Abstract
X-linked dystonia-parkinsonism (XDP) is a debilitating movement disorder endemic to the Panay Island, Philippines. Most studies focus on motor symptoms, hence we reviewed the neurocognitive profile of XDP patients. Neurocognitive testing of XDP patients focused on five domains: general intellectual functioning, episodic memory, language, attention and executive function, and affect. Twenty-nine genetically confirmed patients were included. Twenty-six (89.6%) had impairments in one or more domains, while only three had no impairment in any domain. Attention and executive function was the most commonly affected domain (n = 23, 79.3%). Deficits in general intellect, episodic memory, attention and executive function and affect were seen in our subset of XDP patients. The striatal pathology affecting the frontostriatal circuitry mandating these cognitive processes is mainly implicated in these impairments. The results of our study provided further evidence on the extent of cognitive impairment in XDP using a select battery of neurocognitive tests.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
X-linked dystonia-parkinsonism (XDP) is a movement disorder endemic to Panay Island of the Philippines clinically manifesting as focal dystonia which eventually generalizes with/or is replaced by parkinsonism (Lee et al. 2011). The molecular genetic cause is an inherited SINE-VNTR-Alu (SVA) retrotransposon insertion causing downregulation of the TAF1 (TATA-binding protein-associated factor-1) gene in patients. Within this insertion is a hexanucleotide repeat sequence (CCCTCT)n, the length of which largely determines age at onset as well as other clinical features (Bragg et al. 2017; Aneichyk et al. 2018; Westenberger et al. 2019).
Non-motor symptoms have been reported in other movement disorders, but there is paucity of literature on the non-motor features of XDP (Jamora et al. 2014; Pauly et al. 2020). An extensive review of 414 cases revealed only five cases with information on depression and anxiety (Pauly et al. 2020). A review of five articles with 79 XDP patients showed impaired abstract thinking and motor planning, anxiety (16.7%) and depressive symptoms (54.8–92.9%) (Jamora et al. 2014). A patient who underwent neurocognitive testing prior to deep brain stimulation (DBS) surgery showed deficits in executive functions, memory, visuospatial and language (Howe et al. 2009). Another study reported mild executive dysfunction (Wadia et al. 2010). More recent studies demonstrated impairment of error-related behavioral adaptation, unimpaired response inhibition, and paradoxically better perceptual decision making (Beste et al. 2017a, b). These reports support the need for a comprehensive neuropsychiatric examination among XDP patients to fully illustrate the neurocognitive defects seen in these patients. Thus, we aimed to review the comprehensive assessment of the neurocognitive deficits in a cohort of XDP patients using standardized tests performed on all of them, covering broad domains of general intellectual functioning, language, executive functions, attention, memory, and affect. We also described the potential association between the hexanucleotide repeat length and neuropyschiatric features seen in XDP.
Methods
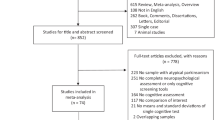
We retrospectively reviewed the records of XDP patients who had neurocognitive assessments between 2009 and 2019 prior to a surgical procedure (DBS or unilateral campotomy). The data reviewed included baseline demographic characteristics, genetic test results, cranial magnetic resonance imaging (MRI) results and information about their medication. All the patients were confirmed to carry the SVA insertion in their DNA using polymerase chain reaction-based detection, as previously reported (Domingo et al. 2015). The length of hexanucleotide repeats within the SVA transposon was also determined.
The neurocognitive evaluation was conducted in English by a licensed and experienced neuropsychologist. A flexible battery testing was employed wherein, depending on the assessment of the neuropsychologist and based on the patient response during the actual examination, a selected number of neurocognitive tests were used to test the five domains (Supplementary Table). Qualitative descriptors were used to standardize the reporting of the results of each neuropsychological test used. The raw scores were converted to scaled scores which are distributed within a normal curve based on different parameters. The scores were then labeled accordingly to the classification levels set per test (Dominguez et al. 2019).
