform motor or cognitive activities (related to attention processes, memory, spatial cognition, equilibrium, and motor coordination functions), including identifying/finding objects, counting, and describing, chasing, or moving items.
Rehabilitation exercises with audiovisual stimuli and feedback involve the perceptual-cognitive abilities of patients, increasing motivation. Each activity has different modes and increasing levels of difficulty so that the therapist can use a predefined or new rehabilitation solution, depending on the patient’s needs (Table 1). The data obtained after the training may be recorded and stored, allowing the therapist to evaluate the patient’s progress and modify the rehabilitation program accordingly. The tool has six types of exercise concerning the patient’s modality of interaction in different virtual tasks (Fig. 1): sprites, follows me, hunts, motion, games, and virtual grasping. Sprites allow exploring the available environment with a single or both upper limbs; this is a beneficial method to recover visual-spatial abilities and spatial cognition. Follows me is indicated to stimulate the upper or lower limb and to improve motor coordination. Hunt is meant to improve the attentional processes and ocular-manual coordination. Motion aims to control movement within fixed positions to improve limb and trunk control. Games allow the interaction of multiple patients in a session and a strategy of taking the turn. Grasping permits stimulating the attention processes, motility, and coordination. Other scenarios were designed to reduce the patient's anxiety, with the therapist's support to practice specific techniques (supplementary Table 1).
A subject with ASD while performing cognitive and behavioral exercises in a virtual reality environment in double modality: on the wall and flooring. In particular, the subject can interact with different virtual scenarios to increase specific cognitive abilities and reduce anxiety symptoms. BTS Nirvana screen allows to work on various domains based on attention and sensorimotor processes (including to indicate the objects, naming’s image, colors, fruits, left–right–center spatial exploration with the visual-spatial scanner, the animal’s position in the virtual space, and so on) and to control emotion and anxiety (recognition of emotion and the use of peculiar diaphragmatic breathing techniques)
The participant was invited to interact with various scenarios to perform motor and cognitive tasks and improve the attention processes and spatial cognition. Moreover, we used specific scenarios with three hierarchically graded levels of exposure. We started from the lowest level without direct therapist assistance (i.e., a quiet dog at a distance and/or water that moves with the participant's movement). In the next levels, the therapist supported the participants in practicing techniques and reducing anxiety (including relaxation exercises, breathing exercises, and stimulating thoughts). If the anxiety increased as the scene became demanding, the therapist suggested relaxation and breathing exercises or moving to relaxation scenes, whichever was necessary. Each level was customized to the participant's needs. After the participant was exposed to the third level, the therapist met the participant and his/her caregivers, giving them indications on managing a more stressful situation resembling real life.
EEG processing and analysis
EEG was recorded for at least 10 min in a resting state (to produce a sufficiently long recording and obtain intervals free from artifacts) while the patient was sitting on a comfortable chair in a silent room with a controlled temperature. A standard EEG headset with 19 channels (placed according to the International 10–20 System) wired to a BrainQuick device (Micromed; Mogliano Veneto, Italy) was used. EEG was sampled at 256 Hz, filtered at 1–60 Hz (by Butterworth filters), and referenced to both mastoids. The EEG segments without eye blink and other gross artifacts were subjected to ICA to be further cleaned of artifacts. Then, the pruned data were subjected to wavelet decomposition using Synchronization Likelihood (SL) as a nonlinear measure of interdependence between EEG signals. This allowed for evidencing abnormalities in functional connectivity of brain networks in all EEG sub-bands and full-band EEG (Stam and Dijk 2002; Zou et al. 2008; Rizzi et al. 2009). We adopted such an approach to identify neuronal-network connectivity changes in specific loci and sub-bands, which may not have been detectable in the full-band EEG.
