Abstract
Here, we report some electrophysiologic and imaging effects of the transcranial direct current stimulation (tDCS) over the dorsolateral prefrontal cortex (dlPFC) in drug addiction, notably in alcohol and crack-cocaine dependence. The low resolution electromagnetic tomography (LORETA) analysis obtained through event-related potentials (ERPs) under drug-related cues, more specifically in its P3 segment (300–500 ms) in both, alcoholics and crack-cocaine users, showed that the ventral medial prefrontal cortex (vmPFC) was the brain area with the largest change towards increasing activation under drug-related cues in those subjects that kept abstinence during and after the treatment with bilateral tDCS (2 mA, 35 cm2, cathodal left and anodal right) over dlPFC, applied repetitively (five daily sessions). In an additional study in crack-cocaine, which showed craving decreases after repetitive bilateral tDCS, we examined data originating from diffusion tensor imaging (DTI), and we found increased DTI parameters in the left connection between vmPFC and nucleus accumbens (NAcc), such as the number of voxels, fractional anisotropy (FA) and apparent diffusion coefficient (ADC), in tDCS-treated crack-cocaine users when compared to the sham-tDCS group. This increasing of DTI parameters was significantly correlated with craving decreasing after the repetitive tDCS. The vmPFC relates to the control of drug seeking, possibly by extinguishing this behavior. In our studies, the bilateral dlPFC tDCS reduced relapses and craving to the drug use, and increased the vmPFC activation under drug cues, which may be of a great importance in the control of drug use in drug addiction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Frontal lobe deficiencies are consistently described in alcoholism (Moselhy et al. 2001; Nakamura-Palacios et al. 2014; Sullivan et al. 2003; Zago-Gomes Mda and Nakamura-Palacios 2009) and also constitute a major structural and behavioral consequence in crack-cocaine dependence (Fein et al. 2002). Frontal executive dysfunction, with deficiency to direct the behavior towards a goal and to plan future actions, to solve problems and to make decisions, to inhibit inadequate behaviors and to change an ongoing behavior when facing a new demand (mental flexibility), and, ultimately, to process working memory, has been associated with poor outcomes following treatment of drug addiction (Moselhy et al. 2001; Goldstein and Volkow 2002).
Imaging studies have shown that drug abusers examined during protracted detoxification show evidence of disrupted activity of frontal regions, including the dorsolateral prefrontal cortex (dlPFC), cingulate gyrus, and orbitofrontal cortex (Koob and Volkow 2010). Fein et al. (2002) showed that chronic crack-cocaine dependence was associated with prefrontal cortex volume reductions that were present at 6 week abstinence, which were associated with poorer performance on tests of executive function.
In subjects chronically exposed to alcohol, magnetic resonance imaging (MRI) studies frequently show a great structural loss not only in the frontal lobes related to executive dysfunctions, but also in other structures involved in memory, such as the hippocampus, mammillary bodies, thalamus, and cerebellar cortex (Sullivan et al. 2000). In a recent study, we observed that the frontal performance was clearly predicted by volumetric changes of gray matter in the prefrontal cortex (PFC) in alcoholics (Nakamura-Palacios et al. 2014), especially from the left rostral middle frontal gyrus, which is mostly related to the dlPFC, and with the left cerebellar cortex, a structure also constituting frontal-subcortical circuits required for adequate executive responses (Constantino and Todd 2003).
Although well-established pharmacologic treatments and bio-psychosocial therapies have been used to treat alcoholism and crack-cocaine addiction, they have shown to be of modest or mixed success in clinical sets (Assanangkornchai and Srisurapanont 2007; Miller et al. 2011; McKay et al. 2005; Siegal et al. 2002). Furthermore, these approaches are often focused on managing acute or protracted abstinence (Siegal et al. 2002), rather than the control of craving and/or relapses. It has to stress that these are high relapsing conditions imposing a great challenge to the success of the abstinence maintenance. Thus, efforts are needed to develop alternatives that could help to improve the control of drug use.
We hypothesized that novel therapeutic approaches to treat drug dependence should be targeted to specific brain areas, notably from the prefrontal region. Because of its main feature of cognitive control, along with other high-order cognitive attributions, we chose to target the dlPFC with a non-invasive brain stimulation technique in drug addicts, starting with alcoholic subjects and crack-cocaine users.
Available evidence for the effects of non-invasive neurostimulation of the dlPFC on craving in substance dependence and food disorder was examined by Jansen et al. (2013) in a meta-analysis including 17 eligible studies. They found a significant medium effect size favoring active non-invasive neurostimulation over sham stimulation for reduction of craving, with no differences between the techniques, between the various substances of abuse, and between substances of abuse and food. They concluded that non-invasive neurostimulation of the dlPFC, irrespectively if transcranial magnetic or direct current stimulation, clearly suggests decreasing craving.
Among these non-invasive brain stimulation techniques, a simple but effective, relatively focal and a good modulator of neuroplasticity—the transcranial direct current stimulation (tDCS)—was chosen as an agent to modulate the dlPFC excitability and, hopefully, change the addictive behavior in drug addicts. This technique has been increasingly shown to benefit many neurobehavioral disorders (Nitsche et al. 2009; Brunoni et al. 2011b, 2012; Faber et al. 2012), and regarding addictive condition, a single session of tDCS over the dlPFC has shown to reduce cue-induced craving for smoking (Fregni et al. 2008a), marijuana (Boggio et al. 2010) and also for food in healthy subjects (Fregni et al. 2008b).
In our first study in alcoholics from the specialized public outpatient service from our Medical School, we observed a small but significant improvement of executive performance after a single application of anodal tDCS over the left dlPFC (with cathode placed extra cephalically—right supradeltoid region) (Nakamura-Palacios et al. 2012). An increase in the mean amplitude of the P3 component in auditory event-related potentials (ERPs) registered under alcohol-related sounds was also observed in the most severely affected alcoholics (2012).
Based on these results, we conducted a clinical trial to investigate clinical and cognitive effects of repetitive (one weekly session for five consecutive weeks) anodal tDCS over the left dlPFC (da Silva et al. 2013). In this study, alcoholic subjects receiving real tDCS seemed to relapse more often when compared to sham-tDCS. However, the gain of executive performance tended to be greater for the real-tDCS group. Also, in this group, the decrease of craving and depressive symptoms was significant (da Silva et al. 2013), but the activation of the PFC was significantly smaller under alcohol-related cues when compared to sham-tDCS by the end of the intervention.
We concluded at this point that repetitive anodal tDCS over the left dlPFC may improve frontal executive functions and reduce craving in alcoholics, but because of the greater proportion of relapses under this treatment, we changed the polarities to cathodal tDCS over the left dlPFC placing the anodal over the right dlPFC, configuring the bilateral tDCS in the following studies in both alcoholic subjects and crack-cocaine dependents.
Under this new montage, a higher proportion (50 %) of alcoholics from outpatient public services who underwent five consecutive sessions of real tDCS, in contrast with 11.8 % from the sham-tDCS group, maintained abstinence from alcohol by the end of 6 months of follow-up. Also, a better quality of life was significantly perceived by alcoholic subjects from real-tDCS group (Klauss et al. 2014).
In the study with outpatient crack-cocaine users, by the end of 3 months of follow-up after tDCS treatment (daily sessions, every other day, up to five sessions), only one out of six subjects (16.6 %) from the sham-tDCS group, but five out of seven subjects (71.4 %) from the real tDCS, maintained abstinence from crack-cocaine use (Conti and Nakamura-Palacios 2014; Conti et al. 2014).
