Abstract
Instrumental measurement of response assets and movement behaviour gained importance as addition to rating procedures to determine the efficacy of therapeutic interventions in patients with Parkinson’s disease. Objectives were to determine the response to standardised 100 mg levodopa application with repeat performance of complex and simple instrumental tests in relation to scored motor behaviour in 53 previously treated patients. Levodopa improved rating scores of motor impairment, execution of complicated movement patterns and complex reaction time. Computed improvements in these instrumental test results correlated with each other. Execution of the simple reaction time paradigm and of plain movement sequences did not ameliorate after levodopa. The changes of these simple test results were not associated to each other. These different response patterns result from the higher cognitive demand of dopamine sensitive association areas of the prefrontal cortex and mesolimbic system for the complex test execution in contrast to the simple task performance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Human performance of movement sequences and response assets involves various brain structures. Progressive disability of movement execution and impairment of responsiveness are typical features of Parkinson’s disease (PD). They reflect basal ganglia dysfunction and the related, predominant dopamine deficit in PD (Birn et al. 1999; Loiodice et al. 2019; Mueller et al. 2019). Neurological examination of impaired movement behaviour is essential tool of commonly applied rating scales, such as the Unified Parkinson’s Disease Rating Scale (UPDRS), to describe treatment effects (Fahn and Elton 1987). Execution of motion sequences and reaction time testing also demand other human skills and features such as motivation, attention, concentration, cognitive abilities, and vigilance (Müller and Benz 2002; Müller et al. 2002, 2004). At least partially, these characteristics are also related to frontostriatal circuits and the mesolimbic system of the brain in addition to basal ganglia interaction. Nearly all these structures are also affected in PD (Lalonde and Botez-Marquard 1997; Nieoullon and Coquerel 2003; Akram et al. 2017). Their adequate function does not only depend on dopamine neurotransmission, but also on adequate stimulation with other neurotransmitters, such as noradrenaline, serotonine or acetylcholine. Their content in various brain structures is also altered in idiopathic PD. This disease entity affects various transmitter systems in an individually pronounced manner (Przuntek et al. 2004). Dopamine supplementation predominantly balances the pronounced dopamine deficit in PD, but also influences function of other neurotransmitter systems. Thus, too high dopamine levels may alter the physiological balance between dopamine and acetylcholine, which is closely related with cognitive abilities (Calabresi et al. 2006; Gratton et al. 2017). Another example for the close interaction between the various neurotransmitter systems is the conversion of levodopa to dopamine in serotonine generating neurons (Hensler et al. 2013; Navailles et al. 2014; Leal et al. 2019). Thus levodopa overflow may down regulate endogenous serotonine generation, which may worsen mood in the long term (Nieoullon and Coquerel 2003; Hensler et al. 2013). Accordingly, clinicians not only report an improvement of motor behaviour, but also an associated amelioration of non-motor systems with cautious, slow and adequate titration of predominant dopamine substituting drugs in PD patients (Müller et al. 2017). It is also well known that predominantly impaired motor behaviour in PD enhances, after standardised stimulation of the nigrostriatal dopaminergic system with levodopa in PD patients. This so-called dopaminergic response represents an important criterion for the diagnosis of idiopathic PD (Gelb et al. 1999). Clinicians often combine clinical rating and performance of specific instrumental tests for the appraisal of the effects of dopamine substitution in PD patients (Müller et al., 2002). Thus instrumental assessment of altered movement behaviour gained importance as an objective tool in combination with rating procedures to determine the efficacy of therapeutic interventions in PD (Goetz et al. 2008; Müller et al. 2017). However, dopamine supplementation or a dopamine overflow may also delay cognitive abilities such as reaction time, particularly when PD patients are previously untreated and receive 200 mg levodopa for the first time in their life (Müller et al. 2000a, 2001). Chronic exposure to dopamine substituting drugs in PD patients changes cognitive function, personality and motor behaviour, all of which may start to fluctuate particularly when levodopa with its short half-life is introduced in the treatment regimen (Martinez-Fernandez et al. 2016; Müller et al. 2017). Currently, digital techniques are developed to monitor these fluctuations of motor behaviour in PD patients. These still experimental monitoring systems often focus on certain aspects of motor behaviour or activity in general only and not on additional features of human behaviour, such as cognition (Lakie and Mutch 1989; Nguyen et al. 2019; Vizcarra et al. 2019). However, not only motor symptoms but also non motor features may vary in response to dopaminergic drugs (Witjas et al. 2002; Müller 2014). Thus, further aspects of movement, such as complexity or simplicity of movement execution, may hypothetically behave in a different manner in response to dopaminergic stimulation in PD patients (Müller et al. 2002). Objectives were to determine the response to standardised levodopa application with complex and simple to execute instrumental tests in relation to scored motor behaviour in previously treated PD patients.