Briefly, we carried out a 4-level wavelet decomposition on each EEG channel in the following frequency bands (Adeli et al. 2007): gamma (30–60 Hz), beta (15–30 Hz), alpha (8–15 Hz), theta (4–8 Hz), and delta (0–4 Hz); omega frequency rage (full range) was also considered. Then, signals were reconstructed in keeping with the Takens theorem (Chan and Tong 2001). Finally, the Fuzzy Synchronization Likelihood (FSL) within and between EEG signals (i.e., EEG signals Xx and Xy obtained from electrodes x and y) from specific regions of interest (ROIs) was computed through averaging the bivariate FSLs (according to FSL-wavelet methodology for the diagnosis of ADHD) (Ahmadlou and Adeli, 2010, 2011; Ahmadlou et al. 2010, 2012). ROIs were categorized into six conventional regions: frontal (F) (Fp1/2, Fz, F3/4, and F7/8), right temporal (rT) (T4/6), left temporal (lT) (T3/5), central (C) (C3/4 and Cz), parietal (P) (P3/P4 and Pz), and occipital (O) (O1/2). Then, 100 EEG signals (20 patients × 5 EEG bands) were obtained and used to extrapolate FSL within and between ROIs in each EEG sub-bands and the whole-band. A 6 × 6 functional connectivity matrix (between all ROIs) in each of the EEG sub-bands was obtained by averaging the bivariate FSL values. Five functional connectivity matrices (one for each of the four sub-bands and the whole-band) for each of the six ROIs (30 functional connectivity matrices overall) were thus obtained.
Statistical analysis
The Kolmogorov–Smirnov test was used to assess the clinical data’s normal distribution (all p > 0.2). Repeated measures ANOVA was calculated to evaluate the significance of clinical outcome changes using the factor time (three levels: T0, T1, and T2). When appropriate, post hoc t tests were applied with Bonferroni correction for multiple comparisons.
The significance of the changes in functional connectivity within each of the EEG bands and the whole EEG frequency range (based on the FSL values) was assessed using repeated-measures ANOVA employing the factors time (two levels: T0 and T1) and ROI (six levels). The connections were more detrimental whether multivariate SLs were lower in the pre- than post-treatment. Finally, we computed the Pearson correlation coefficient as the linear bivariate correlation between the overall clinical improvement and the changes in functional connectivity according to the FSL values within each EEG band and ROI pair. The overall clinical improvement was calculated by adapting the win ratio method on pooled together clinical outcome measures (Pocock et al. 2012). The win ratio was the total number of wins (i.e., improvements in any outcome measure) divided by the total number of losses (i.e., non-improvements in any outcome measure) for each patient.
Results
All patients showed a marked degree of impairment in each administered cognitive test, as indicated by the deviation from the mean normal value for age and gender (n.v. ± SD) in each test. In particular, RCPM showed a decrease of 21% from the n.v. (33 ± 3), RSPM a decrease of 33% from the n.v. (46 ± 5), MTCM rapidity a decrease of 53% from the n.v. (3.2 ± 0.1), MTCM accuracy a decrease of 58% from the n.v. (4.5 ± 0.2), and VMI a decrease of 29% from the n.v. (102 ± 10). Furthermore, all patients showed a marked degree of anxiety as the BAI-Y score was 2% lower than the maximum value (63, n.v. ≤ 7) (Table 2). Two children were on paroxetine for anxiety.
All patients completed the VRT training without reporting any adverse event or side effects. They were provided with just VRT, so they did not practice physiotherapy, counseling, or other individualized approaches. We found a significant time effect concerning anxiety (BAI-Y; reduced) (F(2,38) = 43, p < 0.001, η2 = 0.99), non-verbal fluid intelligence (RCPM, improved, F(2,38) = 29, p < 0.001, η2 = 0.99; RSPM, improved, F(2,38) = 20, p < 0.001, η2 = 0.99) and visuospatial cognition (VMI; improved) (F(2,38) = 26, p < 0.001, η2 = 0.99). All such changes were maintained up to T2, as revealed by the paired t-tests comparing pre and post differences for the total sample (Table 2). Concerning attention, there was a significant time effect for the accuracy score of MTCM (F(2,38) = 7, p = 0.002, η2 = 0.92), which increased. However, this improvement was not maintained at T2. Conversely, the rapidity scores of MTCM improved only at T1, but there was a significant time effect (F(2,38) = 4, p = 0.02, η2 = 0.683) (Table 2).
Electrophysiological data
Patients showed a decreased functional connectivity, especially in the theta and alpha bands at baseline, as suggested by the significantly lower global (i.e., across all pair-wise channels) mean functional connectivity values (t(19) = 3.2, p = 0.02 and, respectively t(19) = 3.4, p = 0.02) as compared to the entire frequency range (Fig. 2).
We found a significant time × ROI main interaction concerning omega (time × ROI F(5,95) = 22, p < 0.001), alpha (time × ROI F(5,95) = 5.7, p < 0.001), and theta (time × ROI F(5,95) = 7, p < 0.001) frequency band. Specifically, there were various changes in FLS values following the intervention, which were significant within the fronto-parietal, centro-parietal, and temporo-occipital connectivity paths and within the abovementioned frequency bands (Fig. 3; Table 3). There were also other, specific-ROI differences in frequency ranges, but these were not significant (time × ROI interaction; Table 3).