Recently, we observed in inpatients crack-cocaine dependents that craving scores were significantly reduced after repetitive bilateral tDCS treatment (daily sessions, every other day, up to five sessions) when compared to sham-tDCS. Anxiety scores were decreased and quality of life was significantly improved in crack-cocaine dependents after tDCS treatment (Batista et al. 2015).
Here, we will be focusing on few electrophysiologic and neuroimaging changes obtained in alcoholics or crack-cocaine addicts from studies mentioned above, after repetitive bilateral (cathodal left/anodal right) tDCS over dlPFC compared to placebo (sham) control.
Methods
Clinical studies originating the surrogate measurements shown here were registered under ClinicalTrials.gov numbers NCT01330394, NCT01337297, NCT02091167. They consisted of parallel double-blind randomized sham (placebo) controlled and single center trials. Subjects were randomly assigned to receive real brain stimulation (tDCS group) or a simulation of this procedure (sham-tDCS group) in a 1:1 ratio using a computer-generated randomization sequence that was kept with the unblinded study coordinator (not involved in the recruitment) and only revealed to the co-investigator conducting treatments immediately before the first session.
Participants
Here, we will show data from 22 outpatient alcoholics referred from three public outpatient services specializing in mental health from the rural region, 9 outpatient crack-cocaine addicts from the Center for Psychosocial Care for treatment of abuse and dependence of psychoactive substances disorders, and 14 inpatient crack-cocaine addicts from a Clinic for Drug Dependence Treatment from Espírito Santo state, Brazil, all meeting criteria for alcohol or crack-cocaine dependence according to the ICD-10 classification of mental and behavioral disorders and the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV), as determined by clinical evaluation, and all were kept under regular outpatient or inpatient bio-psychosocial therapies.
The inclusion criteria for this study were: (1) male patients over the age of 18 years; (2) met criteria for alcohol or crack-cocaine dependence; (3) in stable clinical condition with no need for inpatient care; (4) able to read, write, and speak Portuguese; and (5) no severe withdrawal signs or symptoms at baseline. Conversely, exclusion criteria included: (1) a condition of intoxication or withdrawal due to a substance other than crack-cocaine, (2) unstable mental or medical disorder or substance abuse or addiction other than crack-cocaine dependence, except nicotine and/or caffeine; (3) a diagnosis of epilepsy, convulsions, or delirium tremens during abstinence from crack-cocaine; (4) a previous history of drug hypersensitivity or adverse reactions to diazepam or other benzodiazepines and haloperidol; (5) any contraindication for electrical brain stimulation procedures such as electronic implants or metal implants.
Ethical approval was provided by the Brazilian Institutional Review Board of the Federal University of Espírito Santo (registrations 017/09, 296/10, 384.281), Brazil. The study was conducted in strict adherence to the Declaration of Helsinki and is in accordance with the ethical standards of the Committee on Human Experimentation of the Federal University of Espírito Santo, ES, Brazil, where this study was conducted. Subjects were fully informed about the experimental protocol and voluntarily signed an informed consent form before the start of the experiment.
tDCS
Direct currents were transferred via a pair of carbonated silicone electrodes (35 cm2) with a thick layer of high-conductive EEG gel underneath them according to our previous study (Nakamura-Palacios et al. 2012). The electric current was delivered by an electric stimulator (Striat, Ibramed Indústria Brasileira de Equipamentos Médicos Ltd, São Paulo, Brazil). For tDCS, the cathode was placed over the left dlPFC (F3) while the anode was placed over the right dlPFC (F4) according to the 10–20 international system. In each session, the currents flowed continuously for 20 min (2.0 mA) or in double applications of 13 min with 20 min interval in between (13:20:13 schedule) (Monte-Silva et al. 2013).
For sham tDCS, the electrodes were placed at the same positions, but the stimulator was gradually turned off after 20 s. In this way, subjects remain blinded to the respective stimulation condition, as the itching sensation typical for tDCS is often only experienced initially during stimulation (Brunoni et al. 2011a). A previous study validated the sham procedure of 2 mA tDCS, showing similar blinding efficacy as a placebo pill (Brunoni et al. 2011a, 2014) .
Both groups (sham- and real-tDCS) received one session a day for five consecutive days or, every other day, in a total of five sessions.
Related potentials (ERPs)
EEG recording
Electrophysiologic recording was obtained through a 32-channel system (QuickAmp40, Brain Products Ltd, Munich, Germany) using active electrodes with an integrated impedance converter for noise subtraction circuits (actiCAP BP; Brain Products Ltd, Munich, Germany) placed on the scalp according to the International 10/20 EEG system. Data were recorded with a sampling rate of 1000 Hz, and analog filtered between 0.016 and 1000 Hz with common average reference.
Experimental design and task
We adapted a cue-reactivity paradigm (LaRowe et al. 2007) following standard cue-reactivity paradigms well established for pictures (Prisciandaro et al. 2014) and videos (Volkow et al. 2011a). During picture presentation, the subjects were asked to press a button whenever alcohol beverage or crack-related pictures were presented, and to withhold the response when the neutral pictures were presented (each 50 % of the stimuli). This allowed us to assert that patients were aware about picture presentation.
Stimuli
Three pictures related to the consumption of alcohol beverage or crack-cocaine (i.e., alcohol-related or crack-related cues), such as, someone drinking a beer, a bottle of the most popular Brazilian spirits drink, and a cup of beer being pulled, or crack rocks, pipes or paraphernalia used for substance use, and someone inhaling the substance, constituted the target visual stimuli. Additionally, three neutral pictures that were unrelated to the consumption of crack (i.e., neutral cues), such as, a landscape with a small road, a field of flowers, and a butterfly, constituted the non-target visual stimuli.
The trial consisted of a randomized sequence of 90 visual presentations (15 times for each picture) approximately presented at eye level, using a 17-in. monitor (1280 × 1024 × 32-bit color, 60 Hz refresh rate). Each picture was presented for 1000 ms, at intervals of 2000 ms; the entire procedure lasted 4.5 min. The default screen consisted of a black background at all times. All pictures were presented by Presentation 10.0 software (Presentation, Neurobehavioral Systems, Inc., Albany, CA).
Data processing
All EEG data were processed using BrainVision Analyzer 2.0 Professional (Brain Products Ltd, Munich, Germany). Data were offline-filtered from 1 to 10 Hz. After ocular correction by independent component analysis and visual inspection for artifact removal, all datasets were segmented into epochs from −200 to 800 ms relative to picture onset and averaged. All epochs were retained. Baseline correction was performed using the prestimulus interval (i.e., −200 to 0 ms). Low-resolution brain electromagnetic tomography (LORETA) was applied to estimate the three-dimensional intracerebral current density distribution (μA/mm2). Together with the high temporal resolution of ERP, these functional images of electric neuronal activity have been validated by comparisons with magnetic resonance imaging (MRI) and positron emission tomography (PET) findings (Anderer et al. 2000; Pascual-Marqui et al. 1999, 2002; Worrell et al. 2000). Because we were mostly interested in frontal activity in alcohol or crack-cocaine users and tDCS was applied over the dlPFC, we focused our analysis on PFC areas as regions of interest (ROI), and the mean absolute P3 (300–500 ms) values after stimulus presentation were analyzed.
