Abstract
Glutamate is the major excitatory neurotransmitter of the Central Nervous System (CNS), and it is crucially needed for numerous key neuronal functions. Yet, excess glutamate causes massive neuronal death and brain damage by excitotoxicity—detrimental over activation of glutamate receptors. Glutamate-mediated excitotoxicity is the main pathological process taking place in many types of acute and chronic CNS diseases and injuries. In recent years, it became clear that not only excess glutamate can cause massive brain damage, but that several types of anti-glutamate receptor antibodies, that are present in the serum and CSF of subpopulations of patients with a kaleidoscope of human neurological diseases, can undoubtedly do so too, by inducing several very potent pathological effects in the CNS. Collectively, the family of anti-glutamate receptor autoimmune antibodies seem to be the most widespread, potent, dangerous and interesting anti-brain autoimmune antibodies discovered up to now. This impression stems from taking together the presence of various types of anti-glutamate receptor antibodies in a kaleidoscope of human neurological and autoimmune diseases, their high levels in the CNS due to intrathecal production, their multiple pathological effects in the brain, and the unique and diverse mechanisms of action by which they can affect glutamate receptors, signaling and effects, and subsequently impair neuronal signaling and induce brain damage. The two main families of autoimmune anti-glutamate receptor antibodies that were already found in patients with neurological and/or autoimmune diseases, and that were already shown to be detrimental to the CNS, include the antibodies directed against ionotorpic glutamate receptors: the anti-AMPA-GluR3 antibodies, anti-NMDA-NR1 antibodies and anti-NMDA-NR2 antibodies, and the antibodies directed against Metabotropic glutamate receptors: the anti-mGluR1 antibodies and the anti-mGluR5 antibodies. Each type of these anti-glutamate receptor antibodies is discussed separately in this very comprehensive review, with regards to: the human diseases in which these anti-glutamate receptor antibodies were found thus far, their presence and production in the nervous system, their association with various psychiatric/behavioral/cognitive/motor impairments, their possible association with certain infectious organisms, their detrimental effects in vitro as well as in vivo in animal models in mice, rats or rabbits, and their diverse and unique mechanisms of action. The review also covers the very encouraging positive responses to immunotherapy of some patients that have either of the above-mentioned anti-glutamate receptor antibodies, and that suffer from various neurological diseases/problems. All the above are also summarized in the review’s five schematic and useful figures, for each type of anti-glutamate receptor antibodies separately. The review ends with a summary of all the main findings, and with recommended guidelines for diagnosis, therapy, drug design and future investigations. In the nut shell, the human studies, the in vitro studies, as well as the in vivo studies in animal models in mice, rats and rabbit revealed the following findings regarding the five different types of anti-glutamate receptor antibodies: (1) Anti-AMPA-GluR3B antibodies are present in ~25–30 % of patients with different types of Epilepsy. When these anti-glutamate receptor antibodies (or other types of autoimmune antibodies) are found in Epilepsy patients, and when these autoimmune antibodies are suspected to induce or aggravate the seizures and/or the cognitive/psychiatric/behavioral impairments that sometimes accompany the seizures, the Epilepsy is called ‘Autoimmune Epilepsy’. In some patients with ‘Autoimmune Epilepsy’ the anti-AMPA-GluR3B antibodies associate significantly with psychiatric/cognitive/behavior abnormalities. In vitro and/or in animal models, the anti-AMPA-GluR3B antibodies by themselves induce many pathological effects: they activate glutamate/AMPA receptors, kill neurons by ‘Excitotoxicity’, and/or by complement activation modulated by complement regulatory proteins, cause multiple brain damage, aggravate chemoconvulsant-induced seizures, and also induce behavioral/motor impairments. Some patients with ‘Autoimmune Epilepsy’ that have anti-AMPA-GluR3B antibodies respond well (although sometimes transiently) to immunotherapy, and thanks to that have reduced seizures and overall improved neurological functions. (2) Anti-NMDA-NR1 antibodies are present in patients with autoimmune ‘Anti-NMDA-receptor Encephalitis’. In humans, in animal models and in vitro the anti-NMDA-NR1 antibodies can be very pathogenic since they can cause a pronounced decrease of surface NMDA receptors expressed in hippocampal neurons, and also decrease the cluster density and synaptic localization of the NMDA receptors. The anti-NMDA-NR1 antibodies induce these effects by crosslinking and internalization of the NMDA receptors. Such changes can impair glutamate signaling via the NMDA receptors and lead to various neuronal/behavior/cognitive/psychiatric abnormalities. Anti-NMDA-NR1 antibodies are frequently present in high levels in the CSF of the patients with ‘Anti-NMDA-receptor encephalitis’ due to their intrathecal production. Many patients with ‘Anti-NMDA receptor Encephalitis’ respond well to several modes of immunotherapy. (3) Anti-NMDA-NR2A/B antibodies are present in a substantial number of patients with Systemic Lupus Erythematosus (SLE) with or without neuropsychiatric problems. The exact percentage of SLE patients having anti-NMDA-NR2A/B antibodies varies in different studies from 14 to 35 %, and in one study such antibodies were found in 81 % of patients with diffuse ‘Neuropshychiatric SLE’, and in 44 % of patients with focal ‘Neuropshychiatric SLE’. Anti-NMDA-NR2A/B antibodies are also present in subpopulations of patients with Epilepsy of several types, Encephalitis of several types (e.g., chronic progressive limbic Encephalitis, Paraneoplastic Encephalitis or Herpes Simplex Virus Encephalitis), Schizophrenia, Mania, Stroke, or Sjorgen syndrome. In some patients, the anti-NMDA-NR2A/B antibodies are present in both the serum and the CSF. Some of the anti-NMDA-NR2A/B antibodies cross-react with dsDNA, while others do not. Some of the anti-NMDA-NR2A/B antibodies associate with neuropsychiatric/cognitive/behavior/mood impairments in SLE patients, while others do not. The anti-NMDA-NR2A/B antibodies can undoubtedly be very pathogenic, since they can kill neurons by activating NMDA receptors and inducing ‘Excitotoxicity’, damage the brain, cause dramatic decrease of membranal NMDA receptors expressed in hippocampal neurons, and also induce behavioral cognitive impairments in animal models. Yet, the concentration of the anti-NMDA-NR2A/B antibodies seems to determine if they have positive or negative effects on the activity of glutamate receptors and on the survival of neurons. Thus, at low concentration, the anti-NMDA-NR2A/B antibodies were found to be positive modulators of receptor function and increase the size of NMDA receptor-mediated excitatory postsynaptic potentials, whereas at high concentration they are pathogenic as they promote ‘Excitotoxcity’ through enhanced mitochondrial permeability transition. (4) Anti-mGluR1 antibodies were found thus far in very few patients with Paraneoplastic Cerebellar Ataxia, and in these patients they are produced intrathecally and therefore present in much higher levels in the CSF than in the serum. The anti-mGluR1 antibodies can be very pathogenic in the brain since they can reduce the basal neuronal activity, block the induction of long-term depression of Purkinje cells, and altogether cause cerebellar motor coordination deficits by a combination of rapid effects on both the acute and the plastic responses of Purkinje cells, and by chronic degenerative effects. Strikingly, within 30 min after injection of anti-mGluR1 antibodies into the brain of mice, the mice became ataxic. Anti-mGluR1 antibodies derived from patients with Ataxia also caused disturbance of eye movements in animal models. Immunotherapy can be very effective for some Cerebellar Ataxia patients that have anti-mGluR1 antibodies. (5) Anti-mGluR5 antibodies were found thus far in the serum and CSF of very few patients with Hodgkin lymphoma and Limbic Encephalopathy (Ophelia syndrome). The sera of these patients that contained anti-GluR5 antibodies reacted with the neuropil of the hippocampus and cell surface of live rat hippocampal neurons, and immunoprecipitation from cultured neurons and mass spectrometry demonstrated that the antigen was indeed mGluR5. Taken together, all these evidences show that anti-glutamate receptor antibodies are much more frequent among various neurological diseases than ever realized before, and that they are very detrimental to the nervous system. As such, they call for diagnosis, therapeutic removal or silencing and future studies. What we have learned by now about the broad family of anti-glutamate receptor antibodies is so exciting, novel, unique and important, that it makes all future efforts worthy and essential.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Glutamate and its receptors
Glutamate and its receptors are essential for the healthy brain
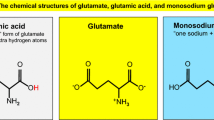
Glutamate is the major excitatory neurotransmitter in the Central Nervous System (CNS) (Meldrum 2000; Platt 2007). There, glutamate is stored in vesicles in pre-synaptic cells within chemical synapses, and upon nerve electrical impulses glutamate is released from these vesicles, binds its receptors expressed on the post-synaptic cells, and activates them, leading eventually to several key effects which are absolutely essential for the healthy brain to perform its multiple tasks.
Glutamate and its various types of receptors are key players in most if not all the neurological functions. Because of its role in synaptic plasticity, glutamate is involved in cognitive functions like learning and memory. In addition, glutamate plays an important role in the regulation of growth cones and synaptogenesis during brain development, and it mediates many other types of neuronal processes.
Although glutamate mediates synaptically confined point-to-point transmission, the recent visualization of extrasynaptic glutamate dynamics in brain tissues supports the suggestion that under certain conditions glutamate may escape from the synaptic cleft (glutamate spillover), accumulate in the extrasynaptic space, and mediate volume transmission to regulate important brain functions (Okubo et al. 2010).
Glutamate has many types and subtypes of glutamate receptors (GluRs), belonging to two main families. First, the Ionotropic glutamate receptors (iGluRs), which are ion channel receptors that are activated by glutamate. There are three main types of iGluRs: The AMPA, NMDA and Kainate receptors, and each of these iGluR types has several subtypes.
Second, the Metabotropic glutamate receptors (mGluRs), which are G-protein coupled receptors that are activated by glutamate. There are eight different types of mGluRs, labeled mGluR1 to mGluR8, which are divided into three major groups: mGluR I, II and III. The mGluR types are grouped based on the receptor structure and physiological activity. The mGluRs are further divided into subtypes, such as mGluR7a and mGluR7b.
The Ionotropic and Metabotropic GluRs are discussed in further detail in part 1.2.
The Ionotropic glutamate receptors (iGluRs)
The Ionotropic GluRs are membrane-spanning multimeric assemblies of four subunits, i.e. tetrameric receptors. They are subdivided into three groups according to their pharmacology, structural similarities, and the synthetic agonist that activates them in a specific and selective manner: either N-methyl-d-aspartate (NMDA), or Alpha-amino-3-hydroxy-5-methylisoxazole-4-propionic acid (AMPA), or 2-carboxy-3-carboxymethyl-4-isopropenylpyrrolidine (Kainate; KA).
Thus, while glutamate can bind and activate all types of iGluRs, there are commercially available glutamate agonists, antagonists and antibodies that bind preferentially selective iGluRs and either activate or block them.
On top of this and also the below very short summary on the different types of iGluR’s, the reader is referred to (Mayer 2011a, b) for recent papers on iGluRs structure and function.
A final note for this very general introduction: although a recent report suggested a novel nomenclature for ligand-gated ion channels, including iGluRs (Collingridge et al. 2009), in this review the former names attributed to these receptors and their subunits will be used as in the original studies.
The NMDA type of iGluRs
The NMDA receptors are the principal receptors in the CNS that control synaptic plasticity and memory (Li and Tsien 2009). NMDA iGluRs are hetero-oligomers composed of two obligatory NR1 subunits which are necessary for Ca2+ conductivity of the receptor’s ion channel, and of two regulatory subunits of the four existing ones: NR2A-D, which determine the electrophysiological and pharmacological properties of the NMDA receptor. The two NR1 subunits and the two NR2 subunits co-assemble to form a tetramer (Rosenmund et al. 1998). Besides the NR1 and NR2 subunits, there is also a third subunit: NR3A/B, which is a regulatory subunit that decreases the NMDA receptor’s channel activity (Das et al. 1998). The assembly of NR3 with NR1 creates a functional glycine receptor that is not activated by glutamate. Importantly, the activation of the NMDA iGluRs requires the binding of two different agonists to two different subunits: the binding of glutamate to the NR2 subunit, and the binding of glycine to the NR1 subunit (Kew and Kemp 2005). In addition, membrane depolarization is needed to abrogate the blockade of the NMDA receptors by Mg2+, allowing the flow of the voltage-dependent Na+ ions and small amounts of Ca2+ ions into the cell (i.e. inward Ca2+ [iCa2+] currents), and of K+ ions out of the cell (i.e., outward K+ currents).
The AMPA type of iGluRs
The AMPA receptors are important for plasticity and synaptic transmission at many postsynaptic membranes. AMPA iGluRs are homo- or hetero-oligomers composed of the GluR1-GluR4 subunits that assemble as functional tetramers (Rosenmund et al. 1998) containing four sites to which glutamate or AMPA receptor agonists can bind (Mayer 2005). The ligand binding site of the AMPA receptor is formed by the N-tail and the extracellular loop between the third and fourth transmembrane domains, which move towards each other to open the channel pore following ligand binding. The iGluR channel opens when two sites are occupied (Platt 2007) and increases its current as more binding sites are engaged (Rosenmund et al. 1998). Permeability of AMPA receptors to Ca2+ is governed by the GluR2 subunit, since the presence of a GluR2 subunit in the receptor renders the channel impermeable to Ca2+. Native AMPA receptors contain GluR2 and are therefore impermeable to Ca2+ ions (Kew and Kemp 2005). Gating of the AMPA receptors by glutamate is extremely fast, in contrast to the slow gating of the NMDA receptors (Dingledine et al. 1999). The different affinities of glutamate for AMPA vs. NMDA receptors have an important functional consequence: as both types of iGluRs are co-localized at neuronal synapses, the fast activation and opening of AMPA receptors alleviate the Mg2+ block of NMDA receptors to facilitate their activation (Dingledine et al. 1999).
The Kainate type of iGluRs
The KA receptors have a somewhat more limited distribution in the brain compared to AMPA and NMDA receptors (Hollmann and Heinemann 1994). KA receptors play a role in both pre and postsynaptic neurons (Huettner 2003) and, interestingly, they can lead to either excitation or inhibition, depending on their location. Thus, the presynaptic KA receptors are implicated in inhibitory neurotransmission, by modulating the release of the inhibitory neurotransmitter Gamma-Amino-Butyric Acid (GABA), while the postsynaptic KA receptors are involved in excitatory neurotransmission. The ion channel formed by KA receptors is permeable to Na+ and K+ ions, but impermeable to Ca2+. KA receptors are composed of tetrameric assemblies: GluR5-7 subunits that can form homomeric functional receptors, as well as combine with KA1 and KA2 to form heteromeric receptors with distinct pharmacological properties. The KA1 and KA2 subunits themselves do not form homomeric functional receptors (Keinanen et al. 1990; Lerma 2006).
The Metabotropic glutamate receptors (mGluRs)
The mGluRs are involved in a variety of functions in the central and peripheral nervous systems, such as learning, memory, anxiety and perception of pain (Ohashi et al. 2002). The mGluRs are found in pre and postsynaptic neurons in synapses of the hippocampus, cerebellum and the cerebral cortex (Hinoi et al. 2001), as well as in other parts of the brain, and in peripheral tissues (Chu and Hablitz 2000). Similar to other types of Metabotropic receptors, mGluRs have seven transmembrane domains that span the cell membrane (Platt 2007). Unlike iGluRs, mGluRs are not ion channels but rather lead, upon their ligation, to the subsequent activation of biochemical cascades that finally result in the modification of other proteins. This can lead to changes in the synapse’s excitability, for example, by presynaptic inhibition of neurotransmission (Sladeczek et al. 1993), or to the modulation and even induction of postsynaptic responses (Bonsi et al. 2005; Endoh 2004; Platt 2007). The mGluRs are subdivided into three groups, termed Group I, II and III mGluRs, based on sequence similarity, pharmacology and intracellular signaling mechanisms. Group I mGluRs (mGluR1 and mGluR5) are associated with Gq proteins and coupled to phospholipase C (PLC), while Group II (mGluR2 and mGluR3) and Group III mGluRs (mGluR4, mGluR6, mGluR7 and mGluR8) are associated with Gi and G0 proteins, and are negatively coupled to adenylate cyclase. These eight mGluRs are products of different genes (Pin and Bockaert 1995; Masu et al. 1991; Tanabe et al. 1992). The mGluRs function as homodimers, with two glutamate molecules being required for full receptor activation (Kew and Kemp 2005).
Excess glutamate induces ‘Excitotoxicity’—excessive stimulation of glutamate receptors leading to massive death of nerve cells
While the release of glutamate in the CNS upon a proper electrical signal is an essential, positive and normal process in the healthy brain, several different abnormal processes lead to rapid and excessive glutamate release and/or to its impaired uptake. Glutamate in excessive concentration is highly detrimental, as it leads to excessive stimulation of GluRs and subsequently to massive cell death in the CNS (Meldrum 1994, 2000). This pathological process by which nerve cells are killed by excessive stimulation of GluRs is called ‘Excitotoxicity’ (Olney 1990; Ankarcrona et al. 1995). In general terms, the scenario of the pathological events leading to ‘Excitotoxicity’ is the following: during normal conditions, glutamate’s concentration can be increased up to 1 mM in the synaptic cleft, which is rapidly decreased in the lapse of milliseconds. When glutamate’s concentration around the synaptic cleft cannot be decreased and reaches higher levels than the ‘allowed’ levels, glutamate accumulation leads to overstimulation of postsynaptic GluRs with intracellular Ca2+ ions overload and neuronal cell death. The abnormally high level of Ca2+ that enter the cells (i.e. the Ca2+ influx) activates a number of enzymes, including phospholipases, endonucleases, and also proteases such as calpain. These enzymes go on to damage several cell structures such as components of the cytoskeleton, membrane and DNA, and eventually kill the cells (Manev et al. 1989).
Excess glutamate can induce cell death either by early necrosis or by delayed apoptosis, and the mitochondrial function is a critical factor that determines the mode of neuronal death due to ‘Excitotoxicity’ (Ankarcrona et al. 1995).
‘Excitotoxicity’ is caused not only by pathological high levels of glutamate, but also by ‘Excitotoxins’ like NMDA and Kainic acid that bind to NMDA and Kainate iGluRs respectively.
Glutamate-mediated ‘Excitotoxicity’ contributes to, and is responsible for, a handful of pathologies in the CNS among them: Spinal cord injury, Stroke, Traumatic brain injury, Epilepsy (status epilepticus), and Neurodegenerative diseases in the CNS such as Multiple Sclerosis, Alzheimer’s disease, Amyotrophic Lateral Sclerosis (ALS), Parkinson’s disease and Huntington’s disease. Glutamate-mediated ‘Excitotoxicity’ also plays a role in Alcoholism or alcohol withdrawal and especially in Benzodiazepine withdrawal, in hearing loss (through noise overexposure or ototoxicity), in hypoglycemia and in various other human pathologies (Meldrum 1994, 2000).
Anti-AMPA-GluR3B antibodies, directed against the ‘B peptide’ (amino acids 372–395) of the GluR3 subunit of the AMPA ionotropic glutamate receptors, are present in ~30 % of Epilepsy patients, activate glutamate/AMPA receptors in neurons, kill neurons, cause multiple brain damage and cognitive/behavioral/motor impairments in animal models, and associate with neurological, psychiatric and behavior impairments in Epilepsy patients
Anti-glutamate receptor antibodies (anti-GluR antibodies) of several types are present in subpopulations of patients with different neurological diseases, as summarized in Fig. 1. Anti-GluR antibodies directed specifically against the ‘B peptide’—amino acids 372–395 of the GluR3 subunit of the AMPA ionotropic glutamate receptors, i.e. anti-AMPA-GluR3 antibodies, were found thus far only in patients with Epilepsy, in contrast to the other types of anti-glutamate receptor antibodies discussed later in this review that are present in various other human neurological diseases, as shown schematically in Fig. 1. The summary of the main features and effects of the anti-AMPA-GluR3B antibodies in Epilepsy patients and in animal models in mice, rat and rabbits are summarized in Fig. 2.
The GluR3 subunit of Glutamate/AMPA receptors
The GluR3 subunit is important for the signaling of the glutamate/AMPA receptors. The modulation in the expression levels of the GluR3 receptor complex, and its dynamic trafficking between the surface membrane and the intracellular organelles play an important role in key physiological brain functions, like memory processes, and also in some pathological conditions in the brain, among them: Epilepsy, Schizophrenia and mood disorders, Diabetic neuropathy and others (Falsafi et al. 2012; Balosso et al. 2009; Miyamoto et al. 2012; Hu et al. ;Porter et al. 2006; Mathern et al. 1998; Beneyto et al. 2007; Tomiyama et al. 2005; Dracheva et al. 2005).
The B peptide of GluR3 named the ‘GluR3B peptide’
The GluR3B peptide is a 24-amino acid (aa) long peptide that corresponds to extracellular aa 372–395 of GluR3, with a sequence of NEYERFVPFSDQQISNDSSSSENR. The GluR3B peptide has a unique topographical location: it is positioned within the iGluR at a hinge region, linking two modular regions of the GluR3 extracellular domain. Interestingly, it is postulated that this unique position of the GluR3B peptide might contribute to: (1) its immunogenicity, i.e. to the fact it ‘looks’ to the immune system like a foreign antigen and as such stimulates the production of autoimmune anti-AMPA-GluR3B antibodies directed against it (discussed in detail in parts 3.1, 3.2, 3.3, 3.4, 3.5, 3.6, 3.7), and (2) to the activation and opening of the glutamate/AMPA receptor’s ion channel by these autoimmune anti-AMPA-GluR3B antibodies (Basile et al. 2001; Carlson et al. 1997; Cohen-Kashi Malina et al. 2006; Koustova et al. 2001; Levite et al. 1999; Twyman et al. 1995) (discussed in detail in part 3.6 below).
In their paper, Carlson et al. (Carlson et al. 1997) write the following, which gives an important insight into the B peptide (copied as is, for the accurate description of these important findings): “We reported (Twyman et al. 1995) that antibodies to a sub region of the glutamate receptor (GluR) subunit GluR3 termed GluR3B (amino acids 372–395), act as highly specific GluR agonists. In this study, we produced additional rabbit anti-GluR3B-specific antibodies, ranked them according to their ability to function as GluR agonists, and characterized the immunoreactivity using deletion and alanine substitution mutagenesis. These anti-GluR3B antibodies bound to a subset of the residues in GluR3B (amino acids 372–386), of which glutamate 375, valine 378, proline 379, and phenylalanine (Phe) 380 were preferred. The level of GluR activation correlated with the binding of the antibody to Phe-380, which suggests that the immunoreactivity directed toward Phe-380 is an index for the anti-GluR agonist potential. Since the identity of this residue varies between respective GluR subunits, this suggested that this residue may be important for imparting antibody subunit specificity. To test this possibility, the alanine in GluR1 was converted to a phenylalanine, which extended the subunit specificity from GluR3 to the modified GluR1. We conclude that antibody contacts with key residues in the GluR3B region define a novel GluR subunit-specific agonist binding site and impart subunit-specific immunoreactivity” (Carlson et al. 1997).
Anti-AMPA-GluR3 antibodies and anti-AMPA-GluR3B antibodies are present in ~25–30% of Epilepsy patients suffering from different types of Epilepsy
Pooling together all the evidences reveled so far in different laboratories on the presence of anti-AMPA-GluR3B antibodies in various Epilepsy patients, we reached a total number of 315 patients tested altogether, out of which 87 (27 %) were found to have such autoimmune antibodies. Thus, according to the studies done so far ~25–30 % of patients with different types of Epilepsy have anti-AMPA-GluR3B antibodies in their serum (see Table 1 in (Levite and Ganor 2008) and the studies cited therein: (Andrews and McNamara 1996; Antozzi et al. 1998; Rogers et al. 1994; Twyman et al. 1995); {Levite 2002 #253; Wiendl et al. 2001 #396; Mantegazza et al. 2002 #269; Baranzini et al. 2002 #37; Ganor et al. 2004 #152; Ganor et al. 2005a #148; Ganor et al. 2005b #153; Ganor et al. 2005d #155; Ganor 2005 #151; Roubertie et al. 2005 #330; Feichtinger et al. 2006 #129; Solaro et al. 2006 #347; Tziperman et al. 2007 #374}, and our newest study (Goldberg-Stern et al. 2014).
The below paragraphs summarize the main studies on this topic.
In the pioneering study by Rogers et al. (1994), anti-AMPA-GluR3 antibodies were found in three out of four patients with Rasmussen’s Encephalitis (RE)—a rare and very severe childhood Epilepsy with unknown etiology (Rasmussen et al. 1958). Later, several studies confirmed the presence of anti-AMPA-GluR3 antibodies in most RE patients, but showed that such antibodies are neither restricted nor specific to RE, as they are clearly found also in the serum and/or Cerebrospinal fluid (CSF) of patients with additional types of Epilepsy, among them: non-inflammatory focal Epilepsy (Wiendl et al. 2001), early onset and intractable seizures (Mantegazza et al. 2002), and Partial and Generalized Epilepsy (Ganor et al. 2004, 2005a, b, d Goldberg-Stern et al. 2014). Thus, subpopulations of patients with various types of Epilepsy have elevated levels of autoimmune anti-AMPA-GluR3B antibodies in their serum ± CSF. Importantly, the anti-GluR3B antibodies can be very pathogenic to the CNS, as they can activate AMPA receptors, kill neurons, damage several brain regions and induce behavioral/cognitive/motor abnormalities, all of which will be discussed in detail in parts 3.6 and 3.7. Based on all that, and also on the positive responses to immunotherapy of some patients having anti-AMPA-Glu3B antibodies (discussed in part 3.8), it is recommended to indeed treat patients having such antibodies, especially in their CSF, with immunotherapy (as discussed later in part 3.8, and recommended in part 10.2).
In further detail, Wiendl et al. (2001) tested for anti-AMPA-GluR3 antibodies in the serum and CSF of eight patients with RE, 40 patients with non-inflammatory focal Epilepsy, and 104 patients with various neurologic diseases. Antibodies against different peptides derived from various portions of GluR3 were detectable in a significantly higher number of patients with focal Epilepsy than in those with other neurologic diseases, but these antibodies were clearly not specific for RE. Subsequently, Mantegazza et al. (2002) investigated the presence of anti-AMPA-GluR3 antibodies directed specifically against either peptide A—aa 245–274 of GluR3, or peptide B—aa 372–395 of GluR3, namely anti-AMPA-GluR3A antibodies and anti-AMPA-GluR3A antibodies, respectively, in patients with RE (n = 11), Partial or Generalized Epilepsy (n = 85) or other neurological diseases not associated with Epilepsy (n = 30). Anti-AMPA-GluR3 antibodies were detected in some of the Epilepsy patients, and once again they were not specific for RE. Particularly high titers of anti-AMPA-GluR3 antibodies characterized a subgroup of non-RE patients with ‘catastrophic’ Epilepsy. The anti-AMPA-GluR3B antibodies were significantly associated with frequent seizures compared to occasional or drug-controlled seizures (Mantegazza et al. 2002).
Bernasconi et al. (2002) then found anti-AMPA-GluR3 antibodies in 82 % of the patients with RE, and in 64 % of the patients with Partial Epilepsy that were included in their study.
In several later studies performed in our own laboratory (Ganor et al. 2004, 2005a, b, d) (Goldberg-Stern et al. 2014), anti-AMPA-GluR3 antibodies were found in many more patients with different types of Epilepsy.
In one of our studies (Ganor et al. 2004) we tested six Epilepsy patients with RE and 71 patients with other epilepsies for the presence in the serum of several types of autoimmune antibodies which included the following: (1) anti-AMPA-GluR3B antibodies, (2) anti-double-stranded DNA (dsDNA) antibodies—the hallmark of the autoimmune disease Systemic Lupus Erythematosus (SLE), and (3) few additional autoimmune antibodies found in some ‘classical’ autoimmune diseases, among them antibodies directed against: glutamic acid-decarboxylase, cardiolipin, beta2-glycoprotein-I and nuclear antigens SS-A and RNP-70. In this study, we also tested the ability of the serum and CSF of the Epilepsy patients to kill neurons in vitro in tissue culture. We found significantly elevated levels of specific anti-AMPA-GluR3B antibodies in the sera of five of six (83 %) RE patients, and in the sera of 17 of 71 (24 %) patients with other types of Epilepsy, compared to 49 neurologically healthy control individuals that did not have elevated levels of such antibodies. Testing the CSF samples available only from four RE patients (but unfortunately not from any other Epilepsy patient included in this study), we found that all of them indeed had significantly elevated levels of anti-AMPA-GluR3B antibodies in their CSF, compared with seven control CSF samples. Interestingly, in two RE patients, the level of anti-AMPA-GluR3B antibodies decreased drastically in the CSF following functional hemispherotomy, in association with seizure cessation and neurological improvement (Ganor et al. 2004).
