Abstract
We report a newly developed analysis algorithm for optical coherence tomography (OCT) that makes a retinal single-layer analysis with calculation of the average thickness of retinal layers possible. The aim of the study was to examine specific patterns of retinal layer pathology as a potential marker of neurodegeneration in Parkinson’s disease (PD), progressive supranuclear palsy (PSP), and multiple system atrophy (MSA). Spectral domain OCT with a semiautomatic algorithm to calculate the average thickness of single retinal layers was applied to foveal scans of 65 PD, 16 PSP, and 12 MSA patients as well as 41 matched controls. Demographic and clinical data were collected for correlation analysis. Only PSP and MSA showed a significant reduction of retinal layers in comparison to controls. In PD, there were no significant findings in single retinal layer measurement. Most remarkably, the thickening of the outer nuclear layer in PSP and the outer plexiform layer in MSA was highly specific for these disease entities and allowed differentiating PSP from MSA with high sensitivity and specificity. With this analysis algorithm of OCT data, disease-specific retinal layer changes could be observed. Despite a general tendency to whole retinal and single retinal layer thinning that may reflect neurodegeneration in all Parkinsonian syndromes, the specific findings in MSA and PSP may serve as a highly sensitive and specific differential diagnostic tool and as a progression marker in these disease entities. Upcoming studies with a longitudinal setting will have to prove this assumption.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Optical coherence tomography (OCT) is able to detect changes of the retina in a manifold of central nervous system diseases (Albrecht et al. 2012a; Dorr et al. 2011; Galetta et al. 2011; Noval et al. 2011). With respect to retinal involvement in the neuropathological process of Parkinson’s disease (PD), some studies have shown segmental and others have shown total retinal nerve fiber layer (RNFL) thinning (Altintas et al. 2008). Even differences of retinal thinning according to tremor-dominant or akinetic-rigid Parkinsonism have been described recently (Rohani et al. 2012). The pattern of RNFL pathology in PD remains heterogenous. Archibald et al. (2009) actually detected no RNFL thinning in PD. Nevertheless, there is growing evidence that neither analysis of the RNFL alone nor the measurement of whole retinal thickness (WRT), but rather examination of the pre-ganglionar layers, adequately depicts retinal pathology in PD (Shrier et al. 2012; Spund et al. 2012). In progressive supranuclear palsy (PSP) and multiple system atrophy (MSA), only few OCT studies have yet been performed. Albrecht et al. (2012b) elicited different patterns of retinal changes in PSP, MSA, corticobasal syndrome (CBS), and PD with the most profound alterations in PSP and MSA. They suggest that the ratio between the outer nuclear layer (ONL) and the outer plexiform layer (OPL) delineates PSP from the other Parkinsonian syndromes. Fischer et al. (2011) report a significant RNFL thinning in MSA.
In contrast to former studies of single retinal layer analysis, we developed a semiautomatic analysis algorithm that is capable of obtaining average thickness measurements of single retinal layers in the perifoveal range. As there is substantial variation in the thickness of the retina (Hood et al. 2009), we consider an average thickness parameter to be more suitable to elicit disease-related alterations of the retinal layers than measurements at single retinal positions.
In this study, we investigated if the examination of the single retinal layer average perifoveal thickness is capable of eliciting specific retinal changes in PD, MSA, and PSP, which may be seen as an expression of the underlying neurodegenerative process and serve as a diagnostic or progression marker in these diseases.
Methods
Patients and controls
Sixteen PSP patients [10 females, 6 males, 68.6 ± 6.8 years (mean ± SD)], 12 MSA patients (8 females, 4 males, 65.9 ± 6.5 years), 65 PD patients (26 females, 39 males, 66.2 ± 12 years), and 41 healthy age- and sex-matched controls (19 females, 22 males, 65.1 ± 9.4 years) were examined. The disease duration was 8.9 years in PD, 4.9 years in MSA, and 3.9 years in PSP. For the diagnosis of PD, the UK Parkinson’s Disease Society Brain Bank criteria were used (Gibb and Lees 1988). The clinical diagnosis of MSA and PSP was made according to the Neuroprotection and Natural History In Parkinson Plus Syndromes (NNIPPS) diagnosis criteria (Bensimon et al. 2009). All patients were assessed and diagnosed by a board-certified neurologist specialized in movement disorders (EHP, JK). The study was approved by the local ethics committee (“Ethikkommission der Universität Ulm”, Local Ethics Committee Agreement: 130/12) and therefore performed in accordance with the ethical standards laid down in the Declaration of Helsinki. All persons gave their informed consent prior to their inclusion in the study. Patients with autoimmune inflammatory diseases of the central nervous system and any patient with any known eye disease (e.g., history of retinopathy, glaucoma, or high myopia) by anamnesis and medical report as well as every patient with a history of diabetes or alcohol dependency were excluded from the study. No patient had a smoking dependency. About 10 % of the patients screened had to be excluded.