Diffusion tensor imaging (DTI)
Magnetic resonance imaging
Fourteen crack-cocaine addicts, seven from real-tDCS group and seven from sham-tDCS group, underwent MRI in a 1.5T scanner (Achieva, Philips Healthcare, Best, The Netherlands) with 8-channel SENSE head coil without paramagnetic contrast administration. Subjects were in the supine position with their legs in parallel, and were asked to stand still during the exam. Briefly, the MRI protocol included a conventional sequence 3D sagittal FLAIR (repetition time (TR)/echo time (TE)/inversion time (TI) of 11000/125/2800 ms, 352/185 matrix, voxel size 0.65 × 0.99 × 5.0, acquisition time: 2 min 12 s), and a spin echo–echo-planar-imaging (SE-EPI) was acquired for DTI imaging with the following parameters: flip angle: 90°, field of view (FOV): 230 × 230 × 125 mm3, isotropic voxel of 2.5 mm3, 92/92 matrix, 50 transverse slices, TR/TE: 5336/75 ms, number of signals averaged (NSA): 1, Echo planar imaging (EPI) factor = 49, spectral presaturation with inversion recovery (SPIR) for fat suppression, acquisition time: 4 min 13 s.
Fiber tracking
A multiple ROI fiber tracking was performed using the magnetic resonance FiberTrak specialist package provided by Philips Healthcare to visualize the diffusion tensor data in specific white matter tracts. In its software, the algorithm is deterministic following the originally proposed by Mori et al. (1999). The anisotropy thresholds for algorithm settings were min FA = 0.15, max angle = 27° and min fiber length = 10 mm. Three main tracts constituting the brain reward circuitry (Weiss 2005; Volkow et al. 2011b; Nakamura Palacios 2011; Tzschentke 2000) were tracked by drawing two ROIs freehand as shown in the Fig. 1a. The mesolimbic pathway was traced by defining the right and left ventral tegmental area (VTA) and the right and left nucleus accumbens (NAcc), respectively. The mesocortical pathway was defined by the right and left VTA and the right and left prefrontal cortex (PFC), respectively. Finally, fibers between ventral medial PFC (vmPFC) and NAcc in the left and right hemisphere were also searched by ROIs definition. Fiber statistics originating after the generation of fiber bundles given as the average plus or minus its standard deviation: FA value (average of fractional anisotropy) for current fiber, ADC [10−3 mm2/s] (average of apparent diffusion coefficient), voxels (number of voxels included in current fiber where the voxel size is equal to the original reconstructed DTI dataset), and lines (number of lines included in current fiber). These values were used for statistical analysis. It needs to be mentioned that persons who processed the fiber tracking were blinded to the tDCS treatment condition of crack-users included in this analysis.
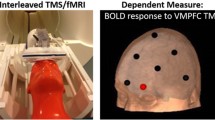
(a) Regions of interest (ROIs) definition by freehand using magnetic resonance FiberTrak specialist package from Philips to visualize the diffusion tensor data in specific white matter tracts, naming mesocortical pathway from ventral tegmental area (VTA) to prefrontal cortex (PFC), mesolimbic pathway from VTA to nucleus accumbens (NAcc), and a pathway from ventral medial PFC (vmPFC) to NAcc; (b) An example of tract’s definition in a crack-user before and after repetitive (5 sessions) application of transcranial direct current stimulation (tDCS), depicting the presence of the vmPFC-NAcc in the left hemisphere after treatment
Statistical analyses
Comparisons of DTI parameters (number of lines, number of voxels, FA and ADC), between groups, and before and after treatment (Fig. 1b) in each side (left or right) of each tract (VTA-PFC, VTA-NAcc or vmPFC-NAcc), were separately analyzed by MANOVA with repeated measures, having groups (sham-tDCS versus tDCS) as the independent factor, and the treatment condition (before, and after tDCS) as the repeated measure factor, including the respective baselines as moderator variables because of baseline inequalities between groups that may exist, and followed by Bonferroni-corrected post hoc t tests. No collinearity was found in all analyses having tolerance >0.1 (between 0.5 and 1.0) and variance inflation factor <3.0 (between 1.0 and 2.0).
Linear regression analyses were applied between differences of DTI parameters (after minus before tDCS or sham-tDCS treatment) and of craving scores for crack use [for craving scale, please see (Batista et al. 2015)].
A two-tailed p value of 0.05 or less was considered to indicate statistical significance. SPSS Statistics Base 17.0 (SPSS Inc., USA) and GraphPad Prism 5.0 (GraphPad Software Inc., USA) were employed for statistical analysis and graphic presentations.
Results
General demographic and drug use characteristics of alcoholics (outpatients) and crack-users (outpatients and inpatients) included in this study are shown in the Table 1.
Visual ERPs
Here, we will only describe the searching of brain region activation by LORETA analysis. Thus, the brain region showing the highest change after treatment when compared to the baseline during the P3 interval (300–500 ms) was searched for each treatment condition (sham-tDCS or real-tDCS) in alcoholics or crack-cocaine users. In this analysis, we considered fourteen alcoholics submitted to the sham-tDCS treatment that had relapsed to the use of alcohol, and eight alcoholics, matched by socio-demographic characteristics and patterns of alcohol use (Table 1), submitted to the real-tDCS treatment, which were able to kept abstinence of alcohol use at least 6 months after the end of the repetitive bilateral tDCS intervention from our previous clinical trial (see (Klauss et al. 2014)).
Although in a smaller number of subjects, we also considered three crack-cocaine users that were able to finish the protocol from sham-tDCS treatment, and six crack-cocaine users from real-tDCS group who had kept abstinence for crack-cocaine use at least for 3 months after the end of tDCS treatment also from our previous clinical trial (see (Conti et al. 2014). They were similar in their pattern of drug use (Table 1).
ERPs were registered in the week before and in the week after the end of brain stimulation treatment in both trials. Interestingly, we found that tDCS-treated subjects that were able to keep abstinence during treatment and for a long-term period after treatment from both drug dependence trials, showed the same area (x = −3, y = 52, z = −6) as the highest changed in brain activation under drug-cued (alcohol or crack-cocaine) stimuli (Fig. 2). According to our LORETA analysis, these coordinates correspond to the Brodmann area 10, or the medial frontal gyrus. The Brodmann area 10 has been related to the frontopolar prefrontal cortex, rostrolateral prefrontal cortex, or anterior prefrontal cortex. However, the referred coordinates may closely correspond to a more particular region from frontopolar cortex, the ventral medial PFC (vmPFC), as described by Bzdok et al. (2013).
Low-resolution brain electromagnetic tomography (LORETA) analysis considering the differences of current densities (μA/mm2) in the P3 segment (300–500 ms) [graphics in the upper panel illustrate event related potentials’ patterns under drug-related cue presentation observed in a sample of thirteen alcoholics compared to six non-alcoholics controls to the left (note the delayed latency and smaller amplitude of the P3 component seen in alcoholics when compared with non-alcoholic controls that are similar to what had been observed in alcoholics or their children (Ciesielski et al. 1985; Berman et al. 1993; Suresh et al. 2003), and in a sample of nine crack-cocaine users compared to nine non-users controls to the right] elicited by drug-related cue presentation (alcohol or crack-cocaine pictures) between the initial (baseline) and final, after bilateral (left cathodal over F3 and right anodal over F4) transcranial direct current stimulation (tDCS, 2 mA, 35 cm2, double stimulation of 13 min with 20 min interval in alcoholics, or for 20 min in crack-cocaine addicts) or respective placebos (sham-tDCS). Coordinates and brain area depicted represent the highest activated brain region. Topographic distributions of the difference (final minus initial) of the current source density (CSD, μV/mm2) over the P3 segment are also shown in small top views. Arrows are pointed to the ventral medial prefrontal cortex (vmPFC)
By contrast, sham-treated alcoholic subjects and crack-cocaine addicts showed very different locations, out of the prefrontal region, as the highest activated region when exposed to drug-cued visual stimuli (Fig. 2): the middle temporal gyrus (Brodmann area 39) in alcoholics, and the inferior parietal lobule (Brodmann area 40) in crack-cocaine users.