In this study, we further found that the serum and CSF of two RE patients, and the serum of 12 of 71 (17 %) patients with other types of Epilepsy, contained also elevated levels of anti-dsDNA antibodies. Furthermore, the sera (but not the CSF) of some RE patients contained also clinically elevated levels of autoimmune antibodies directed against glutamic acid decarboxylase, cardiolipin, beta2-glycoprotein-I and nuclear antigens SS-A and RNP-70, showing that some patients have a broad spectrum ‘Autoimmune Epilepsy’ and various types of autoimmune antibodies, as often occurs in ‘classical’ autoimmune diseases (Ganor et al. 2004).
In another study (Ganor et al. 2005b), we tested 82 patients with different types of Epilepsy and 49 neurologically intact non-epileptic controls for the presence of anti-AMPA-GluR3B antibodies, anti-NMDA-NR2A antibodies, and anti-dsDNA antibodies. Anti-AMPA-GluR3B antibodies were found in 17 of 82 (21 %) of the Epilepsy patients. Anti-NMDA-R2A antibodies were found in 15 of 82 (18 %) of the Epilepsy patients, while anti-dsDNA antibodies were found in 13 of 80 (16 %) of the patients. Interestingly, most of the Epilepsy patients had only one type of these autoimmune antibodies, arguing against cross-reactivity. Furthermore, most of the Epilepsy patients that had anti-glutamate receptor antibodies—either anti-AMPA-GluR3B antibodies or anti-NMDA-NR2A antibodies—did not have a history of brain damage, febrile convulsions, early onset Epilepsy, acute Epilepsy or intractable seizures (Ganor et al. 2005b).
In our third and most recent study (Goldberg-Stern et al. 2014), we tested another pool of 14 relatively young consecutive Epilepsy patients (all under 30 years of age) with different types of chronic intractable Epilepsy, for the presence of anti-AMPA-GluR3B antibodies in the serum. We found that 7 of 14 (50 %) of the patients had elevated levels of anti-AMPA-GluR3B antibodies (p = 0.0061), of which six had symptomatic etiology and one had cryptogenic etiology. Interestingly, and as will be discussed separately later in part 3.5, in this study we also found a significant association between the presence of the anti-AMPA-GluR3B antibodies in the serum, and various cognitive/psychiatric/behavioral abnormalities expressed by the Epilepsy patients. Thus, among the 21 patients with anti-AMPA-GluR3B antibodies, 19 patients (91 %) had learning problems, 16 (78 %) attention problems, and 15 (71 %) psychiatric problems. In contrast, among the 20 patients without anti-AMPA-GluR3B antibodies, only 6 (27 %) had learning problems (p < 0.0001), 4 (20 %) attention problems (p = 0.0017), and 2 (10 %) psychiatric problems (p < 0.0001) (Goldberg-Stern et al. 2014).
In contrast to all the studies described above, that clearly detected anti-AMPA-GluR3B antibodies in a significant proportion of Epilepsy patients, the study of Watson et al. (2004) failed to detect such antibodies in most of the Epilepsy patients they studied. In further detail, Watson et al. looked for serum GluR3 IgG in 30 patients with RE, 49 patients with intractable Epilepsy and 23 healthy individuals, using ELISA with the GluR3B peptide, Western blot analysis of recombinant full length GluR3, immunoprecipitation of [35S]- and [125I]-labeled GluR3 extracellular domains, immunohistochemistry on rat brain sections, and electrophysiology of GluR3 expressed in Xenopus oocytes (Watson et al. 2004). Low levels of anti-AMPA-GluR3B antibodies were detected by ELISA in only 4 of the 79 Epilepsy patients: 2 with RE and 2 with intractable Epilepsy. The binding to GluR3B detected in the other sera was shown to be non-specific. One other patient with intractable Epilepsy had antibodies that bound to the recombinant GluR3 on Western blots. None of the patient’s sera tested precipitated either the [35S]- or the [125I]-labeled GluR3 domains, none bound to rat brain sections in a manner similar to rabbit antibodies to GluR3, and none of the nine sera affected the electrophysiologic function of GluR3. The authors of this study concluded that anti-AMPA-GluR3B antibodies are infrequently found in RE and in intractable Epilepsy.
Together, the summing of most of the studies described above shows that anti-AMPA-GluR3B antibodies are present in significant number of Epilepsy patients with different types of Epilepsy. In view of the detrimental effects of such antibodies in the CNS (described later in part 3.7), these antibodies must be taken into consideration once designing therapy for the patients that bear them in the serum and/or CSF.
Methodologies used thus far for the detection of anti-AMPA-GluR3 antibodies and anti-AMPA-GluR3B antibodies, or for demonstrating their activity
Several methodologies were used successfully thus far by different groups to demonstrate the presence or function of anti-AMPA-GluR3 antibodies and anti-AMPA-GluR3B antibodies. These are summarized in the coming paragraphs:
-
1.
ELISA specific for a large portion of GluR3, or only for the GluR3B peptide, was used successfully for detecting the specific binding of anti-AMPA-GluR3 antibodies and anti-AMPA-GluR3B antibodies present either in Epilepsy patients or in GluR3-immunized mice, rats and rabbits, to their respective GluR3 or GluR3B antigens, while not binding to control molecules (Antozzi et al. 1998; Feichtinger et al. 2006; Ganor et al. 2004, 2005a, b, c, d, 2014; Goldberg-Stern et al. 2014; Levite et al. 1999; Levite and Hermelin 1999; Mantegazza et al. 2002; Twyman et al. 1995; Watson et al. 2004). Such ELISAs indeed managed to detect specific anti-AMPA-GluR3B antibodies that did not cross-react with the control antigens used within the same tests.
-
2.
Immunoblots were used successfully for showing that serum containing anti-AMPA-GluR3 antibodies binds full length GluR3 expressed in its three-dimensional conformation in transfected HEK293 cells (Rogers et al. 1994).
-
3.
Western blots specific for GluR3 were used successfully for showing that antibodies present in the serum of Epilepsy patients bind GluR3-trpE fusion protein (Rogers et al. 1994; Watson et al. 2004).
-
4.
Immunocytochemistry was used successfully for showing that affinity-purified anti-AMPA-GluR3 antibodies derived from patients with RE, and also commercial anti-AMPA-GluR2/3 monoclonal antibody that served as positive control, bind to specific brain regions (Bernasconi et al. 2002; Rogers et al. 1994).
-
5.
Flow cytometry was used successfully for showing that anti-AMPA GluR3B antibodies bind: (1) GluR3 expressed in neurons, (2) the authentic GluR3 expressed in human and mouse T cells (called also T lymphocytes) which are the key cells of the adoptive immune system. Of note, we found that normal, autoimmune and cancerous T cells express high levels of glutamate/AMPA GluR3 on their cell surface (alike some neurons do), and that the direct binding of glutamate in low ~10 nM concentration to its AMPA receptors expressed in such T cells activates by itself several key T cell functions and features among them: adhesion to fibronectin and laminin, chemotactic migration and others (Ganor et al. 2003, 2007, 2009; Ganor and Levite 2012, 2014).
-
6.
Electrophysiology was used successfully for recording ion currents from neurons that express AMPA GluR3, or from cells transfected with AMPA GluR3, following the application of either anti-AMPA-GluR3 antibodies or anti-AMPA-GluR3B antibodies. Such electrophysiological evidences (discussed in further detail below, in part 3.6) were obtained successfully in several studies using different methods and different target tissue/organs (Carlson et al. 1997; Cohen-Kashi Malina et al. 2006; Koustova et al. 2001; Levite et al. 1999; Rogers et al. 1994; Twyman et al. 1995).
Anti-AMPA-GluR3B antibodies associate with psychiatric/cognitive/behavioral impairments in some Epilepsy patients
In our recently published paper (Goldberg-Stern et al. 2014), we describe a study of 41 Epilepsy patients: 21 patients in which we detected elevated levels of anti-AMPA-GluR3B antibodies in the serum, and 20 other age and sex matched Epilepsy patients in which we did not detect them. Of the 21 patients that had elevated levels of anti-AMPA-GluR3B antibodies, 6 had symptomatic Epilepsy, 7 had cryptogenic Epilepsy, and 8 had idiopathic Epilepsy. Of the 20 patients that did not have elevated levels of anti-AMPA-GluR3B antibodies, 16 had Epilepsy with idiopathic etiology, and 4 had non-idiopathic Epilepsy.
We then searched for possible association between the presence of anti-AMPA-GluR3B antibodies and: (1) the severity of the Epilepsy, (2) the psychiatric, cognitive or behavior abnormalities of some of the Epilepsy patients (Goldberg-Stern et al. 2014). We found that among the 21 patients that had elevated levels of anti-AMPA-GluR3B antibodies, the vast majority—19 of 21 (90 %)—had learning problems, most—16 of 21 (76 %)—had attention problems, and most again—15 of 21 (71 %)—had psychiatric problems (Goldberg-Stern et al. 2014). In contrast, among the 20 patients without elevated levels of anti-AMPA-GluR3B antibodies, only 6 of 20 (30 %) had learning problems (p < 0.0001), 5 of 20 (25 %) had attention problems (p = 0.0017), and 2 of 20 (10 %) had psychiatric problems (p < 0.0001) (Goldberg-Stern et al. 2014). These findings show a statistically significant association in the Epilepsy patients that were included in this study between the presence of anti-AMPA-GluR3B antibodies in the serum and their psychiatric, cognitive and/or behavior abnormalities. We hypothesize that this association could result from two alternative putative scenarios. According to the first scenario, the anti-AMPA-GluR3B antibodies come first, due to several putative etiological factors and events suggested schematically in (Levite and Ganor 2008), and once they are in the brain (due to either intrathecal production or migration from the periphery) they bind and activate AMPA receptors expressed in neurons, kill some of the neurons (by ‘Excitotoxicity’ and/or complement fixation), and by doing all this impair the normal brain function. Such CNS impairments can finally lead (directly or indirectly) to psychiatric/cognitive/behavior abnormalities impairments. Such a scenario can explain why psychiatric/cognitive/behavior abnormalities impairments are more frequent among Epilepsy patients that have anti-AMPA-GluR3B antibodies. According to the second scenario, the psychiatric/cognitive/behavior abnormalities come first, and these, by one way or another, increase the immunogenicity and antigenicity of the self AMPA receptors and of their GluR3B peptide. Once the GluR3B is ‘seen’ by the patient’s immune system as a foreign antigen, the immune system produces anti-AMPA-GluR3B antibodies directed against it. And then, if such autoimmune anti-AMPA-GluR3B antibodies are produced in the brain, or if they are produced in the periphery and enter the brain via a leaky BBB, they may bind and activate AMPA receptors in the CNS, kill neurons, and eventually induce further neurological impairments (Goldberg-Stern et al. 2014).
Our personal opinion is that the first scenario is the correct one, and also that the first scenario can lead to the second one. Having said that, it is important to bear in mind that human studies can not answer what comes first—the anti-GluR3B antibodies or the psychiatric/cognitive/behavior abnormalities. Only studies in animal models can do so.
Anti-AMPA-GluR3B antibodies bind the authentic GluR3 expressed in neurons and in T cells, and have a unique ability to activate the respective glutamate/AMPA receptors, open their ion channel and induce ion currents
Both anti-AMPA-GluR3 antibodies and anti-AMPA-GluR3B antibodies of human, rabbit, mouse and rat origin can bind neurons and/or specific brain regions and/or cells transfected with the authentic GluR3, and/or normal human T cells expressing GluR3, as revealed in vitro and in situ in several studies performed by different groups (Bernasconi et al. 2002 {Frassoni et al. 2001 #138}; Cohen-Kashi Malina et al. 2006; Ganor et al. 2009; Levite et al. 1999; Rogers et al. 1994; Twyman et al. 1995; Whitney and McNamara 2000).
Just few examples for the evidences of such binding are the following: (1) Anti-AMPA-GluR3 antibodies present in epileptic RE patients bound in vitro transfected cells that expressed GluR3 (Rogers et al. 1994), (2) Rabbit anti-AMPA-GluR3 antibodies bound cultured fetal mouse cortical neurons (Twyman et al. 1995), (3) Mice anti-AMPA-GluR3B antibodies, produced following immunization with the GluR3B peptide, bound cultured neurons, evoked GluR ion channel activity and killed neurons by ‘Excitotoxicity’ (Levite et al. 1999), (4) Sera of 82 % of patients with RE, and of 64 % of patients with Partial Epilepsy (PE) bound rat brain sections, as evident in immunohistoblots (Bernasconi et al. 2002). The histoblot analysis even showed positive staining in GluR3-specific and NMDA-specific regions of the rat’s brain, providing a comprehensive CNS immunolocalization (Bernasconi et al. 2002). Furthermore and of primary importance: the anti-AMPA-GluR3B antibodies not only bound neurons in specific brain regions and in vitro, but also possessed a unique ability to activate glutamate/AMPA receptors that contain the GluR3 subunit, leading to the elicitation of ion currents through the AMPA receptor ion channel (Basile et al. 2001; Carlson et al. 1997; Cohen-Kashi Malina et al. 2006; Gahring and Rogers 2002; Koustova et al. 2001; Levite et al. 1999; Levite and Ganor 2008; Twyman et al. 1995). Thus, the anti-AMPA-GluR3B antibodies acted as highly specific GluR agonists, despite the fact that they bound to a different binding site within the glutamate/AMPA receptor than glutamate itself.
For reminder, the GluR3B region corresponds to amino acids 372–395 of the GluR3 subunit.
The activation of AMPA receptors by the anti-AMPA-GluR3 antibodies was shown successfully by electrophysiological studies performed by few groups using different methods and different target tissue/organs.
Interestingly, as already cited in part 3, Carlson et al. (1997) found that the anti-AMPA-GluR3B antibodies bind to amino acids 372–386 of GluR3B, of which glutamate 375, valine 378, proline 379, and phenylalanine (Phe) 380 are preferred, and that the level of GluR activation by the anti-AMPA-GluR3B antibodies correlates with the binding of these antibodies to Phe-380. Carlson et al. (1997) concluded that the contact of anti-AMPA-GluR3B antibodies with key residues in the GluR3B region defines a novel GluR subunit-specific agonist binding site, and impart subunit-specific immunoreactivity.
In two of our own studies on the activation of the AMPA receptor by anti-AMPA-GluR3B antibodies, we found the evidences summarized in the coming paragraphs.
In the first study, we revealed that mouse anti-AMPA-GluR3B antibodies (produced following immunization of mice with the GluR3B peptide) evoked GluR/AMPA receptor ion channel activity in cultured neurons, and also killed neurons. These two effects were blocked by CNQX—a specific glutamate/AMPA receptor antagonist (Levite et al. 1999). In the second study, based on the fact that glutamate/AMPA receptors in vivo predominantly assemble into heteromeric receptor-channels, we studied whether affinity-purified anti-AMPA-GluR3B antibodies can activate by themselves homomeric and heteromeric GluR3 expressed in Xenopus oocytes. Indeed, we found that the anti-AMPA-GluR3B antibodies on their own activated both homomeric and heteromeric GluR3, without the requirement of any additional molecules of neuronal, glial or blood origin (Cohen-Kashi Malina et al. 2006). Furthermore, and arguing for the specificity of this effect, CNQX (the AMPA receptor antagonist) blocked almost completely the currents evoked by the anti-AMPA-GluR3B antibodies (Cohen-Kashi Malina et al. 2006).
How can anti-AMPA-GluR3B antibodies, that bind to the ‘B’ region of GluR3 which is remote from glutamate’s own binding site within the AMPA receptor, mimic glutamate and also activate the glutamate/AMPA receptor, induce ion currents and then kill the cells via ‘Excitotoxicity’? We postulated that upon binding to the GluR3B region, the anti-AMPA-GluR3B antibodies induce a conformational change that causes the closure of the bi-lobated S1-S2 agonist binding domain, which in turn causes a shift of the receptor channel equilibrium from a resting state to an open state, thereby activating the channel (Cohen-Kashi Malina et al. 2006).
Finally, it is interesting to bear in mind that by virtue of being activating antibodies that are able to stimulate the glutamate/AMPA receptor’s ion channel and elicit electrical activity, the anti-AMPA-GluR3B antibodies differ markedly from the blocking autoimmune antibodies found in various autoimmune diseases, such as the anti-nicotinic acetylcholine receptor antibodies in Myasthenia Gravis, the anti-voltage-gated calcium channels antibodies in Lambert Eaton, and the anti-voltage-gated potassium channels antibodies in Peripheral Nerve Hyperexcitability.
Anti-AMPA-GluR3B antibodies by themselves kill neurons via either ‘Excitotoxicity’ or complement fixation, change the susceptibility to PTZ-induced seizures, damage the brain, and induce cognitive/behavioral/motor impairments in vivo in rabbits, mice or rats
Several studies have shown that anti-AMPA-GluR3 antibodies or anti-AMPA-GluR3B antibodies can by themselves kill neurons by either ‘Excitotoxicity’ or complement-mediated mechanism, and by doing so induce multiple brain pathology and also behavioral impairments (Antozzi et al. 1998; Bernasconi et al. 2002; Carlson et al. 1997; Cohen-Kashi Malina et al. 2006; Frassoni et al. 2001; Gahring and Rogers 2002; Ganor et al. 2004, d, 2014; Ganor et al. 2005c; He et al. 1998; Koustova et al. 2001; Levite et al. 1999; Levite and Hermelin 1999; Mantegazza et al. 2002; Rogers et al. 1994; Roubertie et al. 2005; Solaro et al. 2006; Twyman et al. 1995; Whitney and McNamara 2000; Wiendl et al. 2001). By doing all that, the anti-AMPA-GluR3B antibodies can clearly be detrimental to the brain and contribute to the overall pathology of Epilepsy patients.
Together, the multiple evidences cited above show that anti-AMPA-GluR3B antibodies can activate AMPA receptors in vitro, kill neurons and damage the brain in vivo in mice, rats and rabbits. Additional findings made in these animal models are discussed in further detail in the following paragraphs, according to the animal model/species they were found in.
Anti-AMPA-GluR3B antibodies in rabbits
Anti-AMPA-GluR3 antibodies induce seizure-like behavior in rabbits.
In their original Science paper in 1994 Rogers et al. reported that during their efforts to raise antibodies to recombinant ionotropic GluRs of several types, behavior typical of seizures, and also inflammatory histopathology in the brain, were detected in two rabbits immunized with a portion of the GluR3 subunit—GluR3 amino acids 245–457 (Rogers et al. 1994). This did not happen in the rabbits that were immunized with the corresponding portions of the GluR1, GluR2 and GluR4 subunits. The brain abnormalities observed in the two GluR3-immunized rabbits resembled the abnormalities observed in epileptic RE patients, and suggested for the first time that autoimmune anti-AMPA-GluR3B antibodies may modulate neuronal excitability and contribute to Epilepsy, and also to inflammatory neuropathology.
Rabbit anti-AMPA-GluR3B antibodies function like glutamate/AMPA agonists and evoke ion currents.
In a later study, rabbit anti-AMPA-GluR3 antisera was tested on cultured fetal mouse cortical neurons. In a subset of kainate-responsive neurons, miniperfusion of the anti-AMPA-GluR3 antisera or IgG evoked ion currents that were blocked by CNQX. Immunoreactivity to synthetic peptides prepared to subregions GluR3A (GluR3 aa 245–274) and GluR3B (GluR3 aa 372–395) was present in the serum of the two rabbits. Preincubation with the GluR3B peptide, but not with the GluR3A peptide, blocked specifically the ion currents evoked by the anti-AMPA-GluR3 antisera or IgG. Similar receptor activation and anti-AMPA-GluR3 antibody reactivity were present in the sera of patients with active RE. These findings suggested that the anti-AMPA-GluR3 antibodies that were produced in rabbits function as glutamate agonists and may be highly specific neurotoxicants in some neurological diseases, primarily Epilepsy (Twyman et al. 1995).
Rabbit anti-AMPA-GluR3 antibodies kill neurons by a complement-dependent mechanism.
In yet another study on anti-AMPA-GluR3 antibodies in rabbits (He et al. 1998), a subset of the rabbits immunized with a GluR3 fusion protein developed a neurological disorder mimicking RE, and anti-AMPA-GluR3 IgG isolated from serum of both ill and healthy GluR3-immunized animals promoted death of cultured cortical cells by a complement-dependent mechanism. IgG immunoreactivity decorated neurons and their processes in the neocortex and hippocampus in ill, but not in healthy, rabbits. Moreover, both IgG and complement membrane attack complex (MAC) immunoreactivities were evident on neurons and their processes in the cortex of a subset of epileptic RE patients. He et al. (1998) suggested that access of IgG to epitopes in the CNS triggers complement-mediated neuronal damage, and contributes to the pathogenesis of both this animal model and the human Epilepsy RE.
Rabbit anti-AMPA-GluR3 antibodies cross-react with interferon alpha receptor (IFNAR-1).
In another study on rabbit anti-AMPA-GluR3 antibodies, a very surprising cross-reactivity between GluR3 and interferon alpha receptor (IFNAR-1) was revealed (Gahring et al. 1998). Moreover, the agonist-like anti-AMPA-GluR3 antibodies prepared in rabbits exhibited greater immunoreactivity towards the human IFNAR-1 than to GluR3. Since the antibodies prepared to a defined region of GluR3 reacted preferentially with an unrelated sequence in the human IFNAR-1, Gahring et al. (1998) proposed that the IFNAR-1 may be an heteroclitic antigen of GluR3.
Anti-AMPA-GluR3B antibodies in mice
Anti-AMPA-GluR3B antibodies were produced in five mouse strains following immunization with the GluR3B peptide, and then bound neurons, activated AMPA receptors, killed neurons by ‘Excitotoxicity’ and caused brain damage in vivo.
We developed the first and thus far the only existing mice model for GluR3B autoimmunity in mice, by immunizing five mouse strains: BALB/c, C3H/HeJ, SJL/J, C57BL/6 and DBA/J with the GluR3B peptide (NEYERFVPFSDQQISNDSSSSENR) emulsified in complete Freund’s adjuvant (CFA) (Levite et al. 1999; Levite and Hermelin 1999; Ganor et al. 2014).
In the first study, we investigated the GluR3B-immunized BALB/c, C3H/HeJ, SJL/J, and C57BL/6 mice for the development of: (1) Anti-AMPA-GluR3B antibodies, (2) Anti-AMPA-GluR3B T cells, (3) Clinical symptoms and abnormal behavior, (4) Brain pathology (Levite and Hermelin 1999). We found that following the immunization with the GluR3B peptide, high levels of specific anti-AMPA-GluR3B antibodies were produced in the BALB/c, C3H/HeJ and SJL/J mice, but not in the C57BL/6 mice. These findings indicated that the genetic background of the mice influenced their ability to mount a humoral autoimmune response towards the GluR3B peptide.
In a second study (Levite et al. 1999), we immunized C3H/HeJ mice with either of the two GluR3 specific peptides: GluR3A, or GluR3B, or with a control scrambled GluR3B peptide. The GluR3B-immunized mice developed high levels of anti-AMPA-GluR3B antibodies, while the GluR3A-immunized mice developed high titers of anti-AMPA-GluR3A antibodies. These two types of anti-AMPA-GluR3 antibodies did not cross-react with one another. Importantly, the anti-AMPA-GluR3B antibodies bound in vitro cultured neurons, activated the AMPA receptors and evoked GluR ion channel activity (Levite et al. 1999). Furthermore, the anti-AMPA-GluR3B antibodies killed in vitro cultured neurons by a mechanism of ‘Excitotoxicity’, which was independent of complement activation. Both the activation of the glutamate/AMPA receptor, and the neuronal death induced by anti-AMPA-GluR3B antibodies were blocked by CNQX—the specific glutamate/AMPA receptor antagonist. Purified anti-AMPA-GluR3B IgG antibodies retained the neuronal killing capacity, and the killing was completely and specifically blocked by pre-incubation of the anti-AMPA-GluR3B antibodies with the GluR3B peptide. This finding confirmed that the binding of anti-AMPA-GluR3B antibodies to the GluR3B peptide within the full length authentic AMPA receptor, is sufficient for the activation of the AMPA receptor by these antibodies, and for the induction of subsequent ion currents through the AMPA receptor’s ion channel. We further found that the excitotoxic neuronal death induced by the anti-AMPA-GluR3B antibodies took place primarily via apoptosis. Interestingly, in contrast to the anti-AMPA-GluR3B antibodies, the anti-AMPA-GluR3A antibodies did not activate the AMPA receptor, and also did not kill neurons, despite their ability to bind neurons. The control anti-scrambled GluR3B antibodies also had no effect, further confirming the specificity of the effects induced only by the anti-AMPA-GluR3B antibodies.
With regard to in vivo effects of the anti-GluR3B antibodies, the GluR3B-immunized mice exhibited several signs of brain pathology: (1) Thickening of the cerebral meninges—a phenomenon resembling the pathology observed in rabbits with RE symptoms, (2) Perivascular lympho-mononuclear cell infiltration, (3) Occasional pathologic gliosis in the cerebrum (observed only in few mice), (4) Cerebellar cortical abiotrophy, with loss of neurons from both the Purkinje cell layer (as described in paraneoplastic neurodegenerative syndromes) and the granule cell layer, (5) Moderate to severe spongiform degeneration. Representative photos of these brain pathologies are shown in Fig. 4 in (Levite et al. 1999).
In the third and most recent study (Ganor et al. 2014), we immunized DBA/2J mice with the GluR3B peptide emulsified in CFA, or for control with either OVA in CFA, CFA alone or PBS alone. The DBA/2J mouse is a widely used inbred mouse strain due to its unique characteristics, including increased susceptibility to audiogenic seizures at a young age. We found that most of the GluR3B-immunized DBA/J mice developed high titers of specific anti-AMPA-GluR3B antibodies, and that the presence of these antibodies worsened PTZ-induced seizures and also induced abnormal behavior in these mice, as will be described in further detail in the coming parts 3.7.2.1 and 3.7.2.2.
In this study, each experimental group consisted of 6–10 mice. Six out of the ten (60 %) of the GluR3B-immunized DBA/2J mice developed high titers of anti-AMPA-GluR3B antibodies, while two mice developed low levels of these antibodies, and another two failed to develop these antibodies altogether (Ganor et al. 2014).
In general, such heterogeneity in the levels of antibody production between individual mice of the same strain, sex and approximately the same age, following their immunization with the very same antigen is seen quiet often in many studies by many different groups, using different antigens and different strains of mice, and is still not well understood.
Importantly, high levels of anti-AMPA-GluR3B antibodies were not produced by any of the other control DBA/2J mice that were immunized with either OVA, CFA, or PBS only. Likewise, the OVA-immunized DBA/2J mice produced anti-OVA antibodies, while neither the GluR3B-immunized DBA/2J mice nor any of the other mice developed such antibodies. Together, these results demonstrated again the high specificity and non-cross-reactivity of the autoimmune antibodies produced in vivo in DBA/2J mice following the above-mentioned immunizations, and especially of the anti-AMPA-GluR3B antibodies (Ganor et al. 2014).
GluR3B-immunized DBA/2J mice that developed anti-AMPA-GluR3B antibodies show increased epileptic activity in response to the chemoconvulsant Pentylenetetrazole (PTZ), and the seizure score correlates with the levels of anti-AMPA-GluR3B antibodies.