Only the fronto-parietal connectivity changes in the theta range were significantly correlated with the overall clinical improvement (r = 0.759, p = 0.0001) (Fig. 4). Furthermore, the anxiety changes significantly correlated with fronto-parietal connectivity changes (r = 0.512, p = 0.02) (Fig. 4).
Discussion
Patients showed functional improvements in anxiety and some cognitive domains, including selective attention, visual research, visuospatial integration, after the provision of semi-immersive VRT. Given that this was a pilot, exploratory, and uncontrolled study, our results can, at most, be interpreted as hinting at a possible utility of VR for the rehabilitation of children with ASD. Despite these limitations, our data offer some innovative and promising information concerning additional ASD management strategies. Only some studies examined VRT as a treatment option for individuals with ASD, focusing on teaching emotion recognition, simple language skills (including learning vocabulary words and receptive language), training social skills, awareness, understanding, and teaching problem solving (Bernard-Opitz et al. 2001; Mitchell et al. 2007a, b; Ozonoff and Miller 1995; Herrera et al. 2008; Beaumont and Sofronoff 2008; Wainer and Ingersoll 2011). Conversely, as far as we know, this is the first study addressing cognitive functions and anxiety in children with ASD. Specifically, our primary aim was to measure non-verbal fluid intelligence, attention processes, anxiety symptoms, and visuo-spatial cognition changes at post–pre training. Former studies evaluated the transfer effects from other and primarily targeted domains (e.g., social cognition) to non-trained domains (e.g., executive functions and anxiety) (Kandalaft et al. 2013). Instead, we hypothesized that stimulating problem solving and reasoning capacities could directly improve anxiety and specific areas of cognition (including non-verbal fluid intelligence, attention processes, and visuo-spatial cognition).
Given that an uncontrolled, open, pre-post design cannot allow us interpreting any result in terms of causality (including correlations, which are not proof of causality), we have to keep clear as hypothetical the discussion on the mechanisms subtending the changes we found. Consistently with these premises, the clinical and electrophysiological changes we found after VRT might benefit from the conjugation of complementary and ecologic virtual scenarios with repetitive, task-oriented exercises and augmented visual-audio feedback. This rehab approach permits addressing cognitive domains specifically and facilitating the dynamic of cognitive processes, such as concentration, abilities in recognition, analogic reasoning, and social skills to potentiate empathy and theory of mind (Wang et al. 2013; Mesa-Gresa et al. 2018). To this end, VRE works as a learning tool that can simulate real-life experiences safely and controllably, up to generalizing these virtual experiences to the real-world setting (Wang et al. 2013; Mesa-Gresa et al. 2018; de Moraes et al. 2020). It is noteworthy that VRE-based systems make cognitive tasks easily accessible to children with neurodevelopmental disorders, including ASD. This is due to the device’s property maintaining patients’ attention (providing structured and individualized activities) and addressing patients’ weaknesses while potentiating patients’ strengths (Mitchell et al. 2007a, b; Parsons et al. 2007). We observed that our patients were very motivated and engaged in the VRT, without significant interruptions during the rehabilitative sessions, which is an essential factor for successful cognitive rehabilitation. Another strength point of VRT is the capability to provide the patients with the knowledge of results (e.g., movement outcomes) and performance (e.g., quality of the movements), thus reinforcing the learning processes and positively impacting the cognitive outcomes (Grynszpan et al. 2014).
We also found a noticeable reduction of the anxiety levels. Addressing anxiety levels may be an important outcome in ASD management. A three-way interaction among cognitive functions, social understanding, and aggression exists with anxiety, and the association between cognition and anxiety is critically determined by social cognition ability development (Niditch et al. 2012). Therefore, anxiety reduction may strengthen the learning processes (as anxiety is known to negatively affect cognitive performance) (Wood et al. 2020), with positive results in task performance and, eventually, cognitive outcomes.