Methods
Subjects
Participants were 53 treated, right handed, idiopathic PD patients [25 men, 28 women; age 61.15 ± 18.54 years; Unified Parkinson’s Disease Rating Scale (UPDRS) mental behaviour (I): 2.87 ± 2.16; UPDRS activities of daily living (II): 9.71 ± 6.47; UPDRS motor examination (III): 26.42 ± 14.44; UPDRS motor complications (IV): 1.19 ± 0.32; Hoehn and Yahr Scale (HYS): 2.02 ± 0.88, Schwab and England Scale score 81.59 ± 15.98] without unpredictable motor fluctuations. Subjects with medical conditions, which may affect the outcomes of the performed instrumental tests, were excluded.
Design
PD patients were taken off their regular PD drug therapy for at least 12 h before rating and execution of devices. First the rating (A.H.), second the assessments with the devices [standardised sequence: peg insertion (first), tapping (second), simple reaction time (third) and complex reaction time (fourth)] were performed (technicians). Then the patients received soluble levodopa/benserazide (Madopar LT®). One hour later UPDRS III rating and the instrumental tests in the same sequence were again executed. To minimize learning and training effects, all PD patients were allowed to practice for one minute on the day before with all instrumental tests.
Rating
Motor symptoms were scored with the part motor examination (III) of the UPDRS (Fahn et al. 1987).
Peg insertion
Subjects were asked to transfer 25 pegs (diameter 2.5 mm, lengh 5 cm) from a rack into one of 25 holes (diameter 2.8 mm) in a computer-based contact board individually and as quickly as possible (manufactured by Schuhfried Ges.m.b.H., Austria). The distance between rack and appropriate holes was 32 cm. The board was positioned in the centre and the task was carried out on each side. When transferring each peg from rack to hole, elbows were allowed to be in contact with the table. The time interval between inserting of the first and the last pin initially with the right- and then the left hand was determined. The measurement of the time period for this task was done by a computer to 100 ms (ms) accuracy. The total peg insertion score is the sum of the time intervals of task performance with the right and left hand in ms (Müller et al. 2002).
Tapping
To execute the tapping test (manufactured by Schuhfried Ges.m.b.H., Austria), the individuals were instructed to tap as quickly as possible on a contact board (3 cm × 3 cm) with a contact pencil for a period of 32 s after the initial flash of a yellow stimulus light. Peak height reached by the pencil was not controlled. The board was positioned in the centre. When performing the task, elbows were allowed to be in contact with the table. The number of contacts was registered by means of a computerized device. Tapping rate was first measured with the right hand and then with the left one (Müller et al. 2002).
Simple reaction time paradigm
The response to a visual simple reaction time task (manufactured by Schuhfried Ges.m.b.H., Austria) was measured. The apparatus consisted of a 31 cm × 42 cm rectangular surface with two stimulus lights (red and yellow), each coupled to the reaction button electrode 1 cm in diameter 15 cm equidistant from a central start button electrode. SRT performance did not depend on the red light, which was not presented and employed during the whole test procedure. The subject was asked to press with the index finger of his right hand the central start button. After the appearance of the yellow stimulus light the subject was asked to switch off the light as quickly as possible by moving his finger from the central start button to the reaction button. Reaction time was considered as elapsed interval between onset of the yellow stimulus light and release of the start button. Movement time was the period between release of the start button and the pressing of the reaction button. Thus this paradigm only asks the subject to detect one stimulus and to produce the same response on every trial. All participants were allowed to get familiar and to practice with the apparatus for a standardized period of time [60 s], to avoid learning and training effects on the day before. Since the more affected hand of PD patients presents slower performance than the other less affected one, PD patients were asked only to use the right dominant hand for this within-subjects comparison. Reaction time and movement time were assessed by a computer to millisecond accuracy. Out of 13 correct answers, a truncated mean of values were used for the statistical analysis. Thus measures greater than or less than two standard deviations of the mean value were excluded (Müller et al. 2001).