We studied the response to the chemoconvulsant agent Pentylenetetrazole (PTZ) of the DBA/2J mice that were immunized with either the GluR3B peptide emulsified in CFA, or OVA in CFA, or CFA only, or PBS only (Ganor et al. 2014). As already described in the preceding part 3.7.2.1, 60 % of the GluR3B-immunized mice, and none of the mice in any of the other groups, developed high titers of specific and no cross-reactive anti-AMPA-GluR3B antibodies (Ganor et al. 2014). Of note, since Epilepsy is characterized by spontaneous recurrent seizures, most of the animal models that are used in Epilepsy research are models of epileptic seizures (acute or chronic) rather than models of Epilepsy (Loscher 2002). Yet, the PTZ model of acute seizures is still currently used in the initial steps of screening for new anti-epileptic drugs (AEDs) (Loscher 2002), and seemed to us reasonably suitable for determining the capacity of anti-AMPA-GluR3B antibodies to affect seizure threshold. Hence, the DBA/2 J mice in all the experimental groups received three injections of PTZ, at 5 weeks intervals, starting at 8 weeks following the last booster injection. Since two animals died following the first PTZ injection, since the mice got older along this long experiment, since the mice were subjected to multiple procedures thought out the study, and since we wanted to avoid non-specific death, we decided to decrease gradually by approximately 30 % the dose of PTZ from the first to the third PTZ injection. The pattern and severity of seizures developing in each individual mouse after each of these three PTZ injections were recorded carefully. Seizure activity was rated according to a well-accepted four phases scale, consisting of the following phases:
Phase 1—Hypoactivity: this phase is characterized by a progressive decrease in motor activity until the animal comes to rest in a crouched or prone position, with abdomen in full contact with the bottom of the cage;
Phase 2—Partial clonus: clonic seizure activity affecting the face, head, and/or forelimbs. Partial or focal seizures are brief, typically lasting for 1–2 s, and are often accompanied by vocalizations. Partial seizures occur either individually or in multiple discrete episodes before generalization;
Phase 3—Generalized clonus: sudden loss of upright posture, and whole body clonus involving all four limbs and tail, rearing, and autonomic sings;
Phase 4—Tonic–clonic (maximal) seizures: generalized seizures are characterized by tonic hindlimb extension. Tonic-clonic maximal seizures are usually associated with death. Latencies to hypoactivity (HA), partial clonus (PC), generalized clonus (GC), and maximal tonic-clonic (TC) behavioral seizures were recorded in all the experimental groups. The seizure severity was calculated with a quantitative seizure score, according to the following equation: seizure score = 0.1 × (1/HA latency) + 0.2 × (1/PC latency) + 0.3 × (1/GC latency) + 0.4 × (1/TC latency).
The results of this study (Ganor et al. 2014) showed that, as expected, in the group of anti-AMPA-GluR3B antibody-negative mice (i.e., all the control mice pooled together), the seizure scores and percentages of animals developing generalized seizures decreased in association with the reduction in the doses of PTZ administered during the first, second and third injections. Yet, in the group of anti-AMPA-GluR3B antibodies positive mice, reducing the PTZ doses during the second and third PTZ injections did not result in lower seizure scores, and also not in a lower percentage of animals developing generalized seizures. These two parameters remained high and unchanged in the second and third PTZ injection, compared to the same parameters in the first PTZ injection. The differences between the groups of anti-AMPA-GluR3B antibodies positive and negative mice were statistically significant for the second and third PTZ injections. These findings demonstrated that the mice that had anti-AMPA-GluR3B antibodies expressed an enhanced acute seizure response to PTZ.
We next found a significant linear correlation between the levels of the anti-AMPA-GluR3B antibodies in the serum of each mice, and the seizure score following the second and third PTZ applications. Together, these findings showed that anti-AMPA-GluR3B antibodies lowered seizure threshold in mice, and suggest that they may do so in humans too (Ganor et al. 2014).
Anti-AMPA-GluR3B antibodies cause cognitive/behavioral/motor problems in mice.
We next asked if the DBA/2J mice that had high titers of anti-AMPA-GluR3B antibodies (following immunization with the GluR3B peptide), compared to all the other control mice (described above in the last paragraphs of part 3.7.2.1, and in part 3.7.2.1), exhibit abnormal behavior (Ganor et al. 2014). The reason for asking if anti-AMPA-GluR3B antibodies can contribute to cognitive, psychiatric and/or behavioral impairments stems from such unresolved impairments in Epilepsy patients. Thus, Epilepsy of all types may be complicated by severe neurological, cognitive, psychiatric and behavioral problems, such as attention-deficit/hyperactivity disorder (ADD, ADHD), mood disorders, and abnormal learning and memory (Berg et al. 2008; Cahn-Weiner et al. 2009; Hermann et al. 1997; Hommet et al. 2006; Nicolai et al. 2006; Roebling et al. 2009; Shehata and Bateh Ael 2009). In fact, the psychiatric/cognitive/behavioral abnormalities can have an even greater adverse impact on the patient’s quality of life than the seizures themselves (Elger et al. 2004; Helmstaedter 2002; Jokeit and Ebner 2002). The nature of the relationship between these abnormalities and Epilepsy is still unclear (Jokeit and Ebner 2002; Fastenau et al. 2009; Kanner and Ostrovskaya 2008a, b). The neurological, cognitive psychiatric and behavioral problems of Epilepsy patients have been attributed many times to the cause, duration, or treatment of the seizures (Cheung et al. 2006; Hessen et al. 2006; Theodore et al. 1999). In addition, recent studies suggest that interictal EEG abnormalities (transient focal neural discharges lasting 50–200 ms) may be at least partly responsible for the cognitive abnormalities of some Epilepsy patients (Binnie 1993; Holmes and Lenck-Santini 2006; Kleen et al. 2010; Shewmon and Erwin 1988).
Back to our study in DBA/2J mice, we asked if the anti-AMPA-GluR3B antibodies could induce various behavioral and/or motor abnormalities (Ganor et al. 2014). To answer this question, the behavior of the mice was studied in three widely used behavioral tests: the open-field, rotarod and grip tests.
To understand the results, an introduction to each of these behavioral tests is required.
Activity in the open-field test: The open-field test is designed to measure behavioral responses, such as hyperactivity, exploratory, and locomotor activity. The open-field test is also used as a measure of anxiety, because mice tend to avoid brightly illuminated, novel and open spaces. Hence, the open-field environment acts as an anxiogenic stimulus, and allows for measurement of anxiety-induced locomotor activity and exploratory behaviors.
In our study (Ganor et al. 2014), all the DBA/J mice were tested for their activity in the open-field after the second PTZ administration. We observed that the anti-AMPA-GluR3B antibodies positive mice had a statistically significant different behavioral pattern, compared to the anti-AMPA-GluR3B antibodies negative mice, as they crossed fewer lines within the field (p < 0.0010), had a longer latency period (p < 0.0010), and had higher anxiety crossing scores (p < 0.0500). These findings showed that the anti-AMPA-GluR3B antibodies positive mice had some problems in their behavioral responses, and that they were more anxious (Ganor et al. 2014).
Performance in the RotaRod test: The RotaRod test assesses motor coordination and balance, fatigue resistance and motor skill learning. In our study (Ganor et al. 2014), the RotaRod test was performed following the three PTZ injections. In all three tests performed, the anti-AMPA-GluR3B antibodies positive mice exhibited statistically significant lower performance than the anti-AMPA-GluR3B antibody-negative mice, as they managed to remain on the accelerating rod for shorter time periods (fall latency, p < 0.0500). These findings showed that anti-AMPA-GluR3B antibodies positive mice had problems in balance, motor coordination and motor skill learning (Ganor et al. 2014).
Performance in the Grip test: The Grip test is used to measure the maximal muscle strength of forelimbs and combined forelimbs and hind limbs. In our study (Ganor et al. 2014), the Grip test was carried out following the three PTZ injections. Statistically significant differences were found between the anti-AMPA-GluR3B antibodies positive and negative mice in the percentage of mice that fell from the rod, thus failing to travel the whole 30-cm distance of the rod. Hence, all (100 %) of the anti-AMPA-GluR3B antibodies positive mice fell from the rod during the test, compared to only 3 of 14 (21.4 %) of the anti-AMPA-GluR3B antibodies negative mice (p = 0.01). These findings suggested that anti-AMPA-GluR3B antibodies positive mice had problems in muscle strength and balance.
Taken together, the findings of this study revealed that the mice that had anti-AMPA-GluR3B antibodies in their serum had significantly more behavioral and motor impairments of several types than mice devoid of such antibodies (Ganor et al. 2014). These findings suggest that anti-AMPA-GluR3B antibodies could induce by themselves, or at least contribute indirectly to the cognitive, psychiatric and/or behavioral problems of Epilepsy patients. If this is indeed the case, one can understand why anti-AMPA-GluR3B antibodies associate with psychiatric/cognitive/behavioral impairments in Epilepsy patients, as we observed recently (Goldberg-Stern et al. 2014) and discussed above in part 3.5.
Anti-AMPA-GluR3B antibodies in rats
Anti-AMPA-GluR3B antibodies produced in rats induce brain damage.
We immunized Lewis rats with the GluR3B peptide, or the GluR3A peptide, or the control scrambled GluR3B peptide, all emulsified in CFA (Ganor et al. 2005d). As a result of these immunizations, each group of rats developed high titers of specific antibodies directed only against the peptide it was immunized with: either anti-AMPA-GluR3B antibodies, or anti-AMPA-GluR3A antibodies, or anti-scrambled GluR3B antibodies. All these antibodies were detected in the serum of the respective rats. The anti-AMPA-GluR3B antibodies were detected also in the CSF of the GluR3B-immunized rats (the evidence for this can be seen in Fig. 4b in (Ganor et al. 2005d).
We then investigated whether the anti-AMPA-GluR3B antibodies induced pathological changes in the brain. For this purpose, we performed immunohistochemical staining of brain sections of all the immunized rats using three different markers: (1) NeuN—a DNA-binding neuron-specific protein that is present in most neuronal cell types, and accepted as an immunocytochemical marker for mature neurons, (2) DCX—a microtubule-associated phosphoprotein that is utilized as a marker of newly born neurons, (3) GFAP—an astrocyte-specific intermediate filament that increases in these cells in response to essentially any CNS pathology. We focused primarily on the cortex, as previous studies have demonstrated that anti-AMPA-GluR3 antibodies can kill cortical neurons (Whitney and McNamara 2000). Evaluating first the total number of surviving mature neurons in the cortex, we found that the number of NeuN-positive mature neurons was significantly lower in the rats that had anti-AMPA-GluR3B antibodies, compared to the control rats that did not have them. This brain pathology were evident in the superficial layer VI of the cortex, in both the motor cortex and the somatosensory cortex. In specific, in comparison to the control rats, ~25 % and ~15 % less mature neurons were present in layer VI of the motor and somatosensory cortex areas of the GluR3B-immunized rats, respectively, and these changes were statistically significant (Ganor et al. 2005c).
We next evaluated the extent of neurogenesis by qualitative analysis of the number of DCT-positive immature neurons in the subventricular zone of the brain. The number of such newly born neurons was previously reported to increase following brain injury (e.g. focal cerebral ischemia), probably as a compensation for the loss of mature neurons. Indeed, we found that the increased loss of mature neurons in the brains of the rats that had anti-AMPA-GluR3B antibodies (detected by the decreased number of NeuN-positive mature neurons) was accompanied by the appearance of more DCT-positive immature neurons in the subventricular zone (Ganor et al. 2005c).
Finally, we analyzed the amount of reactive astrocytes in the superficial layers of the cortex, and found that the rats that had anti-AMPA-GluR3B antibodies had almost twice more GFAP-positive astrocytes in both the motor cortex and the somatosensory cortex. Importantly, the GFAP-positive astrocytes had the characteristic reactive appearance, i.e. hypertrophy of their cellular processes filled with increased amounts of GFAP, which is indicative of reactive gliosis. In addition, the rats that had anti-AMPA-GluR3B antibodies had almost twice more GFAP-positive reactive astrocytes in the basal ganglia, compared to the rats that did not have these antibodies.
Taken together, these results showed that one can study specific anti-AMPA-GluR3B antibodies in Lewis rats, and that in this animal model the anti-AMPA-GluR3B antibodies killed mature neurons, caused reactive gliosis in the brain, and also stimulated the production immature neurons, the latter probably occurring as an attempt of the brain to compensate for the loss of the mature neurons (Ganor et al. 2005c).
Anti-AMPA-GluR3B antibodies in rats confer partial protection from PTZ-induced seizures.
The Lewis rats described in the preceding part, and in (Ganor et al. 2005d), that had anti-AMPA-GluR3B antibodies both in the serum and in the CSF, and that expressed the brain pathologies described in part 3.7.2.2, did not develop frequent and overt spontaneous seizures, at least not in day time, and at least as reported by the animal technician that looked at the rats once a day for few minutes only.
We then studied the response of the GluR3B-immunized rats, the GluR3A-immunized rats and the scrambled GluR3B-immunized rats to the chemoconvulsant PTZ [as we did with the GluR3B-immunized DBA/J mice (Ganor et al. 2004)].
Surprisingly, and in contrast to what we observed in the DBA/J mice (Ganor et al. 2014), in response to PTZ the GluR3B-immunized rats displayed fewer jerks, a lower percentage of generalized seizures, and a lower overall seizure severity score than the three groups of control rats: the GluR3A-immunized, scrambled GluR3B-immunized, and the non-immunized rats. These findings, combined with the previously demonstrated ability of anti-AMPA-GluR3B antibodies to bind, activate and kill neurons and glia, and with their ability to worsen PTZ-induced seizures in DBA/J mice (Ganor et al. 2014), suggest that the neuronal death caused by these antibodies can on the one hand be by itself pro-epileptic and induce or worsen seizures (as observed in DBA/J mice), but on the other hand can also decrease the excitability of seizure-related neural circuits, thereby conferring partial protection from seizures induced by other exogenously-applied epileptogenic stimuli like PTZ [as observed in Lewis rats (Ganor et al. 2005c)]. In addition, it could be that the exact nature and magnitude of the effects in the brain induced by the anti-GluR3B antibodies differ between mice and rats bearing these antibodies, since these two species also differed in the extent of brain pathology induced by these antibodies. Finally, the pathological processes occurring in the brains of Epilepsy patients that have such anti-GluR3B antibodies may resemble the pathologies seen either in mice (Levite and Hermelin 1999; Ganor et al. 2014) or in rats (Ganor et al. 2005c), or in rabbits (Rogers et al. 1994) that have such antibodies, or rather different than the brain pathologies seen in all of them.
Are the autoimmune AMPA-GluR3B antibodies produced due to a specific viral or bacterial infection?
Molecular mimicry between the LP-BM5 murine-leukemia virus and the AMPA receptor leads to the production in mice of cross-reacting antibodies that activate AMPA receptors and kill neurons
In general, in all autoimmune diseases characterized by ‘forbidden’ anti-self immune responses, one suspects and investigates a bacterial or viral etiology, based on the assumption that an originally ‘legitimate’ and beneficial immune response evoked against an external virus or bacteria that threatens the healthy body, can go wrong at some point, due to several genetic, epigenetic or environmental reasons and mechanisms and end up in detrimental autoimmune responses against self ‘innocent’ molecules. And then, the autoimmune responses can cause various types of structural and functional damage to the healthy cells and tissues, and eventually lead to a life-time autoimmune disease. Several mechanisms have been proven or suggested as the means by which a bacterial or viral infection can initiate an autoimmune response that can eventually lead an autoimmune disease. The most straight forward one is ‘Molecular mimicry’ (Cusick et al. 2012). Molecular mimicry refers to a situation in which a specific peptide/antigen of a foreign infectious organism, usually or virus or bacteria, shares similarity with a self peptide/antigen. As such, the ‘legitimate’ immune response which is directed originally against the foreign bacterial or viral antigen, and which is mediated by specific antibodies and/or T cells that react against it, can shift to a detrimental cross-reactive autoimmune response directed against the self peptide/antigen.
A support for molecular mimicry between viral peptides and self GluR3 as a cause of anti-AMPA-GluR3 antibodies production and CNS damage comes from the tantalizing studies of Koustova et al. (2001) and Basile et al. (2001). Their studies showed that mice that were immunized with the LP-BM5 murine-leukemia virus, which manifest by excitotoxic brain lesions and hypergammaglobulinemia, produced antibodies that strongly reacted not only with the LP-BM5 viral peptides, but also with self AMPA receptors, among them GluR3. These studies also showed elegantly that the production of such cross-reactive anti-LP-BM5/AMPA receptors antibodies was due to partial molecular mimicry between the LP-BM5 murine-leukemia virus and the self AMPA receptor. Strikingly, the cross-reactive and self-reactive anti-LP-BM5/AMPA receptor antibodies activated AMPA receptors, evoked inward currents and caused significant neuronal death (Basile et al. 2001; Koustova et al. 2001). Furthermore, the cross-reactive anti-LP-BM5/AMPA receptor antibodies derived from the brains of the LP-BM5-infected mice were suppressed in vitro by immobilized LP-BM5 virus proteins, indicating that some viral proteins and the self AMPA receptors indeed have common epitopes.
High frequency of epileptic RE patients had preceding infections, and from a genetic point of view, have certain immunogenetic alleles and haplotypes of HLA class I molecules that may be risk factors for developing autoimmunity
It is currently unknown why anti-AMPA-GluR3B antibodies are being produced in some individuals and in some not. Our own working hypothesis is that the production of these autoimmune anti-glutamate receptor antibodies occurs in some individuals that have a certain immunogenetic background, and that it is initiated by either of the following: (1) an ongoing/chronic activation of the immune system in general, and of T cells in particular, due to an unresolved viral or bacterial infection. And then, the chronic immune activation leads to chronic inflammation and neuroinflammation, and all that increases the risk to develop autoimmunity. We further postulate that this scenario may take place only in some individuals that have a certain immunogenetic background that makes them incapable of eradicating efficiently certain microorganisms; (2) An abnormal/excessive immune response to certain vaccinations that contain certain attenuated or dead bacteria or viruses; 3) Severe food poisoning, due to eating food contaminated by certain infectious organisms; 4) A severe non-specific breakdown of immune tolerance to self antigens, due to a major injury, trauma or stress. A proposed scheme of events that may lead from all these initial events to the production of autoimmune anti-AMPA-GluR3B antibodies is shown in Levite and Ganor (2008).
An infectious etiology on the basis of a specific immunogenetic background is supported by the paper of Takahashi et al. (2006), showing that almost half of the Japanese RE patients they studied had some preceding causative factors. Infections were found in 38.2 % of these patients, vaccinations in 5.9 %, and head trauma in 8.9 %. Interestingly, in a patient with seizure onset after influenza A infection, cross-reaction of the patient’s lymphocytes with GluR epsilon 2, i.e., NMDA NR2B, and influenza vaccine components, was demonstrated by a lymphocyte stimulation test.
Subsequent database analysis revealed that the foreign influenza A virus hemagglutinin and the self GluR epsilon 2 molecules contain peptides that have the patient’s HLA class I binding motif (HLA-A*0201). According to Takahashi et al., the relative risks of HLA class I genotypes for RE are: 6.1 (A*2402), 6.4 (A*0201), 6.3 (A*2601) and 11.4 (B*4601). The relative risks of HLA class I-A and B haplotypes are infinity (A*2601 + B*5401), 21.1 (A*2402 + B*1501), 13.3 (A*2402 + B*4801) and 5.1 (A*2402 + B*5201) (Takahashi et al. 2006).
The conclusions and suggestions of Takahashi et al. were that some alleles and haplotypes of HLA class I may be the risk factors in Japanese RE patients, and that cross-reactivity of cytotoxic T lymphocytes may contribute to the processes leading from infection to the involvement of CNS.
Some Epilepsy patients that have autoimmune anti-AMPA-GluR3 antibodies respond well to immunotherapy
Over the years, encouraging results have been obtained in a relatively small number of Epilepsy patients bearing anti-AMPA-GluR3 antibodies, with regard to their responses to immunotherapy of several modalities (Andrews et al. 1996; Antozzi et al. 1998; Granata et al. 2003; Leach et al. 1999; Rogers et al. 1994).
In these cases, treatment of Epilepsy patients that had anti-AMPA-GluR3 antibodies with repeated plasmapheresis (Andrews et al. 1996, 1997; Rogers et al. 1994), Intravenous Immunoglobulins (IVIG) (Granata et al. 2003; Leach et al. 1999), or long-term selective IgG immunoadsorption (Antozzi et al. 1998), caused a transient reduction in seizure frequency and also a significant improvement in neurological function, in correlation with reduced serum titers of the anti-AMPA-GluR3 antibodies. For readers interested in the general topic of immunotherapy for autoimmune and/or inflammatory epilepsies, the following reviews may be useful (Bien et al. 2012; Granata et al. 2003; Levite and Hart 2002; Nabbout 2012; Villani and Avanzini 2002).
Few examples of successful immunotherapy given to Epilepsy patients having anti-AMPA-GluR3 antibodies are cited in the coming paragraphs.
Plasmapheresis—(1) Rogers et al. (1994) found that repeated plasma exchanges in one seriously ill epileptic child transiently reduced the serum titers of anti-AMPA-GluR3 antibodies, decreased the seizure frequency and improved the neurologic function, (2) Andrews et al. (1996, 1997) studied four patients with pathologically confirmed RE who were treated with repeated plasmapheresis. Three patients exhibited repeated and dramatic yet transient responses to the plasmapheresis, manifested by reduced seizure frequency and improved neurologic function. One patient exhibited marginal improvement, (3) Andrews et al. (1997) studied two more patients with pathologically confirmed RE and increased levels of circulating anti-AMPA-GluR3 antibodies prospectively before, during, and after trials of plasmapheresis and other modes of immunomodulation. The frequency, duration and intensity of the clinical seizures were directly correlated with the abundance of the interictal epileptiform activity on serial EEGs. The clinical and EEG parameters of the epileptogenesis were transiently diminished by plasmapheresis, which suggested that ‘circulating factors’ induced dose dependent, reversible epileptogenic effects in some RE patients.
IgG immunoadsorption—Antozzi et al. (1998) reported that long-term selective immunoglobulin G immunoadsorption by protein A (PAI) improved seizure frequency and neuropsychological deficits in a 16-year-old patient with severe treatment-resistant RE. Clinical improvement correlated with reduction of anti-AMPA-GluR3 antibodies.
IVIG—Leach et al. (1999) studied the immediate and chronic effects of high-dose and long-term human IVIG therapy in two patients with advanced adult-onset RE. The treatment started with monthly cycles of high-dose IVIG (0.4 g/kg/day for 5 days), followed by maintenance therapy (0.4 g/kg 1 day each month) after the patient’s conditions began to improve. Outcome measures included clinical, psychological, functional, and laboratory assessments before the treatment, and at relevant intervals throughout a year of treatment. In both patients, unrelenting pretreatment deterioration halted, and thereafter the patients displayed striking improvements in seizure control, hemiparesis and cognition, that produced useful recovery of function. Improvements were delayed until after 2–4 monthly cycles of high-dose IVIG, and continued when the patients switched to maintenance treatment. Their recoveries were accompanied by increased cerebral perfusion on interictal SPECT, and by suppression of inflammatory markers in the CSF. Leach et al. (1999) concluded that IVIG can be a useful, possibly disease-modifying, long-term therapy for adult-onset RE, and that as such it should be considered before any radical surgery is performed. Because improvements can be delayed, proposed guidelines for intensive and prolonged trials of immunomodulatory therapy in adults with this syndrome were outlined.
In another paper, Villani et al. (2001) report on a positive response to high-dose therapy with IVIG in an adult epileptic RE patient. Later, Villani wrote a broader review on the use of IVIG for the treatment of Epilepsy (Villani and Avanzini 2002).
Combined immunomodulatory treatment that included IVIG and other types of immunotherapy—Granata et al. (2003) investigated the responses to high-dose IVIG treatments of 15 RE patients with RE: 14 with childhood and one with adolescent onset RE. Positive time-limited responses were obtained in 11 RE patients using variable combinations of high-dose IVIG, corticosteroids and apheresis.
In contrast to these successful experiences, Feichtinger et al. (2006) report on a lack of effect of immunomodulatory therapy given to a 18-year-old patient that had treatment-refractory left mesial temporal lobe Epilepsy accompanied by high levels of anti-AMPA-GluR3 antibodies. Thus, in this single case, in difference from the few other good experiences in RE patients that responded well to immunotherapy, the immunomodulatory therapy based on IVIG neither altered the levels of anti-AMPA-GluR3 antibodies in the serum, nor had any effect on the seizure frequency. Interestingly, the levels of anti-AMPA-GluR3 antibodies in the serum of this patient remained high even after successful surgical intervention that led to patient’s seizure freedom (Feichtinger et al. 2006).
Anti-GluR3B T cells are also being produced in mice after immunization with the GluR3B peptide
A previous report has shown local clonal expansion of infiltrating T cells in brain lesions of RE patients (Li et al. 1997), suggesting that a specific cellular T cell-mediated immune response has occurred in RE, as often seen in inflammatory tissue lesions.
In general, a hallmark of a specific T cell response is a proliferating T cells that have a restricted repertoire of the T cell receptor (TCR) β-chain variable region (Vβ).
In view of the above, we asked whether mice that are immunized with the GluR3B peptide produce not only highly specific anti-AMPA-GluR3B antibodies (as described in (Levite and Hermelin 1999) and in the first few paragraphs of part 3.7.2.1), but also anti-AMPA-GluR3B T cells. We also asked whether the arising T cells show a restricted, or significantly biased, TCR expression pattern, suggestive of a highly specific T cell-mediated immune response (Levite and Hermelin 1999). To answer these questions, we analyzed the TCR-Vβ expression of the total T cell population rescued from individual GluR3B-immunized mice. Due to the technical difficulty in obtaining T cells from detectable mouse brain lesions in situ, T cells were taken from the spleens of the GluR3B-immunized mice. This compromise was made bearing in mind that in general, the TCR repertoire of splenocytes has a much lower probability of being highly restricted than that of T cells at the site of a lesion. Another limitation was that the spleen cells from the GluR3B-immunized mice clearly included T cells directed against antigens other than the GluR3B peptide. Bearing these limitations in mind, we measured the binding of T cells of the GluR3B-immunized mice to FITC-conjugated monoclonal antibodies directed against 14 different (out of the existing 22) Vαβ regions: Vβ 2, 4, 5.1/5.2, 6, 8.1/8.2, 9, 10, 11, 12, 13, 15 and 17. For normalization, the T cells from the individual mice were assessed in parallel also for their total level of expression of TCR-Vβ gene products, using FITC-conjugated monoclonal antibodies directed against the α- and β-chains of the TCR. For readout of the binding, we used a Fluorescence-Activated Cell Sorter (FACS).
These tests revealed two main findings: (1) all the different TCR-Vβ gene products expressed in the spleen of normal C3H/HeJ mice were also expressed by the GluR3B immunized mice, thus providing no evidence for a deficient or limited TCR-Vβ usage, (2) there were significantly biased frequencies of particular TCR-Vβ families in the spleens of the GluR3B-immunized mice, in comparison to normal mice. The most significant biases found in the GluR3B-immunized mice were increased frequencies of Vβ11, Vβ7 and Vβ8, which were expressed, respectively, 2.9, 2.2 and 1.7 times more than in control mice. This skewed pattern of expression of particular TCR-Vβ families suggested that there was a clonal proliferation of specific T cell populations in spleens of the GluR3B-immunized mice, in response to the GluR3B peptide. If so, the self GluR3B peptide is a self peptide/antigen that induces both a humoral antibody-mediated immune response, and a cellular T cell-mediated immune response, both directed specifically against it (Levite and Hermelin 1999). It could very well be that the anti-AMPA GluR3B-specific T cells also induce brain damage (alike the anti-AMPA-GluR3B antibodies do) by being cytotoxic to AMPA-GluR3-expressing neurons, and by secreting various pro-inflammatory cytokines in the brain. A postulated scheme of events showing how both antibodies and T cells directed against the GluR3B peptide can be produced, and then reach the brain and damage it, is shown in our review on autoimmunity against glutamate receptors published in 2008 (Levite 2008).
Anti-NMDA-NR1 antibodies, directed against the NR1 subunit of glutamate/NMDA receptors, are found in patients with autoimmune ‘Anti-NMDA receptor Encephalitis’, decrease the expression of synaptic NMDA receptors by crosslinking and internalization, associate with neuropsychiatric abnormalities, and can be removed or silenced in patients by immunotherapy
The human diseases in which anti-NMDA-NR1 antibodies were found thus far are shown schematically in Fig. 1, while their main features and effects in humans and animal models are summarized in Fig. 3, and will be discussed in the below parts 5.1, 5.2, 5.3 and 5.4.