DTI
Crack-cocaine addicts randomly assigned to constitute sham-tDCS (7 subjects) or tDCS (other 7 subjects) groups, matched by general demographic characteristics and pattern of drug use (Table 1), underwent MRI scanner for DTI acquisition before and after 5-sessions of treatment with sham (placebo) or real-tDCS, respectively. Because of our interest on specific tracts, their DTI data were preliminarily analyzed by manual fiber tracking.
Regarding lines, representing the number of lines constituting a fiber, no significant differences between groups or within treatment condition (pre versus post) were found in any of fiber tracts analyzed (Fig. 3).
Mean number of lines and voxels (±standard error of the mean—SEM) as diffusion tensor imaging (DTI) parameters of tracts defined by FiberTrak package between ventral tegmental area (VTA) and prefrontal cortex (PFC) or nucleus accumbens (NAcc) and from ventral medial PFC (vmPFC) to NAcc in the left or right hemispheres before (pre) and after (post) 5-session application of bilateral transcranial direct current stimulation (tDCS, n = 7) or placebo (sham-tDCS, n = 7) in crack-cocaine addicts. *p < 0.05 when compared to sham-tDCS, + p < 0.05 when compared to pre (before treatment). Bonferroni’s post hoc test following MANOVA with repeated measures adjusted for baseline
However, the number of voxels included in a fiber was found different between groups only for the left vmPFC to NAcc projection. There was a significant interaction between groups and treatment condition [F(1,11) = 7.4, p = 0.02, partial η 2 = 0.4], in which tDCS-treated subjects showed larger (p = 0.02) number of voxels in this fiber after treatment when compared to sham-tDCS-treated subjects (Fig. 3). It was also significantly increased (p = 0.049) after treatment in this tract in the tDCS group when compared to the number of voxels obtained before treatment (Fig. 3).
MANOVA on FA and ADC parameters also found statistically significant differences only for fibers connecting the left vmPFC and NAcc (Fig. 4). Statistically significant interactions between groups and treatment condition were observed [F(1,11) = 8.1, p = 0.016, partial η 2 = 0.42 for FA, and, F(1,11) = 5.99, p = 0.032, partial η 2 = 0.35 for ADC]. FA and ADC were larger in the tDCS group when compared to sham-tDCS group (p = 0.016 for FA and p = 0.032 for ADC) and they were increased after tDCS treatment (p = 0.018 for FA and p = 0.022 for ADC) comparing to values obtained before treatment (Fig. 4).
Mean fractional anisotropy (FA) and apparent diffusion coefficient (ADC) (±standard error of the mean—SEM) as diffusion tensor imaging (DTI) parameters of tracts defined by FiberTrak package between ventral tegmental area (VTA) and prefrontal cortex (PFC) or nucleus accumbens (NAcc) and from ventral medial PFC (vmPFC) to NAcc in the left or right hemispheres before (pre) and after (post) 5-session application of bilateral transcranial direct current stimulation (tDCS, n = 7) or placebo (sham-tDCS, n = 7) in crack-cocaine addicts. *p < 0.05 when compared to sham-tDCS, + p < 0.05 when compared to pre (before treatment). Bonferroni’s post hoc test following MANOVA with repeated measures adjusted for baseline
DTI and craving
An additional analysis was performed correlating differences of DTI parameters (diff DTI parameter) obtained after the tDCS treatment minus values obtained before the tDCS treatment, with differences of craving scores (diff craving scores) for crack-cocaine use obtained after versus before tDCS treatment. Craving was scored by a brief scale adapted from the Obsessive Compulsive Cocaine Use Scale [please see (Batista et al. 2015) for full details].
Linear regression analysis, having diff craving scores as independent variable and diff DTI parameter as dependent measures, showed statistically significant regressions for differences of FA [Y = 0.047 − 0.029X, r 2 = 0.34, F(1,12) = 6.171, p = 0.029] and of ADC [Y = 0.117 − 0.06X, r 2 = 0.29, F(1,12) = 4.98, p = 0.046] of the left vmPFC-NAcc tract, suggesting that the larger the decreasing on craving scores for crack use, the larger was the increasing of FA and ADC values in the left vmPFC-NAcc tract, irrespective of stimulation treatment (Fig. 5a). When separating the subjects in their treatment groups (sham-tDCS or tDCS), linear regression analysis was no longer statistically significant (Fig. 5b), but note that it was in subjects who received the real-tDCS treatment that larger changes on craving scores in parallel with larger changes in FA and ADC values were observed.
Correlations between differences of values obtained after versus before tDCS treatment of DTI parameters (diff DTI parameter): FA (average of fractional anisotropy) and ADC (average of apparent diffusion coefficient) in the tract between the ventral medial prefrontal cortex and nucleus accumbens (vmPFC-NAcc), with differences of craving scores (diff craving scores) for crack-cocaine use obtained after versus before tDCS treatment, in the total sample (a) and separated by treatment groups (sham-tDCS and tDCS) (b). In a diff FA [Y = 0.047 − 0.029X, r 2 = 0.34, F(1,12) = 6.171, p = 0.029] and diff ADC [Y = 0.117 − 0.06X, r 2 = 0.29, F(1,12) = 4.98, p = 0.046] by linear regression analysis
There was no significant correlation between diff craving scores and differences of number of lines or voxels. There was also no significant correlation between differences of other clinical outcomes (Hamilton Depression Rating Scale and Hamilton Anxiety Rating Scale) with DTI parameters in the left vmPFC-NAcc tract, and between diff of DTI parameters of other tracts (right vmPFC-NAcc, right and left VTA-PFC, and right and left VTA-NAcc) and diff of craving scores and of the other clinical outcomes.
Discussion
The evidence of the same brain region identified as the vmPFC as the highest drug-related activity change in the P3 segment (300–500 ms) seen by LORETA in outpatient alcoholics and crack-cocaine dependents who were able to maintain drug abstinence after repetitive bilateral tDCS over the dlPFC was the outcome that intrigued the most. This electrophysiologic finding was further supported by fiber tracking analysis on DTI acquired in inpatient crack-cocaine dependents after repetitive bilateral tDCS over the dlPFC, which showed important increases on DTI parameters in the tract searched between vmPFC and NAcc after brain stimulation. This increasing on DTI parameters was significantly correlated with craving decreasing after the repetitive tDCS.
In these trials, the cathode was externally placed over the left and the anode over the right dlPFC. It has been acknowledged that the current applied over the scalp is able to reach directly the superficial cortical layers underneath the direct current (DC) stimulation (Wagner et al. 2007; Rahman et al. 2013), not allowing us to expect the activation of the medial portion of the brain. However, recent studies have demonstrated that changes induced by the DC stimulation may reach brain structures beyond those that are directly targeted (Hess 2013; Tanaka et al. 2013; Manuel et al. 2014).
Indeed, a recent study in rodents describes that cathodal, but not anodal, tDCS over the frontal cortex yielded a large and long-lasting increase of extracellular dopamine levels in the striatum (Tanaka et al. 2013) in its more ventral portion, which includes the NAcc (Millan et al. 2011).
Imaging studies in human being suggested that prefrontal brain regions regulate the value of rewards by modulating dopamine increases in the ventral striatum, a regulatory mechanism that becomes dysfunctional in addicted individuals (Volkow et al. 2007). In fact, Volkow et al. (2007) showed that the dopamine release is profoundly decreased in the ventral striatum in detoxified alcoholics.