Statistical analysis was done by one of the authors (CTRS). R statistical software (R Foundation for Statistical Computing, Vienna, Austria) was used for all analyses with p value set at < 0.05. Descriptive statistics were used to characterize the sample. Quantitative variables were expressed as means ± standard deviation (SD) while qualitative variables were expressed as percentages. Wilcoxon signed-rank test was used to check for difference between repeat number length in subjects with and without any abnormality in the cognitive domains tested. Kendall correlation coefficient was used to correlate repeat number length with number of impaired domains.
This study was approved by the Ethics Review Board of the University of the Philippines Manila (NEU-2015-26401) and was performed in accordance with the ethical standards of the 1964 Declaration of Helsinki and its amendments.
Results
A total of 29 patients were included. Twenty-four patients underwent DBS [10 were part of the 16-patient cohort operated in Lübeck, Germany (Brüggemann et al. 2019); 14 were operated in Manila, Philippines, 11 of whom have been reported (Abejero et al. 2019)], four patients (one has been reported as an abstract) underwent unilateral transcranial magnetic resonance-guided focused ultrasound campotomy (Chang et al. 2019), and one patient was screened, but eventually declined the DBS.
The mean age was 39.14 ± 7.02 years. The mean disease duration at the time of examination was 3.40 ± 2.01 years. The mean duration of education was 13.97 ± 1.59 years. Three patients had 10 years of education. Twenty-four (86%) patients with readily available clinical MRI results showed varying degrees of caudate head and/or putaminal atrophy typically seen in XDP (Table 1).
Twenty-seven patients had the length of hexanucleotide repeats determined within the SVA transposon. The mean length of the hexanucleotide repeat domain was 43.85 ± 3.30 (36–51). The patients without impairments (n = 2) in any of the domains had a mean repeat length of 44.5 ± 0.71 while patients with impairment (n = 25) in any of the five domains had a mean repeat length of 43.9 ± 3.42. The repeat number length was not different among patients with one abnormal domain and patients with no abnormal domain (p = 0.927). There was also no correlation between repeat number length and number of impaired domains (p = 0.9652).
The patients were on one or more of the following drugs: clonazepam (n = 21), biperiden (n = 19), zolpidem (n = 11), and carbidopa/levodopa (n = 4). Four patients had botulinum toxin injections. Fifteen patients (52%) were on both benzodiazepines and anticholinergics.
Table 2 summarizes the results for the neurocognitive tests done. Of the 29 patients, 26 (89%) had one or more cognitive tests with scores classified as extremely low or impaired. Eighteen patients (62%) showed impairment in more than one domain. Eight patients (28%) had one impaired domain, seven of whom had attention and executive functions impairment and one with moderate depression. Only three patients had no impairment in all five domains. Of the five domains, attention and executive functions was most commonly affected (n = 23/29, 79%).
General intellectual functioning
Nine patients (31%) had impairments in both or one of verbal comprehension or perceptual reasoning skills using the Wechsler Adult Intelligence Scale–Third or Fourth Edition (WAIS-III or WAIS-IV). Verbal intelligence quotient (VIQ), which was tested using vocabulary and comprehension subtests, was impaired in 29% (n = 8/28). Three (10%) patients had extremely low to borderline perceptual reasoning scores, signifying impairment in performance IQ (PIQ).
Episodic memory
Some patients (n = 11/23, 48%) had low scores in one or more of the tests for episodic memory. Fifty-three percent (n = 9/17) showed impairments in auditory memory using the Wechsler Memory Scale (WMS). On the Wide Range Assessment of Memory and Learning–Second Edition (WRAML2) verbal learning subtest which assesses the ability to learn via exposure to the same list of words over four trials, impairment was noted in 26% (n = 6/23). On the design memory subtest which assesses the ability to store and retrieve visually presented material, 38% (n = 6/16) had impairment. There was a tendency to perform better on the recognition part of the WRAML2. For the design memory subtest, 11/16 patients fared better in the recognition part while 16/23 scored better on the recognition part of the verbal learning subtest. Among the patients with impaired scores in WRAML2, recognition scores were better than recall in all except one wherein immediate recall and recognition were both scored extremely low. The results were more heterogenous with the WMS, however, with nine having equal scores for logical memory and recognition parts, three with better logical memory scores and five with better recognition scores.