At last, we observed a change in the baseline detrimental connectivity within several frontal-parietal connections, including the frontal–central–parietal, frontal–temporal, temporal–occipital, and central–temporal paths, with particular regard to the alpha and theta frequency ranges. This represents an original finding. Such functional connectivity triggering was markedly correlated with the changes observed in sensorimotor integration, visual-spatial cognition, attention abilities, and anxiety. Given the nature of the present study, we cannot be sure of a stringent causal link between cognitive, anxiety, and connectivity improvement. Notwithstanding, we observed a significant change in the most detrimental frequency ranges and connectivity paths in the baseline resting state (Kester and Lucyshyn 2018; Weiss et al. 2018; Uhlhaas and Singer 2007; Larrain-Valenzuela et al. 2017; Chou et al. 2012) after the VRT provision. Therefore, it is likely that theta frequency modulation within several large-scale brain networks may have a significant role concerning some cognitive domains in patients with ASD. Such a frequency modulation may be in keeping with the role of theta activity concerning cognitive performance and the importance of theta deterioration in patients with ASD concerning cognitive performance (Larrain-Valenzuela et al. 2017; Wang et al. 2013; Boutros et al. 2015; Sun et al. 2012; Gandal et al. 2010; Stroganova et al. 2012; Peiker et al. 2015). Furthermore, such a frequency modulation recalls a model of dysfunctional excitatory-inhibitory coordination mechanisms among neuronal assemblies in distinct frontoparietal areas as a putative neurobiological mechanism underlying ASD (Rubenstein and Merzenich 2003; Nelson and Valakh 2015), of which theta oscillation deterioration could be a marker (Buzsáki 2010). Therefore, a reshaping of the abovementioned excitatory-inhibitory coordination mechanisms could favor a better theta-frequency information flow that, in turn, allows for an improvement in cognitive and behavioral performance (Wang et al. 2013; Boutros et al. 2015; Rubenstein and Merzenich 2003; Nelson and Valakh 2015). All of the abovementioned modifications in connectivity patterns may be achieved through specific mechanisms involved in neuroplasticity and neural repair mechanisms, consistently with cognitive-motor learning principles (Ruggeri et al. 2020; Niederkofler et al. 2015).
Strengths, limitations, and conclusions
Compared to the other VRT-based approach in children with ASD reported in the literature, our approach was designed to train subskills of cognition specifically. Furthermore, the approach we adopted, i.e., with a “coach” who could provide immediate feedback (Schilbach et al. 2013), favored the practice of online cognitive tasks (that involves an integrative understanding of social perception and reciprocal communication) rather than offline cognitive tasks (i.e., passively observing an interaction). Finally, our protocol was specifically designed for children (as we used the pediatric module of BTSN). Therefore, VRT could be promising to safely practice and rehearse cognitive skills in children with ASD in an innovative and motivating manner (at least limitedly to the approach we adopted).
However, the evidence by our study is subject to some limitations. First, the present study was uncontrolled, as we did not compare CBT vs. VRT by either a parallel-group design or a randomized cross design). Second, the study focused on a limited number of trained skills and specific outcome measures that were relatively objective (instead of adopting more subjective rating scales). These two issues limit result interpretation, as they mean that the simple time effect cannot be ruled out to explain our findings as the study design was not experimental, and it did not even contain a simple waitlist control group. Therefore, it is necessary to rule out whether a concomitant CBT may equally sustain such broad and lasting changes. Third, the sample size and the follow-up period were limited but consistent with the pilot nature of the study. Fourth, this was a single-user VRT design, so the issues of social cognition and skills remain to be further assessed. Lastly, the magnitude of our EEG findings may depend on the specific analysis procedures we adopted. We applied a generalized measurement of synchronization with full-band EEG and EEG sub-bands (namely FSL) (Ahmadlou and Adeli 2010, 2011; Ahmadlou et al. 2010, 2012) to investigate the aberrant functional connectivity in ASD, instead of employing linear measurements of functional connectivity, as formerly carried out (Rippon et al. 2007; Coben et al. 2008; Chan et al. 2011). Further research is warranted to verify whether the detrimental theta range connectivity represents or not a specific target of VRT. Besides, the generalizability of the reshaping of frontoparietal connectivity in the alpha and theta range following VRT is limited somehow by the EEG approach's intrinsic spatial resolution.
In conclusion, our results hint at a possible utility of VR for the rehabilitation of children with ASD, given that we observed functional improvements in some cognitive domains (including selective attention, visual research, and visuospatial integration) and a reduction of anxiety after VRT, which could have actively contributed to cognitive improvement. However, it will be necessary for future studies to develop consistent validations confirming the hypothesis that VRT can represent a complementary treatment to ASD cognitive rehabilitation. Similarly, whether VRT may determine a large reshape of long-range connectivity patterns, mainly in the theta range, possibly mediating the ASD-related cognitive dysfunction recovery should be further ascertained.