The NAcc and the VTA, along with the PFC, more specifically its medial portion (mPFC), are brain structures connected by mesocortical and mesolimbic dopamine pathways constituting the brain reward circuitry (Nakamura-Palacios 2011; Nestler 2004; Koob and Volkow 2010; Tzschentke 2001; Volkow et al. 2011b). Drugs of abuse, such as alcohol or crack-cocaine, seem to hold these pathways seized to their action (Volkow et al. 2011b; Hyman et al. 2006), yielding highly addictive behavior (Goldstein and Volkow 2002, 2011), and impairing frontal functions (Volkow et al. 2011b; Park et al. 2010), both conditions that are highly related to the risk of relapse to the drug use.
According to Bzdok et al. (2013), the mPFC has two separate clusters: ventral and dorsal mPFC. The vmPFC is strongly connected to the NAcc, and also to hippocampus, posterior cingulate cortex, and retrosplenial cortex, i.e., preferentially connected with limbic and reward-related medial brain areas associated with reward-related tasks; therefore, subserving predominantly non-ambiguous subjective-value-related evaluative processes involved in bottom-up driven, approach/avoidance-modulation, and evaluation-related processing (Bzdok et al. 2013). This was the cluster showing important change in our alcoholics and crack-cocaine users after the repetitive bilateral tDCS over the dlPFC, which may suggest that the brain stimulation over the dlPFC bilaterally would possibly change the bottom-up driven evaluative processing of rewarding properties of drug-related stimuli, which may have resulted in the modulation of the behavior toward the avoidance of drug use possibly represented here by the parallel reduction of craving to the crack-cocaine use.
Interestingly, when investigating the neural correlates of cue-induced cocaine craving through the use of positron emission tomography, Bonson et al. (2002) found an unexpected deactivation in the left ventral pole and left medial PFC when cocaine abusers were exposed to cocaine-related cues, whereas, other brain areas were activated, such as, left amygdala/rhinal cortex, left lateral orbitofrontal cortex, right superior frontal cortex, and right cerebellum, as it was expected. These authors (Bonson et al. 2002) found difficult to explain the meaning of this deactivation in the frontal pole in cocaine-addicted subjects.
However, more recently, Seo et al. (2013) also showed that alcohol-dependent patients displayed decreased activation in the vmPFC and anterior cingulate cortex (ACC) during stress and alcohol cue trials in functional MRI study when compared to matched non-alcoholics controls, which in its turn, showed robust vmPFC/ACC activation under this condition. Conversely, healthy controls showed vmPFC/ACC deactivation when exposed to neutral-relaxed trials, whereas the alcoholics showed increased activation of the cluster connecting the vmPFC/ACC and ventral striatum under this condition. These authors (Seo et al. 2013) concluded that disrupted vmPFC/ACC function in alcoholics may represent the functional neural state that drives high alcohol craving and relapse risk in recovering alcohol-dependent patients.
Interestingly, they also observed that the hypoactivity of vmPFC/ACC under stress and alcohol cue exposition in alcoholics was able to predict alcohol use severity after their relapses to the drug use (Seo et al. 2013). By contrast, we found that increases of DTI parameters on vmPFC-NAcc tract were correlated with decreasing on craving scores, which seems to nicely match to the evidence above.
Besides drug addiction, a hypofunction of the vmPFC has also been related with pathological gambling (George and Koob 2013). Subjects with pathological gambling, which may be considered an addictive condition sharing core features with drug dependence, also show relatively diminished BOLD signal change induced by gambling stimuli in the vmPFC when compared to subjects without this condition (Potenza 2008).
As already mentioned above, the primary efferent projection from vmPFC is the NAcc shell (Peters et al. 2008). Ghazizadeh et al. (2012) showed evidence suggesting that the vmPFC and the NAcc shell are critical elements of brain circuits relevant to suppression of inappropriate actions, probably by promoting and sustaining the extinction of unreinforced actions. According to these authors, extinction is a learning process that improves performance efficiency by inhibiting irrelevant actions. They showed that vmPFC is crucial for this function, because, actions inhibited by extinction training reappeared when this area was temporarily inactivated in rodents. Besides, they suggest that vmPFC controls the inhibition of action through its inhibitory action over two distinct populations of neurons in the NAcc shell: one composed by phasically inhibited neurons receiving direct glutamatergic projections from vmPFC, and another that promotes actions during the task by phasically excited neurons, which are indirectly inhibited by vmPFC by an intervening GABAergic influence.
Dysfunction in this inhibitory control mediated by vmPFC in drug users may result in uncontrollable drug seeking. In animal research, operant responding for drug of abuse can be acquired by successive training of drug self-administration procedure, stabilizing the drug seeking behavior (Peters et al. 2008, 2009). This drug seeking behavior can be further extinguished, also by a learning procedure, and can subsequently be reinstalled when extinguished animals are exposed to the drug itself, stress or conditioned stimuli that were paired with the drug during self-administration (Oever et al. 2010). By using this model, Peters et al. (2008) showed that, in rodents, the suppression of cocaine seeking produced by prior extinction training required the activity in the infralimbic cortex, a brain area that is closely related to the vmPFC in human being (Oever et al. 2010; Peters et al. 2008). They showed that when the infralimbic cortex was deactivated by gamma-aminobutyric acid (GABA) agonists the cocaine seeking was reinstated, and when neural activity in this cortical region was increased by α-Amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) agonist, the reinstatement of drug seeking by a cocaine injection was inhibited. Thus, this neuronal network, the infralimbic cortex and accumbens shell, is recruited by extinction training to suppress cocaine seeking (Peters et al. 2008).
Many evidences have also identified a role for infralimbic region in the acquisition, consolidation, and expression of fear extinction (Millan et al. 2011), a condition that shares commonalities with addiction (Peters et al. 2009). The extinction training and/or expression of extinction is associated with increases in the neuronal activity in the infralimbic region as indexed by single unit recording or c-Fos protein expression, and when this region is stimulated, the expression of fear is suppressed (Millan et al. 2011).
Thus, the change toward increasing the activation of vmPFC in alcoholics and crack-cocaine users and of the vmPFC-NAcc tract in crack-cocaine users after repetitive tDCS seen in our studies may represent an effort of recovering of a putative disrupted or defected activity of the vmPFC and its connectivity in alcoholics and crack-cocaine users. Unfortunately, we have not compared the activity of this prefrontal area and its connectivity between alcoholics or crack-cocaine users and non-drug users–healthy controls in our studies yet. These are ongoing studies and these comparisons will be focused in our future analysis.
The vmPFC has been also related to decision-making, especially because, it serves to couple two systems that are crucial to this ability, one in which the dlPFC is the key as neural substrate for working memory and its executive processes, and the other system that is critical for processing emotions, having insular cortex and posterior cingulate as key structures (Verdejo-Garcia and Bechara 2009). The integrity of these systems is essential for the vmPFC to mediate efficient decision-making, thus, any impairment in one of them may compromise its functionality (Verdejo-Garcia and Bechara 2009). The disrupted ability to make decisions in drug addicts is one of the commonalities in patients with vmPFC lesions (Verdejo-Garcia and Bechara 2009), which endorses the hypothesis of dysfunction decision-making as an important mechanism involved in drug addiction.
Considering the vmPFC as associated with the attribution of stimulus values, Hare et al. (2014) demonstrated in a fMRI study that the connectivity from left dlPFC to a region of vmPFC increases during trials in which subjects chose to wait for a delayed reward, a response requiring more self-control. According to Rudorf and Hare (2014), the functional interaction between dlPFC and vmPFC is a key aspect of context-dependent valuation, which has a specific application when choices between competing outcomes preferences requires adequate self-control to make a decision. Drug addicts exhibit poor self-control, if any, with a deficiency in the valuation of drug-context as consequence, which may be associated with the compulsive drug seeking for immediate rewarding effects, or relief of abstinence symptoms, in opposing to any postponed reward that the drug abstinence could provide.