Language testing
There were no significant impairments seen in all patients (n = 25) who took the Boston Naming Test–Revised (BNT-R) that assesses confrontation naming. An average score was seen in 16 patients (64%), five patients (20%) had high average scores, and four patients had below average scores.
Attention and executive functioning
Twenty-three (79%) patients showed impairment on at least one of the tests for attention and executive functions. There was no impairment on the Stroop Color and Word Test for response inhibition. Forty percent (n = 10/25) of the patients showed impairment on Controlled Oral Word Association Test for semantic fluency. Three (n = 21, 14%) patients displayed impairment on the Delis–Kaplan Executive Function System tower test for planning, monitoring, self-regulation and problem solving. Most patients (n = 19/27, 70%) had impairment on cognitive flexibility as seen on the Wisconsin Card Sorting Test.
Affect
The Hamilton Depression Rating Scale was administered to 24 patients, with half of the patients exhibiting various degrees of depression. Montgomery–Åsberg Depression Rating Scale was administered to five patients, which all had normal results. Insomnia and weight loss were the most frequently reported symptoms. In the subset of subjects with depression, the most commonly reported symptoms were depressed mood, retardation, problems with work and interests, and weight loss.
Discussion
This was a comprehensive investigation on the neurocognitive profiles in a large group of XDP patients who underwent standardized cognitive tests. Many of the affected domains were consistent with those reported in earlier publications (Howe et al. 2009; Wadia, et al. 2010; Jamora et al. 2014).
Anticholinergics and benzodiazepines may play a part, although not directly causative, in the cognitive impairment seen in dystonic patients (Kuyper et al. 2011). However, there has been no clear evidence that medications are directly causative (Howe et al. 2009; Jamora et al. 2014). Thus, anti-dystonic medications may not be solely contributory to the memory impairments seen in XDP.
Structural and functional deficits in the striatum are thought to be responsible for the cognitive dysfunction seen in XDP. The majority of our patients showed bilateral caudate head and putaminal atrophy and hyperintense putaminal rims on cranial MRI which was consistent with the imaging findings of XDP (Arasaratnam et al. 2020). Studies have also shown a reduction in normalized striatal glucose metabolism and reduced striatal uptake of fluorodopa on positron emission topography (Eidelberg et al. 1993; Brüggemann et al. 2017; Kawarai et al. 2017). The decreased uptake of dopamine in XDP may likewise be related to the occurrence of cognitive dysfunction as it has been reported that dopamine contributes to the regulation of cognitive and attentional processes (Nieoullon 2002).
In our cohort of patients, the length of the hexanucleotide repeat domain within the SVA retrotransposon ranged from 36 to 51. Initial studies have found that the repeat number length was found to be negatively correlated to cognitive function using the Mini Mental State Exam score (Westenberger et al. 2019). This provides evidence that the cognitive defects in XDP may not only be due to the structural and functional changes in XDP but it may likewise be modified by the SVA transposon insertion. The repeat number length was not seen to affect the presence of neurocognitive deficits and does not influence the number of impaired domains. These findings may however be limited by the small number of subjects studied, specifically the group with normal neurocognitive testing consisting of only three subjects.
We conducted the neurocognitive tests in English. A majority (n = 26, 90%) of our patients finished tertiary/college (14 years of education) and 3 (10%) finished secondary/high school (10 years of education). These patients have a good grasp of the English language. English and Filipino are taught in schools in the primary/elementary levels, with both becoming the primary languages of instruction in junior and senior high school levels (Official Gazette 2002). In addition, English is the official business language in the Philippines and is spoken widely (Philippine Statistics Office 2021).
General intellectual functioning
In a report, an XDP patient presented with mild deficits in intelligence, showing borderline PIQ and low average VIQ on WAIS-III (Howe et al. 2009). However, the results were attributed to acculturation and the presence of language barrier, with the authors having administered the test in English in the United States to a Filipino gentleman (Howe et al. 2009).