Summary of ‘Anti-NMDA receptor Encephalitis’
The disease called now ‘Anti-NMDA receptor Encephalitis’ or in short ‘NMDA Encephalitis’ is associated with, and mediated by, anti-NMDA-NR1 antibodies. It is a severe, treatable and potentially reversible neurological disorder presenting with memory deficits, psychiatric symptoms, autonomic instability including hypoventilation and seizures. In this disease, the memory problems and neurobehavioral changes can even start before seizures onset (Dalmau et al. 2008, 2011; Finke et al. 2012; Florance et al. 2009; Frechette et al. 2011; Hughes et al. 2010; Iizuka et al. 2008; Irani et al. 2010; Irani and Vincent 2011; Manto et al. 2010; 2011; Sansing et al. 2007).
A very good, comprehensive and updated review on ‘Anti-NMDA receptor Encephalitis’, and on the anti-NMDA-R1 antibodies that cause this disease, was written by Dalmau et al. (2011) and published in 2011 in ‘The Lancet’. For the benefit of the readers, and as a special tribute to Dalmau et al. (2007, 2008, 2011) for their pioneering and key discoveries over the years in regards to ‘Anti-NMDA receptor Encephalitis’ (Iizuka et al. 2008), I copy herein the summary of this review, almost as is (Dalmau et al. 2011).
“Since 2007, the Encephalitis associated with antibodies against the N-methyl-d-aspartate receptor (NMDAR) has entered the mainstream of neurology and other disciplines. Most patients with ‘Anti-NMDA receptor Encephalitis’ develop a multistage illness that progresses from psychosis, memory deficits, seizures, and language disintegration into a state of unresponsiveness with catatonic features often associated with abnormal movements, and autonomic and breathing instability. The disorder predominantly affects children and young adults, occurs with or without tumor association, and responds to treatment, but can relapse. The presence of a tumor (usually an ovarian teratoma) is dependent on age, sex and ethnicity, being more frequent in women older than 18 years, and slightly more predominant in black women than in white women. Patients treated with tumor resection and first-line immunotherapy: Corticosteroids, IVIG, or plasma exchange, respond faster to treatment and less frequently need second-line immunotherapy: Cyclophosphamide or Rituximab, or both, than do patients without a tumor who receive similar initial immunotherapy. More than 75 % of all patients have substantial recovery that occurs in inverse order of symptom development and is associated with a decline of antibody titers. Patient’s anti-NMDA-NR1 antibodies cause a titer-dependent, reversible decrease of synaptic NMDA receptor by a mechanism of crosslinking and internalization. On the basis of models of pharmacological or genetic disruption of NMDA receptor, these antibody effects reveal a probable pathogenic relation between the depletion of receptors and the clinical features of ‘Anti-NMDA receptor Encephalitis’” (Dalmau et al. 2011).
The exact incidence of ‘Anti-NMDA receptor Encephalitis’ is unknown, but on the basis of the rapid accrual of patients and increasing number of case reports, it seems to be more frequent than any other known Paraneoplastic Encephalitis. The experience of Dalmau et al. (2011) with ~400 patients with ‘Anti-NMDA receptor Encephalitis’ in just 3 years indeed suggests a relatively frequent disorder. And as Dalmau states: “Many of the patients with ‘Anti-NMDA receptor Encephalitis’ are children and young adults with or without an associated tumor”.
Irani et al. report on the finding of anti-NMDA receptor antibodies of the IgG1 subclass in the serum and CSF of 44 patients. Importantly, these antibodies were able to activate complement on human embryonic kidney cells that expressed the NMDA receptor. A high proportion of these 44 patients were without a detected tumor (35/44, 80 %: follow-up of 3.6–121 months, median of 16 months). Among the latter were 15 (43 %) adult females, 10 (29 %) adult males and 10 (29 %) children, with four in the first decade of life. Overall, there was a high proportion (29 %) of non-Caucasians. Good clinical outcomes, as defined by reductions in modified Rankin scores, correlated with decreased anti-NMDA receptor antibody levels, and were associated with early (<40 days) administration of immunotherapies in non-paraneoplastic patients, and earlier tumor removal in paraneoplastic patients. Ten patients (23 %) who were first diagnosed during relapses had no evidence of tumors, but received minimal or no immunotherapy during earlier episodes. Temporal analysis of the onset of the neurological features suggested progression through two main stages. The time of onset of the early features, characterized by neuropsychiatric symptoms and seizures, preceded by a median of 10–20 days the onset of movement disorders, reduction in consciousness and dysautonomia. This temporal dichotomy was also seen in the timing of CSF, electroencephalographic and in the rather infrequent cerebral imaging changes. Irani et al. (2010) concluded that their data support a model in which the early features are associated with CSF lymphocytosis, and the later features are associated with appearance of oligoclonal bands. They also suggested a putative scenario for the immunological events and neuronal mechanisms underlying these observations according to which the early stage represents diffusion of serum antibodies into the cortical gray matter, whereas the later stage results from secondary expansion of the immunological repertoire within the intrathecal compartment acting on subcortical neurons.
Anti-NMDA-NR1 antibodies are present in the CSF of patients with ‘Anti-NMDA receptor Encephalitis’, and in most cases are being produced intrathecally
Dalmau et al. (2008, 2011) found that the CSF of patients with ‘Anti-NMDA receptor Encephalitis’ is initially abnormal in 80 % of patients, and becomes abnormal later in the disease in most other patients. The abnormal findings in the patient’s CSF include moderate lymphocytic pleocytosis, normal or mildly increased protein concentration, and, in 60 % of patients, CSF-specific oligoclonal bands. A very interesting and important fact is that most patients have intrathecal synthesis of anti-NMDA-NR1 antibodies (Dalmau et al. 2008, 2011; Pruss et al. 2010). Remarkably, Dalmau et al. report that of the 431 patients they studied (412 with paired serum and CSF), they have NOT encountered a single patient in whom the anti-NMDA-NR1 antibodies were only present in serum!
The study of Irani et al. (2010) provides further evidence for a profound intrathecal synthesis of anti-NMDA receptor antibodies in patients. Yet, in their patients, despite this intrathecal synthesis, the absolute levels of the anti-NMDA receptor antibodies were higher in serum than in CSF (Irani et al. 2010).
Together, these evidences show that the autoimmune process against NMDA-NR1 is active, ongoing and ‘stormy’ inside the CNS of patients with ‘Anti-NMDA receptor Encephalitis’.
The detrimental effects of anti-NMDA-NR1 antibodies and of anti-NMDA-NR1/NR2 heterodimer antibodies on: NMDA receptor expression in neurons, glutamate levels, the response to glutamate, and on other neuronal features and processes in vitro and in animal models
Study 1: CSF and purified IgG of patients with ‘Anti-NMDA receptor Encephalitis’ injected into rat’s brain increased the concentrations of glutamate in the extracellular space, and impaired both the NMDA- and the AMPA-mediated synaptic regulation of glutamate. Manto et al. (2010) studied the in vivo acute metabolic effects of CSF and purified IgG of patients with ‘Anti-NMDA receptor Encephalitis’. Injections were performed into the CA1 area of Ammon’s horn and into the premotor cortex of rats. Patient’s CSF increased the concentrations of glutamate in the extracellular space. The increase was dose-dependent and dramatic with purified IgG. Patient’s CSF impaired both the NMDA- and the AMPA-mediated synaptic regulation of glutamate, while not affecting the glial transport of glutamate.
Together, the results of this study provided evidence that in vivo, in rats, anti-NMDA receptor antibodies deregulate glutamatergic pathways, and that the Encephalitis associated with these antibodies is an autoimmune synaptic disorder.
Study 2: Anti-NMDA-NR 1 antibodies decrease the level of NMDA receptors expressed on the cell surface. Hughes et al. (2010) found that patient’s anti-NMDA-NR1 antibodies decreased NMDA surface receptors and synaptic localization, and that these effects correlated with patient’s antibody titers. Such a reduction of NMDA receptors induced by the anti-NMDA-NR1 antibodies may decrease the ability of neurons to respond to glutamate and, by doing so, harm multiple essential neuronal functions that depend on, and are mediated by, glutamate signaling.
Study 3: Patient’s serum containing anti-NMDA receptor IgA antibodies decrease dramatically the levels of NMDA receptors and other synaptic proteins in neurons, along with prominent changes in NMDA receptor-mediated currents. Prüss et al. (2012b) studied 24 patients with progressive cognitive dysfunction of unclear etiology, and examined them for onconeuronal and synaptic receptor antibodies. The effect of the patient’s serum on cultures of dissociated mouse hippocampal neurons growing in tissue culture was also investigated. The findings showed that seven patients had anti-NMDA receptor IgA antibodies, but no IgG antibodies. Patient’s serum that contained anti-NMDA receptor IgA antibodies, but not serum from control individuals, decreased dramatically the levels of NMDA receptors expressed in neurons, along with prominent changes in NMDA receptor-mediated currents. The patient’s serum also decreased the levels of additional synaptic proteins (Pruss et al. 2012b). These effects correlated with the titer of anti-NMDA receptor IgA antibodies, and were reversed after removing the patient’s serum from the culture media. When available, a comprehensive clinical assessment and brain metabolic imaging showed neurologic improvement after immunotherapy. Pruss et al. (2012b) concluded that a subset of patients with slowly progressive cognitive impairment has an underlying synaptic autoimmunity that decreases the density of NMDA receptors and of other synaptic proteins, and alters synaptic currents. This autoimmunity can be demonstrated by examining patient’s serum and CSF for the presence of anti-NMDA receptor IgA antibodies, identifying possible candidates for immunotherapy.
Study 4: Some patients with Herpes Simplex Virus Encephalitis (HSE) contain anti-NMDA-NR 1 /NR 2 antibodies, and the serum of these patients causes substantial decrease of NMDA receptors and of the synaptic marker synapsin in hippocampal neurons growing in tissue culture. Pruss et al. (2012a) analyzed retrospectively 44 patients with Herpes Simplex virus Encephalitis (HSE) for the presence of a large panel of antibodies directed against onconeuronal and synaptic receptors. The effect of the patient’s serum was also studied in cultures of primary mouse hippocampal neurons. Anti-NMDA receptor antibodies of the immunoglobulin (Ig) subtypes IgA, IgG, or IgM were detected in 13 of 44 (30 %) patients in the course of HSE, suggesting secondary autoimmune mechanisms. The anti-NMDA receptor antibodies were directed against the NMDA-NR1/NR2 heterodimers, and did not react with NMDA-NR1 alone. Such antibodies were often detected at hospital admission, but in some patients they developed after the first week of HSE. When the primary hippocampal neurons growing in cell cultures were incubated for 3 days with the sera of patients that contained the anti-NMDA-NR1/NR2 antibodies, the result was a substantial decrease of NMDA receptors. The effect was not induced by the sera of healthy individuals. Interestingly, the patient’s sera containing the anti-NMDA-NR1/NR2 antibodies induced also a marked reduction in the expression of the synaptic marker Synapsin in the hippocampal neurons. The Synapsins are a family of proteins that have been implicated in the regulation of neurotransmitter release at synapses, and have an important modulatory role in synaptic function. Based on all the above, Pruss et al. (2012a) concluded that some patients with HSE develop IgA, IgG, or IgM autoimmune antibodies directed against NMDA receptors, and suggest that these antibodies (and/or perhaps other autoimmune antibodies present in the serum of these patients) may alter the density of neuronal synaptic markers, and as such may have a potentially pathogenic disease-modifying effect. These findings have implications for the understanding of autoimmunity in infectious diseases, and call for further studies to reveal whether the subgroup of patients with HSE and anti-NMDA receptor antibodies may benefit from immunotherapy, alike patients with ‘Anti-NMDA receptor Encephalitis’.
Study 5: Upon injection of CSF of patients with Encephalitis, that contained anti-NMDA-NR 1 /NR 2 heterodimer antibodies, or of IgG purified from the patient’s sera, into rat’s brain, there was an increase in the afferent facilitation of corticomotor responses. Manto et al. (2011) injected the CSF of patients with Encephalitis, that contained anti-NMDA-NR1/NR2 heterodimer antibodies, into rFr2 (the prefrontal area) of rat’s brain, and studied its effect on the afferent facilitation in a conditioning paradigm for corticomotor responses. The afferent facilitation was assessed in the forelimbs and hind limbs of the rats, before and after application of trains of high-frequency stimulation (HFS), which are known to modulate the excitability of M1. Before HFS, the patient’s CSF did not modify afferent facilitation. After HFS, the amplitudes of corticomotor responses before conditioning were significantly larger in the forelimbs and hind limbs. There was an increase in the afferent facilitation in the forelimbs. The same effect was observed after injection of purified IgGs from patient’s sera. Taken together, these findings showed that IgGs of patients with anti-NMDA receptor antibodies induce a state of corticomotor hyperexcitability following application of HFS over the prefrontal area (Manto et al. 2011).
Study 6: Anti-NMDA receptor antibodies activate complement on NMDA receptor-expressing human embryonic kidney cells. Irani et al. (2010) established a sensitive cell-based assay for detection of anti-NMDA receptor antibodies in the serum or CSF, and a quantitative fluorescent immunoprecipitation assay for serial studies. They tested patients with encephalopathy, and found that although there was a marked intrathecal synthesis of the anti-NMDA receptor antibodies, the absolute levels of these antibodies were higher in the serum than in the CSF. The anti-NMDA receptor antibodies were of the immunoglobulin IgG1 subclass, and they were able to activate complement on NMDA receptor-expressing human embryonic kidney cells (Irani et al. 2010).
Anti-NMDA-NR1 antibodies may contribute to the cognitive deficits of patients following ‘Anti-NMDA receptor Encephalitis’
Finke et al. (2012) investigated the cognitive performance of nine patients with proven ‘Anti-NMDA receptor Encephalitis’ after recovery from the acute disease period (median 43 months after disease onset, range 23–69). Patients underwent a comprehensive neuropsychological assessment, including memory tasks that have previously been shown to be sensitive for hippocampal dysfunction. Substantial persistent cognitive impairments were observed in eight out of the nine patients that mainly consisted of deficits in executive functions and memory. The severity of these deficits varied inter-individually. Patients with early immunotherapy performed significantly better. The most severe deficits were observed with inefficient or delayed initial treatment. These findings, although not showing directly that anti-NMDA-NR1 antibodies cause cognitive deficits (this can be shown only in animal models), suggest that cognitive deficits constitute a major long-term morbidity of ‘Anti-NMDA receptor Encephalitis’—a disease mediated by these antibodies. These cognitive deficits relate to the distribution of NMDA receptors in the human brain, and to their functional role in normal cognition. Finke et al. (2012) also suggested that good cognitive long-term outcome may depend on early and aggressive treatment.
Are the anti-NMDR-NR1 antibodies being produced due to a specific viral or bacterial infection?
In their review on few hundred patients with ‘Anti-NMDA receptor Encephalitis’, Dalmau et al. (2011) state that because the presentation of this disease often suggests an infectious process, many patients undergo extensive blood and CSF assessments. Dalmau et al. report on their own patients with ‘Anti-NMDA receptor Encephalitis’, of which a few had positive serological tests suggesting an infection.
Examples for a possible infectious etiology were revealed in the studies summarized in the coming paragraphs.
Gable et al. (2009) studied 10 young patients (median age of 18.5 years) with anti-NMDA receptor antibodies, and a characteristic progression with prominent psychiatric symptoms, autonomic instability, significant neurologic abnormalities, and seizures. Four patients (40 %) were found to have serologic evidence of acute mycoplasma pneumonia infection.
Baltagi et al. (2010) studied four children with neurological complications attributed to 2009 influenza A (H1N1). The four children were admitted to the pediatric intensive care unit with altered mental status and influenza infection. All the children demonstrated a coryzal prodrome, fever, and altered level of consciousness at admission, and one child presented with clinical seizures. All the children had abnormal electroencephalograms early in their intensive care unit course, and 50 % of them had abnormal imaging studies. All the children survived, but 50 % of them had neurologic deficits at hospital discharge. One child had anti-NMDA receptor antibodies. The clinical picture of this patient, but not of the other three, was typical of ‘Anti-NMDA receptor Encephalitis’. None of the above-mentioned patients had CSF findings indicating direct viral involvement of the CNS. Baltagi et al. concluded that H1N1 can cause significant acute and residual neurologic sequelae.
Hofmann et al. (2010) reported on two patients that developed ‘Anti-NMDA receptor Encephalitis’ after vaccination against H1N1 influenza, and one patient after a booster vaccination against tetanus, diphtheria, pertussis, and poliomyelitis.
Verhelst et al. (2010) reported on a 3-year-old boy who developed ‘Anti-NMDA receptor Encephalitis’ 1 month after a respiratory infection. Moreover, array-comparative genomic hybridization in this patient revealed an inherited micro deletion in chromosome band 6p21.32, including the HLA-DPB1 and HLA-DPB2 genes. Verhelst et al. (2010) discuss in their paper the clinical relevance of this micro deletion.
Despite these examples, since there does not seem to be a consistent infectious organism that is associated with ‘Anti-NMDA receptor Encephalitis’, Dalmau et al. (2011) do NOT think that molecular mimicry between a specific virus or bacteria and self NMDA-NR1 could be the trigger for the production of the autoimmune anti-NMDA-NR1 antibodies. Having said that, non-specific systemic infections or vaccinations can act as an adjuvant of the autoimmune response.
Many patients with ‘Anti-NMDA receptor Encephalitis’ respond very well to immunotherapy
Many patients with ‘Anti-NMDA receptor Encephalitis’, that have anti-NMDA-NR1 antibodies in their serum and CSF were treated with either first-line immunotherapy: Steroids, IVIG, or plasmapheresis/plasma exchange, or with second-line immunotherapy: Rituximab or Cyclophosphamide or both. In many cases, these immunotherapies led to a substantial recovery, and were associated with a decline in the titers of the anti-NMDA-NR1 antibodies (Dalmau et al. 2011; Finke et al. 2012; Irani and Vincent 2011). Good cognitive long-term outcome seems to depend on early and aggressive treatment.
Dalmau et al. report on a very impressive proportion: ~75 % of the patients with anti-NMDA-NR1 antibodies that recovered or had mild sequelae. All the other patients remained severely disabled or died. Dalmau et al. (2008) recommend that the management of ‘Anti-NMDA receptor Encephalitis’ should initially focus on immunotherapy, and on the detection and removal of a teratoma. Most patients receive Corticosteroids, IVIG or plasma exchange as first-line of immunotherapy, and these treatments have enhanced effectiveness and speed of action when the patients have an underlying tumor that is removed (Florance et al. 2009; Irani et al. 2010). In patients without a tumor, or with delayed diagnosis, additional treatment with second-line immunotherapy (Rituximab, Cyclophosphamide, or both) is usually needed. The experience of Dalmau et al. with 105 consecutively diagnosed patients in 2009 accords with these findings (see Fig. 3 in Dalmau et al. 2011). Although 80 % of patients with a tumor (mostly teratomas) had substantial improvement after tumor removal and first-line immunotherapy, only 48 % of those without a tumor had a similar degree of improvement after first-line immunotherapy and needed second-line immunotherapy more often.
Overall, second-line immunotherapy resulted in substantial improvement in 15 of 23 (65 %) patients. The final outcome and substantial improvement was much of the same in patients with or without tumor. Spontaneous neurological improvement has been reported, but usually occurred at the expense of longer hospital stay and slower recoveries (Dalmau et al. 2011).
Interestingly, Finke et al. (2012) found that immunotherapy seemed to improve also the cognitive impairments of patients with ‘Anti-NMDA receptor Encephalitis’ that had anti-NMDA-NR1 antibodies. Thus, eight out of nine (88.8 %) patients with ‘Anti-NMDA receptor Encephalitis’ that expressed substantial persistent cognitive impairments, that mainly consisted of deficits in executive functions and memory, and that received early immunotherapy, performed significantly better (Finke et al. 2012).
Anti-NMDA-NR2A/B antibodies, directed against subunit NR2A/B of the NMDA type of ionotropic glutamate receptor, are found in subpopulations of patients with Systemic Lupus Erythematosus, Epilepsy, Encephalitis, Schizophrenia, Mania, Stroke or Sjorgen syndrome. These anti-glutamate receptor antibodies can kill neurons, damage the brain, and in some cases induce or associate with neuropsychiatric or cognitive impairments
The human diseases in which anti-NMDA-NR2 antibodies were found thus far are shown schematically in Fig. 1, while their main features and effects in patients, in vitro and in vivo in animal models, are summarized in Fig. 4.
Anti-NMDA-NR2A/B antibodies are present in a subpopulation of patients with Systemic Lupus Erythematosus that have neuropsychiatric problems, and in animal models of this disease
Systemic Lupus Erythematosus and ‘Neuropsychiatric lupus’
The autoimmune disease Systemic Lupus Erythematosus (SLE) is characterized by impairment of B cell and T cell functions, cytokine dysregulation and immune complex depositions, which are accompanied by systemic clinical manifestations (Hahn 1993; Thanou and Merrill 2014; Winchester 1996). The hallmark of SLE is the presence of a variety of autoimmune antibodies that are directed mostly against dsDNA, nuclear antigens, ribonucleoproteins and certain cell surface antigens.
‘Neuropsychiatric SLE’ is a generic term for the cerebral manifestations that may arise in SLE patients (Asano et al. 2013; Borchers et al. 2005; Fanouriakis et al. 2013; Hahn 1993; Thanou and Merrill 2014; Winchester 1996). Definitions and normative descriptions for ‘Neuropsychiatric SLE’ syndromes have been proposed by the American College of Rheumatology (1999). Based on various reports, ‘Neuropsychiatric SLE’ affects 15–80 % of individuals with SLE (Borchers et al. 2005), and the great variability is attributed, at least in part, to the lack of standardized case definitions and assessment of this neurological impairment (Asano et al. 2013; Borchers et al. 2005; Fanouriakis et al. 2013; Hahn 1993; Thanou and Merrill 2014; Winchester 1996).
The disturbances in ‘Neuropsychiatric SLE’ may be only neurological, as seizures and demyelinating syndromes, of a more psychological nature, as in mood disorders and psychoses, or cognitive abnormalities. In fact, any major area of cognitive functioning can be impaired in SLE patients, but deficits are most consistently observed in tasks assessing psychomotor speed, complex attention and memory (i.e., short-term, long-term, verbal and visuospatial memory) (Asano et al. 2013; Borchers et al. 2005; Fanouriakis et al. 2013; Hahn 1993; Rheumatology 1999; Thanou and Merrill 2014; Winchester 1996).
No definite single mechanism has consistently been proven to be responsible for the wide range of ‘Neuropsychiatric SLE’ manifestations. However, the association of ‘Neuropsychiatric SLE’ with the ‘Anti Phospholipid Syndrome (APS)’, with anti-phospholipid antibodies which are present in 25–40 % of SLE patients, and with other autoimmune antibodies like those that are directed against the ribosomal phosphoproteins P0, P1 and P2, or those directed against the NMDA-NR2A/B subunits of the glutamate/NMDA receptors (discussed in much further detail below), suggests that such autoimmune antibodies can indeed contribute to the pathophysiology of ‘Neuropsychiatric SLE’ (Asano et al. 2013; Borchers et al. 2005; Fanouriakis et al. 2013; Levite and Ganor 2008).
Advances in neuroimaging techniques and cognitive testing have improved the diagnosis of ‘Neuropsychiatric SLE’ and allowed earlier and more successful therapeutic intervention (Borchers et al. 2005). Further, the association of ‘Neuropsychiatric SLE’ with the anti-phospholipid antibodies present in APS, other autoimmune antibodies and inflammatory cytokines has also provided clues for the diagnosis and pathophysiology of this disease. Treatment of ‘Neuropsychiatric SLE’ is largely symptom-based, and the outcome depends on appropriate diagnosis (Borchers et al. 2005).
There are several animal models of SLE, which develop spontaneously in several animal strains following naturally occurring genetic mutations. In these models, the uncontrolled autoimmunity in the periphery is often accompanied by behavioral disturbances that are chronic and progressive. MRL-lpr/lpr mice develop spontaneously an accelerated and aggressive SLE-like illness that is characterized by immune-mediated damage to several organs, such as the heart, kidney, brain, lungs, joints and brain. This animal model and few others have been used thus far for investigating the cognitive impairments in SLE (Asano et al. 2013; Borchers et al. 2005; Fanouriakis et al. 2013; Levite and Ganor 2008; Tomita et al. 2004).
Summary of the involvement of anti-NMDA-NR2A/B antibodies in SLE
The NMDA receptors that contain the NR2A and NR2B subunits are expressed in neurons throughout the brain, but are at highest density within cells of the hippocampus, amygdala and hypothalamus.
Anti-NMDA-NR2A/B antibodies were detected thus far by several groups in a significant proportion of patients with SLE. The exact percentage of SLE patients having anti-NMDA-NR2A/B antibodies varies in different studies as follows: 35 % (Hanly et al. 2006), 33 % (Lapteva et al. 2006), 31 % (Husebye et al. 2005), 26 % (Harrison et al. 2006), 19 % (Omdal et al. 2005) and 14 % (Kozora et al. 2010).
The anti-NMDA-NR2A/B antibodies will be discussed in much further detail below in parts 6.1.3 and 6.1.4. In some cases (but not always) the NMDA-NR2A/NR2B antibodies also bind dsDNA, and as such can be seen as cross-reactive anti-NMDA-NR2A/NR2B/dsDNA antibodies. In some cases (but again, not always) the anti-NMDA antibodies, or in fact the cross-reactive anti-NMDA-NR2A/NR2B/dsDNA antibodies, correlate with the neuropsychiatric complications of the SLE patients. This way or another (regardless of the cross-reactivity with dsDNA), the most important finding on this topic, revealed by some studies that were performed in lupus-prone mice, is that the anti-NMDA-NR2A/NR2B antibodies are undoubtedly neurotoxic by accessing the brain and eliciting neuronal death, with ensuing cognitive dysfunction and emotional disturbance ! (DeGiorgio et al. 2001 #101; Kowal et al. 2004 #238; Kowal et al. 2006 #237; Husebye et al. 2005 #205; Omdal et al. 2005 #304; Rice et al. 2005 #324; Huerta et al. 2006 #202; Lapteva et al. 2006 #247; Hanly et al. 2006 #181; Harrison et al. 2006 #183; Yoshio et al. 2013 #404; Steup-Beekman et al. 2007 #354; Arinuma et al. 2008 #23; Levite 2008 #257; Kozora et al. 2010 #241; Gao et al. 2010 #161; Faust et al. 2010 #128; Gono et al. 2011 #169; Appenzeller 2011 #21; Sato et al. 2011 #333; Lauvsnes and Omdal 2012 #249; Kowal and Diamond (2012 #239; Lauvsnes et al. 2013 #248).
In their recently published paper, Lauvsnes and Omdal review the most relevant mechanisms known so far for ‘Neuropsychiatric SLE’, with a special emphasis on the role of the anti-NMDA-NR2 antibodies (Lauvsnes and Omdal 2012). The review covers the published articles on anti-NMDA-NR2 antibodies and brain involvement, and discuss the studies in mice in which anti-NMDA-NR2 antibodies gained access to the brain, either due to their injection directly into the brain, or due to systemic immunization and abrogation of the BBB. Once they were in the brain, the anti-NMDA-NR2 antibodies induced neuronal cell death and subsequent neuropsychopathology: either impaired memory and hippocampal atrophy, or emotional disturbances and atrophy of the amygdala that followed the neuronal death, seemingly dependent on the method used in the studies for disruption of the BBB. The review also discusses the very interesting recent findings showing that the effect of the anti-NMDA-NR2 antibodies is dose-dependent: at low concentrations the anti-NMDA-NR2 antibodies alter synaptic function, while at higher concentrations they can cause neuronal cell death by apoptosis. According to this review, an association between anti-NMDA-NR2 antibodies and ‘Neuropsychiatric SLE’ has been confirmed in 6 out of 13 human studies performed altogether on this topic, and the documented manifestations are primarily of diffuse cerebral character (Lauvsnes and Omdal 2012). The findings of the most important studies on this topic will be summarized here in the coming parts 6.1.3, 6.1.4 and 6.1.5.