Choice reaction time paradigm
The motor response was measured with a computer. The paradigm presented optical and acoustic stimuli alone or in combination following a standardized pattern. The apparatus consisted of a 31 cm × 42 cm rectangular surface with two stimulus lights (red and yellow), each coupled to the reaction button electrode 1 cm in diameter 15 cm equidistant from a central start button electrode (manufactured by Schuhfried Ges.m.b.H., Austria). The acoustic signal was provided by a small loud speaker fixed between the two stimulus lights. The subject was asked to press with the index finger of his right (dominant) hand the central start button. Only after the appearance of the yellow stimulus light the subject had to switch off the light as quickly as possible by moving his finger from the central start button to the reaction button. Thus this task may also be classified as discrimination reaction time paradigm, which employs a number of several stimuli, but always need only one type of response all the time. Reaction time was considered as elapsed interval between onset of the yellow stimulus light and release of the start button. Movement time was the time between release of the start button and the pressing of the reaction button. Participants were asked only to use the right dominant hand for this within-subjects comparison. Thus a bias of severity of PD was avoided, since the more affected hand of PD patients presents slower simple reaction times than the contra lateral less affected one. Out of 26 correct answers a truncated mean of values was used for the statistical analysis. Results greater than or less than two standard deviations of the mean value were thus excluded (Müller et al. 2000a).
Statistics
There was a normal data distribution according to the Kolmogorov–Smirnov test. Consequently parametric tests were performed. The t-test for dependent samples was employed for comparisons within each group. Outcomes of both hands of the peg insertion and tapping procedure were added to reduce data for the comparison analysis. Various assessment qualities (UPDRS scoring, four instrumental tests) were conducted. Therefore, the significance level of the p-value was adjusted to 0.01 for comparisons in this exploratory analysis. Correlations with Pearson product-moment correlation between instrumental test results and UPDRS III scores were done at the two assessment moments before and after levodopa intake. Only peg insertion, tapping outcomes, results of total simple- and complex-reaction time assessments were used, to reduce the number of correlations. Differences between outcomes of start of assessment and end of measurement were computed according to the formula: difference = outcome (start)—outcome (end). Pearson product-moment correlation coefficient above 0.4 was considered as significant.
Ethics
The study was approved by the local institutional ethics committee of the Ruhr University of Bochum. The study was performed in the Department of Neurology, St Joseph Hospital (Head at that time: Professor Dr. H. Przuntek). The investigation represented a non-interventional study, i.e. the rules imposed for this observational plan did not interfere with the physician’s common therapy. Patient’s written informed consent regarding the forwarding and storing of medical data was obtained.
Results
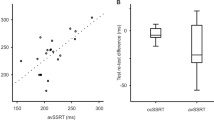
Comparisons
UPDRS III scores improved as to be expected in PD patients (Fig. 1) [before levodopa intake: 26.6 ± 14.4; after levodopa intake: 19 ± 12.7 (mean ± standard deviation are given in the whole paragraph), p < 0.0001]. The interval necessary for performance of the peg insertion task shortened (Fig. 2) [before levodopa intake: 1155 ± 333.3; after levodopa intake: 1076 ± 285.4 (100 ms accuracy), p < 0.0001]. The number of taps did not change (Fig. 3) [before levodopa intake: 304.4 ± 42.3; after levodopa intake: 302.5 ± 51.2, p = n.s.]. The total interval necessary for simple reaction task performance did not change (Fig. 4) [before levodopa intake: 658.2 ± 136.6; after levodopa intake: 666.2 ± 124 (ms), p = n.s.]. Accordingly, neither the reaction time [before levodopa intake: 384.5 ± 90.3; after levodopa intake: 388.3 ± 84.6 (ms), p = n.s.] nor the movement time [before levodopa intake: 266.7 ± 79.3; after levodopa intake: 273.2 ± 66 (ms), p = n.s.] changed. There was no change in the number of right answers [before levodopa intake: 12.4 ± 2.5; after levodopa intake: 12.9 ± 1.6 (right answers), p = n.s.] The total time period needed for performance of the choice reaction time task went down (Fig. 5) [before levodopa intake: 892 ± 172; after levodopa intake: 838.8 ± 155.7 (ms), p = 0.0029]. This effect was due to the reduction of reaction time (Fig. 6) [before levodopa intake: 587.3 ± 133.6; after levodopa intake: 544.1 ± 112,2 (ms), p = 0.0003], whereas movement time did not modify [before levodopa intake: 290.9 ± 84.5 after levodopa intake: 283.2 ± 84.6 (ms), p = n.s.]. The number of right answers improved [before levodopa intake: 23.9 ± 3.2; after levodopa intake: 24.8 ± 2.2 (right answers), p = 0.01].