In the present study, the tDCS was applied bilaterally over the dlPFC and it was the vmPFC, the area showing the major changes of activation in alcoholics and crack-cocaine users after treatment. Thus, according to the evidence above, tDCS may have helped the context-dependent valuation by increasing the functioning of the vmPFC, providing more adequate self-control and, subsequently, more efficient decision-making. This may be also related to the correlation found between the increasing of DTI parameters in the vmPFC-NAcc tract and craving reduction observed in crack-cocaine users in this study.
There are limitations of this study that need to be considered. Samples of alcoholics and especially of crack-cocaine users were very small because of their own clinical characteristics (high rates of drop-outs, low adherence to bio-psychosocial or to any other therapeutics, etc.) and the complexity of the experimental protocol (clinical and cognitive evaluation, EEG/ERP, MRI), limiting assumptions about the clinical relevance of our findings. Although temporally adequate, the great disadvantage of LORETA analysis is the low spatial resolution, which may be compensated by neuroimaging techniques, such as DTI. The fiber tracking, however, was based on manual definition of ROIs, which may be biased by the experimenter’s experience. Besides, it has to be mentioned that the algorithm employed in the magnetic resonance FiberTrak specialist package based on a modified fiber assignment by continuous tracking (FACT) may not be the one that provides the best anatomic accuracy but it is not worse to give incorrectly displayed fibers in a comparison among different fiber tracking packages done by Feigl et al. (2014), and it has to be considered that, here, we used the same parameters to compare the same subjects before and after the repetitive tDCS treatment. We are aware that this is a very preliminary method of analysis, deserving to be complemented by more robust DTI processing, which is a working in progress. However, this work was intended to explore one point of view regarding brain activity changes induced by prefrontal non-invasive brain stimulation on specific brain structures and their connectivity in drug addiction, which we found worth to share.
Conclusions
Here, we show evidence that vmPFC was the region most activated after repetitive tDCS intervention in alcoholics and crack-cocaine addicts when they were exposed to drug-related cues. Considering all evidence mentioned above, especially that healthy control subjects, but not alcoholics, activate this brain region when they are exposed to stress and alcohol cued imagery trials (Seo et al. 2013), it is reasonable to suggest that the repetitive tDCS over the dlPFC bilaterally may reinstate or facilitate the vmPFC recruitment under the exposition of drug-related cues to provide more self-control over drug seeking by reducing craving and thus, helping to extinguish this behavior, and further recovering the ability to make decisions for better outcomes.
Even considering the limitations of this study, these findings reported here may open important avenues in the managing of drug addiction and in the understanding of modulatory characteristics of the direct current stimulation that need to be carefully investigated in future studies.
References
Anderer P, Saletu B, Pascual-Marqui RD (2000) Effect of the 5-HT(1A) partial agonist buspirone on regional brain electrical activity in man: a functional neuroimaging study using low-resolution electromagnetic tomography (LORETA). Psychiatry Res 100(2):81–96
Assanangkornchai S, Srisurapanont M (2007) The treatment of alcohol dependence. Curr opin psychiatry 20(3):222–227. doi:10.1097/YCO.0b013e3280fa837d
Batista EK, Klauss J, Fregni F, Nitsche MA, Nakamura-Palacios EM (2015) A randomized placebo-controlled trial of targeted prefrontal cortex modulation with bilateral tDCS in patients with crack-cocaine dependence. Int J Neuropsychopharmacol. doi:10.1093/ijnp/pyv066
Berman SM, Whipple SC, Fitch RJ, Noble EP (1993) P3 in young boys as a predictor of adolescent substance use. Alcohol 10(1):69–76
Boggio PS, Zaghi S, Villani AB, Fecteau S, Pascual-Leone A, Fregni F (2010) Modulation of risk-taking in marijuana users by transcranial direct current stimulation (tDCS) of the dorsolateral prefrontal cortex (DLPFC). Drug Alcohol Depend 112(3):220–225. doi:10.1016/j.drugalcdep.2010.06.019
Bonson KR, Grant SJ, Contoreggi CS, Links JM, Metcalfe J, Weyl HL, Kurian V, Ernst M, London ED (2002) Neural systems and cue-induced cocaine craving. Neuropsychopharmacology 26(3):376–386. doi:10.1016/S0893-133X(01)00371-2
Brunoni AR, Amadera J, Berbel B, Volz MS, Rizzerio BG, Fregni F (2011a) A systematic review on reporting and assessment of adverse effects associated with transcranial direct current stimulation. Int J Neuropsychopharmacol 14(8):1133–1145. doi:10.1017/S1461145710001690
Brunoni AR, Valiengo L, Baccaro A, Zanao TA, de Oliveira JF, Vieira GP, Bueno VF, Goulart AC, Boggio PS, Lotufo PA, Bensenor IM, Fregni F (2011b) Sertraline vs. electrical current therapy for treating depression clinical trial–SELECT TDCS: design, rationale and objectives. Contemp Clin Trials 32(1):90–98. doi:10.1016/j.cct.2010.09.007
Brunoni AR, Nitsche MA, Bolognini N, Bikson M, Wagner T, Merabet L, Edwards DJ, Valero-Cabre A, Rotenberg A, Pascual-Leone A, Ferrucci R, Priori A, Boggio PS, Fregni F (2012) Clinical research with transcranial direct current stimulation (tDCS): challenges and future directions. Brain Stimul 5(3):175–195. doi:10.1016/j.brs.2011.03.002
Brunoni AR, Schestatsky P, Lotufo PA, Bensenor IM, Fregni F (2014) Comparison of blinding effectiveness between sham tDCS and placebo sertraline in a 6-week major depression randomized clinical trial. Clin Neurophysiol 125(2):298–305. doi:10.1016/j.clinph.2013.07.020
Bzdok D, Langner R, Schilbach L, Engemann DA, Laird AR, Fox PT, Eickhoff SB (2013) Segregation of the human medial prefrontal cortex in social cognition. Front Hum Neurosci 7:232. doi:10.3389/fnhum.2013.00232
Ciesielski KT, Madden JS, Bligh JG, Schopflocher D (1985) Long-term brain impairment in chronic alcoholics: N2-P3 cognitive potentials in a template-matching memory task. Alcohol Alcohol 20(4):403–408
Constantino JN, Todd RD (2003) Autistic traits in the general population: a twin study. Arch Gen Psychiatry 60(5):524–530. doi:10.1001/archpsyc.60.5.524
Conti CL, Nakamura-Palacios EM (2014) Bilateral transcranial direct current stimulation over dorsolateral prefrontal cortex changes the drug-cued reactivity in the anterior cingulate cortex of crack-cocaine addicts. Brain Stimul 7(1):130–132. doi:10.1016/j.brs.2013.09.007