The presence of anti-NMDA-NR2 antibodies that cross-react with dsDNA in patients with lupus, their association with neuropsychiatric impairments, their pathogenic activity in the brain of animal models, and their mechanism of action
Anti-dsDNA antibodies are the hallmark of SLE and cause profound immune complexes and tissue damage (Hahn 1998). Pioneering studies by DeGiorgio et al. (2001) demonstrated that the pentapeptide Asp/Glu-Trp-Asp/Glu-Tyr-Ser/Gly (DWEYS) is present both in dsDNA and in aa 283–287 of the extracellular ligand binding domain of the murine and human NMDA receptor subunits NR2A and NR2B. Thus, it was surprisingly revealed that the NMDA NR2 subunit was recognized by both murine and human anti-DNA antibodies. Cross-reactive anti-NMDA-NR2 (aa 283–287)/dsDNA antibodies were detected in the serum of four SLE patients, and in the CSF of one patient. Importantly, the cross-reactive anti-NMDA-NR2 (aa 283-287)/dsDNA antibodies were found to be very pathogenic, since they mediated apoptotic death of neurons in vivo and in vitro (DeGiorgio et al. 2001). Furthermore, DeGiorgio et al. (2001) showed that the DWEYS epitope is also recognized by the unique murine anti-dsDNA monoclonal antibody named R4A. Upon intracerebral injection of affinity-purified human NMDA-NR2 (aa 283–287)/dsDNA antibodies derived from SLE patients, or of the murine R4A monoclonal antibody, into the brain of C57BL/6 mice, death of neurons in the hippocampus and cortex was documented in vivo. This neuronal death caused by the anti-NMDA-NR2 (aa 283–287)/dsDNA antibodies was mediated by activation of NMDA receptors and by induction of ‘Excitotoxicity’, alike induced by excess levels of glutamate or glutamate agonists, or by excitotoxic anti-AMPA-GluR3B antibodies (Levite et al. 1999) or by excitotoxic anti-LP-BM5 virus/AMPA cross-reactive antibodies (Koustova et al. 2001) (Basile et al. 2001). Systemic administration of the NMDA antagonist MK-801 before the administration of the human anti-NMDA-NR2 (aa 283–287)/dsDNA antibodies, or of the anti-dsDNA R4A antibody, prevented these antibodies from inducing neuronal injury. In vitro, adding the affinity-purified human anti-NMDA-NR2 (aa 283–287)/dsDNA antibodies, or the anti-dsDNA R4A antibody to neuronal cultures, caused apoptotic cell death of primary neurons (DeGiorgio et al. 2001).
Taken together, all these observations showed that in some SLE patients there are cross-reactive autoimmune antibodies that bind both DNA and NMDA receptors, and that such antibodies are often present in the CSF, activate NMDA receptors, kill neurons by ‘Excitotoxicity’, and may mediate non-thrombotic and non-vasculitic abnormalities of the CNS. These findings also led to a novel notion, that in some SLE patients the binding of NMDA receptors in the brain by the cross-reactive anti-NMDA-NR2 (aa 283–287)/dsDNA antibodies may induce the neurological/psychiatric complications often associated with SLE and called collectively ‘Neuropsychiatric SLE’.
In later studies, BALB/c mice immunized with the DNA peptide mimotope arrayed as an octamer on a polylysine backbone (MAP peptide) developed cross-reactive anti-NMDA-NR2 (aa 283–287)/dsDNA antibodies (Kowal et al. 2004; Huerta et al. 2006). Upon abrogation of the BBB, these antibodies gained access to the CNS, bound neurons and caused neuronal death. Interestingly, in these animal models, the manner by which the BBB was disrupted determined the brain region that was affected, and also the CNS impairment that followed. Thus, administration of Lipopolysaccharide (LPS) to the MAP peptide-immunized mice led to antibody-mediated damage in the hippocampus and to memory disturbance (as assessed by performance in T-maze tasks) (Kowal et al. 2004), while treatment with Epinephrine, which breaks the BBB in a different manner, led to neuronal loss in the amygdala, and to a behavioral change marked by aberrant pavlonian fear conditioning (as assessed in an electric shock model) (Huerta et al. 2006).
In another study, Kowal et al. (2006) showed that serum extracted from lupus patients, that contained antibodies that reacted with both DNA and NMDA receptors, elicited cognitive impairment in mice receiving the serum intravenously, and given LPS to compromise the BBB integrity. Brain histopathology showed hippocampal neuron damage, and behavioral testing revealed hippocampus-dependent memory impairment.
To determine whether the anti-NMDA receptor antibodies existed in the brains of the SLE patients, Kowal et al. (2006) eluted IgG from the brain of an SLE patient, and studied its binding profile and effect in vivo when injected to mice. The IgG bound both DNA and NMDA receptors and caused neuronal apoptosis when injected into brains of mice. Four more brains of patients with ‘Neuropsychiatric lupus’ were then examined and found to have endogenous IgG colocalizing with anti-NMDA receptor antibodies. These findings showed that SLE patients have circulating anti-NMDA receptor antibodies that are capable of causing neuronal damage and memory deficit if they breach the BBB, and that these antibodies also exist within the brains of the SLE patients.
Another important study by Omdal et al. (2005) identified anti-NMDA-NR2 antibodies that were directed against the decapeptide DWEYSVWLSN that contains the DWEYS sequence, in the sera of 19 % of SLE patients. Furthermore, poor performances on several cognitive and psychological tests were significantly associated with elevated levels of these anti-NMDA-NR2 antibodies. These findings indicated an association between anti-NMDA-NR2 antibodies and depressed mood, in addition to decreased short-time memory and learning, and suggested that anti-NMDA-NR2 antibodies may indeed represent one of the several mechanisms responsible for the cerebral dysfunction in SLE patients (Omdal et al. 2005).
Lapteva et al. (2006) assessed the association of cognitive dysfunction and depression with serum anti-NMDA-NR2A antibodies, and analyzed the clinical and neuroimaging correlates in SLE patients. Sixty SLE patients underwent neurocognitive assessment, evaluation for depression with the Beck Depression Inventory II (BDI-II) and psychiatric interview [Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria], Brain Magnetic Resonance Imaging (MRI), and proton magnetic resonance spectroscopy imaging. Cognition was assessed in five domains: memory, attention/executive, visuospatial, motor, and psychomotor, and adjusted to each individual’s best level of prior cognitive functioning estimated from the reading subtest of the Wide Range Achievement Test-3 (WRAT-3). Serum anti-NMDA-NR2A antibodies were measured by ELISA using a pentapeptide from the human NMDA receptor. Lapteva et al. found cognitive dysfunction in 28 of 60 (46.6 %) patients (mild in 8, moderate in 20) before adjustment for WRAT-3, and in 35 of 60 (58.3 %) patients (mild in 15, moderate in 11, and severe in 9) after adjustment for WRAT-3. The changes were most pronounced in the memory and visuospatial domains. On 1H-MRSI, patients with moderate or severe cognitive dysfunction had significantly higher choline:creatine ratios in the dorsolateral prefrontal cortex and the white matter, compared with patients with mild or absent cognitive dysfunction.
Twenty of 60 (33 %) patients were positive for anti-NMDA-NR2A antibodies Lapteva et al. (2006). There was no significant association between the levels of the anti-NMDA-NR2A antibodies and cognition. Yet, the anti-NMDA-NR2A antibodies correlated significantly with the BDI scores; patients with BDI-II scores of ≥14 had higher serum levels of anti-NMDA-NR2A antibodies (p = 0.005, 95 % confidence interval 0.83, 4.31), and there was a trend towards higher levels of anti-NMDA-NR2A antibodies among patients who fulfilled the DSM-IV criteria for major depression. Lapteva et al. (2006) concluded that serum anti-NMDA-NR2A antibodies are associated with depressive mood, but not with cognitive dysfunction, in SLE.
In a recent and important study by Faust et al. (2010), novel, unique and interesting features were found on two distinct mechanisms of action by which cross-reactive anti-NMDA-NR2/dsDNA antibodies can alter brain function (Faust et al. 2010). This study continued the investigations of the same group of researchers on such cross-reactive antibodies, which already showed in adult mouse models that when the BBB is compromised, these cross-reactive anti-NMDA-NR2/dsDNA antibodies access the brain and induce neuronal death with ensuing cognitive dysfunction and emotional disturbance. In their newer study, Faust et al. (2010) found that the cross-reactive anti-NMDA-NR2/dsDNA antibodies had two very different effects, either positive or negative, at two different concentrations: at low concentration they were positive modulators of receptor function that increased the size of NMDA receptor-mediated excitatory postsynaptic potentials, whereas at high concentration they were pathogenic as they promoted ‘Excitotoxicity’ through enhanced mitochondrial permeability transition. Thus, the local concentration of the cross-reactive anti-NMDA-NR2/dsDNA antibodies determined the exact nature of their effect in the brain.
Activation of NMDA receptors was required for producing both the synaptic and the mitochondrial effects. Other synaptic receptors were completely unaffected by the anti-NMDA-NR2/dsDNA antibodies.
Faust et al. (2010) argued that their findings reveal the mechanisms by which autoimmune anti-NMDA-NR2 antibodies trigger graded cellular alterations, which are likely to be responsible for the transient and permanent neuropsychiatric symptoms observed in SLE patients.
Arinuma et al. (2008) tested if anti-NMDA-NR2A IgG antibodies are present in the serum and CSF of 56 patients with ‘Neuropsychiatric lupus’: 38 with diffuse psychiatric/neuropsychological syndromes (diffuse ‘Neuropsychiatric lupus’), and 18 with neurologic syndromes or peripheral neuropathy (focal ‘Neuropsychiatric lupus’), in comparison to 20 control patients with non-inflammatory neurologic diseases. The findings were rather surprising: the levels of anti-NMDA-NR2A antibodies in the CSF were significantly elevated in patients with diffuse ‘Neuropsychiatric lupus’, compared to the control patients, or to the patients with focal ‘Neuropsychiatric lupus’. In contrast, there were no significant differences in the levels of the anti-NMDA-NR2A antibodies in the serum of the patients in the three groups. In 31 of the 38 (81.6 %) patients with diffuse ‘Neuropsychiatric lupus’, and in 8 of the 18 (44.4 %) patients with focal ‘Neuropsychiatric lupus’, the levels of anti-NMDA-NR2 antibodies in the CSF were more than 3 standard deviation (SD) above their mean level in the control patients. The conclusion based on these important findings was that anti-NMDA-NR2A antibodies in CSF, but NOT in serum, are associated with diffuse ‘Neuropsychiatric lupus’ (Arinuma et al. 2008). In view of these findings, it is essential to test for anti-NMDA-NR2 antibodies in the CSF of patients. Moreover, it is important to bear in mind that one should treat the patients that have such autoimmue antibodies with immunotherapeutic drugs or procedures that are able to decrease the levels, or suppress the activity, of these autoimmune anti-glutamate receptor antibodies in the ‘site of crime’: the brain, since using drugs and treatments that have only peripheral effects may be useless, especially in cases where there is an intrathecal production of anti-NMDA-NR2 antibodies.
The recent and very interesting study by Yoshio et al. (2013) reveals another new insight into the unique and completely unexpected effects of the cross-reactive anti-NMDA-NR2/dsDNA antibodies present in SLE patients, primarily associated with their ability to activate endothelial cells (ECs) in the BBB. In further detail, Yoshio et al. found that purified anti-NMDA-NR2 IgG antibodies present in some SLE patients bound dsDNA in an IgG-dose-dependent manner, and that this interaction up-regulated the expression of endothelial leukocyte adhesion molecule 1, vascular cell adhesion molecule 1, and intercellular adhesion molecule 1, on the EC surface. This interaction led to additional surprising effects: increased production by ECs of the pro-inflammatory IL-6 cytokine, and of the IL-8 chemokine, but not of two other pro-inflammatory cytokines: tumor necrosis factor alpha (TNFα) and IL-1beta. The purified anti-NMDA-NR2 antibodies also activated the degradation of cytoplasmic IkappaB, indicating the activation of NF-kappaB in the ECs. Based on these findings, Yoshio et al. (2013) proposed that EC activation through the NF-kappaB signaling pathway induced by anti-NMDA-NR2 IgG antibodies in the CNS of SLE patients may lead to inflammation of the BBB, and initiate the pathogenesis of ‘Neuropsychiatric SLE’.
Finally, in their recent paper published in ‘Methods Mol Biol’, Kowal and Diamond (2012) describe the methods they utilized for establishing a mouse model of anti-NMDA-NR2 antibodies and ‘Neuropsychiatric lupus’. In this paper, they provide useful basic concepts and protocols for the following: (1) Induction of anti-NMDA/dsDNA antibodies, (2) Testing by ELISA the levels of such antibodies in the serum, (3) Breaching the BBB integrity with LPS and Epinephrine, (4) Passive transfer of pathology by injecting the human and mouse brain-reactive autoimmune anti-glutamate receptor antibodies into adult mouse, as well as injecting these antibodies into gestating mice and transfer of the antibodies from dam to fetus, (5) Blocking NMDA receptor-mediated pathogenicity in vivo, (6) Evacuation of blood from the brain by cardiac perfusion to preserve the brain for histology, (7) Evaluating injured/apoptotic neurons in brain histology, (8) Preparing membrane-enriched brain fractions for NMDA receptor analysis (Kowal and Diamond 2012).
The presence in SLE patients of anti-NMDA-NR2 antibodies that cross-react with dsDNA, but that do not associate with psychiatric impairments
In contrast to all the findings described above in part 6.1.3, few studies published during the past years claim that although anti-NMDA-NR2A antibodies are indeed present in a substantial proportion of SLE patients, they are NOT necessarily associated with cognitive impairments and neuropsychiatric symptoms in these patients. The findings of few of these studies are summarized in the following paragraphs.
Study 1: Lapteva et al. (2006), in a study already described in detail at the end of part 6.1.3, found that serum anti-NMDA-NR2 antibodies are associated with depressive mood, but not with cognitive dysfunction in SLE at a given time point.
Study 2: Harrison et al. (2006) found that of 93 SLE patients tested, 24 (26 %) were positive for anti-NMDA-NR2A antibodies. However, no significant association was found between the presence of these antibodies and cognitive dysfunction, depressive symptoms or anxiety. The conclusion of this study was that the presence of anti-NMDA-NR2A antibodies alone does not have a direct effect on cognitive functioning, or on any other neuropsychiatric manifestation of SLE.
Study 3: Hanly et al. (2006) found anti-NMDA-NR2A antibodies in 23 of 65 (35 %) women with SLE. Moreover, 18 of the 23 (78 %) patients that had anti-NMDA-NR2A antibodies had also anti-dsDNA antibodies. The other 22 % of SLE patients had anti-NMDA-NR2A antibodies but not anti-dsDNA antibodies, showing the existence of both cross-reactive and non-cross-reactive anti-NMDA-NR2A antibodies in SLE patients. The presence of anti-NMDA-NR2A antibodies in the circulation was not associated with cognitive dysfunction: there was no association between global cognitive impairment, domain-specific cognitive impairment, or a history of clinically overt ‘Neuropsychiatric SLE’, and between the presence or the level of anti-NMDA-NR2A antibodies or of anti-dsDNA antibodies. When a change in cognitive performance, or the occurrence of new ‘Neuropsychiatric SLE’ events over the 5-year follow-up period, was examined, no significant association with persistent elevation of either types of autoimmune antibodies was found. Similarly, there was no association between a rise in the autoimmune antibodies over time, and the development of overt neuropsychiatric events or cognitive decline. Taken together, the results of this study indicated that anti-NMDA-NR2A antibodies are present in 35 % of women with SLE, but that their presence in the circulation is not necessarily associated with cognitive dysfunction at a single time point, or with clinically overt ‘Neuropsychiatric SLE’ (Hanly et al. 2006).
Study 4: In a study by Steup-Beekman et al. (2007) the mean level of anti-NMDA-NR2A antibodies was found to be significantly elevated in the plasma of SLE patients, compared with the healthy unrelated controls, as well as in first-degree relatives of SLE patients, compared with healthy unrelated controls. However, no difference in the levels of anti-NMDA-NR2A antibodies was found between the SLE patients and their first-degree relatives, or between SLE patients with and without neuropsychiatric symptoms. Thus, while the anti-NMDA-NR2A antibodies were more frequent among SLE patients than in healthy individuals, they were not specific for patients with neuropsychiatric symptoms. The presence of anti-NMDA-NR2A antibodies in both SLE patients and their first-degree relatives suggested that a familial basis was responsible for the autoimmune response against the NMDA receptor (Steup-Beekman et al. 2007).
Study 5: Kozora et al. (2010) found elevations of serum anti-NMDA-NR2 antibodies in 14 % of 43 SLE patients without a history of major neuropsychiatric syndromes (non-NPSLE), and in 7.4 % of the healthy controls (p = 0.47). There was no relationship between an elevated anti-NMDA-NR2 antibodies status and a higher global ‘Cognitive Impairment Index’ (CII) or performance on the ‘Memory Impairment Index’ (MII). Also, no relationship between the levels of the anti-NMDA-NR2 antibodies and depressive symptoms was found. The conclusions of this study were that the frequency of elevated anti-NMDA-NR2 antibodies was low (14 %) in SLE patients and not significantly different from controls, and that there is no relationship between the presence of NMDA-NR2 antibodies in the serum of SLE patients and their global cognitive or memory indices, or with their depression (Kozora et al. 2010).
The presence in lupus patients of anti-NMDA/NR2 antibodies that do not cross-react with dsDNA, their association with various neurological impairments, and their pathogenic activity in the brain of animal models
Study 1: In one of our own studies, we tested the serum of 109 SLE patients for anti-NMDA-NR2A antibodies that recognize the 15-aa peptide SVSYDDWDYSLEARV (aa 278–292) derived from NR2A, which contains the DWEYS sequence. We found that 31 % of these SLE patients had elevated levels of such anti-NMDA-NR2A (aa 278–292) antibodies in their serum (Husebye et al. 2005). In comparison, only 6 % of the control patients with Myasthenia Gravis, 5 % patients with APS, and 4 % of healthy controls (all studied in parallel) had such anti-NMDA-NR2A antibodies (Husebye et al. 2005). Interestingly, the levels of the anti-NMDA-NR2A antibodies in the SLE patients did not correlate with the levels of their anti-dsDNA antibodies. The sera of individual SLE patients with the highest levels of anti-NR2A (aa 278–292) antibodies were negative for anti-dsDNA antibodies, and most of the sera that contained the highest levels of anti-dsDNA antibodies were negative for anti-NMDA-NR2A (aa 278–292) antibodies (Husebye et al. 2005).
These findings revealed the existence of an independent population of anti-NMDA-NR2A antibodies in SLE patients that do not cross-react with dsDNA. These NMDA-NR2A (aa 278–292) antibodies seem to differ from the cross-reactive anti-NMDA-NR2A (aa 283–287)/dsDNA antibodies that were found in some SLE patients in the studies described above, and also from the R4A anti-dsDNA antibody that cross-reacts with NMDA-NR2.
A reminder of relevant findings: In a study on 82 patients with Epilepsy of different types, we found that 18 % of them had elevated levels of anti-NMDA-NR2 antibodies, 21 % had anti-AMPA-GluR3B antibodies, and 16 % had anti-dsDNA antibodies (Ganor et al. 2005c). There was no cross-reactivity between these different types of autoimmune antibodies. Thus, there was a subpopulation of Epilepsy patients, like the SLE patients we studied and describe in Husebye et al. (2005), that had anti-NMDA-NR2 antibodies that did not cross-react with dsDNA.
Back to the study on the 109 SLE patients (Husebye et al. 2005)—in a group analysis we found no significant correlation between the presence of anti-NMDA-NR2A (aa 278–292) antibodies and any SLE-related clinical manifestation. Interestingly, however, the two SLE patients with the highest levels of anti-NMDA-NR2A (aa 278–292) antibodies had CNS manifestations, and in one of these patients, who suffered from organic brain syndrome, cranial nerve disorders and visual disturbances, the titers of the NMDA-NR2A (aa 278–292) antibodies correlated with the severity of the neurological involvement. The clinical improvement of the neurological symptoms of this specific SLE patient was associated with a significant decrease in the level of the anti-NR2A (aa 278–292) antibodies. When the neurological manifestations in this SLE patient worsened again, the level of the anti-NMDA-NR2A (aa 278–292) antibodies also increased. During this period, no anti-dsDNA antibodies were detected in the serum of this patient (Husebye et al. 2005). These observations, although not statistically significant, suggested that the anti-NMDA-NR2 antibodies may indeed associate with neurological manifestations in some SLE patients, and that in principle they may contribute to neuropathology without binding dsDNA.
Study 2: Gao et al. (2010) studied depression and various autoimmune antibodies in young MRL/lpr lupus-prone mice, and found that MRL/lpr females exhibited significant depression as early as 5 weeks (at which time elevated levels of autoimmune antibodies were already present), as compared to MRL/lpr males, where depression was noted only at 18 weeks. Depression was significantly correlated with the autoimmune antibodies directed against nuclear antigens, NMDA receptors and ribosomal P (Gao et al. 2010).
Study 3: Gono et al. (2011) found that SLE patients had anti-NMDA-NR2 antibodies that were directed specifically against either DWEYS or DWDYS core peptide present in both NMDA-NR2 and dsDNA. Yet, no correlation was found between the titer of the anti-NMDA-NR2A antibodies and the titer of the anti-dsDNA antibodies. Despite this, the non-cross-reactive anti-NMDA-NR2A antibodies associated significantly with the frequency of ‘Neuropsychiatric SLE’ (Gono et al. 2011).
Anti-NMDA-NR2A/B antibodies are present in ~20 % of Epilepsy patients
In one of our studies mentioned already in brief above (Ganor et al. 2005b), we studied 82 Epilepsy patients with different types of Epilepsy: 51 Partial Epilepsy, 20 Generalized Epilepsy, and 11 Infantile spasms, in comparison to 49 neurologically intact non-epileptic controls. We tested the sera of all these individuals for the presence of elevated levels of 3 different autoimmune antibodies, and found the following: (1) Anti-NMDA-NR2 antibodies were present in 15 of 82 (18 %) patients, (2) Anti-AMPA-GluR3B antibodies were present in 17 (21 %) patients, and (3) Anti-dsDNA antibodies were present in 13 (16 %) patients. The vast majority—14 of the 15 (93.3 %) patients that had anti-NMDA-NR2 antibodies had Partial Epilepsy. Only one patient with General Epilepsy and none with Infantile Spasms had such anti-NMDA-NR2 antibodies. Out of the 17 patients that had anti-AMPA-GluR3B antibodies, only 9 (~50 %) had Partial Epilepsy, and the other 8 (~50 %) had General Epilepsy. Interestingly, 10 of 15 (66.6 %) patients that were positive for anti-NMDA-NR2A antibodies were negative for anti-AMPA-GluR3B antibodies. Thus, individual Epilepsy patients had either of these different types of anti-glutamate receptor antibodies, or both of them, or none (Ganor et al. 2005b).These findings showed that the two types of anti-glutamate receptor antibodies are not cross-reactive. Finally, we found elevated levels of anti-dsDNA antibodies in the sera of 13 of 80 (16 %) Epilepsy patients: 6 of 49 (12 %) with Partial Epilepsy, 6 of 20 (30 %) with General Epilepsy, and only 1 of 11 (9 %) with Infantile Spasms. The majority (8 of 12) of anti-dsDNA antibody-positive Epilepsy patients had neither the NMDA-NR2 antibodies nor the AMPA-GluR3B antibodies (Ganor et al. 2005b). These findings showed that the two types of anti-glutamate receptor antibodies do not bind dsDNA.
In this study, we further found that nearly all the anti-dsDNA antibody-positive patients did not have anti-nuclear autoimmune antibodies. Most patients had no history of brain damage, febrile convulsions, early onset Epilepsy, acute Epilepsy or intractable seizures. Taken together, the findings of this study showed that antibodies against glutamate receptors are found in a significant proportion of Epilepsy patients, and that there are distinct subpopulations of Epilepsy patients that harbor in their serum either anti-AMPA-GluR3B antibodies, or anti-NMDA NR2A antibodies, or anti-dsDNA antibodies. In the discussion of this paper, we analyzed these findings and their possible implications, and recommended that a routine test for various types of autoimmune antibodies, which we collectively call ‘Autoimmune fingerprints’, would be performed on the serum, and more importantly on the CSF, of Epilepsy patients, for diagnostic and therapeutic purposes (Ganor et al. 2005b).
Anti-NMDA-NR2A/B antibodies are present in some Encephalitis patients
Anti-NMDA-R2A antibodies are not only found in a significant subpopulations of patients with either SLE or Epilepsy (as described in the preceding parts), but also in a subpopulation of patients with some types of Encephalitis, as revealed in few of the studies summarized in the coming paragraphs.
Study 1: Nakajima et al. (2007) found antibodies against glutamate receptor subunit epsilon2 (i.e., NR2B) in the CSF of a patient with chronic progressive limbic Encephalitis caused by enterovirus (the latter being a frequent cause of aseptic meningitis, particularly in children), and in whom lesions were found in the bilateral hippocampus, medial temporal lobe and hypothalamus.
Study 2: Iizuka et al. (2008) reported on anti-NMDA-NR1/NR2 heteromer antibodies in the serum/CSF of Japanese women previously diagnosed with juvenile acute non-herpetic Encephalitis of unclear etiology. An ovarian teratoma was subsequently demonstrated in three patients (all confirmed pathologically). All patients sequentially developed prodromal symptoms, psychosis, hypoventilation, severe orofacial dyskinesias and bizarre immunotherapy-resistant involuntary movements that lasted 1–12 months (Iizuka et al. 2008).
Study 3: Okamoto et al. (2007) reported on anti-NMDA-R2A antibodies in the CSF of one patient with Paraneoplastic Limbic Encephalitis. The 35 year old woman with consciousness disturbance was diagnosed initially as suffering from non-herpetic Encephalitis. Her signs and symptoms improved with Acyclovir and steroid pulse therapy. However, after the treatment, an ovarian tumor was discovered, and anti-NMDA-R2A antibodies were detected in the CSF (Okamoto et al. 2007).
Study 4: Sansing et al. (2007) found anti-NMDA-R2A antibodies in a 34 year old woman presenting with headache, feverish sensation and anxiety, that were rapidly followed by homicidal ideation, aggressive agitation, seizures, hypoventilation, hyperthermia, and prominent autonomic instability requiring intubation and sedation. The final diagnosis was of Paraneoplastic Encephalitis associated with immature teratoma of the ovary.
Anti-NMDA-NR2 antibodies are present in some patients with Transient Ischemic Attack and Stroke
Stroke is a multisystemic disorder that includes mechanisms of thrombosis and neurotoxic coupling. Key metabolites of the molecular cascade following biochemical events appear simultaneously in brain tissue, the BBB and brain vessels. In principle, one can envision how these pathological processes, and the subsequent encounter of the immune system with self-proteins in a new context of cell/tissue destruction and inflammatory milieu, can activate the immune system and generate ‘forbidden’ autoimmune antibodies and T cells directed against key brain proteins.
Dambinova et al. (2003) tested if anti-NMDA-NR2A/2B antibodies are present in altogether 360 serum samples of: 105 patients with Transient Ischemic Attack (TIA)/Stroke patients and 255 controls, including patients with controlled hypertension/atherosclerosis and gender- and age-matched healthy individuals. Patients with TIA (n = 56) and Acute Stroke (IS) (n = 31) were found to have significantly higher levels of anti-NMDA-NR2A/2B antibodies than controls (p < 0.0001). The test sensitivities for TIA and IS were 95 and 97 %, respectively, and the predictive values were 86 and 91 % at a cutoff point of 2.0 μg/L. Interestingly, monitoring the anti-NMDA-NR2A/2B antibodies within 72 h differentiated IS and ICH (p < 0.001), and was confirmed by MRI and computed tomography. Dambinova et al. (2003) concluded that anti-NMDA-NR2A/2B antibodies are independent and sensitive serologic markers capable of detecting TIA with a high post test probability and, in conjunction with neurologic observation and neuroimaging, ruling out intracerebral hemorrhage.
In a later study by the same group, Weissman et al. (2011) studied 120 patients presenting with a history of Stroke or TIA, to determine whether serum levels of anti-NMDA-NR2A antibodies reflected the presence of recent Stroke, compared with controls. The results were that males and females with multiple recent Stroke, and females with acute Stroke, had elevated levels of anti-NMDA-NR2 antibodies compared to non-Stroke patients or controls. Using a multiple regression model, the predictive value for the anti-NMDA-NR2 antibodies was compared to the clinical risk factors. In men, the presence of Stroke correlated with hypertension and the levels of anti-NMDA-NR2A antibodies, and in women the presence of Stroke correlated with Hypertension, Diabetes, Atrial fibrillation and the anti-NMDA-NR2 antibodies. These results suggested that the levels of anti-NMDA-NR2 antibodies reflect a history of multiple Strokes, and may serve as a predictive factor for Stroke (Weissman et al. 2011).