In an MRI study among healthy subjects, it was found that bilateral caudate volume, independent of total brain volume, was significantly positively correlated to full scale intelligence quotient and VIQ and weakly associated to PIQ (Grazioplene et al. 2015). This was attributed to the availability of dopamine D2 and D3 receptors in the striatum; the abundance of which is correlated to caudate nuclei volume and density as well as higher VIQ among healthy subjects (Guo et al. 2006; Woodward et al. 2009). In two studies on XDP patients using 123iodobenzamine (IBZM) SPECT, it was demonstrated that dopamine D2 receptor density was reduced among symptomatic XDP patients (Tackenberg et al. 2007; Brüggemann et al. 2017). The degree of reduction in IBZM binding was also found to be associated with bilateral caudate atrophy and right putaminal atrophy (Brüggemann et al. 2017). Although volumetric analysis of the caudate and functional imaging studies were not done in this study, we can infer that caudate atrophy and decrease in dopamine D2 receptor density may be reasons for the presence of intellectual dysfunction in XDP.
Episodic memory
In a previous study, the use of visual and verbal cues also improved performance, implying a deficit in recall (Jamora et al. 2014). Similarly, deficits in recall was seen among our patients. The verbal learning subtest showed that storage of orally presented new information improved when there is repeated exposure. One possible explanation is that learning is still intact in XDP, enabling patients to develop strategies to improve performance for the second task. This also suggests that subjects may have difficulty in generating initial strategies to deal with new tasks, something that has been previously suggested (Jamora et al. 2014).
The striatal atrophy seen in Huntington’s disease (HD) and subsequent dysfunction in the connection between the prefrontal cortex and the striatum is a factor in the impaired recall, cued recall, and recognition were all significantly impaired in symptomatic patients (Montoya et al. 2006; Woodward et al. 2009). In addition, among pre-symptomatic HD gene carriers, episodic memory impairments were also seen (Montoya et al. 2006; Solomon et al. 2007). Using volumetric MRI analysis, it was observed that smaller striatal volumes were independently associated with lower verbal episodic memory test scores (Solomon et al. 2007). Thus, it may also be inferred that due to the striatal involvement in XDP, this may be contributory to the episodic memory seen in these patients.
Language
Impairment of confrontation naming has been reported, so it is not completely spared in XDP (Wu et al. 2020). It can be argued, however, that our patients were younger (39.14 ± 7.02 years) than the 67-year-old XDP patient in the report (Howe et al. 2009). Age has been known to be inversely correlated with BNT scores among normal subjects, which may partially explain the language impairment observed in the older XDP patient (Randolph 1999; Howe et al. 2009).
Numerous neural substrates have been identified for confrontation naming using blood oxygen level-dependent (BOLD) functional MRI (fMRI) studies (Abrahams et al. 2003). The areas particularly activated were the left inferior frontal gyrus, middle and inferior occipital gyri, and the inferior temporal gyrus (Abrahams et al. 2003). These regions have not yet been elucidated to be affected in XDP patients, which may explain the absence of language deficits in our patients. Further proof was seen in a study among HD patients versus controls, wherein no significant difference was seen in the number of spontaneous correct responses in BNT between the two groups (Azambuja et al. 2012). In addition, the XDP patient described in the case report has been symptomatic for 10 years and has had cognitive deficits for 2 years prior to the neuropsychological examination (Howe et al. 2009), hence he has had a much more advanced course than most of our subjects with a mean disease duration of only 3 years. In view of these findings, it must be noted that the BNT-R used in our patients and in the studies cited may not have completely captured the different process required for naming and that a number of tests designed for language testing administered together may be necessary for this purpose (Harry and Crowe 2014).