Data acquisition and postprocessing
Horizontal, transfoveal “5-Line-HD” images were obtained from each participant with a Zeiss Cirrus HD-OCT 4000 (Carl Zeiss Meditec AG, Jena, Germany; Software version 5.1.1.6). Each of the images shows a 6 mm cross section of the macula that consists of 4096 A-scans with an axial resolution of 5 μm. The OCT device used in this study did not provide a feature to correct for ocular motion artifacts. In case of a blurred image, acquisition had to be repeated until the results were free from artifacts. If the acquisition of HD images was impossible, patients were excluded from analysis.
Data analysis was conducted by a newly developed analysis software based on the tensor imaging and fiber tracking (TIFT) software (Muller et al. 2007). A semi-automatic algorithm applies recognition of gray-level thresholds to separate the retinal layers. To correct for measurement errors caused by off-center measuring, each image had to be realigned horizontally and cut by 25 % to a length of 4.5 mm (i.e., 2.25 mm each in the temporal and nasal direction, Fig. 1b). This analysis software is device independent and can be used with any existing OCT machine if a high-resolution bitmap export of the OCT scan is possible.
a Mean absolute and relative average retinal layer thickness for progressive supranuclear palsy (PSP), multiple system atrophy (MSA), Parkinson’s disease (PD), and controls (Ctrl). RNFL retinal nerve fiber layer, GCL + IPL ganglion cell layer plus inner plexiform layer, INL inner nuclear layer, OPL outer plexiform layer, ONL outer nuclear layer, WRT whole retinal thickness, ONL/OPL ratio of outer nuclear layer to outer plexiform layer. b Overhead view: area of macular region measured; origin of 4.5 mm cross section marked in white. Cross section view: 4.5 mm cross section, semiautomatic delineation of single retinal layers’ areas by use of the tensor imaging and fiber tracking (TIFT) software: retinal nerve fiber layer (RNFL; red), ganglion cell layer plus inner plexiform layer (GCL + IPL; green), inner nuclear layer (INL; blue), outer plexiform layer (OPL; yellow), and outer nuclear layer (ONL; purple)
Average thickness was calculated for RNFL, ganglion cell layer plus inner plexiform layer (GCL + IPL), inner nuclear layer (INL), OPL, and ONL. The outer border of the ONL was set to the retinal pigment epithelium (RPE). Additionally, relative thickness in comparison to total retinal thickness was calculated to elicit possible disproportional changes in certain retinal layers.
A correlation analysis of whole retinal and single-layer thickness was executed in comparison to age, disease duration, the Short Motor Disability Scale (SMDS), the Unified Parkinson’s Disease Rating Scale (UPDRS) part III in the “off”-state and the NNIPPS-Parkinson Plus Scale (NPPS) (Payan et al. 2011) in MSA and PSP.
Statistical analysis
SPSS 19.0 Software (IBM, Armonk, NY, USA) was used. An analysis of variance (ANOVA) was performed with Dunnet’s multiple comparisons post hoc test for absolute and relative thicknesses as a quotient of single-layer thickness divided by WRT. A significance level of P < 0.05 was used. The Spearman-Rho correlation coefficient was used to perform the correlation analysis between OCT data and clinical scores. Additionally, the sensitivity, specificity, and receiver operating characteristic (ROC) curve were calculated for the ratio of ONL and OPL for comparison between MSA and PSP.
Results
Clinical and demographic data
The results are summarized in Tables 1 and 2. Neither the patient groups nor patients and controls differed significantly in age. The mean disease duration was longer in PD than in MSA and PSP. The mean UPDRS-III score in PD (29) was significantly lower than in MSA (45) and PSP (44). Likewise, the mean SMDS in PD (3) was significantly lower than in MSA (9) and PSP (7). The mean NPPS was 33 in MSA and 31 in PSP.
Semiautomatic retinal single-layer analysis
The results are summarized in Tables 1 and 2, the diagrams of all retinal layer measurements are delineated in Figs. 1a and 2.