Interestingly, in another later study by the same group, Dambinova et al. (2012) studied 192 patients with suspected Stroke, and tested the levels of the NR2 peptide itself (i.e., the levels of the NMDA-NR2 antigen, not of the antibodies directed against it), which is a product of the proteolytic degradation of the NMDA receptor. The aim of this study was to find out if the levels of the NR2 peptide can differentiate Acute Ischemic Stroke (IS) from Stroke mimics and persons with vascular risk factors/healthy controls. The highest elevations in the levels of the NR2 peptide were found in patients with IS, and these peaked 12 h following symptom onset. A moderate correlation between the NR2 peptide values and the acute ischemic cortical lesions was found. Based on these findings, Dambinova et al. (2012) concluded that the NR2 peptide may be a brain-specific biomarker for diagnosis of acute IS, and may allow the differentiation of IS from stroke mimics and controls. In addition, the findings of this study suggested that the rise of the NR2 peptide levels may increase the risk of subsequent production of autoimmune anti-NMDA-NR2 antibodies that later damage the brain.
Anti-NMDA-NR2 antibodies are present in some patients with Sjogren’s syndrome, and associate with impaired learning and memory, and with depression
Sjogren's syndrome is a chronic autoimmune and inflammatory disease in which the body's white blood cells destroy the exocrine glands, specifically the salivary and lacrimal glands, that produce saliva and tears, respectively. Lauvsnes et al. (2013) reported on memory dysfunction in primary Sjogren’s syndrome that is associated with anti-NMDA-NR2 antibodies in the serum and CSF. The aim of this study was to understand the etiology and pathogenesis of the neuropsychiatric involvement in primary Sjogren’s syndrome, and to investigate the possible contribution of anti-NMDA-NR2 antibodies to these neuropsychiatric problems.
For this reason, 66 patients with Sjogren’s syndrome and 66 age- and sex-matched healthy control underwent clinical examination and neuropsychological evaluation. Anti-NMDA-NR2 antibodies were measured in the serum and CSF. Hippocampus volume was estimated using software extensions to SPM5. Lauvsnes et al. found that the patients with primary Sjogren’s syndrome had smaller hippocampi than healthy subjects. In patients with primary Sjogren’s syndrome, the anti-NMDA-NR2 antibodies in the CSF associated with a worse performance in 8 of 10 memory and learning tests. The anti-NMDA-NR2 antibodies in the serum were associated with a worse performance in 6 of those same tests. In addition, a higher proportion of patients with depression than patients without depression had serum anti-NMDA-NR2 antibodies levels above the cutoff value. Based on these findings, Lauvsnes et al. (2013) concluded that anti-NMDA-NR2 antibodies may represent one of the pathogenetic mechanisms for cognitive disturbances and mood disorders in patients with primary Sjogren’s syndrome.
Anti-NMDA-NR2 antibodies and anti-NMDA NR1/NR2 heterodimer antibodies are present in a small subpopulation of patients with Schizophrenia or Mania
Study 1: Anti-NMDA-NR 1 / 2 heterodimer antibodies were found in ~10 % of Schizophrenia patients with initial diagnosis of the disease. Steiner et al. (2013) compared the specificity and prevalence of anti-NMDA receptor antibodies in Schizophrenia (DSM-IV criteria) with those of other psychiatric diagnoses, and with those of ‘Anti-NMDA receptor Encephalitis’. The serum of 459 patients admitted with acute Schizophrenia, Major Depression (MD) or Borderline Personality Disorder (BLPD), and of individuals serving as matched controls, was obtained from the scientific blood bank, and tested for the following types of anti-glutamate receptor antibodies: (1) Anti-NMDA-NR1 IgA/IgG/IgM antibodies, (2) Anti-NR1A/NR2B heterodimer antibodies, and (3) Anti-AMPA-GluR1/GluR2 antibodies. Unfortunately, the serum of the patients was not tested for anti-AMPA-GluR3B antibodies. Two hundred and thirty matched healthy controls were compared with patients (unmedicated for at least 6 weeks) with Schizophrenia (n = 121), MD (n = 70), or BLPD (n = 38). The primary outcome was the overall number of seropositive cases for anti-NR1A/NR2B antibodies and for anti-AMPA-GluR1/GluR2 antibodies; the secondary outcome was disease specificity of IgA/IgG/IgM antibodies and epitope specificity for clinical subgroups. Diverse anti-NMDA receptor antibodies were identified in 15 subjects, primarily those with an initial Schizophrenia diagnosis (9.9 %), opposed to MD (2.8 %), BLPD (0), and controls (0.4 %). Retrospectively, 2 patients initially classified as having catatonic or disorganized Schizophrenia were reclassified as having misdiagnosed ‘Anti-NMDA-NR1 Encephalitis’ (with specific serum and CSF IgG anti-NMDA-NR1A antibodies). In all other seropositive cases, the antibodies consisted of classes IgA and/or IgM, or were directed against NR1A/NR2B heterodimer, and not against the NR1A alone. None of the patients or controls had anti-AMPA GluR1/2 antibodies. Steiner et al. (2013) concluded that acutely ill patients with an initial Schizophrenia diagnosis show an increased prevalence of anti-NMDA receptor antibodies, and that the repertoire of antibody subtypes in patients with Schizophrenia and MD is different from that in patients with ‘Anti-NMDA receptor Encephalitis’. On this basis, they recommend that the latter disorder should be considered as a differential diagnosis, particularly in young females with acute disorganized behavior or catatonia.
Study 2: Anti-NMDA-NR 2 antibodies are elevated during the acute phase of Mania. Dickerson et al. (2012) measured the levels of anti-NMDA-NR2 antibodies in the serum of 60 individuals with different subtypes of Mania, including schizoaffective cases. The patients were assessed up to three time points. In addition, these antibodies were measured in 295 individuals with other psychiatric diseases, and in 170 non-psychiatric controls. The individuals with Mania were found to have increased levels of anti-NMDA-NR2 antibodies during the acute phase of Mania, but not at follow-up or later evaluation times. The levels of the anti-NMDA-NR2 antibodies in individuals with other psychiatric diseases did not differ significantly from the levels measured in the control population. Within the Mania group, there was a significant decrease in the antibody levels over the three time points of the study. Dickerson et al. (2012) concluded that anti-NMDA-NR2 antibodies are elevated during the acute phase of Mania, and that they may play a role in the pathogenesis of acute Mania.
Paper 3—Review: Approximately 8 % (115 of 1,441) of patients with Schizophrenia/psychosis were found so far to have anti-NMDA receptor antibodies. Pollak et al. (2013) wrote a review on anti-NMDA receptor antibodies in Schizophrenia, based on their systematic literature search aimed to establish what proportion of patients with Schizophrenia and related psychoses were found so far to have such antibodies. The studies that were taken into consideration were those fulfilling the following criteria: (1) Patients had a diagnosis of Schizophrenia, Schizophrenia spectrum disorder, or First Episode Psychosis (FEP) using standard criteria, (2) The serum was analyzed for the presence of anti-NMDA receptor antibodies, and (3) The purpose of the study was to look for the presence of anti-NMDA receptor antibodies in patients with a primary psychiatric diagnosis without clinical signs of Encephalitis. The review reports on seven studies comprising altogether 1,441 patients, of whom 115 (7.98 %) were found to have anti-NMDA receptor antibodies. Of these, 21 (1.46 %) patients had anti-NMDA receptor antibodies of the IgG subclass. Prevalence rates were greater in patients than in controls only for IgG anti-NMDA receptor antibodies; other subclasses were of less certain etiological relevance. There was a significant heterogeneity in terms of patient characteristics and the antibody assay used. Pollak et al. (2013) concluded that a minority of patients with Psychosis have anti-NMDA receptor antibodies, and that it remains to be established whether this subset of patients differs from antibody-negative patients in terms of underlying pathology and response to antipsychotic treatment, and whether immunomodulatory treatments are effective in alleviating psychotic symptoms in this group.
Paper 4—Review: Maneta and Garcia (2013) wrote a review on the role of the NMDA receptor in both ‘Anti-NMDA receptor Encephalitis’ and Schizophrenia, in terms of symptom presentation and neurobiology. They claim that there is an increasing need for psychiatrists to become aware of the disorder and consider it in their differential diagnosis, as they are often the first to be consulted on patients with ‘Anti-NMDA receptor Encephalitis’. They also argue that similarities identified between ‘Anti-NMDA receptor Encephalitis’ and Schizophrenia spectrum illnesses raise questions about a common underlying pathophysiology, particularly with regard to the NMDA receptor (Maneta and Garcia 2013).
Anti-NMDA NR1/NR2 heterodimer antibodies are present in ~30 % of patients with Herpes Simplex Encephalitis
Pruss et al. (2012a) found anti-NMDA-NR1/NR2 heterodimer antibodies of the IgA, IgG, or IgM immunoglobulin subtypes in 13 of 44 (30 %) patients in the course of Herpes Simplex Encephalitis. These anti-NMDA receptor antibodies reacted only with NMDA-NR1/NR2 heterodimers, and not with the NMDA-NR1 alone. Such anti-NMDA-NR1/NR2 heterodimer antibodies were often present at hospital admission, but in some patients developed after the first week of Herpes Simplex Encephalitis. As already mentioned in part 5.3, patient’s serum containing the anti-NMDA-NR1/NR2 heterodimer antibodies caused substantial decrease of NMDA receptors in the membrane fraction of primary hippocampal neurons growing in tissue culture, and also reduced markedly the expression of the synaptic marker Synapsin in these cells, in comparison to sera of healthy individuals that did not induce such effects (Pruss et al. 2012a). Taken together, these findings showed that some patients with Herpes Simplex Encephalitis develop IgA, IgG, or IgM anti-NMDA-NR1/NR2 heterodimer antibodies, and suggest that these antibodies alter the density of neuronal synaptic markers and, by doing so, induce neuropathology. The findings of this study also suggested that a subgroup of patients with Herpes Simplex Encephalitis that have anti-NMDA receptor antibodies may benefit from immunotherapy (Pruss et al. 2012a).
Antibodies to Metabotropic glutamate receptors in neurological diseases
On top of the antibodies to Ionotropic glutamate receptors—the anti-AMPA receptor antibodies and the anti-NMDA receptors antibodies—found so far in various neurological diseases, as described in the preceding parts of this review, antibodies to Metabotropic glutamate receptors, mainly of two types—anti-mGluR1 antibodies and anti-mGluR5 antibodies—were found in the serum and CSF of very few patients with either Paraneoplastic Cerebellar Ataxia or Hodgkin lymphoma and Limbic Encephalopathy (Ophelia syndrome), respectively (Coesmans et al. 2003; Sillevis Smitt et al. 2000). Importantly, the anti-mGluR antibodies are often in much higher levels in the CSF than in the serum due to intrathecal production, and they can be very detrimental to the CNS. The main findings revealed thus far regarding anti-mGluR antibodies are summarized in Fig. 5, and also discussed in further detail in the coming parts 9.1 and 9.2.
Antibodies to Metabotropic glutamate receptor 1 (mGluR1) antibodies are: present in serum and CSF of some patients with Paraneoplastic Cerebellar Ataxia, being produced intrathecally, and cause Cerebellar Ataxia in mice by functional blocking of mGluR1 in the cerebellum
Study 1: Two patients with severe Cerebellar Ataxia that developed during remission from Hodgkin’s disease had anti-mGluR1 antibodies in their serum and CSF (Sillevis Smitt et al. 2000).
A. Background: There are many types of Cerebellar Ataxia, including Ataxia due to congenital or metabolic disorders, and a paraneoplastic form in patients with gynecologic cancer, breast cancer, lung cancer, or a specific type of lymphoma (i.e., cancer of the lymphatic system)—Hodgkin’s disease (Sillevis Smitt et al. 2000). In Hodgkin’s disease, the lymphoma precedes the ataxia by months to years in 80 % of patients, and the Ataxia often occurs during a prolonged complete remission. Among patients with this type of Ataxia, 30 % have anti-Purkinje-cell antibodies, some of which have the features of the specific anti-neuronal antibodies named anti-Tr. antibodies (Graus et al. 1997; Hammack et al. 1992; Sillevis Smitt et al. 2000; de Graaff et al. 2012).
B. Two patients with severe Cerebellar Ataxia, that developed during remission from Hodgkin’s disease, were found to have anti-mGluR 1 antibodies in their serum and CSF. The serum and CSF of these patients bound neurons in several brain regions in a pattern similar to the distribution of the mGluR 1. Sillevis Smitt et al. (2000) described in their very interesting case report (published in New England Journal of Medicine) two patients with severe Cerebellar Ataxia that developed while they were in remission from Hodgkin’s disease. The diagnosis of one patient was Paraneoplastic Cerebellar Ataxia, and that of the other was severe Cerebellar Ataxia and short-term memory loss. Sillevis Smitt et al. found anti-mGluR1 antibodies in the serum and CSF of both patients. Moreover, the serum and CSF of both patients displayed similar specific immunohistochemical staining patterns on sections of mouse brain. Purkinje-cell bodies were strongly stained, and distinctive punctate staining, compatible with labeling of the Purkinje-cell spines, was observed in the molecular layer of the cerebellum. Strong staining of neurons and neuropil was also observed in the glomeruli of the olfactory bulb, the olfactory tubercle (including the islands of Calleja), the superficial layer of the cerebral cortex, the CA3 area of the hippocampus, the thalamus, the superior colliculus, and the spinal trigeminal nucleus. The immunohistochemical staining pattern appeared to be similar to the distribution of the mGluR1. To confirm the specificity of the reactivity of the serum with native mGluR1 proteins, living CHO cells that expressed rat mGluR1 or mGluR5a were incubated with the serum of both patients. It was found that the two serum samples strongly labeled CHO cells that expressed mGluR1, but not the cells that expressed mGluR5a. The reactivity of the patient’s IgG and CSF with CHO cells that expressed human mGluR1, and with human cerebellar sections, was also demonstrated. These findings indicated that antibodies of the IgG isotype, which were present in the serum and CSF of both patients, reacted specifically with the amino-terminal extracellular domain of the native mGluR1. Normal human IgG had no effect. IgG from the two patients did not block the activation of mGluR5a, a finding indicating its specificity to mGluR1.
C. The patient’s anti-mGluR 1 antibodies blocked a glutamate-induced effect in vitro, and were very pathogenic in the brain in vivo, as they caused a rapid, very severe and reversible Ataxia in mice. Sillevis Smitt et al. further found that purified IgG derived from the serum of both patients blocked a glutamate-induced effect, namely glutamate-stimulated formation of inositol phosphates in Chinese-hamster-ovary (CHO) cells that expressed mGluR1α. Moreover and of the highest importance was the observation that these antibodies were very pathogenic in vivo. Thus, 30 mins after injection of the antibodies of the IgG isotype derived from the two patients into the subarachnoid space of normal mice, near the cerebellum, the mice became increasingly ataxic, with a wide gait!. These mice were unable to walk a straight line, and the distance between their steps was small and irregular, an indication of cerebellar dysfunction. At the peak of the symptoms, the most strongly affected mice could hardly walk or stand up because of severe truncal Ataxia. As assessed by the RotoRod test, the ataxic behavior peaked at about 2–4 h. after the injection of the patient’s IgG and subsided after 24 h. Significant effects on the behavior of the mice could be detected with as little as 10 μg of IgG from Patient 1. No effect was detected with the control normal human IgG. The in vivo effect induced by the IgG from the patients was caused by the anti-mGluR1 antibodies and not by other antibodies, since when the patient’s IgG was absorbed with mGluR1, it completely lost its effect, but when it was absorbed with mGluR5a it remained effective. The injected IgG was restricted largely to the cerebellum, and penetrated throughout various layers of the cerebellar cortex. Furthermore, antibodies eluted from the cells that expressed mGluR1 caused similar ataxic behavior in mice at a low concentration.
Together, these striking and important findings indicated that anti-mGluR1 antibodies derived from two patients with Paraneoplastic Cerebellar Ataxia caused Cerebellar Ataxia in mice, by functional blocking of mGluR1 in the cerebellum (Sillevis Smitt et al. 2000).
D. The anti-mGluR 1 antibodies were synthesized intrathecally in the two patients with Paraneoplastic Cerebellar Ataxia. The titers of the anti-mGluR1 antibodies in the CSF and serum samples of both the patients discussed above were examined by end-point titration of immunohistochemical mGluR1 staining in sections of rat brain (Sillevis Smitt et al. 2000). Before Patient 1 received plasma exchanges, the titers of the anti-mGluR1 antibodies in her CSF and serum were 512 and 3200, respectively. When these values were normalized according to concentrations of IgG, the anti-mGluR1 antibody titer per unit of IgG was 31 times as high in CSF as in serum (!)—an indication of intrathecal antibody synthesis. Using these values, Sillevis Smitt et al. (2000) found that the anti-mGluR1 antibody content in the CSF was 25 times as high as that in the IC of serum IgG. In Patient 2, after she received plasma exchanges, the anti-mGluR1 titer in serum was 400, and the titer in CSF was 256. Normalized according to IgG concentrations, the anti-mGluR1 IgG titer per unit of IgG was 36 times as high in CSF as in serum (!). In Patient 2, the content of anti-mGluR1 antibody in CSF was, therefore, 28 times that in the IC50 of serum IgG.
D. One of the two patients with the severe Cerebellar Ataxia, that was found to have anti-mGluR 1 antibodies in the serum and CSF, responded very well to immunotherapy, in correlation with a drop in the levels of these antibodies. Patient 1—In this patient, the most striking symptom at presentation was gait ataxia. This patient was unable to walk with a tandem gait. At that time, the titers of the anti-mGluR1 antibodies in the serum and CSF were 3,200 and 512, respectively. After 25 days of treatment with Prednisone and four plasma exchanges, the patient’s gait improved and the serum and CSF titers of the antibodies dropped to 200 and 64, respectively. Later, when the patient was asymptomatic, the anti-mGluR1 antibodies were not detected in serum. Patient 2—In this patient, the serum was first tested when she had severe Ataxia for almost 1 year. At that time, the titer of the anti-mGluR1 antibodies in the serum was 3,200. After 14 plasma exchanges the patient continued to have severe Ataxia and was unable to walk without support. Although the titer of anti-mGluR1 antibody in the plasma dropped to 400 after the plasma exchanges, the CSF titer remained high, an indication of ongoing intrathecal synthesis of anti-mGluR1 antibodies (Sillevis Smitt et al. 2000). In terms of choosing the right treatment, these important findings show that when there is a ‘stormy’ and continuous intrathecal synthesis of autoimmune antibodies, treating the patient with plasmapheresis may be somewhat useless, since while this mode of immunotherapy can reduce substantially the levels of antibodies in the plasma, it seems to be sometimes unable to lower effectively enough the levels of the autoimmune antibodies in the patient’s brain, and it is the latter that cause the neurological damage.
Study 2: Coesmans et al. found that in vitro application of IgG purified from the serum of patients with Paraneoplastic Cerebellar Ataxia to cerebellar slices of mice acutely reduced the basal activity of Purkinje cells (Coesmans et al. 2003). In addition, application of such IgG to the flocculus of mice evoked in vivo acute disturbances in the performance of their compensatory eye movements. Moreover, the anti-mGluR1 antibodies blocked the induction of long-term depression in cultured mouse Purkinje cells, whereas the cerebellar motor learning behavior of the patients was affected in that they showed impaired adaptation of their saccadic eye movements. Finally, postmortem analysis of the cerebellum of a Paraneoplastic Cerebellar Ataxia patient showed that the number of Purkinje cells was significantly reduced by approximately two-thirds compared with three controls. Coesmans et al. (2003) concluded that anti-mGluR1 antibodies are present in some patients with Paraneoplastic Cerebellar Ataxia, and that such antibodies can cause cerebellar motor coordination deficits by a combination of rapid effects on both acute and plastic responses of Purkinje cells and chronic degenerative effects.
Study 3: Marignier et al. (2010) report on a third case of a subacute Cerebellar Ataxia associated with anti-mGluR1 antibodies. The 50-year-old woman was admitted for acute severe isolated static and kinetic cerebellar syndrome. Brain MRI showed diffuse abnormal hyperintensity in the whole cerebellum on fluid-attenuated inversion recovery and diffusion sequences. Results of the biological workup were negative for general inflammation, vitamin deficiency, and bacterial and viral infections. Immunohistochemical analysis of the serum and CSF of the patient demonstrated staining for Purkinje cell bodies and the molecular layer of the cerebellum. Finally, anti-mGluR1 antibodies were detected in serum and CSF of the patient by a cell-based assay. There was no evidence for underlying tumor, including Hodgkin lymphoma. Importantly, immunotherapy was found very useful for this patient, since the disease was stabilized after a course of IVIG and continuous treatment with Mycophenolate Mofetil (an immunosuppressive agent used usually with other medicines to lower the body’s natural immunity in patients who receive organ transplants) during a follow-up of 40 months (Marignier et al. 2010).
Two patients with Hodgkin lymphoma and Limbic Encephalopathy (Ophelia syndrome) were found to have anti-mGluR5 antibodies. The patient’s sera reacted with the neuropil of hippocampus and the cell surface of live hippocampal neurons
Lancaster et al. (2011) describe the finding of anti-mGluR5 antibodies in two patients with Hodgkin lymphoma and Limbic Encephalopathy (Ophelia syndrome). The symptoms of both patients were consistent with Limbic Encephalopathy: One patient had MRI findings typical of this disorder, and the other had more extensive radiologic involvement, including parietal and occipital cortex. Patient’s sera contained antibodies that predominantly reacted with the neuropil of hippocampus and the cell surface of live hippocampal neurons. Immunohistochemistry with brain tissue and cultures of rat hippocampal neurons was used to demonstrate anti-mGluR5 antibodies. Immunoprecipitation, mass spectrometry, and mGluR5-null mice served to identify the antigen. HEK293 cells that were transfected with mGluR5 or mGluR1 were used to determine immunologic cross-reactivity. Immunoprecipitation from cultured neurons and mass spectrometry demonstrated that the antigen was mGluR5—a receptor involved in processes of learning and memory. The reactivity of patient’s sera was abrogated in the brain of mGluR5-null mice, further confirming the fact that the antibodies were directed specifically against GluR5. Studies with a large number of controls, including 2 patients with Cerebellar Ataxia and anti-mGluR1 antibodies, showed that mGluR5 was only identified by sera of the 2 patients with the Ophelia syndrome, and that despite the homology of this receptor with mGluR1, each autoantigen was specific for a distinct syndrome. Based on these findings, Lancaster et al. (2011) recommended to test for anti-mGluR5 antibodies in patients with symptoms of Limbic Encephalitis and Hodgkin lymphoma (Ophelia syndrome), and stated that recognition of this disorder is especially important because it can affect young individuals and is reversible.
Ophelia syndrome with anti-mGluR5 antibodies in the CSF is also discussed in (Mat et al. 2013).
Summary, recommendations, challenges and prospects
Summary
Collectively, the family of anti-glutamate receptor autoimmune antibodies seem to be the most widespread, potent, dangerous and interesting anti-brain autoimmune antibodies discovered up to now. This impression stems from taking together the presence of various types of anti-glutamate receptor antibodies in a kaleidoscope of human neurological and autoimmune diseases, their high levels in the CNS due to intrathecal production, their multiple pathological effects in the brain, and the unique and diverse mechanisms of action by which they can affect glutamate receptors, signaling and effects and subsequently impair neuronal signaling and induce brain damage.
Figure 1 shows schematically which type of anti-glutamate receptor antibodies was found thus far in each neurological and/or autoimmune diseases. As can be seen in this figure, and as discussed throughout this review, a large body of evidences that accumulated in the last ~20 years (and that keeps growing) show collectively that anti-glutamate receptor antibodies of several types, directed against specific subunits of Ionotropic glutamate receptors: AMPA-GluR3, NMDA-NR1, or NMDA-NR2, or against specific members of Metabotropic glutamate receptors: mGluR1 or mGluR5, are present in the serum and CSF of subpopulations of patients with a kaleidoscope of neurological and/or psychiatric and/or autoimmune diseases. Among these diseases are the following: Epilepsy, Encephalitis of few types, Cerebellar Ataxia of few types, Lupus and Neuropsychiatric Lupus, Neuropsychiatric Sjogren’s syndrome, Schizophrenia, Mania and Stroke. On top of all these, it may well be that anti-glutamate receptor antibodies (of the same types as those found thus far or others) will be found in the future in additional neurological and/or psychiatric and/or autoimmune diseases not associated thus far with these antibodies.
As to the site of production of the anti-glutamate receptor antibodies: there is now clear cut evidence for a substantial ongoing intrathecal production of several types of autoimmune anti-glutamate receptor antibodies in patients with several neurological diseases. Due to this, the anti-glutamate receptor antibodies are sometimes even present in much higher levels in the brain than in the serum.
As to the detrimental effects induced by the anti-glutamate receptor antibodies: once these antibodies are present in the brain, due to either intrathecal production or entry into the CNS via a leaky/damaged BBB, their neuropathogenic potential could be unveiled. Then, they may impair the normal brain function and induce substantial damage in several brain regions, and they can do so by several ways. Collectively, the evidences revealed thus far (which are discussed in this review and summarized in Figs. 2, 3, 4, 5) show that in vitro, as well as in vivo in animal models, the various types of anti-glutamate receptor antibodies can induce all the following effects: bind glutamate receptors in several brain regions, activate glutamate receptors in an abnormal manner, kill neurons by ‘Excitotoxicity’ and/or by complement fixation and/or by induction of apoptosis, reduce the membranal expression of glutamate receptors in neurons, block certain glutamate-induced effects, increase glutamate’s concentration in the extracellular space, impair synaptic regulation of glutamate, activate endothelial cells in the BBB, cause brain damage in several brain regions, and induce or facilitate in vivo: epileptic seizures, Ataxia, and additional behavior/motor/cognitive abnormalities.
The main types of anti-glutamate receptor antibodies found thus far in patients with neurological and autoimmune diseases, and their main features and detrimental effects on cells, processes and functions of the CNS (as summarized in Figs. 1, 2, 3, 4, 5) are the following (as already summarized in the abstract of this review):
-
1.
Anti-AMPA-GluR3 B antibodies were found thus far in ~30 to 35 % of patients with different types of Epilepsy. When such anti-glutamate receptor antibodies, or other types of autoimmune antibodies directed against brain proteins/antigens’ are present in epileptic patients and can induce or contribute to the seizures and to the accompanying neurological and psychiatric/behavioral problems, the Epilepsy is called ‘Autoimmune Epilepsy’ [a term first coined by the author of this review in a Nature Immunology paper (Levite 2002)].
In some Epilepsy patients, the anti-AMPA-GluR3B antibodies associate significantly with psychiatric/cognitive/behavior abnormalities (Goldberg-Stern et al. 2014). In vitro and/or in vivo in animal models, the anti-AMPA-GluR3B antibodies can be very pathogenic since by themselves they can: activate glutamate/AMPA receptors, kill neurons by induction of ‘Excitotoxicity’ and/or apoptosis, and/or activation of complement, cause multiple brain damage, aggravate chemoconvulsant-induced seizures and also induce behavioral impairments. Some Epilepsy patients that have high levels of anti-AMPA-GluR3B antibodies respond well to immunotherapy and express reduced seizures and overall improved neurological functions. Yet, the improvement is sometimes partial and requires continuation of the treatment, and also inclusion of treatment that can reduce the levels or suppress the anti-AMPA-GluR3B antibodies in the brain, not only in the circulation.
-
2.
Anti-NMDA NR 1 antibodies are present in patients with ‘Anti-NMDA receptor Encephalitis’ and characterize this autoimmune neurological disease. In vitro and/or in vivo in humans and animal models, the anti-NMDA NR1 antibodies are very pathogenic since they can cause pronounced decrease of surface NMDA receptors in hippocampal neurons, and also reduce their cluster density and synaptic localization, by crosslinking and internalization of these receptors. Such changes can impair NMDA receptor-mediated currents and functions and can lead to various neuronal/behavior/cognitive/psychiatric abnormalities. Anti-NMDA-NR1 antibodies are often present in the CSF, and even in much higher levels than in the serum, due to their intrathecal production. Many of the patients with ‘Anti-NMDA receptor Encephalitis’ respond well to several modes of immunotherapy.