Attention and executive function
The prefrontal cortex and caudate nucleus have been implicated as the neural substrates governing attention and executive function (Wu et al. 2020). A study among primary and secondary dystonia patients who underwent pre-operative neuropsychiatric evaluation prior to DBS found that 81% of patients had at least one recordable cognitive deficit (Zacharia et al. 2018). A meta-analysis of 652 fMRI studies examining executive function, particularly conflict processing, flexibility, inhibition, and planning subdomains, revealed significant activation increase in specific cortical regions together with the bilateral caudate nuclei (Wu et al. 2020). In Parkinson’s disease (PD) patients, executive impairment was commonly seen and imaging studies demonstrate impairments in the frontostriatal circuitry (Ray and Strafella 2012). It has been shown using fMRI BOLD studies that dopamine deficiency in the caudate leads to decreased activation of the prefrontal cortex thereby impairing processing of these striatal inputs (Beste et al. 2018). Likewise, reduced uptake of presynaptic dopaminergic ligands in the striatum was correlated to the severity of executive dysfunction seen in PD (Ray and Strafella 2012). Executive dysfunction was likewise seen among dystonia patients implicating the frontostriatal pathology (Tackenberg et al. 2007). Among idiopathic and genetic forms of dystonia, verbal learning, set-shifting deficits, performance of dual tasks and category fluency were seen to be impaired (Tackenberg et al. 2007).
Recent neurophysiological studies provide evidence of executive dysfunction in XDP patients (Beste et al. 2017a, b, 2018). In one study, striosomal dysfunction, via its connections to the anterior cingulate cortex, affects error processing and error-related behavioral adaptation in XDP patients (Beste et al. 2017a). In another study, striosomal connections to the medial prefrontal cortex, which help mediate conflict processing were tested and XDP patients were found to have difficulty in increasing cognitive control when confronted with conflicting situations (Beste et al. 2018). Interestingly, XDP patients showed weakened predictive coding processes and in turn performed better in perceptual-decision making compared to healthy controls (Beste et al. 2017b).
Affect
There has been a higher incidence and severity of depressive symptoms in XDP compared to controls (Jamora et al. 2014). As of 2010, there were 21/194 deaths in XDP patients attributed to suicide, exhibiting a suicide rate higher than that of the general population (Jamora et al. 2015). Most of those who committed suicide were in the generalized dystonia stage and assisted or dependent in their activities of daily living (Jamora et al. 2015). Hence, poor functionality may play a role in driving up the suicide rate. Depression has been described in other forms of dystonia (Tackenberg et al. 2007; Stamelou et al. 2012). Cortico-limbic-striatal dysfunction is said to be involved in depression in dystonia patients (Stamelou et al. 2012; Jamora et al. 2014). While it is not clear if the mood symptoms in XDP are part of the pathophysiology of the disorder or due to its social and functional impact on the individual, studies that check for a higher incidence of depression even in asymptomatic carriers or study the correlation of depression with disease severity may help to clarify the matter further.
There are limitations to this study. There were different tests used in the different domains as a flexible battery of neurocognitive testing was employed. It would have been ideal to conduct similar tests in all patients, but limitations in time and resources as well as variable patient response during the actual examination prevented us from doing so. There was no follow-up neurocognitive testing done. While a repeat test may be useful in documenting progression of cognitive impairment, a repeat test will not be a priority given its cost and the other expenses associated with the disease. In a recent cost-analysis paper, the estimated costs in the management of XDP was 30 times the average annual health expenditure of an average Filipino (de Roxas and Jamora 2019). Complete neurocognitive profiling of XDP patients during the different phases of the disease in conjunction with functional imaging and neurophysiological studies on the neuroanatomic and functional changes in XDP may also be helpful. With our study documenting cognitive dysfunction in these areas, the use of the Montreal Cognitive Assessment may be a more cost-effective test. It has also been validated in Hiligaynon (the language used in Panay Island) (Aliling et al. 2019). One also has to remember that these tests (timed or not) cannot be administered to patients with severe oromandibular or cervical dystonia due to the inherent problems in speech brought about by the dystonia. In addition, neurocognitive testing of asymptomatic, but genetically-confirmed XDP patients to act as a control group may help further characterize the neurocognitive profile of these patients. However, this was not possible as these normal individuals at risk would not be consulting at the clinic and partly due to the individual’s hesitancy to know his status and the associated stigma. Moreover, there are no known disease-modifying therapy for XDP. Nevertheless, this was the only study that looked into a bigger cohort of XDP patients and their neurocognitive profile testing multiple domains.