All patient groups showed a thinning of WRT, RNFL, GCL + IPL, and INL in comparison to controls; however, a significant thinning could only be found in PSP for WRT and INL. The same was true for the relative thickness values except for the GCL + IPL in PD. In contrast to the general tendency of single retinal layer thinning, the measurement of ONL and OPL presented with an increase in relative and absolute OPL thickness in PSP in comparison to all other groups, which proved to be significant in comparison to MSA. Likewise, there was an increase in absolute and relative ONL thickness in MSA compared with all other groups, which was significant versus PSP. Furthermore, only ONL and OPL measurements showed significant differences between MSA and controls as well as between MSA and PD. Notably, only PD did not show any significant change in comparison with controls. In summary, a cluster of significant changes could be found in the ONL and OPL measurements in MSA and PSP. The ratio of increased ONL thickness in MSA and increased OPL thickness in PSP proved to be significant in the comparison of these diseases.
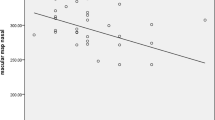
Specificity and sensitivity of ONL/OPL ratio in the comparison of MSA and PSP
In accordance with Albrecht et al. (2012b), we found significant reverse changes of thinner ONL and thicker OPL in our PSP patients. Additionally, we found the opposite reverse changes with thicker ONL and thinner OPL in MSA. Hence, we calculated the specificity and sensitivity of the ONL/OPL ratio for a possible best differentiation between these groups. With a cutoff of 5.03 for the ONL/OPL ratio, we were able to discriminate between PSP and MSA with a sensitivity of 88 % and a specificity of 91 %. The ROC curve for the threshold value of 5.03 showed an area under curve of 0.90 (Fig. 3).
Correlation analysis
Controls, and PD and MSA patients showed significant correlations of retinal thickness with age (P < 0.05); PSP showed no such correlation. Nevertheless, the distribution of significant correlations with age in controls, PD, and MSA showed a heterogenous pattern. In PD and controls GCL + IPL thinning and in PD and MSA WRT thinning correlated with age. There was no correlation of WRT or a single retinal layer’s absolute or relative thickness with any clinical score (UPDRS-III, SMDS, NPPS) in any patient group.
Discussion
In this study, we report about retinal single-layer pathology in PD, PSP, and MSA, examined with a semiautomatic algorithm for average single retinal layer thickness analysis. Due to the optimized resolution of the latest OCT systems, an analysis of single retinal layers beyond the RNFL and WRT is possible (Syc et al. 2012).
The analysis of WRT and single retinal layer thickness showed a general tendency to thinning in all patient groups in comparison to controls. It is remarkable that despite this general tendency, there were two exceptions, i.e., an increased OPL thickness in PSP and an increased ONL thickness in MSA. However, as shown in Tables 1 and 2, significance levels of retinal changes in the comparison of patients and controls and among the patient groups showed a heterogenous pattern, except for a cluster of significant results in the comparison of ONL and OPL thickness between MSA and PSP. Hence, the ONL to OPL ratio is a highly discriminatory marker between these diseases with a sensitivity of 88 % and a specificity of 91 % at a threshold ratio of 5.03. Furthermore, it is remarkable that only PD did not show any significant retinal changes in comparison with controls. This finding lines up with the heterogeneous state of current literature according retinal changes in PD and complies with the comparatively minor changes in brain MRI morphometry in PD. By contrast, the more pronounced retinal changes in atypical Parkinsonian syndromes are reflected in MRI morphometry with a distinct pattern of atrophy in MSA and PSP (Messina et al. 2011).
The findings in PSP are in line with the study of Albrecht et al. (2012b) who found nasal OPL to be significantly thicker in PSP compared to controls. A significant ONL thickening in MSA has not been reported before.
Many of the previous OCT studies in Parkinsonism have focused on the measurement of the RNFL and WRT with a heterogenous pattern of sector-wise retinal pathology (Altintas et al. 2008; Archibald et al. 2011; Fischer et al. 2011). Nevertheless, based on recent findings, there is growing evidence that retinal pathology in PD presents as a thinning of neural tissues that are involved in the processing of visual signals before they reach the optic nerve (Spund et al. 2012). Hence, WRT analysis or RNFL analysis may not be suitable to capture the retinal changes that are crucial in neurodegeneration with Parkinsonism.