-
3.
Anti-NMDA-NR 2A/B antibodies are found thus far in many patients with SLE with or without neuropsychiatric impairments. The exact percentage of SLE patients having anti-NMDA-NR2A/B antibodies varies in different studies from 35 % (Hanly et al. 2006), to 33 % (Lapteva et al. 2006), 31 % (Husebye et al. 2005), 26 % (Harrison et al. 2006), 19 % (Omdal et al. 2005) or 14 % (Kozora et al. 2010). And in one study, the anti-NMDA-NR2A/B antibodies were found in 81 % of patients with diffuse ‘Neuropshychiatric SLE’, and in 44 % of patients with focal ‘Neuropshychiatric SLE’ (Arinuma et al. 2008). Anti-NMDA-NR2A/B antibodies are also present in subpopulations of patients with either of the following diseases: Epilepsy, Encephalitis of different types, Schizophrenia, Mania, Stroke and Sjorgen syndrome. Some of the anti-NMDA-NR2A/B antibodies cross-react with dsDNA and some do not. Some anti-NMDA-NR2A/B antibodies associate with neuropsychiatric or cognitive impairments in lupus patients and some do not. The anti-NMDA-NR2A/B antibodies can be very pathogenic in the brain, since they kill neurons and cause brain damage, activate endothelial cells in the BBB, and also induce behavioral/cognitive impairments. Yet, the concentration of these anti-NMDA-NR2A/B antibodies seems to determine if they have positive or negative effects on the activity of glutamate receptors and on the survival of neurons (Faust et al. 2010). Thus, at low concentration, the anti-NMDA-NR2A/B antibodies were found to be positive modulators of receptor function and increase the size of NMDA receptor-mediated excitatory postsynaptic potentials, whereas at high concentration they are pathogenic as they promote ‘Excitotoxcity’ through enhanced mitochondrial permeability transition (Faust et al. 2010). Also, in animal models, the manner by which the BBB was disrupted determined the brain region that was affected by the anti-NMDA-NR2A/B antibodies, and also the neurobehavioral impairment that followed (Kowal et al. 2004; Huerta et al. 2006).
-
4.
Anti-mGluR 1 antibodies were found thus far in very few patients with Paraneoplastic Cerebellar Ataxia, in which they were produced intrathecally, and therefore present in much higher levels in the CSF than in the serum. These anti-mGluR1 antibodies can be very pathogenic since they can reduce the basal activity and block the induction of long-term depression of Purkinje cells, and cause cerebellar motor coordination deficits by a combination of rapid effects on both the acute and the plastic responses of Purkinje cells, and also by chronic degenerative effects. In animal models, the anti-mGluR1 antibodies were also shown to be very pathogenic in the brain, since 30 min after the injection of patient’s purified IgGs that contained anti-mGluR1 antibodies into the subarachnoid space of normal mice, the mice became increasingly ataxic, were unable to walk straight, and had additional signs of cerebellar dysfunction (Sillevis Smitt et al. 2000).
-
5.
Anti-mGluR5 antibodies were found thus far in very few patients with Hodgkin lymphoma and Limbic Encephalopathy (Ophelia syndrome). The sera of these patients, that contained anti-GluR5 antibodies, reacted with the neuropil of hippocampus and cell surface of live rat hippocampal neurons. Immunoprecipitation from cultured neurons and mass spectrometry demonstrated that the antigen was mGluR5. Anti-GluR5 antibodies are also present in the CSF of some patients.
Recommendations: be aware, diagnose, study and treat
Based on all the evidences discussed in this review, my own humble recommendations are the following:
-
1.
Be aware: Neurologists, Psychiatrists and Psychologists should be aware of the fact that autoimmune processes mediated by several types of anti-glutamate receptor antibodies turn out to be much more common in the brains of various patients with neurological diseases then ever realized before. Moreover, the autoimmune anti-glutamate receptor antibodies are sometimes present in very high levels in the brain due to their intrathecal production, and therefore can impair glutamate receptor’s expression, signaling and function in the brain. As such, the family of anti-glutamate receptor antibodies can contribute to a variety of neurological/psychiatric/cognitive/motor/behavioral problems, and play an active role in certain neurological diseases.
-
2.
Diagnose: Based on all the solid and rich body of evidences regarding the prevalence and many detrimental effects in the CNS of the various types of anti-glutamate receptor antibodies, it seems advantageous to test routinely all patients with neurological and psychiatric diseases for these autoimmune antibodies, and mainly for the five types discussed in this review: the anti-AMPA-GluR3B antibodies, anti-NMDA-NR1 antibodies, anti-NMDA-NR2A/B antibodies, anti-mGluR1 antibodies and anti-mGluR5 antibodies. Such tests are especially recommended in ‘mysterious’ cases when the etiology of the neurological problems is unknown, when the symptoms are confusing, when the diagnosis is unclear, when the response to ‘classical therapy’ is poor, and when the patient is suffering for a prolonged period of time and loses hope. Furthermore, testing for anti-glutamate receptor antibodies, and if positive, treating the patient with immunotherapy (advised below under “Treat”) should certainly be done before any brain surgery or other drastic, dangerous and irreversible procedures. Testing for the anti-glutamate receptor antibodies in the CSF is a must! Testing for these antibodies only in the serum is not enough and may even be very misleading and give false negative results, due to the fact that in many patients the autoimmune anti-glutamate receptor antibodies seem to be produced primarily, and maybe even only, in the CNS.
The diagnosis of the all the above-mentioned types of anti-glutamate receptor antibodies can be done by several methods, as described in part 3.4.
In addition to anti-glutamate receptor antibodies, other pathogenic autoimmune antibodies may be present in the brains of patients with various neurological diseases. Accordingly, in cases of severe and enigmatic neurological diseases, and especially when the patient does not respond well to conventional therapy, broad diagnostic tests should be done on the patient’s serum and CSF for as many types of autoimmune antibodies as possible.
-
3.
Test: Once anti-glutamate receptor antibodies of any type are found in a given patient, such antibodies can be studied and tested by many different ways and methods for their in vitro effects, and also for their in vivo effects in animal models, as described in several parts of the review. Such tests are not a must, since clinicians can move on to immunotherapy without them, but they can provide direct proofs for the pathogenicity of the specific antibodies detected in that patient.
In addition, once anti-glutamate receptor antibodies are detected in a given patient, I would recommend performing a board test for as many types of infectious organisms as possible on the serum and CSF of the patient, for revealing a possible infectious etiology. And of course, if a certain infectious organism is detected, a proper treatment should be given to eradicate it, in parallel to the immunotherapy given for the autoimmunity.
Finally, once anti-glutamate receptor antibodies are detected in a given patient, I would recommend testing the serum of the patient’s parents, brothers and sisters for such autoimmune antibodies. And if the patient is found positive also for a certain infectious organism, I would test his family members also for that.
-
4.
Treat: Unfortunately, when it comes to treating autoimmune diseases, be them as they may, medicine is still in a relatively poor state, since there are still no specific therapeutic means to specifically remove/eradicate/arrest/silence only a specific type of autoimmune antibodies, or a specific clone of plasma cells that produce and secrete these autoimmune antibodies, or a specific clone of autoimmune T cells. Due to that, treatment of autoimmune diseases is, in the best and minority of cases, based on life time compensation for the protein/s that are in insufficient levels due to autoimmune attack and destruction, and in most of the other cases based on non-specific immunotherapy of several types. As a whole, the non-specific immunotherapies either remove non-specifically from the body many types of antibodies (regardless of whether they are autoimmune or not), or suppress non-specifically many types of immune responses (both the beneficial immune responses and the detrimental autoimmune responses). Such therapies are often very effective and lead to substantial improvement, but they are nevertheless not free of side effects.
On these grounds, treatment of autoimmune diseases and neuropathological processes caused by anti-glutamate receptor antibodies can unfortunately still not rely on any specific therapeutic means to get rid only of these autoimmune antibodies, while sparing the many other types of normal (i.e. non autoimmune) and needed antibodies. Therefore, one has to settle here, as in most autoimmune diseases, with the available non-specific immunotherapeutic tools, and use them in a smart, careful and patient-tailored manner, for as long as they are effective and safe for the specific patient that receives the immunotherapy.
In practice, patients with neurological diseases/complications found to have high levels of any type of anti-glutamate receptor antibodies should better receive some type of immunotherapy chosen from the currently approved and used ones. ‘First-line immunotherapy’ currently includes mainly: Steroids, IVIG, plasmapheresis and immunoabsorption, while ‘second-line immunotherapy’ currently includes mainly Rituximab and Cyclophosphamide. Such types of immunotherapy may lead to very significant improvement, especially when given early, and should be continued or given repeatedly for as long as the patient needs them. And in parallel, the levels of the anti-glutamate receptor antibodies should be measured before, several times during, and then after the immunotherapy, for obtaining important direct proofs for the association between them and the neurological condition.
The exact type of immunotherapy and of the time period of the treatment should: (a) be tailored to each patient based on all his symptoms, background, and overall condition; (b) better be decided by the treating neurologist/s in consultation with experts in immunology and autoimmunity; (c) take into consideration the accumulated positive experience and published reports on successful immunotherapy already given to neurological patients that were found to have anti-glutamate receptor antibodies in their serum and/or CSF.
Finally, and as already mentioned earlier in this review: it is of primary importance to make sure that the chosen immunotherapy is effective ‘in the site of crime’, i.e. in the brain, and that it is able to reduce/silence/block the autoimmune antibodies that are produced intrathecally and active in the brain. Immunotherapy that has only peripheral effects and cannot ‘deal’ with intrathecal production of anti-glutamate receptor antibodies may be useless, misleading and even harmful to the patient.
Challenges and prospects: develop, study and design
The multiple pathological effects in the brain caused by the various types of anti-glutamate receptor antibodies, the unique mechanisms by which they exert these effects, which do not resemble the mechanisms of action of any other autoimmune antibodies known so far, and their prevalence in so many neurological diseases/complications set up now new challenges for experts of many disciplines among them: neurobiologists/neurologists, immunologists, experts in autoimmunity, experts in designing new animal models of human diseases, experts in immunotherapy, experts in drug design, and experts in drug delivery to the brain across the BBB. All these experts should better work in coordination to meet the following challenges:
-
1.
Develop new additional animal models suitable for studying the pathogenic activity in the brain of each type of anti-glutamate receptor antibodies found thus far in patients and proven to be pathogenic to the CNS: anti-AMPA-GluR3B antibodies, anti-NMDA-NR1 antibodies, anti-NMDA-NR2 antibodies, anti-mGluR1 antibodies and anti-mGluR5 antibodies. The reason for this need is that the commonly studied animal models of various neurological and psychiatric diseases/complications completely ignore the possibility that autoimmune anti-glutamate receptor antibodies may in fact be the primary pathological factor responsible for the onset and/or for the deterioration of the brain damage and neurological impairments.
-
2.
Study systematically in patients the association between anti-glutamate receptor autoimmune antibodies and a preceding or ongoing infection that could be caused by a large panel of infectious organisms. Be aware that the preceding infection could be in any part of the body, and that it could be caused also in the context of vaccination or food poisoning.
-
3.
Study systematically in patients the association between the autoimmune anti-glutamate receptor antibodies and other autoimmune diseases that the patient may suffer from.
-
4.
Study in animal models whether an infection with certain viruses/bacteria can lead to the development of anti-glutamate receptor antibodies.
-
5.
Study systematically in patients the association between anti-glutamate receptor antibodies and immunogenetic factors, starting with an analysis of the HLA haplotypes that could contribute to increase the susceptibility to develop this specific autoimmunity.
-
6.
Try to design novel types of immunotherapy that can effectively eliminate or silence in the CNS, each type of anti-glutamate receptor antibodies discover so far.
The perfect wishful drug for treating neurological diseases that are caused or mediated by anti-glutamate receptor antibodies, should be able to do the following:
-
a.
Cross the BBB and be effective inside the CNS;
-
b.
Block the binding of anti-glutamate receptor antibodies to the respective glutamate receptors expressed in neurons and in several other cells;
-
c.
Block the activation of glutamate receptors induced by the anti-glutamate receptor antibodies;
-
d.
Block the detrimental effects of the anti-glutamate receptor antibodies on the levels of glutamate receptors expressed on the cell surface of neurons, and on glutamate’s concentrations, signaling and effects;
-
e.
Block the killing of neurons and glia induced by the anti-glutamate receptor antibodies;
-
f.
Block the brain damage caused by the anti-glutamate receptor antibodies in various brain regions;
-
g.
Block the behavioral/cognitive/psychiatric/motor impairments caused/mediated by the anti-glutamate receptor antibodies.
In parallel to all the above, the desired drug/s against anti-glutamate receptor antibodies should of course not impair normal glutamate-mediated signaling, not cause severe side effects, and not be immunogenic (to avoid a humoral/cellular immune response against the drug itself).
Clearly, when it comes to anti-glutamate receptor antibodies, there is still lot to be studied, unveiled. Yet, what we have learned by now about these autoimmune antibodies is so exciting, novel, unique and important, that it makes all our future efforts worthy and essential.
References
Andrews PI, McNamara JO (1996) Rasmussen’s encephalitis: an autoimmune disorder? Curr Opin Neurobiol 6:673–678
Andrews PI, Dichter MA, Berkovic SF, Newton MR, McNamara JO (1996) Plasmapheresis in Rasmussen’s encephalitis. Neurology 46:242–246
Andrews PI, McNamara JO, Lewis DV (1997) Clinical and electroencephalographic correlates in Rasmussen’s encephalitis. Epilepsia 38:189–194
Ankarcrona M, Dypbukt JM, Bonfoco E, Zhivotovsky B, Orrenius S, Lipton SA, Nicotera P (1995) Glutamate-induced neuronal death: a succession of necrosis or apoptosis depending on mitochondrial function. Neuron 15:961–973
Antozzi C, Granata T, Aurisano N, Zardini G, Confalonieri P, Airaghi G, Mantegazza R, Spreafico R (1998) Long-term selective IgG immuno-adsorption improves Rasmussen’s encephalitis. Neurology 51:302–305
Appenzeller S (2011) NR2 antibodies in neuropsychiatric systemic lupus erythematosus. Rheumatology (Oxford) 50(9):1540–1541
Arinuma Y, Yanagida T, Hirohata S (2008) Association of cerebrospinal fluid anti-NR2 glutamate receptor antibodies with diffuse neuropsychiatric systemic lupus erythematosus. Arthritis Rheum 58(4):1130–1135
Asano NM, Coriolano MD, Asano BJ, Lins OG (2013) Psychiatric comorbidities in patients with systemic lupus erythematosus: a systematic review of the last 10 years. Rev Bras Rheumatol 53:431–437
Balosso S, Ravizza T, Pierucci M, Calcagno E, Invernizzi R, Di Giovanni G, Esposito E, Vezzani A (2009) Molecular and functional interactions between tumor necrosis factor-alpha receptors and the glutamatergic system in the mouse hippocampus: implications for seizure susceptibility. Neuroscience 161:293–300
Baltagi SA, Shoykhet M, Felmet K, Kochanek PM, Bell MJ (2010) Neurological sequelae of 2009 influenza A (H1N1) in children: a case series observed during a pandemic. Pediatr Crit Care Med 11:179–184
Baranzini SE, et al (2002) Analysis of antibody gene rearrangement, usage, and specificity in chronic focal encephalitis. Neurology 58(5):709–716
Basile AS, Koustova E, Ioan P, Rizzoli S, Rogawski MA, Usherwood PN (2001) IgG isolated from LP-BM5 infected mouse brain activates ionotropic glutamate receptors. Neurobiol Dis 8:1069–1081
Beneyto M, Kristiansen LV, Oni-Orisan A, McCullumsmith RE, Meador-Woodruff JH (2007) Abnormal glutamate receptor expression in the medial temporal lobe in schizophrenia and mood disorders. Neuropsychopharmacology 32:1888–1902
Berg AT, Langfitt JT, Testa FM, Levy SR, DiMario F, Westerveld M, Kulas J (2008) Global cognitive function in children with epilepsy: a community-based study. Epilepsia 49:608–614
Bernasconi P, Cipelletti B, Passerini L, Granata T, Antozzi C, Mantegazza R, Spreafico R (2002) Similar binding to glutamate receptors by Rasmussen and partial epilepsy patient’s sera. Neurology 59:1998–2001
Bien CG, Vincent A, Barnett MH, Becker AJ, Blumcke I, Graus F, Jellinger KA, Reuss DE, Ribalta T, Schlegel J, Sutton I, Lassmann H, Bauer J (2012) Immunopathology of autoantibody-associated encephalitides: clues for pathogenesis. Brain 135:1622–1638
Binnie CD (1993) Significance and management of transitory cognitive impairment due to subclinical EEG discharges in children. Brain Dev 15:23–30
Bonsi P, Cuomo D, De Persis C, Centonze D, Bernardi G, Calabresi P, Pisani A (2005) Modulatory action of metabotropic glutamate receptor (mGluR) 5 on mGluR1 function in striatal cholinergic interneurons. Neuropharmacology 49(Suppl 1):104–113
Borchers AT, Aoki CA, Naguwa SM, Keen CL, Shoenfeld Y, Gershwin ME (2005) Neuropsychiatric features of systemic lupus erythematosus. Autoimmun Rev 4:329–344
Cahn-Weiner DA, Wittenberg D, McDonald C (2009) Everyday cognition in temporal lobe and frontal lobe epilepsy. Epileptic Disord 11:222–227
Carlson NG, Gahring LC, Twyman RE, Rogers SW (1997) Identification of amino acids in the glutamate receptor, GluR3, important for antibody-binding and receptor-specific activation. J Biol Chem 272:11295–11301
Cheung MC, Chan AS, Chan YL, Lam JM, Lam W (2006) Effects of illness duration on memory processing of patients with temporal lobe epilepsy. Epilepsia 47:1320–1328
Chu Z, Hablitz JJ (2000) Quisqualate induces an inward current via mGluR activation in neocortical pyramidal neurons. Brain Res 879:88–92
Coesmans M, Smitt PA, Linden DJ, Shigemoto R, Hirano T, Yamakawa Y, van Alphen AM, Luo C, van der Geest JN, Kros JM, Gaillard CA, Frens MA, de Zeeuw CI (2003) Mechanisms underlying cerebellar motor deficits due to mGluR1-autoantibodies. Ann Neurol 53:325–336
Cohen-Kashi Malina K, Ganor Y, Levite M, Teichberg VI (2006) Autoantibodies against an extracellular peptide of the GluR3 subtype of AMPA receptors activate both homomeric and heteromeric AMPA receptor channels. Neurochem Res 31:1181–1190
Collingridge GL, Olsen RW, Peters J, Spedding M (2009) A nomenclature for ligand-gated ion channels. Neuropharmacology 56:2–5
Cusick MF, Libbey JE, Fujinami RS (2012) Molecular mimicry as a mechanism of autoimmune disease. Clin Rev Allergy Immunol 42:102–111
Dalmau J, Tuzun E, Wu HY, Masjuan J, Rossi JE, Voloschin A, Baehring JM, Shimazaki H, Koide R, King D, Mason W, Sansing LH, Dichter MA, Rosenfeld MR, Lynch DR (2007) Paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma. Ann Neurol 61:25–36
Dalmau J, Gleichman AJ, Hughes EG, Rossi JE, Peng X, Lai M, Dessain SK, Rosenfeld MR, Balice-Gordon R, Lynch DR (2008) Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies. Lancet Neurol 7:1091–1098
Dalmau J, Lancaster E, Martinez-Hernandez E, Rosenfeld MR, Balice-Gordon R (2011) Clinical experience and laboratory investigations in patients with anti-NMDAR encephalitis. Lancet Neurol 10:63–74
Dambinova SA, Khounteev GA, Izykenova GA, Zavolokov IG, Ilyukhina AY, Skoromets AA (2003) Blood test detecting autoantibodies to N-methyl-d-aspartate neuroreceptors for evaluation of patients with transient ischemic attack and stroke. Clin Chem 49:1752–1762
Dambinova SA, Bettermann K, Glynn T, Tews M, Olson D, Weissman JD, Sowell RL (2012) Diagnostic potential of the NMDA receptor peptide assay for acute ischemic stroke. PLoS ONE 7:e42362
Das S, Sasaki YF, Rothe T, Premkumar LS, Takasu M, Crandall JE, Dikkes P, Conner DA, Rayudu PV, Cheung W, Chen HS, Lipton SA, Nakanishi N (1998) Increased NMDA current and spine density in mice lacking the NMDA receptor subunit NR3A. Nature 393:377–381
de Graaff E, Maat P, Hulsenboom E, van den Berg R, van den Bent M, Demmers J, Lugtenburg PJ, Hoogenraad CC, Sillevis Smitt P (2012) Identification of delta/notch-like epidermal growth factor-related receptor as the Tr antigen in paraneoplastic cerebellar degeneration. Ann Neurol 71:815–824
DeGiorgio LA, Konstantinov KN, Lee SC, Hardin JA, Volpe BT, Diamond B (2001) A subset of lupus anti-DNA antibodies cross-reacts with the NR2 glutamate receptor in systemic lupus erythematosus. Nat Med 7(11):1189–1193
Dickerson F, Stallings C, Vaughan C, Origoni A, Khushalani S, Yolken R (2012) Antibodies to the glutamate receptor in mania. Bipolar Disord 14:547–553
Dingledine R, Borges K, Bowie D, Traynelis SF (1999) The glutamate receptor ion channels. Pharmacol Rev 51:7–61
Dracheva S, McGurk SR, Haroutunian V (2005) mRNA expression of AMPA receptors and AMPA receptor binding proteins in the cerebral cortex of elderly schizophrenics. J Neurosci Res 79:868–878
Elger CE, Helmstaedter C, Kurthen M (2004) Chronic epilepsy and cognition. Lancet Neurol 3:663–672
Endoh T (2004) Characterization of modulatory effects of postsynaptic metabotropic glutamate receptors on calcium currents in rat nucleus tractus solitarius. Brain Res 1024:212–224
Falsafi SK, Ghafari M, Pollak A, Hoger H, Lubec G (2012) Hippocampal AMPA-type receptor complexes containing GluR3 and GluR4 are paralleling training in the multiple T-Maze. Neurochem Int 60:425–430
Fanouriakis A, Boumpas DT, Bertsias GK (2013) Pathogenesis and treatment of CNS lupus. Curr Opin Rheumatol 25:577–583
Fastenau PS, Johnson CS, Perkins SM, Byars AW, deGrauw TJ, Austin JK, Dunn DW (2009) Neuropsychological status at seizure onset in children: risk factors for early cognitive deficits. Neurology 73:526–534
Faust TW, Chang EH, Kowal C, Berlin R, Gazaryan IG, Bertini E, Zhang J, Sanchez-Guerrero J, Fragoso-Loyo HE, Volpe BT, Diamond B, Huerta PT (2010) Neurotoxic lupus autoantibodies alter brain function through two distinct mechanisms. Proc Natl Acad Sci USA 107(43):18569–18574
Feichtinger M, Wiendl H, Korner E, Holl A, Gruber L, Fazekas F, Schrottner O, Eder H, Ott E (2006) No effect of immunomodulatory therapy in focal epilepsy with positive glutamate receptor type 3-antibodies. Seizure 15(5):350–354
Finke C, Kopp UA, Pruss H, Dalmau J, Wandinger KP, Ploner CJ (2012) Cognitive deficits following anti-NMDA receptor encephalitis. J Neurol Neurosurg Psychiatry 83:195–198
Florance NR, Davis RL, Lam C, Szperka C, Zhou L, Ahmad S, Campen CJ, Moss H, Peter N, Gleichman AJ, Glaser CA, Lynch DR, Rosenfeld MR, Dalmau J (2009) Anti-N-methyl-d-aspartate receptor (NMDAR) encephalitis in children and adolescents. Ann Neurol 66:11–18
Frassoni C, Spreafico R, Franceschetti S, Aurisano N, Bernasconi P, Garbelli R, Antozzi C, Taverna S, Granata T, Mantegazza R (2001) Labeling of rat neurons by anti-GluR3 IgG from patients with Rasmussen encephalitis. Neurology 57(2):324–327
Frechette ES, Zhou L, Galetta SL, Chen L, Dalmau J (2011) Prolonged follow-up and CSF antibody titers in a patient with anti-NMDA receptor encephalitis. Neurology 76:S64–S66
Gable MS, Gavali S, Radner A, Tilley DH, Lee B, Dyner L, Collins A, Dengel A, Dalmau J, Glaser CA (2009) Anti-NMDA receptor encephalitis: report of ten cases and comparison with viral encephalitis. Eur J Clin Microbiol Infect Dis 28:1421–1429
Gahring LC, Rogers SW (2002) Autoimmunity to glutamate receptors in the central nervous system. Crit Rev Immunol 22:295–316
Gahring LC, Carlson NG, Rogers SW (1998) Antibodies prepared to neuronal glutamate receptor subunit3 bind IFNalpha-receptors: implications for an autoimmune process. Autoimmunity 28:243–248
Ganor Y, Levite M (2012) Glutamate in the immune system: glutamate receptors in immune cells, potent effects, endogenous production and involvement in disease. In: Levite M (ed) Nerve-Driven immunity: Neurotransmitters and Neuropeptides in the Immune System. Springer, Vienna, pp 121–161
Ganor Y, Levite M (2014) The Neurotransmitter Glutamate and human T cells: Glutamate receptors and glutamate-induced direct and potent effects on normal human T cells, cancerous human leukemia and lymphoma T cells, and autoimmune human T cells. J Neural Transm (in press, Abstract available online)