References
Adeli H, Ghosh-Dastidar S, Dadmehr N (2007) A wavelet-chaos methodology for analysis of EEGs and EEG subbands to detect seizure and epilepsy. IEEE Trans Biomed Eng 54:205–211
Ahmadlou M, Adeli H (2010) Wavelet-synchronization methodology: a new approach for EEG-based diagnosis of ADHD. Clin EEG Neurosci 41(1):1–10
Ahmadlou M, Adeli H (2011) Fuzzy synchronization likelihood for automated EEG-based diagnosis of attention-deficit/hyperactivity disorder. Clin EEG Neurosci 42:6–14
Ahmadlou M, Adeli H, Adeli A (2010) Fractality and a wavelet-chaos-neural network methodology for EEG-based diagnosis of autistic spectrum disorder. J Clin Neurophysiol 27:328–333
Ahmadlou M, Adeli H, Adelih A (2012) Fuzzy synchronization likelihood-wavelet methodology for diagnosis of autism spectrum disorder. J Neurosci Methods 211:203–209
American Psychological Association (2015) Neurobehavioral disorders: Autism spectrum disorder, diagnostic and statistical manual of mental disorders (DSM-5), 5th edn. American Psychiatric Association, Washington, D.C.
Beaumont R, Sofronoff K (2008) A multi-component social skills intervention for children with Asperger syndrome: the Junior Detective Training Program. J Child Psychol Psychiatry 49(7):743–753
Beck JS, Jolly JB, Steer RA (2005) Beck youth inventories—second edition for children and adolescents manual (BYI-2). PsyCorp, San Antonio
Beery KE, Beery NA (2004) The beery-buktenica developmental test of visual-motor integration: administration, scoring, and teaching manual, 5th edn. NCS Pearson, Minneapolis
Bellani M, Fornasari L, Chittaro L, Brambilla P (2011) Virtual reality in autism: state of the art. Epidemiol Psychiatr Sci 20(3):235–238
Ben-Sasson A, Hen L, Fluss R, Cermak SA, Engel-Yeger B, Gal E (2009) A meta-analysis of sensory modulation symptoms in individuals with autism spectrum disorders. J Autism Dev Disord 39:1–11
Bernard-Opitz V, Sriram N, Nakhoda-Sapuan S (2001) Enhancing social problem solving in children with autism and normal children through computer-assisted instruction. J Autism Dev Disord 31(4):377–384
Biancardi ASE (1997) The Bells Test revised: a proposal for the study of attention in childhood. Psichiatria dell’Infanzia e dell’Adolescenza 64:73–84
Boutros NN, Lajiness-O’Neill R, Zillgitt A, Richard AE, Bowy SM (2015) EEG changes associated with autistic spectrum disorders. Neuropsychiatr Electrophysiol 1:3
Brentani H, Paula CS, Bordini D, Rolim D, Sato F, Portolese J, Pacifico MC, McCracken JT (2013) Autism spectrum disorders: an overview on diagnosis and treatment. Revista Brasileira de Psiquiatria (Sao Paulo, Brazil : 1999) 35(Suppl 1):S62–S72
Buzsáki G (2010) Neural syntax: cell assemblies, synapsembles, and readers. Neuron 68:362–385
Chan K-S, Tong H (2001) Chaos: a statistical perspective. Springer, New York, pp 113–122
Chan AS, Cheung MC, Tsui WJ, Sze SL, Shi D (2011) Dejian mind-body intervention on depressive mood of community-dwelling adults: a randomized controlled trail. Evid Based Complement Alternat Med 2011:473961
Chou YH, Weingarten C, Madden D, Song A, Chen NK (2012) Applications of virtual reality technology in brain imaging studies. In: Eichenberg C (ed) Virtual reality in psychological, medical and pedagogical applications. IntechOpen
Coben R, Clarke AR, Hudspeth W, Barry RJ (2008) EEG power and coherence in autistic spectrum disorder. Clin Neurophysiol 119:1002–1009
Conaughton RJ, Donovan CL, March S (2017) Efficacy of an internet-based CBT program for children with comorbid high functioning autism spectrum disorder and anxiety: a randomised controlled trial. J Affect Disord 218:260–268
De Luca R, Russo M, Naro A, Tomasello P, Leonardi S, Santamaria F et al (2018) Effects of virtual reality-based training with BTs-Nirvana on functional recovery in stroke patients: preliminary considerations. Int J Neurosci 128(9):791–796
De Luca R, Leonardi S, Portaro S, Le Cause M, De Domenico C, Colucci PV et al (2019) Innovative use of virtual reality in autism spectrum disorder: a case-study. Appl Neuropsychol Child, 1–11