Correlations
There were significant associations before levodopa administration between all outcomes of the rating and the instrumental test procedures with the exception of the missing relation between the tapping and UPDRS III score (Table 1, columns 3, 4). Significant correlations also appeared after levodopa application between all parameters, but not between the tapping but the total complex reaction time and the UPDRS III score only (Table 1, columns 7, 8). The correlation analysis of the computed differences only showed associations between the peg insertion and the total complex reaction time test and between the simple- and complex-reaction time paradigm (Table 1, columns 5, 6).
Discussion
Neurotransmission of dopamine in the nigrostriatal system is generally essential for execution of all kinds of movement patterns. In previously treated PD patients, our outcomes show that dopamine supplementation improves execution of complex movement patterns and decision making. They ask for higher cognitive load in contrast to a more automated performance of response to the tapping procedure with its demand for execution of simple motion sequences or the simple structure of the decision making process in response to the simple reaction time task (Müller et al. 2000b; Pal et al. 2001; Müller et al. 2002; Taylor Tavares et al. 2005). Peg insertion is characterized by performance of complex movement sequences with an additional need for visual and spatial cognition, self-elaboration of internal strategies, sorting and planning (Müller et al. 2000b; Pal et al. 2001; Müller et al. 2002; Haaland et al. 2004; Taylor Tavares et al. 2005; Espay et al. 2009). A demand for repeat decision making with a “yes or no” answer to the various provided stimuli particularly characterises the complex reaction time task. Thus, both, the peg insertion task and the complex reaction time paradigm, which is also classified as a “go or no go” reaction pattern, hypothetically involve higher cognitive functions (Lalonde and Botez-Marquard 1997; Müller et al. 2000a). The complexity of the execution of both instrumental paradigms is hypothetically not only modulated by the striatal dopamine content, but also influenced by dopamine sensitive association areas of the prefrontal cortex and in the mesolimbic system (Lalonde and Botez-Marquard 1997; Akram et al. 2017; Cools et al. 2019; Trujillo et al. 2019) This hypothesis of the involvement of similar brain structures for the execution of both tasks is supported by the significant relationship between the computed differences of complex reaction time outcomes and the peg insertion results in the correlation analysis. Performance of both more complex tasks also asks for more attention and vigilance in contrast to the execution of the tapping- and simple reaction time task with their demand for more automated performance of movement sequences respectively reaction responses. Thus movement time of the choice reaction time tasks measures performance a simple movement sequence similar to the tapping procedure or the components of the instrumental simple reaction time tool. Consequently it did not improve in contrast to reaction time which reflects the need for a more complex decision process with more necessary cognitive load and attention.