Conclusion
Cognitive deficits were present in XDP patients. More than half (n = 18, 62%) had impairment in more than one domain. The most commonly affected domain was attention and executive function. Problems in general intellect, episodic memory and affect were likewise seen. The results of our study provided further evidence regarding the extent of cognitive and behavioral impairments in XDP using a select battery of neurocognitive tests.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Abejero JE, Jamora RD, Vesagas TS et al (2019) Long-term outcomes of pallidal deep brain stimulation in X-linked dystonia parkinsonism (XDP): up to 84 months follow-up and review of literature. Parkinsonism Relat Disord 60:81–86. https://doi.org/10.1016/j.parkreldis.2018.09.022
Abrahams S, Goldstein LH, Simmons A et al (2003) Functional magnetic resonance imaging of verbal fluency and confrontation naming using compressed image acquisition to permit overt responses. Hum Brain Mapp 20:29–40. https://doi.org/10.1002/hbm.10126
Aliling NB, Rivera AS, Jamora RD (2019) Translation, cultural adaptation, and validation of the Hiligaynon Montreal Cognitive Assessment Tool (MoCA-Hil) among patients with X-linked dystonia parkinsonism (XDP). Front Neurol 10:1249. https://doi.org/10.3389/fneur.2019.01249
Aneichyk T, Hendriks WT, Yadav R et al (2018) Dissecting the causal mechanism of X-linked dystonia-parkinsonism by integrating genome and transcriptome assembly. Cell 172:897-909.e21. https://doi.org/10.1016/j.cell.2018.02.011
Arasaratnam CJ, Singh-Bains MK, Waldvogel HJ, Faull RL (2020) Neuroimaging and neuropathology studies of X-linked dystonia parkinsonism. Neurobiol Dis 148:105186. https://doi.org/10.1016/j.nbd.2020.105186
Azambuja MJ, Radanovic M, Haddad MS et al (2012) Language impairment in Huntington’s disease. Arq Neuropsiquiatr 70:410–415. https://doi.org/10.1590/s0004-282x2012000600006
Beste C, Mückschel M, Rosales R et al (2017a) Striosomal dysfunction affects behavioral adaptation but not impulsivity-evidence from X-linked dystonia-parkinsonism. Mov Disord 32:576–584. https://doi.org/10.1002/mds.26895
Beste C, Mückschel M, Rosales R et al (2017b) Dysfunctions in striatal microstructure can enhance perceptual decision making through deficits in predictive coding. Brain Struct Funct 222:3807–3817. https://doi.org/10.1007/s00429-017-1435-x
Beste C, Mückschel M, Rosales R et al (2018) The basal ganglia striosomes affect the modulation of conflicts by subliminal information-evidence from X-linked dystonia parkinsonism. Cereb Cortex 28:2243–2252. https://doi.org/10.1093/cercor/bhx125
Bragg DC, Mangkalaphiban K, Vaine CA et al (2017) Disease onset in X-linked dystonia-parkinsonism correlates with expansion of a hexameric repeat within an SVA retrotransposon in TAF1. Proc Natl Acad Sci USA 114:E11020–E11028. https://doi.org/10.1073/pnas.1712526114
Brüggemann N, Rosales RL, Waugh JL et al (2017) Striatal dysfunction in X-linked dystonia-parkinsonism is associated with disease progression. Eur J Neurol 24:680–686. https://doi.org/10.1111/ene.13256
Brüggemann N, Domingo A, Rasche D et al (2019) Association of pallidal neurostimulation and outcome predictors with X-linked dystonia parkinsonism. JAMA Neurol 76:211–216. https://doi.org/10.1001/jamaneurol.2018.377
Chang WC, Taira T, Jamora RD, Chiu PY, Lin W (2019) First experience with MR-guided focused ultrasound in the treatment of X-linked dystonia-parkinsonism (XDP). Mov Disord 34(suppl 2). https://www.mdsabstracts.org/abstract/first-experience-with-mr-guided-focused-ultrasound-in-the-treatment-of-x-linked-dystonia-parkinsonism-xdpXDP/