de Moraes Í, Monteiro C, Silva T, Massetti T, Crocetta TB, de Menezes L, Andrade G, Ré A, Dawes H, Coe S, Magalhães FH (2020) Motor learning and transfer between real and virtual environments in young people with autism spectrum disorder: a prospective randomized cross over controlled trial. Autism Res 13(2):307–319
Didehbani N, Allen T, Kandalat M, Krawczyk D, Chapman S (2016) Virtual reality social cognition training for children with high functioning autism. Comput Hum Behav 62:703–711
Doniger GM, Beeri MS, Bahar-Fuchs A, Gottlieb A, Tkachov A, Kenan H, Livny A, Bahat Y, Sharon H, Ben-Gal O, Cohen M (2018) Virtual reality–based cognitive-motor training for middle-aged adults at high Alzheimer’s disease risk: a randomized controlled trial. Alzheimer Dement 4:118–129
Douglas PS (2019) Pre-emptive intervention for autism spectrum disorder: theoretical foundations and clinical translation. front Integr Neurosci 13:66
Edgington L, Hill V, Pellicano E (2016) The design and implementation of a CBT-based intervention for sensory processing difficulties in adolescents on the autism spectrum. Res Dev Disabil 59:221–233
Fan J, Mccandliss B, Fossella J, Flombaum J, Posner M (2005) The activation of attentional networks. Neuroimage 26:471–479
Faria AL, Andrade A, Soares L et al (2016) Benefits of virtual reality based cognitive rehabilitation through simulated activities of daily living: a randomized controlled trial with stroke patients. J Neuroeng Rehabil 13:96
Fuentes J, Bakare M, Munir K, Aguayo P, Gaddour N, Öner Ö (2014) Autism spectrum disorder. In: Rey JM (ed) IACAPAP e-textbook of child and adolescent mental health. International Association for Child and Adolescent Psychiatry and Allied Professions, Geneva
Gandal MJ, Edgar JC, Ehrlichman RS, Mehta M, Roberts TP, Siegel SJ (2010) Validating γ oscillations and delayed auditory responses as translational biomarkers of autism. Biol Psychiat 68:1100–1106
Gaus VL, Attwood T (2018) Cognitive-behavioral therapy for adults with autism spectrum disorder (2nd edn). Guilford Publications
Grynszpan O, Weiss PL, Perez-Diaz F, Gal E (2014) Innovative technology-based interventions for autism spectrum disorders: a meta-analysis. Autism 18:346–361
Herrera G, Alcantud F, Jordan R, Blanquer A, Labajo G, De Pablo C (2008) Development of symbolic play through the use of virtual reality tools in children with autistic spectrum disorders: two case studies. Autism 12(2):143–157
Hofmann SG, Asnaani A, Vonk IJ, Sawyer AT, Fang A (2012) The efficacy of cognitive behavioral therapy: a review of meta-analyses. Cogn Ther Res 36(5):427–440
Kandalaft MR, Didehbani N, Krawczyk DC, Allen TT, Chapman SB (2013) Virtual reality social cognition training for young adults with high-functioning autism. J Autism Dev Disord 43(1):34–44
Kester KR, Lucyshyn JM (2018) Cognitive behavior therapy to treat anxiety among children with autism spectrum disorders: a systematic review. Res Autism Spectr Disord 52:37–50
Kitago T, Krakauer JW (2013) Motor learning principles for neurorehabilitation. Handb Clin Neurol 110:93–103
Kose LK, Fox L, Storch EA (2018) Effectiveness of cognitive behavioral therapy for individuals with autism spectrum disorders and comorbid obsessive-compulsive disorder: a review of the research. J Dev Phys Disabil 30(1):69–87
Larrain-Valenzuela J, Zamorano F, Soto-Icaza P et al (2017) Theta and alpha oscillation impairments in autistic spectrum disorder reflect working memory deficit. Sci Rep 7:14328
Leichsenring F, Steinert C (2017) Is cognitive behavioral therapy the gold standard for psychotherapy? The need for plurality in treatment and research. JAMA 318(14):1323–1324
Maskey M, Rodgers J, Grahame V, Glod M, Honey E, Kinnear J et al (2019) A randomised controlled feasibility trial of immersive virtual reality treatment with cognitive behaviour therapy for specific phobias in young people with autism spectrum disorder. J Autism Dev Disord 49:1912–1927
Mesa-Gresa P, Gil-Gómez H, Lozano-Quilis JA, Gil-Gómez JA (2018) Effectiveness of virtual reality for children and adolescents with autism spectrum disorder: an evidence-based systematic review. Sensors (Basel, Switzerland) 18(8):2486