Dopamine is also involved in the regulation of attention via the frontal lobe and basal ganglia (Pal et al. 2001; Nieoullon and Coquerel 2003; Akram et al. 2017; Cools et al. 2019; Trujillo et al. 2019). Previous investigations also demonstrated that selective lesions of this dopamine-regulated components of the mesolimbic system and its associated frontal cortical circuit causes cognitive deficits (Pal et al., 2001; Nieoullon and Coquerel 2003; Akram et al. 2017; Cools et al. 2019; Trujillo et al. 2019). Therefore dopamine is also looked upon as a powerful regulator of different aspects of cognitive brain functions (Nieoullon and Coquerel 2003; Cools et al. 2019; Trujillo et al. 2019). Additionally, ameliorated execution of the choice reaction time and the peg insertion paradigm following levodopa intake may also result from an increased vigilance (Müller et al. 2001; Nieoullon and Coquerel 2003; Trujillo et al. 2019). This hypothesis may cause a controversy. PD patients often complain sedative adverse events following the administration of dopaminergic drugs like levodopa or dopamine agonists. Clinicians observed yawning as an aura for onset of a levodopa-induced “ON” - phase in PD. It may resemble a temporary onset of fatigue. The occurrence of a decreased number of oxytocin-immunoreactive neurons in the paraventricular nucleus of the hypothalamus in PD may be responsible (Purba et al. 1994; Chini et al. 2014). This structure receives afferent projections from midbrain dopaminergic neurons. Oxytocin release from this area in response to dopaminergic stimulation is believed to mediate yawning (Goren and Friedman 1998; Teive et al. 2018). A further hypothetical consideration on levodopa caused fatigue concerns interactions between dopamine and noradrenaline due to the consecutive peripheral lowering of blood pressure (Garber and Friedman 2003; Pursiainen et al. 2012; Fabbri et al. 2017). However, one may also assume that long-term application of dopaminergic drugs, like in our investigated previously treated PD patients, induces a certain tolerance and capacity to compensate all these mechanisms similar to several other dopamine mediated side effects, like nausea or hypotension (Nieoullon and Coquerel 2003). Therefore, we hypothesize in conclusion that we found an improved complex reaction time task performance in contrast to earlier findings in previously untreated PD patients, which orally received 200 mg levodopa and 50 mg benserazide. In that trial, a delay of complex reaction time was shown, probably as consequence of a missing tolerance to the aforementioned sedative dopamine mediated effects or as a result of too high stimulation with dopamine (Müller et al. 2001). It is well known, dopamine overflow may also reduce cognition processing speed in areas like the prefrontal cortex with relatively intact dopaminergic systems (Korf and Loopuijt 1988; Nieoullon and Coquerel 2003). Our results also support the view, that dopamine sensitive areas other than the nigrostriatal system are more vulnerable to fluctuations of dopamine. Therefore, features of non-motor fluctuations often precede the onset of motor fluctuations (Korf and Loopuijt 1988; Witjas et al. 2002; Martinez-Fernandez et al. 2016).
The correlation analysis confirms earlier findings in previously untreated PD patients, that both peg insertion and tapping outcomes are associated with each other in terms of measurement of disability in PD (Müller et al. 2000b; Müller et al. 2002). Earlier investigations also showed that peg insertion in contrast to tapping results are superior to reflect UPDRS III scoring of motor behaviour and response to titration with dopaminergic drugs (Müller et al. 2000b; Müller et al. 2002). Since execution of both reaction time paradigms is somehow very closely related, the found associations may be looked upon as an expected outcome to a certain extent.
One limitation of this trial is that we did not change the sequence of tasks performance to exclude or to discuss a certain overloading effect on our results. Further drawbacks are the missing comparisons against placebo application and that we did not run the same study in healthy controls and previously untreated PD patients.