Conti CL, Moscon JA, Fregni F, Nitsche MA, Nakamura-Palacios EM (2014) Cognitive related electrophysiological changes induced by non-invasive cortical electrical stimulation in crack-cocaine addiction. Int J Neuropsychopharmacol 17(9):1465–1475. doi:10.1017/S1461145714000522
da Silva MC, Conti CL, Klauss J, Alves LG, do Nascimento Cavalcante HM, Fregni F, Nitsche MA, Nakamura-Palacios EM (2013) Behavioral effects of transcranial direct current stimulation (tDCS) induced dorsolateral prefrontal cortex plasticity in alcohol dependence. J Physiol Paris 107(6):493–502. doi:10.1016/j.jphysparis.2013.07.003
Faber M, Vanneste S, Fregni F, De Ridder D (2012) Top down prefrontal affective modulation of tinnitus with multiple sessions of tDCS of dorsolateral prefrontal cortex. Brain Stimul 5(4):492–498. doi:10.1016/j.brs.2011.09.003
Feigl GC, Hiergeist W, Fellner C, Schebesch KM, Doenitz C, Finkenzeller T, Brawanski A, Schlaier J (2014) Magnetic resonance imaging diffusion tensor tractography: evaluation of anatomic accuracy of different fiber tracking software packages. World Neurosurg 81(1):144–150. doi:10.1016/j.wneu.2013.01.004
Fein G, Di Sclafani V, Meyerhoff DJ (2002) Prefrontal cortical volume reduction associated with frontal cortex function deficit in 6-week abstinent crack-cocaine dependent men. Drug Alcohol Depend 68(1):87–93
Fregni F, Liguori P, Fecteau S, Nitsche MA, Pascual-Leone A, Boggio PS (2008a) Cortical stimulation of the prefrontal cortex with transcranial direct current stimulation reduces cue-provoked smoking craving: a randomized, sham-controlled study. J Clin Psychiatry 69(1):32–40
Fregni F, Orsati F, Pedrosa W, Fecteau S, Tome FA, Nitsche MA, Mecca T, Macedo EC, Pascual-Leone A, Boggio PS (2008b) Transcranial direct current stimulation of the prefrontal cortex modulates the desire for specific foods. Appetite 51(1):34–41. doi:10.1016/j.appet.2007.09.016
George O, Koob GF (2013) Control of craving by the prefrontal cortex. Proc Natl Acad Sci USA 110(11):4165–4166. doi:10.1073/pnas.1301245110
Ghazizadeh A, Ambroggi F, Odean N, Fields HL (2012) Prefrontal cortex mediates extinction of responding by two distinct neural mechanisms in accumbens shell. J Neurosci 32(2):726–737. doi:10.1523/JNEUROSCI.3891-11.2012
Goldstein RZ, Volkow ND (2002) Drug addiction and its underlying neurobiological basis: neuroimaging evidence for the involvement of the frontal cortex. Am J Psychiatry 159(10):1642–1652
Goldstein RZ, Volkow ND (2011) Dysfunction of the prefrontal cortex in addiction: neuroimaging findings and clinical implications. Nat Rev Neurosci 12(11):652–669. doi:10.1038/nrn3119
Hare TA, Hakimi S, Rangel A (2014) Activity in dlPFC and its effective connectivity to vmPFC are associated with temporal discounting. Front Neurosci 8:50. doi:10.3389/fnins.2014.00050
Hess CW (2013) Modulation of cortical-subcortical networks in Parkinson’s disease by applied field effects. Front Hum Neurosci 7:565. doi:10.3389/fnhum.2013.00565
Hyman SE, Malenka RC, Nestler EJ (2006) Neural mechanisms of addiction: the role of reward-related learning and memory. Annu Rev Neurosci 29:565–598. doi:10.1146/annurev.neuro.29.051605.113009
Jansen JM, Daams JG, Koeter MW, Veltman DJ, van den Brink W, Goudriaan AE (2013) Effects of non-invasive neurostimulation on craving: a meta-analysis. Neurosci Biobehav Rev 37(10 Pt 2):2472–2480. doi:10.1016/j.neubiorev.2013.07.009
Klauss J, Penido Pinheiro LC, Silva Merlo BL, de Almeida Correia Santos G, Fregni F, Nitsche MA, Miyuki Nakamura-Palacios E (2014) A randomized controlled trial of targeted prefrontal cortex modulation with tDCS in patients with alcohol dependence. Int J Neuropsychopharmacol 17(11):1793–1803. doi:10.1017/S1461145714000984
Koob GF, Volkow ND (2010) Neurocircuitry of addiction. Neuropsychopharmacology 35(1):217–238. doi:10.1038/npp.2009.110
LaRowe SD, Saladin ME, Carpenter MJ, Upadhyaya HP (2007) Reactivity to nicotine cues over repeated cue reactivity sessions. Addict Behav 32(12):2888–2899. doi:10.1016/j.addbeh.2007.04.025
Manuel AL, David AW, Bikson M, Schnider A (2014) Frontal tDCS modulates orbitofrontal reality filtering. Neuroscience 265:21–27. doi:10.1016/j.neuroscience.2014.01.052
McKay JR, Foltz C, Stephens RC, Leahy PJ, Crowley EM, Kissin W (2005) Predictors of alcohol and crack cocaine use outcomes over a 3-year follow-up in treatment seekers. J Subst Abuse Treat 28(Suppl 1):S73–S82. doi:10.1016/j.jsat.2004.10.010
Millan EZ, Marchant NJ, McNally GP (2011) Extinction of drug seeking. Behav Brain Res 217(2):454–462. doi:10.1016/j.bbr.2010.10.037
Miller PM, Book SW, Stewart SH (2011) Medical treatment of alcohol dependence: a systematic review. Int J Psychiatry Med 42(3):227–266
Monte-Silva K, Kuo MF, Hessenthaler S, Fresnoza S, Liebetanz D, Paulus W, Nitsche MA (2013) Induction of late LTP-like plasticity in the human motor cortex by repeated non-invasive brain stimulation. Brain Stimul 6(3):424–432. doi:10.1016/j.brs.2012.04.011
Mori S, Crain BJ, Chacko VP, van Zijl PC (1999) Three-dimensional tracking of axonal projections in the brain by magnetic resonance imaging. Ann Neurol 45(2):265–269
Moselhy HF, Georgiou G, Kahn A (2001) Frontal lobe changes in alcoholism: a review of the literature. Alcohol Alcohol 36(5):357–368
Nakamura Palacios EM (2011) Working memory and prefrontal cortex and their relation with the brain reward system and drug addiction. In: Levin ES (ed) Working memory: capacity, developments and improvement techniques. Nova Science Publishers, New York
Nakamura-Palacios EM (2011) Working memory and prefrontal cortex and their relation with the brain reward system and drug addiction. In: Levin ES (ed) Working memory: capacity, developments and improvement techniques. Neuroscience research progress. Nova Science Publisher, New York
Nakamura-Palacios EM, de Almeida Benevides MC, da Penha Zago-Gomes M, de Oliveira RW, de Vasconcellos VF, de Castro LN, da Silva MC, Ramos PA, Fregni F (2012) Auditory event-related potentials (P3) and cognitive changes induced by frontal direct current stimulation in alcoholics according to Lesch alcoholism typology. Int J Neuropsychopharmacol 15(5):601–616. doi:10.1017/S1461145711001040
Nakamura-Palacios EM, Souza RS, Zago-Gomes MP, de Melo AM, Braga FS, Kubo TT, Gasparetto EL (2014) Gray matter volume in left rostral middle frontal and left cerebellar cortices predicts frontal executive performance in alcoholic subjects. Alcohol Clin Exp Res 38(4):1126–1133. doi:10.1111/acer.12308
Nestler EJ (2004) Molecular mechanisms of drug addiction. Neuropharmacology 47(Suppl 1):24–32. doi:10.1016/j.neuropharm.2004.06.031