Mitchell P, Parsons S, Leonard A (2007a) Using virtual environments for teaching social understanding to 6 adolescents with autistic spectrum disorders. J Autism Dev Disord 37(3):589–600
Mitchell P, Parsons S, Leonard A (2007b) Using virtual environments for teaching social understanding to 6 adolescents with autistic spectrum disorders. J Autism Dev Disord 37:589–600
Nelson SB, Valakh V (2015) Excitatory/inhibitory balance and circuit homeostasis in autism spectrum disorders. Neuron 87:684–698
Niditch LA, Varela RE, Kamps JL, Hill T (2012) Exploring the association between cognitive functioning and anxiety in children with autism spectrum disorders: the role of social understanding and aggression. J Clin Child Adolesc Psychol 41(2):127–137
Niederkofler V, Asher TE, Dymecki SM (2015) Functional interplay between dopaminergic and serotonergic neuronal systems during development and adulthood. ACS Chem Neurosci 6:1055–1070
Ogundele MO (2018) Behavioural and emotional disorders in childhood: a brief overview for paediatricians. World J Clin Pediatr 7(1):9–26
Ozonoff S, Miller JN (1995) Teaching theory of mind: a new approach to social skills training for individuals with autism. J Autism Dev Disord 25(4):415–433
Park SH, Song Y, Demetriou EA, Pepper KL, Norton A, Thomas EE, Guastella AJ (2019) Disability, functioning, and quality of life among treatment-seeking young autistic adults and its relation to depression, anxiety, and stress. Autism 23:1675–1686
Parsons S, Mitchell P (2002) The potential of virtual reality in social skills training for people with autistic spectrum disorders. J Intellect Disabil Res 46(Pt 5):430–443
Parsons S, Mitchell P, Leonard A (2005) Do adolescents with autistic spectrum disorders adhere to social conventions in virtual environments? Autism 9(1):95–117
Parsons TD, Bowerly T, Buckwalter JG, Rizzo AA (2007) A controlled clinical comparison of attention performance in children with ADHD in a virtual reality classroom compared to standard neuropsychological methods. Child Neuropsychol 13:363–381
Peiker I, David N, Schneider TR, Nolte G, Schöttle D, Engel AK (2015) Perceptual integration deficits in autism spectrum disorders are associated with reduced interhemispheric gamma-band coherence. J Neurosci 35:16352–16361
Petzinger GM, Fisher BE, McEwen S, Beeler JA, Walsh JP, Jakowec MW (2013) Exercise-enhanced neuroplasticity targeting motor and cognitive circuitry in Parkinson’s disease. Lancet Neurol 12(7):716–726
Pocock SJ, Ariti CA, Collier TJ, Wang D (2012) The win ratio: a new approach to the analysis of composite endpoints in clinical trials based on clinical priorities. Eur Heart J 33(2):176–182
Raven JC, Court JH, Raven J (1998) Raven’s progressive matrices. Oxford Psychologists Press, Oxford
Rippon G, Brock J, Brown C, Boucher J (2007) Disordered connectivity in the autistic brain: challenges for the “new psychophysiology.” Int J Psychophysiol 63:164–172
Rizzi M, D’Aloia M, Castagnolo B (2009) Computer aided detection of microcalcifications in digital mammograms adopting a wavelet decom position. Integr Comput Aided Eng 16:91–103
Rizzo A, Buckwater J (2004) Virtual reality and cognitive assessment and rehabilitation: the state of the art. Stud Health Technol Inform 44:157–165
Rubenstein JL, Merzenich MM (2003) Model of autism: increased ratio of excitation/inhibition in key neural systems. Genes Brain Behav 2:255–267
Ruggeri A, Dancel A, Johnson R, Sargent B (2020) The effect of motor and physical activity intervention on motor outcomes of children with autism spectrum disorder: a systematic review. Autism 24(3):544–568
Schilbach L, Timmermans B, Reddy V, Costall A, Bente G, Schlicht T, Vogeley K (2013) Toward a second-person neuroscience. Behav Brain Sci 36(4):393–414
Spain D, Sin J, Paliokosta E, Furuta M, Prunty JE, Chalder T, Happé FG (2017) Family therapy for autism spectrum disorders. Cochrane Database Syst Rev 5(5):CD011894
Stam CJ, van Dijk BW (2002) Synchronization likelihood: an unbiased measure of generalized synchronization in multivariate data sets. Phys D Nonlinear Phenom 163:236–251