In conclusion, we show that levodopa response may differ dependent on the necessary cognitive load for execution of an instrumental task in previously treated PD patients.
References
Akram H, Wu C, Hyam J, Foltynie T, Limousin P, De VE, Yousry T, Jahanshahi M, Hariz M, Behrens T, Ashburner J, Zrinzo L (2017) l-Dopa responsiveness is associated with distinctive connectivity patterns in advanced Parkinson's disease. Mov Disord 32:874–883
Birn RM, Bandettini PA, Cox RW, Shaker R (1999) Event-related fMRI of tasks involving brief motion. Hum Brain Mapp 7:106–114
Calabresi P, Picconi B, Parnetti L, Di FM (2006) A convergent model for cognitive dysfunctions in Parkinson's disease: the critical dopamine-acetylcholine synaptic balance. Lancet Neurol 5:974–983
Chini B, Leonzino M, Braida D, Sala M (2014) Learning about oxytocin: pharmacologic and behavioral issues. Biol Psychiatry 76:360–366
Cools R, Frobose M, Aarts E, Hofmans L (2019) Dopamine and the motivation of cognitive control. Handb Clin Neurol 163:123–143
Espay AJ, Morgante F, Lang AE, Chen R (2009) Impairments of speed and amplitude of movement in Parkinson's disease: a pilot study. Mov Disord 24(7):1001–1008
Fabbri M, Coelho M, Guedes LC, Chendo I, Sousa C, Rosa MM, Abreu D, Costa N, Godinho C, Antonini A, Ferreira JJ (2017) Response of non-motor symptoms to levodopa in late-stage Parkinson's disease: results of a levodopa challenge test. Parkinsonism Relat Disord 39:37–43
Fahn S, Elton RL (1987) Unified Parkinson's disease rating scale. In: Fahn S, Marsden CD, Calne D, Goldstein M (eds) Recent devolpments in Parkinson’s disease. Macmillon Healthcare Information, Florham Park, pp 153–163
Garber CE, Friedman JH (2003) Effects of fatigue on physical activity and function in patients with Parkinson's disease. Neurology 60:1119–1124
Gelb DJ, Oliver E, Gilman S (1999) Diagnostic criteria for Parkinson disease. Arch Neurol 56:33–39
Goetz CG, Stebbins GT, Wolff D, Deleeuw W, Bronte-Stewart H, Elble R, Hallett M, Nutt J, Ramig L, Sanger T, Wu AD, Kraus PH, Blasucci LM, Shamim EA, Sethi KD, Spielman J, Kubota K, Grove AS, Dishman E, Taylor CB (2008) Testing objective measures of motor impairment in early Parkinson's disease: feasibility study of an at-home testing device. Mov Disord 24:549–554
Goren JL, Friedman JH (1998) Yawning as an aura for an L-dopa-induced "on" in Parkinson's disease. Neurology 50:823
Gratton C, Yousef S, Aarts E, Wallace DL, D'Esposito M, Silver MA (2017) Cholinergic, but not dopaminergic or noradrenergic, enhancement sharpens visual spatial perception in humans. J Neurosci 37:4405–4415
Haaland KY, Elsinger CL, Mayer AR, Durgerian S, Rao SM (2004) Motor Sequence complexity and performing hand produce differential patterns of hemispheric lateralization. J Cognit Neurosci 16:621–636
Hensler JG, Artigas F, Bortolozzi A, Daws LC, De DP, Milan L, Navailles S, Koek W (2013) Catecholamine/serotonin interactions: systems thinking for brain function and disease. Adv Pharmacol 68:167–197
Korf J, Loopuijt LD (1988) Synaptic and non-synaptic striatal dopamine D2 receptors: possible implications in normal and pathological behaviour. Acta Morphol Neerl Scand 26:177–190
Lakie M, Mutch WJ (1989) Finger tremor in Parkinson's disease. J Neurol Neurosurg Psychiatry 52:392–394
Lalonde R, Botez-Marquard T (1997) The neurobiological basis of movement initiation. Rev Neurosci 8:35–54
Leal PC, Bispo JMM, Engelberth RCGJ, Silva KD, Meurer YR, Ribeiro AM, Silva RH, Marchioro M, Santos JR (2019) Serotonergic dysfunction in a model of parkinsonism induced by reserpine. J Chem Neuroanat 96:73–78
Loiodice S, Wing YH, Rion B, Meot B, Montagne P, Denibaud AS, Viel R, La Drieu RC (2019) Implication of nigral dopaminergic lesion and repeated L-dopa exposure in neuropsychiatric symptoms of Parkinson's disease. Behav Brain Res 360:120–127
Martinez-Fernandez R, Schmitt E, Martinez-Martin P, Krack P (2016) The hidden sister of motor fluctuations in Parkinson's disease: a review on nonmotor fluctuations. Mov Disord 31:1080–1094
Mueller K, Jech R, Ballarini T, Holiga S, Ruzicka F, Piecha FA, Moller HE, Vymazal J, Ruzicka E, Schroeter ML (2019) Modulatory effects of levodopa on cerebellar connectivity in Parkinson's disease. Cerebellum 18:212–224