de Roxas RC, Jamora RD (2019) Cost-analysis of the different treatment modalities in X-linked dystonia-parkinsonism. Front Neurol 10:500. https://doi.org/10.3389/fneur.2019.00500
Domingo A, Westenberger A, Lee LV et al (2015) New insights into the genetics of X-linked dystonia-parkinsonism (XDP, DYT3). Eur J Hum Genet 23:1334–1340. https://doi.org/10.1038/ejhg.2014.292
Dominguez JC, Phung TKT, de Guzman MFP et al (2019) Determining Filipino normative data for a battery of neuropsychological tests: the Filipino Norming Project (FNP). Dement Geriatr Cogn Dis Extra 9:260–270. https://doi.org/10.1159/000500519
Eidelberg D, Takikawa S, Wilhelmsen K et al (1993) Positron emission tomographic findings in Filipino X-linked dystonia–parkinsonism. Ann Neurol 34:185–191. https://doi.org/10.1002/ana.410340214
Grazioplene RG, Ryman SG, Gray JR et al (2015) Subcortical intelligence: caudate volume predicts IQ in healthy adults. Hum Brain Mapp 36:1407–1416. https://doi.org/10.1002/hbm.22710
Guo JF, Yang YK, Chiu NT et al (2006) The correlation between striatal dopamine D2/D3 receptor availability and verbal intelligence quotient in healthy volunteers. Psychol Med 36:547–554. https://doi.org/10.1017/S0033291705006732
Harry A, Crowe SF (2014) Is the Boston Naming Test still fit for purpose? Clin Neuropsychol 28:486–504. https://doi.org/10.1080/13854046.2014.892155
Howe LL, Kellison IL, Fernandez HH et al (2009) Neuropsychological profile of a Filipino gentleman with X-linked dystonia–parkinsonism: a case report of Lubag disease. Clin Neuropsychol 23:100–117. https://doi.org/10.1080/13854040801894714
Jamora RD, Ledesma LK, Domingo A, Cenina AR, Lee LV (2014) Nonmotor features in sex-linked dystonia parkinsonism. Neurodegener Dis Manag 4:283–289. https://doi.org/10.2217/nmt.14.16
Jamora RD, Cenina AR, Teleg RA, Lee L (2015) Suicidality among patients with sex-linked dystonia-parkinsonism (XDP). Acta Med Philipp 49:20–23
Kawarai T, Morigaki R, Kaji R, Goto S (2017) Clinicopathological phenotype and genetics of X-linked dystonia-parkinsonism (XDP; DYT3; Lubag). Brain Sci 7:1–13. https://doi.org/10.3390/brainsci7070072
Kuyper DJ, Parra V, Aerts S et al (2011) Nonmotor manifestations of dystonia: a systematic review. Mov Disord 26:1206–1217. https://doi.org/10.1002/mds.23709
Lee LV, Rivera C, Teleg RA et al (2011) The unique phenomenology of sex-linked dystonia parkinsonism (XDP, DYT3, “Lubag”). Int J Neurosci 121:3–11. https://doi.org/10.3109/00207454.2010.526728
Montoya A, Pelletier M, Menear M et al (2006) Episodic memory impairment in Huntington’s disease: a meta-analysis. Neuropsychologia 44:1984–1994. https://doi.org/10.1016/j.neuropsychologia.2006.01.015
Nieoullon A (2002) Dopamine and the regulation of cognition and attention. Prog Neurobiol 67:53–83. https://doi.org/10.1016/s0301-0082(02)00011-4
Official Gazette (2002) What is K to 12 program? https://www.officialgazette.gov.ph/k-12/. Accessed 6 Feb 2021
Pauly MG, Ruiz López M, Westenberger A et al (2020) Expanding data collection for the MDSGene database: X-linked dystonia-parkinsonism as use case example. Mov Disord 35:1933–1938. https://doi.org/10.1002/mds.28289
Philippine Statistics Office (2021). Language. https://psa.gov.ph/ICSDGS/information-note/language. Accessed 6 Feb 2021
Randolph C (1999) Determinants of confrontation naming performance. Arch Clin Neuropsychol 14:489–496