Stroganova TA, Orekhova EV, Prokofyev AO, Tsetlin MM, Gratchev VV, Morozov AA, Obukhov YV (2012) High-frequency oscillatory response to illusory contour in typically developing boys and boys with autism spectrum disorders. Cortex 48:701–717
Sukhodolsky DG, Bloch MH, Panza KE, Reichow B (2013) Cognitive-behavioral therapy for anxiety in children with high-functioning autism: a meta-analysis. Pediatrics 132(5):e1341–e1350
Sun L, Grützner C, Bölte S, Wibral M, Tozman T, Schlitt S et al (2012) Impaired gamma-band activity during perceptual organization in adults with autism spectrum disorders: evidence for dysfunctional network activity in frontal-posterior cortices. J Neurosci 32:9563–9573
Toth K, Munson J, Meltzoff AN, Dawson G (2006) Early predictors of communication development in young children with autism spectrum disorder: joint attention, imitation, and toy play. J Autism Dev Disord 36(8):993–1005
Tzanavari A, Charalambous-Darden N, Herakleous K, Poullis C (2015) Effectiveness of an Immersive Virtual Environment (CAVE) for teaching pedestrian crossing to children with PDD-NOS. In: Proceedings—IEEE 15th International Conference on Advanced Learning Technologies: Advanced Technologies for Supporting Open Access to Formal and Informal Learning, ICALT 2015 pp 423–427
Uhlhaas PJ, Singer W (2007) What do disturbances in neural synchrony tell us about autism? Biol Psychiatry 62:190–191
Wainer AL, Ingersoll BR (2011) The use of innovative computer technology for teaching social communication to individuals with autism spectrum disorders. Res Autism Spectrum Disord 5:96–107
Wallace S, Parsons S, Westbury A, White K, White K, Bailey A (2010) Sense of presence and atypical social judgments in immersive virtual environments. Responses of adolescents with autism spectrum disorders. Autism 14(3):199–213
Walters S, Loades M, Russell A (2016) A systematic review of effective modifications to cognitive behavioural therapy for young people with autism spectrum disorders. Rev J Autism Dev Disord 3:137–153
Wang M, Reid D (2013) Using the virtual reality-cognitive rehabilitation approach to improve contextual processing in children with autism. Sci World J 2013:716890
Wang J, Barstein J, Ethridge LE, Mosconi MW, Takarae Y, Sweeney JA (2013) Resting State EEG abnormalities in autism spectrum disorders. J Neurodev Disord 5:24
Weiss JA, Thomson K, Burnham Riosa P, Albaum C, Chan V, Maughan A, Tablon P, Black K (2018) A randomized waitlist-controlled trial of cognitive behavior therapy to improve emotion regulation in children with autism. J Child Psychol Psychiatry 59:1180–1191
Werchan DM, Baumgartner HA, Lewkowicz DJ, Amso D (2018) The origins of cortical multisensory dynamics: evidence from human infants. Dev Cogn Neurosci 34:75–81
Weston L, Hodgekins J, Langdon PE (2016) Effectiveness of cognitive behavioural therapy with people who have autistic spectrum disorders: a systematic review and meta-analysis. Clin Psychol Rev 49:41–54
Wood JJ, Ehrenreich-May J, Alessandri M, Fujii C, Renno P, Laugeson E et al (2015) Cognitive behavioral therapy for early adolescents with autism spectrum disorders and clinical anxiety: a randomized, controlled trial. Behav Ther 46:7–19
Wood JJ, Kendall PC, Wood KS, Kerns CM, Seltzer M, Small BJ, Lewin AB, Storch EA (2020) Cognitive behavioral treatments for anxiety in children with autism spectrum disorder: a randomized clinical trial. JAMA Psychiatry 77(5):474–483
Zou W, Chi Z, Lo KC (2008) Improvement of image classification using wavelet coefficients with structured-based neural network. Int J Neural Syst 18:195–205
Zwick GP (2017) Neuropsychological assessment in autism spectrum disorder and related conditions. Dialogues Clin Neurosci 19(4):373–379
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
De Luca, R., Naro, A., Colucci, P.V. et al. Improvement of brain functional connectivity in autism spectrum disorder: an exploratory study on the potential use of virtual reality. J Neural Transm 128, 371–380 (2021). https://doi.org/10.1007/s00702-021-02321-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-021-02321-3