Müller T (2014) Tolcapone addition improves Parkinson's disease associated nonmotor symptoms. Ther Adv Neurol Disord 7:77–82
Müller T, Benz S (2002) Quantification of the dopaminergic response in Parkinson's disease. Parkinsonism Relat Disord 8:181–186
Müller T, Benz S, Przuntek H (2000a) Choice reaction time after levodopa challenge in Parkinsonian patients. J Neurol Sci 181:98–103
Müller T, Schäfer S, Kuhn W, Przuntek H (2000b) Correlation between tapping and inserting of pegs in Parkinson's disease. Can J Neurol Sci 27:311–315
Müller T, Benz S, Börnke C (2001) Delay of simple reaction time after levodopa intake. Clin Neurophysiol 112:2133–2137
Müller T, Benz S, Przuntek H (2002) Tapping and peg insertion after levodopa intake in treated and de novo parkinsonian patients. Can J Neurol Sci 29:73–77
Müller T, Benz S, Bornke C, Przuntek H (2004) Differential response in choice reaction time following apomorphine based on prior dopaminergic treatment. Acta Neurol Scand 109:348–354
Müller T, Öhm G, Eilert K, Möhr K, Rotter S, Haas T, Küchler M, Lütge S, Marg M, Rothe H (2017) Benefit on motor and non-motor behavior in a specialized unit for Parkinson's disease. J Neural Transm (Vienna) 124:715–720
Navailles S, Di GG, De DP (2014) Predicting dopaminergic effects of L-DOPA in the treatment for Parkinson's disease. CNS Neurosci Ther 20:699–701
Nguyen A, Roth N, Ghassemi NH, Hannink J, Seel T, Klucken J, Gassner H, Eskofier BM (2019) Development and clinical validation of inertial sensor-based gait-clustering methods in Parkinson's disease. J Neuroeng Rehabil 16:77
Nieoullon A, Coquerel A (2003) Dopamine: a key regulator to adapt action, emotion, motivation and cognition. Curr Opin Neurol 16(Suppl 2):S3–S9
Pal PK, Lee CS, Samii A, Schulzer M, Stoessl AJ, Mak EK, Wudel J, Dobko T, Tsui JK (2001) Alternating two finger tapping with contralateral activation is an objective measure of clinical severity in Parkinson's disease and correlates with PET. Parkinsonism Relat Disord 7:305–309
Przuntek H, Müller T, Riederer P (2004) Diagnostic staging of Parkinson's disease: conceptual aspects. J Neural Transm (Vienna) 111:201–216
Purba JS, Hofman MA, Swaab DF (1994) Decreased number of oxytocin-immunoreactive neurons in the paraventricular nucleus of the hypothalamus in Parkinson's disease. Neurology 44:84–89
Pursiainen V, Lyytinen J, Pekkonen E (2012) Effect of duodenal levodopa infusion on blood pressure and sweating. Acta Neurol Scand 126:e20–e24
Taylor Tavares AL, Jefferis GS, Koop M, Hill BC, Hastie T, Heit G, Bronte-Stewart HM (2005) Quantitative measurements of alternating finger tapping in Parkinson's disease correlate with UPDRS motor disability and reveal the improvement in fine motor control from medication and deep brain stimulation. Mov Disord 20:1286–1298
Teive HAG, Munhoz RP, Camargo CHF, Walusinski O (2018) Yawning in neurology: a review. Arq Neuropsiquiatr 76:473–480
Trujillo P, van Wouwe NC, Lin YC, Stark AJ, Petersen KJ, Kang H, Zald DH, Donahue MJ, Claassen DO (2019) Dopamine effects on frontal cortical blood flow and motor inhibition in Parkinson's disease. Cortex 115:99–111
Vizcarra JA, Sanchez-Ferro A, Maetzler W, Marsili L, Zavala L, Lang AE, Martinez-Martin P, Mestre TA, Reilmann R, Hausdorff JM, Dorsey ER, Paul SS, Dexheimer JW, Wissel BD, Fuller RLM, Bonato P, Tan AH, Bloem BR, Kopil C, Daeschler M, Bataille L, Kleiner G, Cedarbaum JM, Klucken J, Merola A, Goetz CG, Stebbins GT, Espay AJ (2019) The Parkinson's disease e-diary: developing a clinical and research tool for the digital age. Mov Disord 34:676–681
Witjas T, Kaphan E, Azulay JP, Blin O, Ceccaldi M, Pouget J, Poncet M, Cherif AA (2002) Nonmotor fluctuations in Parkinson's disease: frequent and disabling. Neurology 59:408–413
Acknowledgement
We thank Tanja Steiner, Bettina Marchewitz, Gudrun Edler, Ute Claussnitzer and Christine Stamm for technical assistance. We thank the participating PD patients.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Müller, T., Harati, A. Different response to instrumental tests in relation to cognitive demand after dopaminergic stimulation in previously treated patients with Parkinson’s disease. J Neural Transm 127, 265–272 (2020). https://doi.org/10.1007/s00702-020-02148-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-020-02148-4