Nitsche MA, Boggio PS, Fregni F, Pascual-Leone A (2009) Treatment of depression with transcranial direct current stimulation (tDCS): a review. Exp Neurol 219(1):14–19. doi:10.1016/j.expneurol.2009.03.038
Park SQ, Kahnt T, Beck A, Cohen MX, Dolan RJ, Wrase J, Heinz A (2010) Prefrontal cortex fails to learn from reward prediction errors in alcohol dependence. J Neurosci 30(22):7749–7753. doi:10.1523/JNEUROSCI.5587-09.2010
Pascual-Marqui RD, Lehmann D, Koenig T, Kochi K, Merlo MC, Hell D, Koukkou M (1999) Low resolution brain electromagnetic tomography (LORETA) functional imaging in acute, neuroleptic-naive, first-episode, productive schizophrenia. Psychiatry Res 90(3):169–179
Pascual-Marqui RD, Esslen M, Kochi K, Lehmann D (2002) Functional imaging with low-resolution brain electromagnetic tomography (LORETA): a review. Methods Find Exp Clin Pharmacol 24:91–95
Peters J, LaLumiere RT, Kalivas PW (2008) Infralimbic prefrontal cortex is responsible for inhibiting cocaine seeking in extinguished rats. J Neurosci 28(23):6046–6053. doi:10.1523/JNEUROSCI.1045-08.2008
Peters J, Kalivas PW, Quirk GJ (2009) Extinction circuits for fear and addiction overlap in prefrontal cortex. Learn Mem 16(5):279–288. doi:10.1101/lm.1041309
Potenza MN (2008) Review. The neurobiology of pathological gambling and drug addiction: an overview and new findings. Philos Trans R Soc Lond B Biol Sci 363(1507):3181–3189. doi:10.1098/rstb.2008.0100
Prisciandaro JJ, McRae-Clark AL, Myrick H, Henderson S, Brady KT (2014) Brain activation to cocaine cues and motivation/treatment status. Addict Biol 19(2):240–249. doi:10.1111/j.1369-1600.2012.00446.x
Rahman A, Reato D, Arlotti M, Gasca F, Datta A, Parra LC, Bikson M (2013) Cellular effects of acute direct current stimulation: somatic and synaptic terminal effects. J Physiol 591(Pt 10):2563–2578. doi:10.1113/jphysiol.2012.247171
Rudorf S, Hare TA (2014) Interactions between dorsolateral and ventromedial prefrontal cortex underlie context-dependent stimulus valuation in goal-directed choice. J Neurosci 34(48):15988–15996. doi:10.1523/JNEUROSCI.3192-14.2014
Seo D, Lacadie CM, Tuit K, Hong KI, Constable RT, Sinha R (2013) Disrupted ventromedial prefrontal function, alcohol craving, and subsequent relapse risk. JAMA Psychiatry 70(7):727–739. doi:10.1001/jamapsychiatry.2013.762
Siegal HA, Li L, Rapp RC (2002) Abstinence trajectories among treated crack cocaine users. Addict Behav 27(3):437–449
Sullivan EV, Deshmukh A, Desmond JE, Lim KO, Pfefferbaum A (2000) Cerebellar volume decline in normal aging, alcoholism, and Korsakoff’s syndrome: relation to ataxia. Neuropsychology 14(3):341–352
Sullivan EV, Harding AJ, Pentney R, Dlugos C, Martin PR, Parks MH, Desmond JE, Chen SH, Pryor MR, De Rosa E, Pfefferbaum A (2003) Disruption of frontocerebellar circuitry and function in alcoholism. Alcohol Clin Exp Res 27(2):301–309. doi:10.1097/01.ALC.0000052584.05305.98
Suresh S, Porjesz B, Chorlian DB, Choi K, Jones KA, Wang K, Stimus A, Begleiter H (2003) Auditory P3 in female alcoholics. Alcohol Clin Exp Res 27(7):1064–1074. doi:10.1097/01.ALC.0000075549.49800.A0
Tanaka T, Takano Y, Tanaka S, Hironaka N, Kobayashi K, Hanakawa T, Watanabe K, Honda M (2013) Transcranial direct-current stimulation increases extracellular dopamine levels in the rat striatum. Front Syst Neurosci 7:6. doi:10.3389/fnsys.2013.00006
Tzschentke TM (2000) The medial prefrontal cortex as a part of the brain reward system. Amino Acids 19(1):211–219
Tzschentke TM (2001) Pharmacology and behavioral pharmacology of the mesocortical dopamine system. Prog Neurobiol 63(3):241–320
Van den Oever MC, Spijker S, Smit AB, De Vries TJ (2010) Prefrontal cortex plasticity mechanisms in drug seeking and relapse. Neurosci Biobehav Rev 35(2):276–284. doi:10.1016/j.neubiorev.2009.11.016
Verdejo-Garcia A, Bechara A (2009) A somatic marker theory of addiction. Neuropharmacology 56(Suppl 1):48–62. doi:10.1016/j.neuropharm.2008.07.035
Volkow ND, Wang GJ, Telang F, Fowler JS, Logan J, Jayne M, Ma Y, Pradhan K, Wong C (2007) Profound decreases in dopamine release in striatum in detoxified alcoholics: possible orbitofrontal involvement. J Neurosci 27(46):12700–12706. doi:10.1523/JNEUROSCI.3371-07.2007
Volkow ND, Tomasi D, Wang GJ, Fowler JS, Telang F, Goldstein RZ, Alia-Klein N, Wong C (2011a) Reduced metabolism in brain “control networks” following cocaine-cues exposure in female cocaine abusers. PLoS One 6(2):e16573. doi:10.1371/journal.pone.0016573
Volkow ND, Wang GJ, Fowler JS, Tomasi D, Telang F (2011b) Addiction: beyond dopamine reward circuitry. Proc Natl Acad Sci USA 108(37):15037–15042. doi:10.1073/pnas.1010654108
Wagner T, Fregni F, Fecteau S, Grodzinsky A, Zahn M, Pascual-Leone A (2007) Transcranial direct current stimulation: a computer-based human model study. Neuroimage 35(3):1113–1124. doi:10.1016/j.neuroimage.2007.01.027
Weiss F (2005) Neurobiology of craving, conditioned reward and relapse. Curr Opin Pharmacol 5(1):9–19. doi:10.1016/j.coph.2004.11.001
Worrell GA, Lagerlund TD, Sharbrough FW, Brinkmann BH, Busacker NE, Cicora KM, O’Brien TJ (2000) Localization of the epileptic focus by low-resolution electromagnetic tomography in patients with a lesion demonstrated by MRI. Brain Topogr 12(4):273–282
Zago-Gomes Mda P, Nakamura-Palacios EM (2009) Cognitive components of frontal lobe function in alcoholics classified according to Lesch’s typology. Alcohol Alcohol 44(5):449–457. doi:10.1093/alcalc/agp043
Acknowledgments
I want to thank patients and families who agreed to participate in this study. I also want to thank José Luiz Aranda who acquired the MRI data, the Greenhouse Clinic team, especially to Dr. Luis Henrique Casagrande, who allowed us to run this study in patients from this Clinic for Treatment of Mental Disorders and Drug Dependence, to use its facilities, and made all effort to help us. This work was supported by Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) (Grants numbers 475232/2013-5; 443824/2014-2 and 466650/2014-0 to E.M.N.P.). E.M.N.P. was recipient of researcher capixaba fellowship from Fundação de Amparo à Pesquisa do Espírito Santo (FAPES) and is now recipient of researcher fellopship from Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) (proc. 304374/2014-8).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors reported no financial interests or potential conflicts of interest.
Rights and permissions
About this article
Cite this article
Nakamura-Palacios, E.M., Lopes, I.B.C., Souza, R.A. et al. Ventral medial prefrontal cortex (vmPFC) as a target of the dorsolateral prefrontal modulation by transcranial direct current stimulation (tDCS) in drug addiction. J Neural Transm 123, 1179–1194 (2016). https://doi.org/10.1007/s00702-016-1559-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-016-1559-9