Ganor Y, Besser M, Ben-Zakay N, Unger T, Levite M (2003) Human T cells express a functional ionotropic glutamate receptor GluR3, and glutamate by itself triggers integrin-mediated adhesion to laminin and fibronectin and chemotactic migration. J Immunol 170:4362–4372
Ganor Y, Goldberg-Stern H, Amrom D, Lerman-Sagie T, Teichberg VI, Pelled D, Futerman AH, Zeev BB, Freilinger M, Verheulpen D, Van Bogaert P, Levite M (2004) Autoimmune Epilepsy: some epilepsy patients harbor autoantibodies to glutamate receptors and dsDNA on both sides of the blood-brain barrier, which may kill neurons and decrease in brain fluids after hemispherotomy. Clin Dev Immunol 11:241–252
Ganor Y, Freilinger M, Dulac O, Levite M (2005a) Monozygotic twins discordant for epilepsy differ in the levels of potentially pathogenic autoantibodies and cytokines. Autoimmunity 38:139–150
Ganor Y, Golgberg-stern H, Lerman-Sagie T, Teichberg V, Levite M (2005b) Autoimmune Epilepsy: Distinct subpopulation of epilepsy patients harbor serum autoantibodies to either glutamate/AMPA receptor GluR3, glutamate/NMDA receptor subunit NR2A or double-stranded DNA. Epilepsy Res 65(1–2):11–22
Ganor Y, Gottlieb M, Eilam R, Otmy H, Teichberg V, Levite M (2005c) Immunization with the glutamate receptor derived peptide GluR3B induced neuronal death and reactive gliosis, but confer partial protection from pentylenetetrazole-induced seizures. Exp Neurol 195(1):92–102
Ganor Y, Goldberg-Stern H, Blank M, Shoenfeld Y, Dobrynina LA, Kalashnikova L, Levite M (2005d) Antibodies to glutamate receptor subtype 3 (GluR3) are found in some patients suffering from epilepsy as the main disease, but not in patients whose epilepsy accompanies antiphospholipid syndrome or Sneddon’s syndrome. Autoimmunity 38:417–424
Ganor Y, Teichberg VI, Levite M (2007) TCR activation eliminates glutamate receptor GluR3 from the cell surface of normal human T cells, via an autocrine/paracrine granzyme B-mediated proteolytic cleavage. J Immunol 178:683–692
Ganor Y, Grinberg I, Reis A, Cooper I, Goldstein RS, Levite M (2009) Human T-leukemia and T-lymphoma express glutamate receptor AMPA GluR3, and the neurotransmitter glutamate elevates the cancer-related matrix-metalloproteinases inducer CD147/EMMPRIN, MMP-9 secretion and engraftment of T-leukemia in vivo. Leuk Lymphoma 50:985–997
Ganor Y, Goldberg-Stern H, Cohen R, Teichberg V, Levite M (2014) Glutamate receptor antibodies directed against AMPA receptors subunit 3 peptide B (GluR3B) can be produced in DBA/2J mice, lower seizure threshold and induce abnormal behavior. Psychoneuroendocrinology 42:106–117
Gao HX, Sanders E, Tieng AT, Putterman C (2010) Sex and autoantibody titers determine the development of neuropsychiatric manifestations in lupus-prone mice. J Neuroimmunol 229(1–2):112–122
Goldberg-Stern H, Ganor Y, Cohen R, Pollak L, Teichberg VI, Levite M (2014) Glutamate receptor antibodies directed against AMPA receptors subunit 3 peptide B (GluR3B) associate with some cognitive/psychiatric/behavioral abnormalities in epilepsy patients. Psychoneuroendocrinology 40:221–231
Gono T, Kawaguchi Y, Kaneko H, Nishimura K, Hanaoka M, Kataoka S, Okamoto Y, Katsumata Y, Yamanaka H (2011) Anti-NR2A antibody as a predictor for neuropsychiatric systemic lupus erythematosus. Rheumatology (Oxford) 50(9):1578–1585
Granata T, Fusco L, Gobbi G, Freri E, Ragona F, Broggi G, Mantegazza R, Giordano L, Villani F, Capovilla G, Vigevano F, Bernardina BD, Spreafico R, Antozzi C (2003) Experience with immunomodulatory treatments in Rasmussen’s encephalitis. Neurology 61:1807–1810
Graus F, Dalmau J, Valldeoriola F, Ferrer I, Rene R, Marin C, Vecht CJ, Arbizu T, Targa C, Moll JW (1997) Immunological characterization of a neuronal antibody (anti-Tr) associated with paraneoplastic cerebellar degeneration and Hodgkin’s disease. J Neuroimmunol 74:55–61
Hahn BH (1993) An overview of the pathogenesis of systemic lupus erythematosus. In: Wallace DJ, Hahn BH (eds) Dubois’ lupus erythematosus. Williams and Wilkins, Philadelphia, pp 69–76
Hahn BH (1998) Antibodies to DNA. N Engl J Med 338:1359–1368
Hammack J, Kotanides H, Rosenblum MK, Posner JB (1992) Paraneoplastic cerebellar degeneration. II. Clinical and immunologic findings in 21 patients with Hodgkin’s disease. Neurology 42:1938–1943
Hanly JG, Robichaud J, Fisk JD (2006) Anti-NR2 glutamate receptor antibodies and cognitive function in systemic lupus erythematosus. J Rheumatol 33(8):1553–1558
Harrison MJ, Ravdin LD, Lockshin MD (2006) Relationship between serum NR2a antibodies and cognitive dysfunction in systemic lupus erythematosus. Arthritis Rheum 54(8):2515–2522
He XP, Patel M, Whitney KD, Janumpalli S, Tenner A, McNamara JO (1998) Glutamate receptor GluR3 antibodies and death of cortical cells. Neuron 20:153–163
Helmstaedter C (2002) Effects of chronic epilepsy on declarative memory systems. Prog Brain Res 135:439–453
Hermann BP, Seidenberg M, Schoenfeld J, Davies K (1997) Neuropsychological characteristics of the syndrome of mesial temporal lobe epilepsy. Arch Neurol 54:369–376
Hessen E, Lossius MI, Reinvang I, Gjerstad L (2006) Influence of major antiepileptic drugs on attention, reaction time, and speed of information processing: results from a randomized, double-blind, placebo-controlled withdrawal study of seizure-free epilepsy patients receiving monotherapy. Epilepsia 47:2038–2045
Hinoi E, Ogita K, Takeuchi Y, Ohashi H, Maruyama T, Yoneda Y (2001) Characterization with [3H]quisqualate of group I metabotropic glutamate receptor subtype in rat central and peripheral excitable tissues. Neurochem Int 38:277–285
Hofmann C, Baur MO, Schroten H (2010) Anti-NMDA receptor encephalitis after TdaP-IPV booster vaccination: cause or coincidence? J Neurol 258:500–501
Hollmann M, Heinemann S (1994) Cloned glutamate receptors. Annu Rev Neurosci 17:31–108
Holmes GL, Lenck-Santini PP (2006) Role of interictal epileptiform abnormalities in cognitive impairment. Epilepsy Behav 8:504–515
Hommet C, Sauerwein HC, De Toffol B, Lassonde M (2006) Idiopathic epileptic syndromes and cognition. Neurosci Biobehav Rev 30:85–96
Huerta PT, Kowal C, DeGiorgio LA, Volpe BT, Diamond B (2006) Immunity and behavior: antibodies alter emotion. Proc Natl Acad Sci USA 103(3):678–683
Huettner JE (2003) Kainate receptors and synaptic transmission. Prog Neurobiol 70:387–407
Hughes EG, Peng X, Gleichman AJ, Lai M, Zhou L, Tsou R, Parsons TD, Lynch DR, Dalmau J, Balice-Gordon RJ (2010) Cellular and synaptic mechanisms of anti-NMDA receptor encephalitis. J Neurosci 30:5866–5875
Husebye ES, Sthoeger ZM, Dayan M, Zinger H, Elbirt D, Levite M, Mozes E (2005) Autoantibodies to a NR2A peptide of the glutamate/NMDA receptor in sera of patients with systemic lupus erythematosus. Ann Rheum Dis 64(8):1210–1213
Iizuka T, Sakai F, Ide T, Monzen T, Yoshii S, Iigaya M, Suzuki K, Lynch DR, Suzuki N, Hata T, Dalmau J (2008) Anti-NMDA receptor encephalitis in Japan. Long-term outcome without tumor removal. Neurology 70(7):504–511
Irani SR, Vincent A (2011) NMDA receptor antibody encephalitis. Curr Neurol Neurosci Rep 11:298–304
Irani SR, Bera K, Waters P, Zuliani L, Maxwell S, Zandi MS, Friese MA, Galea I, Kullmann DM, Beeson D, Lang B, Bien CG, Vincent A (2010) N-methyl-D-aspartate antibody encephalitis: temporal progression of clinical and paraclinical observations in a predominantly non-paraneoplastic disorder of both sexes. Brain 133:1655–1667
Jokeit H, Ebner A (2002) Effects of chronic epilepsy on intellectual functions. Prog Brain Res 135:455–463
Kanner AM, Ostrovskaya A (2008a) Long-term significance of postictal psychotic episodes I. Are they predictive of bilateral ictal foci? Epilepsy Behav 12:150–153
Kanner AM, Ostrovskaya A (2008b) Long-term significance of postictal psychotic episodes II. Are they predictive of interictal psychotic episodes? Epilepsy Behav 12:154–156
Keinanen K, Wisden W, Sommer B, Werner P, Herb A, Verdoorn TA, Sakmann B, Seeburg PH (1990) A family of AMPA-selective glutamate receptors. Science 249:556–560
Kew JN, Kemp JA (2005) Ionotropic and metabotropic glutamate receptor structure and pharmacology. Psychopharmacology 179:4–29
Kleen JK, Scott RC, Holmes GL, Lenck-Santini PP (2010) Hippocampal interictal spikes disrupt cognition in rats. Ann Neurol 67:250–257
Koustova E, Sei Y, Fossom L, Wei ML, Usherwood PN, Keele NB, Rogawski MA, Basile AS (2001) LP-BM5 virus-infected mice produce activating autoantibodies to the AMPA receptor. J Clin Investig 107:737–744
Kowal C, Diamond B (2012) Aspects of CNS lupus: mouse models of anti-NMDA receptor antibody mediated reactivity. Methods Mol Biol 900:181–206
Kowal C, DeGiorgio LA, Nakaoka T, Hetherington H, Huerta PT, Diamond B, Volpe BT (2004) Cognition and immunity; antibody impairs memory. Immunity 21(2):179–188
Kowal C, Degiorgio LA, Lee JY, Edgar MA, Huerta PT, Volpe BT, Diamond B (2006) Human lupus autoantibodies against NMDA receptors mediate cognitive impairment. Proc Natl Acad Sci USA 103(52):19854–19859
Kozora E, West SG, Maier SF, Filley CM, Arciniegas DB, Brown M, Miller D, Grimm A, Zhang L (2010) Antibodies against N-methyl-D-aspartate receptors in patients with systemic lupus erythematosus without major neuropsychiatric syndromes. J Neurol Sci 295(1–2):87–91
Lancaster E, Martinez-Hernandez E, Titulaer MJ, Boulos M, Weaver S, Antoine JC, Liebers E, Kornblum C, Bien CG, Honnorat J, Wong S, Xu J, Contractor A, Balice-Gordon R, Dalmau J (2011) Antibodies to metabotropic glutamate receptor 5 in the Ophelia syndrome. Neurology 77:1698–1701
Lapteva L, Nowak M, Yarboro CH, Takada K, Roebuck-Spencer T, Weickert T, Bleiberg J, Rosenstein D, Pao M, Patronas N, Steele S, Manzano M, van der Veen JW, Lipsky PE, Marenco S, Wesley R, Volpe B, Diamond B, Illei GG (2006) Anti-N-methyl-D-aspartate receptor antibodies, cognitive dysfunction, and depression in systemic lupus erythematosus. Arthritis Rheum 54(8):2505–2514
Lauvsnes MB, Omdal R (2012) Systemic lupus erythematosus, the brain, and anti-NR2 antibodies. J Neurol 259(4):622–629
Lauvsnes MB, Maroni SS, Appenzeller S, Beyer MK, Greve OJ, Kvaloy JT, Harboe E, Goransson LG, Tjensvoll AB, Omdal R (2013) Memory dysfunction in primary Sjogren’s syndrome is associated with anti-NR2 antibodies. Arthritis Rheum 65(12):3209–3217
Leach JP, Chadwick DW, Miles JB, Hart IK (1999) Improvement in adult-onset Rasmussen’s encephalitis with long-term immunomodulatory therapy. Neurology 52:738–742
Lerma J (2006) Kainate receptor physiology. Curr Opin Pharmacol 6:89–97
Levite M (2002) Autoimmune Epilepsy. Nat Immunol 3:500
Levite M (2008) Neurotransmitters activate T-cells and elicit crucial functions via neurotransmitter receptors. Curr Opin Pharmacol 8:460–471
Levite M, Ganor Y (2008) Autoantibodies to glutamate receptors can damage the brain in Epilepsy, Systemic Lupus Erythematosus and Encephalitis. Expert Rev Neurother 8:1141–1160
Levite M, Hart IK (2002) Immunotherapy for Epilepsy. Expert Rev Neurother 2:804–819
Levite M, Hermelin A (1999) Autoimmunity to the glutamate receptor in mice - a model for Rasmussen’s encephalitis? J Autoimmun 13:73–82
Levite M, Fleidervish IA, Schwarz A, Pelled D, Futerman AH (1999) Autoantibodies to the glutamate receptor kill neurons via activation of the receptor ion channel. J Autoimmun 13:61–72
Li F, Tsien JZ (2009) Memory and the NMDA receptors. N Engl J Med 361:302–303
Li Y, Uccelli A, Laxer KD, Jeong MC, Vinters HV, Tourtellotte WW, Hauser SL, Oksenberg JR (1997) Local-clonal expansion of infiltrating T lymphocytes in chronic encephalitis of Rasmussen. J Immunol 158:1428–1437
Loscher W (2002) Animal models of epilepsy for the development of antiepileptogenic and disease-modifying drugs. A comparison of the pharmacology of kindling and post-status epilepticus models of temporal lobe epilepsy. Epilepsy Res 50:105–123
Maneta E, Garcia G (2013) Psychiatric manifestations of anti-NMDA receptor encephalitis: neurobiological underpinnings and differential diagnostic implications. Psychosomatics 55(1):37–44
Manev H, Favaron M, Guidotti A, Costa E (1989) Delayed increase of Ca2+ influx elicited by glutamate: role in neuronal death. Mol Pharmacol 36:106–112
Mantegazza R, Bernasconi P, Baggi F, Spreafico R, Ragona F, Antozzi C, Bernardi G, Granata T (2002) Antibodies against GluR3 peptides are not specific for Rasmussen’s encephalitis but are also present in epilepsy patients with severe, early onset disease and intractable seizures. J Neuroimmunol 131(1–2):179–185
Manto M, Dalmau J, Didelot A, Rogemond V, Honnorat J (2010) In vivo effects of antibodies from patients with anti-NMDA receptor encephalitis: further evidence of synaptic glutamatergic dysfunction. Orphanet J Rare Dis 5:31
Manto M, Dalmau J, Didelot A, Rogemond V, Honnorat J (2011) Afferent facilitation of corticomotor responses is increased by IgGs of patients with NMDA-receptor antibodies. J Neurol 258:27–33
Marignier R, Chenevier F, Rogemond V, Sillevis Smitt P, Renoux C, Cavillon G, Androdias G, Vukusic S, Graus F, Honnorat J, Confavreux C (2010) Metabotropic glutamate receptor type 1 autoantibody-associated cerebellitis: a primary autoimmune disease? Arch Neurol 67:627–630
Masu M, Tanabe Y, Tsuchida K, Shigemoto R, Nakanishi S (1991) Sequence and expression of a metabotropic glutamate receptor. Nature 349:760–765
Mat A, Adler H, Merwick A, Chadwick G, Gullo G, Dalmau JO, Tubridy N (2013) Ophelia syndrome with metabotropic glutamate receptor 5 antibodies in CSF. Neurology 80:1349–1350
Mathern GW, Pretorius JK, Leite JP, Kornblum HI, Mendoza D, Lozada A, Bertram EH 3rd (1998) Hippocampal AMPA and NMDA mRNA levels and subunit immunoreactivity in human temporal lobe epilepsy patients and a rodent model of chronic mesial limbic epilepsy. Epilepsy Res 32:154–171
Mayer ML (2005) Glutamate receptor ion channels. Curr Opin Neurobiol 15:282–288
Mayer ML (2011a) Emerging models of glutamate receptor ion channel structure and function. Structure 19:1370–1380
Mayer ML (2011b) Structure and mechanism of glutamate receptor ion channel assembly, activation and modulation. Curr Opin Neurobiol 21:283–290
Meldrum BS (1994) The role of glutamate in epilepsy and other CNS disorders. Neurology 44:S14–S23
Meldrum BS (2000) Glutamate as a neurotransmitter in the brain: review of physiology and pathology. J Nutr 130:1007S–1015S
Miyamoto M, Tsuboi Y, Honda K, Kobayashi M, Takamiya K, Huganir RL, Kondo M, Shinoda M, Sessle BJ, Katagiri A, Kita D, Suzuki I, Oi Y, Iwata K (2012) Involvement of AMPA receptor GluR2 and GluR3 trafficking in trigeminal spinal subnucleus caudalis and C1/C2 neurons in acute-facial inflammatory pain. PLoS ONE 7:e44055
Nabbout R (2012) Autoimmune and inflammatory epilepsies. Epilepsia 53(Suppl 4):58–62
Nakajima H, Hosoya M, Takahashi Y, Matsuyama K, Tagami M, Ishida S, Furutama D, Sugino M, Kimura F, Shinoda K, Hanafusa T (2007) A chronic progressive case of enteroviral limbic encephalitis associated with autoantibody to glutamate receptor epsilon2. Eur Neurol 57:238–240
Nicolai J, Aldenkamp AP, Arends J, Weber JW, Vles JS (2006) Cognitive and behavioral effects of nocturnal epileptiform discharges in children with benign childhood epilepsy with centrotemporal spikes. Epilepsy Behav 8:56–70
Ohashi H, Maruyama T, Higashi-Matsumoto H, Nomoto T, Nishimura S, Takeuchi Y (2002) A novel binding assay for metabotropic glutamate receptors using [3H] l-quisqualic acid and recombinant receptors. Z Naturforsch C 57:348–355
Okamoto S, Hirano T, Takahashi Y, Yamashita T, Uyama E, Uchino M (2007) Paraneoplastic limbic encephalitis caused by ovarian teratoma with autoantibodies to glutamate receptor. Intern Med 46:1019–1022
Okubo Y, Sekiya H, Namiki S, Sakamoto H, Iinuma S, Yamasaki M, Watanabe M, Hirose K, Iino M (2010) Imaging extrasynaptic glutamate dynamics in the brain. Proc Natl Acad Sci USA 107:6526–6531
Olney JW (1990) Excitotoxicity: an overview. Can Dis Wkly Rep 16(Suppl 1E):47–57 discussion 57–58
Omdal R, Brokstad K, Waterloo K, Koldingsnes W, Jonsson R, Mellgren SI (2005) Neuropsychiatric disturbances in SLE are associated with antibodies against NMDA receptors. Eur J Neurol 12(5):392–398
Pin JP, Bockaert J (1995) Get receptive to metabotropic glutamate receptors. Curr Opin Neurobiol 5:342–349
Platt SR (2007) The role of glutamate in central nervous system health and disease—a review. Vet J 173:278–286
Pollak TA, McCormack R, Peakman M, Nicholson TR, David AS (2013) Prevalence of anti-N-methyl-D-aspartate (NMDA) antibodies in patients with schizophrenia and related psychoses: a systematic review and meta-analysis. Psychol Med, pp 1–13
Porter BE, Cui XN, Brooks-Kayal AR (2006) Status epilepticus differentially alters AMPA and kainate receptor subunit expression in mature and immature dentate granule neurons. Eur J Neurosci 23:2857–2863
Pruss H, Dalmau J, Arolt V, Wandinger KP (2010) Anti-NMDA-receptor encephalitis. An interdisciplinary clinical picture. Nervenarzt 81:396, 398, 400, passim
Pruss H, Finke C, Holtje M, Hofmann J, Klingbeil C, Probst C, Borowski K, Ahnert-Hilger G, Harms L, Schwab JM, Ploner CJ, Komorowski L, Stoecker W, Dalmau J, Wandinger KP (2012a) N-methyl-D-aspartate receptor antibodies in herpes simplex encephalitis. Ann Neurol 72:902–911
Pruss H, Holtje M, Maier N, Gomez A, Buchert R, Harms L, Ahnert-Hilger G, Schmitz D, Terborg C, Kopp U, Klingbeil C, Probst C, Kohler S, Schwab JM, Stoecker W, Dalmau J, Wandinger KP (2012b) IgA NMDA receptor antibodies are markers of synaptic immunity in slow cognitive impairment. Neurology 78:1743–1753
Rasmussen T, Olszewski J, Lloydsmith D (1958) Focal seizures due to chronic localized encephalitis. Neurology 8:435–445
Rheumatology TA (1999) The American College of Rheumatology nomenclature and case definitions for neuropsychiatric lupus syndromes. Arthritis Rheum 42:599–608
Rice JS, Kowal C, Volpe BT, DeGiorgio LA, Diamond B (2005) Molecular mimicry: anti-DNA antibodies bind microbial and nonnucleic acid self-antigens. Curr Top Microbiol Immunol 296:137–151
Roebling R, Scheerer N, Uttner I, Gruber O, Kraft E, Lerche H (2009) Evaluation of cognition, structural, and functional MRI in juvenile myoclonic epilepsy. Epilepsia 50:2456–2465
Rogers SW, Andrews PI, Gahring LC, Whisenand T, Cauley K, Crain B, Hughes TE, Heinemann SF, McNamara JO (1994) Autoantibodies to glutamate receptor GluR3 in Rasmussen’s encephalitis. Science 265:648–651
Rosenmund C, Stern-Bach Y, Stevens CF (1998) The tetrameric structure of a glutamate receptor channel. Science 280:1596–1599
Roubertie A, Boukhaddaoui H, Sieso V, de Saint-Martin A, Lellouch-Tubiana A, Hirsch E, Echenne B, Valmier J (2005) Antiglial cell autoantibodies and childhood epilepsy: a case report. Epilepsia 46(8):1308–1312
Sansing LH, Tuzun E, Ko MW, Baccon J, Lynch DR, Dalmau J (2007) A patient with encephalitis associated with NMDA receptor antibodies. Nat Clin Pract Neurol 3:291–296
Sato S, Kawashima H, Hoshika A, Yoshio T (2011) Clinical analysis of anti-NR2 glutamate receptor antibodies and interleukin-6 with neuropsychiatric systemic lupus erythematosus. Rheumatology (Oxford) 50(11):2142–2144
Shehata GA, Bateh Ael A (2009) Cognitive function, mood, behavioral aspects, and personality traits of adult males with idiopathic epilepsy. Epilepsy Behav 14:121–124
Shewmon DA, Erwin RJ (1988) The effect of focal interictal spikes on perception and reaction time I. General considerations. Electroencephalogr Clin Neurophysiol 69:319–337
Sillevis Smitt P, Kinoshita A, De Leeuw B, Moll W, Coesmans M, Jaarsma D, Henzen-Logmans S, Vecht C, De Zeeuw C, Sekiyama N, Nakanishi S, Shigemoto R (2000) Paraneoplastic cerebellar ataxia due to autoantibodies against a glutamate receptor. N Engl J Med 342:21–27
Sladeczek F, Momiyama A, Takahashi T (1993) Presynaptic inhibitory action of a metabotropic glutamate receptor agonist on excitatory transmission in visual cortical neurons. Proc Biol Sci 253:297–303
Solaro C, Mantegazza R, Bacigalupo A, Uccelli A (2006) Intractable myoclonus associated with anti-GluR3 antibodies after allogeneic bone marrow transplantation. Haematologica 91(12 Suppl):ECR62
Steiner J, Walter M, Glanz W, Sarnyai Z, Bernstein HG, Vielhaber S, Kastner A, Skalej M, Jordan W, Schiltz K, Klingbeil C, Wandinger KP, Bogerts B, Stoecker W (2013) Increased prevalence of diverse N-methyl-D-aspartate glutamate receptor antibodies in patients with an initial diagnosis of schizophrenia: specific relevance of IgG NR1a antibodies for distinction from N-methyl-d-aspartate glutamate receptor encephalitis. JAMA Psychiatry 70:271–278
Steup-Beekman G, Steens S, van Buchem M, Huizinga T (2007) Anti-NMDA receptor autoantibodies in patients with systemic lupus erythematosus and their first-degree relatives. Lupus 16(5):329–334
Takahashi Y, Matsuda K, Kubota Y, Shimomura J, Yamasaki E, Kudo T, Fukushima K, Osaka H, Akasaka N, Imamura A, Yamada S, Kondo N, Fujiwara T (2006) Vaccination and infection as causative factors in Japanese patients with Rasmussen syndrome: molecular mimicry and HLA class I. Clin Dev Immunol 13:381–387
Tanabe Y, Masu M, Ishii T, Shigemoto R, Nakanishi S (1992) A family of metabotropic glutamate receptors. Neuron 8:169–179
Thanou A, Merrill JT (2014) Treatment of systemic lupus erythematosus: new therapeutic avenues and blind alleys. Nat Rev Rheumatol 10:23–34
Theodore WH, Bhatia S, Hatta J, Fazilat S, DeCarli C, Bookheimer SY, Gaillard WD (1999) Hippocampal atrophy, epilepsy duration, and febrile seizures in patients with partial seizures. Neurology 52:132–136
Tomita M, Khan RL, Blehm BH, Santoro TJ (2004) The potential pathogenetic link between peripheral immune activation and the central innate immune response in neuropsychiatric systemic lupus erythematosus. Med Hypotheses 62:325–335
Tomiyama M, Furusawa K, Kamijo M, Kimura T, Matsunaga M, Baba M (2005) Upregulation of mRNAs coding for AMPA and NMDA receptor subunits and metabotropic glutamate receptors in the dorsal horn of the spinal cord in a rat model of diabetes mellitus. Brain Res Mol Brain Res 136:275–281
Twyman RE, Gahring LC, Spiess J, Rogers SW (1995) Glutamate receptor antibodies activate a subset of receptors and reveal an agonist binding site. Neuron 14:755–762
Tziperman B, Garty BZ, Schoenfeld N, Hoffer V, Watemberg N, Lev D, Ganor Y, Levite M, Lerman-Sagie T (2007) Acute intermittent porphyria, Rasmussen encephalitis, or both? J Child Neurol 22(1):99–105
Verhelst H, Verloo P, Dhondt K, De Paepe B, Menten B, Dalmau J, Van Coster R (2010) Anti-NMDA-receptor encephalitis in a 3 year old patient with chromosome 6p21.32 microdeletion including the HLA cluster. Eur J Paediatr Neurol 15:163–166
Villani F, Avanzini G (2002) The use of immunoglobulins in the treatment of human epilepsy. Neurol Sci 23(Suppl 1):S33–S37
Villani F, Spreafico R, Farina L, Giovagnoli AR, Bernasconi P, Granata T, Avanzini G (2001) Positive response to immunomodulatory therapy in an adult patient with Rasmussen’s encephalitis. Neurology 56:248–250
Watson R, Jiang Y, Bermudez I, Houlihan L, Clover L, McKnight K, Cross JH, Hart IK, Roubertie A, Valmier J, Hart Y, Palace J, Beeson D, Vincent A, Lang B (2004) Absence of antibodies to glutamate receptor type 3 (GluR3) in Rasmussen encephalitis. Neurology 63:43–50
Weissman JD, Khunteev GA, Heath R, Dambinova SA (2011) NR2 antibodies: risk assessment of transient ischemic attack (TIA)/stroke in patients with history of isolated and multiple cerebrovascular events. J Neurol Sci 300:97–102
Whitney KD, McNamara JO (2000) GluR3 autoantibodies destroy neural cells in a complement-dependent manner modulated by complement regulatory proteins. J Neurosci 20:7307–7316
Wiendl H, Bien CG, Bernasconi P, Fleckenstein B, Elger CE, Dichgans J, Mantegazza R, Melms A (2001) GluR3 antibodies: prevalence in focal epilepsy but no specificity for Rasmussen’s encephalitis. Neurology 57(8):1511–1514
Winchester RJ (1996) Systemic lupus erythematosus pathogenesis. In: Koopman W (ed) Arthritis and allied conditions. Williams andWilkins, Birmingham, pp 1361–1391
Yoshio T, Okamoto H, Hirohata S, Minota S (2013) IgG anti-NR2 glutamate receptor autoantibodies from patients with systemic lupus erythematosus activate endothelial cells. Arthritis Rheum 65(2):457–463
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Levite, M. GLUTAMATE RECEPTOR ANTIBODIES IN NEUROLOGICAL DISEASES: Anti-AMPA-GluR3 antibodies, Anti-NMDA-NR1 antibodies, Anti-NMDA-NR2A/B antibodies, Anti-mGluR1 antibodies or Anti-mGluR5 antibodies are present in subpopulations of patients with either: Epilepsy, Encephalitis, Cerebellar Ataxia, Systemic Lupus Erythematosus (SLE) and Neuropsychiatric SLE, Sjogren’s syndrome, Schizophrenia, Mania or Stroke. These autoimmune anti-glutamate receptor antibodies can bind neurons in few brain regions, activate glutamate receptors, decrease glutamate receptor’s expression, impair glutamate-induced signaling and function, activate Blood Brain Barrier endothelial cells, kill neurons, damage the brain, induce behavioral/psychiatric/cognitive abnormalities and Ataxia in animal models, and can be removed or silenced in some patients by immunotherapy. J Neural Transm 121, 1029–1075 (2014). https://doi.org/10.1007/s00702-014-1193-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-014-1193-3
Keywords
- Anti-glutamate receptor antibodies
- Anti-GluR3 antibodies
- Anti-NR2 antibodies
- Anti-NR1 antibodies
- Glutamate
- Glutamate receptors
- AMPA
- NMDA
- GluR3
- GluR3B
- NMDA-NR1
- NMDA-NR2
- NMDA-NR2A/B
- mGluR1
- mGluR5
- Epilepsy
- Autoimmune Epilepsy
- NMDA encephalitis
- Anti-NMDA receptor Encephalitis
- Encephalitis
- Systemic Lupus Erythematosus (SLE)
- Neuropsychiatric lupus
- Neuropsychiatric Sjogren's Syndrome
- Schizophrenia
- Seizures
- Mania
- Stroke
- Paraneoplastic cerebellar ataxia
- Ophelia syndrome
- Immunotherapy for Epilepsy
- Neuropsychiatric impairments