Ray NJ, Strafella AP (2012) The neurobiology and neural circuitry of cognitive changes in Parkinson’s disease revealed by functional neuroimaging. Mov Disord 27:1484–1492. https://doi.org/10.1002/mds.25173
Solomon AC, Stout JC, Johnson SA et al (2007) Verbal episodic memory declines prior to diagnosis in Huntington’s disease. Neuropsychologia 45:1767–1776. https://doi.org/10.1016/j.neuropsychologia.2006.12.015
Stamelou M, Edwards MJ, Hallett M, Bhatia KP (2012) The non-motor syndrome of primary dystonia: clinical and pathophysiological implications. Brain 135:1668–1681. https://doi.org/10.1093/brain/awr224
Tackenberg B, Metz A, Unger M et al (2007) Nigrostriatal dysfunction in X-linked dystonia-parkinsonism (DYT3). Mov Disord 22:900–902. https://doi.org/10.1002/mds.21462
Wadia PM, Lim SY, Lozano AM et al (2010) Bilateral pallidal stimulation for X-linked dystonia parkinsonism. Arch Neurol 67:1012–1015. https://doi.org/10.1001/archneurol.2010.187
Westenberger A, Reyes CJ, Saranza G et al (2019) A hexanucleotide repeat modifies expressivity of X-linked dystonia parkinsonism. Ann Neurol 85:812–822. https://doi.org/10.1002/ana.25488
Woodward ND, Zald DH, Ding Z et al (2009) Cerebral morphology and dopamine D2/D3 receptor distribution in humans: a combined [18F]fallypride and voxel-based morphometry study. Neuroimage 46:31–38. https://doi.org/10.1016/j.neuroimage.2009.01.049
Wu T, Chen C, Spagna A et al (2020) The functional anatomy of cognitive control: a domain-general brain network for uncertainty processing. J Comp Neurol 528:1265–1292. https://doi.org/10.1002/cne.24804
Zacharia SJ, Sokratous G, Samuel M et al (2018) Neuropsychological and neuropsychiatric concerns for deep brain stimulation in dystonia: preoperative profiles in a deep brain stimulation cohort and postoperative changes in three case series reports. Cureus 10:e3507. https://doi.org/10.7759/cureus.3507
Acknowledgements
We would like to thank Dr. Aloysius Domingo, Ms. Joyce Monding-Yabres, Ms. Estrela Silverio and Ms. Ena Anadelle Honrado for their assistance with this study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
RDGJ: conceptualization, data curation, formal analysis, interpretation of data, writing–original draft, writing–review, and editing. CTRS: conceptualization, data curation, formal analysis, interpretation of data, writing-original draft, writing-review, and editing. JECB: conceptualization, data curation, formal analysis, interpretation of data, writing–original draft, and writing–review. GMIR: conceptualization, data curation, formal analysis, interpretation of data, writing–original draft, and writing–review. AW: formal analysis, interpretation of data, writing–review, and editing. CK: formal analysis, interpretation of data, writing–review, and editing. LKL: conceptualization, data curation, formal analysis, interpretation of data, writing–review, and editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethics approval and consent to participate
This was a retrospective study approved by the Ethics Review Board of the University of the Philippines Manila (NEU-2015-26401).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Jamora, R.D.G., Suratos, C.T.R., Bautista, J.E.C. et al. Neurocognitive profile of patients with X-linked dystonia-parkinsonism. J Neural Transm 128, 671–678 (2021). https://doi.org/10.1007/s00702-021-02317-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-021-02317-z