Tissue loss in PD most probably represents not only that of dopaminergic amacrine cells, but may be related to an underlying more general neurodegenerative process possibly linked to alpha-synuclein pathology (Bodis-Wollner 2013). Especially in atypical Parkinsonism, retinal pathology may shadow the neurodegenerative pathological changes in the brain and hence may be linked to alpha-synuclein pathology in MSA and Tau-pathology in PSP. Ho et al. (2012) report that filamentous Tau-inclusions in the retina are formed, similar to those found in the brain, but there is no evidence of retinal Tau in PSP itself. We know from the studies by Braak et al. (2002) that pathological folding of alpha-synuclein in PD initially affects neurons other than the dopaminergic ones and neurites. Alpha-synuclein can be found ubiquitously in the retina (Martínez-Navarrete et al. 2007), but there is yet no neuropathologic evidence of specific alpha-synuclein related findings in PD or MSA so far.
The reason for the confirmed observation of OPL thickening in PSP and for the new finding of ONL thickening in MSA is not fully understood yet. Reports of rod bipolar cell dendrites sprouting from OPL into ONL in aging mice (Liets et al. 2006) indicate that a neuronal growth in OPL and ONL may reflect a compensatory reaction in response to a disease-related neurodegenerative process in the inner retinal layers with consecutive impaired synaptic transmission between rods and rod bipolar cells (Dick et al. 2003).
The semiautomatic approach of the analysis method used entails the risk of an examiner-induced bias in layer thickness measurements. However, the calculation of relative layer thickness showed mostly the same results in comparison to absolute thickness measurement; hence, a systematic error—if existent—would be negligible to the results, as discussed here.
In conclusion, selective changes of retinal layers may be seen as a reflection of neurodegenerative processes in the brain in Parkinsonism. The new method of single retinal layers’ average thickness analysis is capable to elicit differences between the disease entities and in comparison with controls. These findings go beyond the observation of a general retinal thinning and indicate to a cell population specific process especially in MSA and PSP. Yet, the hypothesis that this process is related to the underlying alpha-synuclein pathology in MSA and Tau-pathology in PSP needs further neuropathological examination. The findings in PSP and MSA (i.e., the ONL/OPL ratio) may have potential as progression marker in these entities. In PD, further investigations are needed to identify a reliable OCT parameter that depicts the neurodegenerative process. The latest studies by Bodis-Wollner and coworkers hint at a specific remodeling of the foveal pit in PD that may serve as such a tool (Spund et al. 2012).
Nevertheless, due to the still small sample sizes throughout all studies with atypical Parkinsonism and study-specific not fully comparable methods of measurement, larger cohorts of patients in a longitudinal setting and adapted analysis methods—most preferably in a multicenter study setting—will be necessary to evolve OCT into a useful marker of neurodegeneration in Parkinsonism.
References
Albrecht P, Muller AK, Ringelstein M et al (2012a) Retinal neurodegeneration in Wilson’s disease revealed by spectral domain optical coherence tomography. PLoS ONE 7:e49825. doi:10.1371/journal.pone.0049825
Albrecht P, Muller AK, Sudmeyer M et al (2012b) Optical coherence tomography in Parkinsonian syndromes. PLoS ONE 7:e34891. doi:10.1371/journal.pone.0034891
Altintas O, Iseri P, Ozkan B, Caglar Y (2008) Correlation between retinal morphological and functional findings and clinical severity in Parkinson’s disease. Doc Ophthalmol 116:137–146. doi:10.1007/s10633-007-9091-8
Archibald NK, Clarke MP, Mosimann UP, Burn DJ (2009) The retina in Parkinson’s disease. Brain J Neurol 132:1128–1145. doi:10.1093/brain/awp068
Archibald NK, Clarke MP, Mosimann UP, Burn DJ (2011) Retinal thickness in Parkinson’s disease. Parkinsonism Relat Disord 17:431–436. doi:10.1016/j.parkreldis.2011.03.004
Bensimon G, Ludolph A, Agid Y et al (2009) Riluzole treatment, survival and diagnostic criteria in Parkinson plus disorders: the NNIPPS study. Brain J Neurol 132:156–171. doi:10.1093/brain/awn291
Bodis-Wollner I (2013) Foveal vision is impaired in Parkinson’s disease. Parkinsonism Relat Disord 19:1–14. doi:10.1016/j.parkreldis.2012.07.012
Braak H, Del Tredici K, Bratzke H et al (2002) Staging of the intracerebral inclusion body pathology associated with idiopathic Parkinson’s disease (preclinical and clinical stages). J Neurol 249:III/1–III/5. doi:10.1007/s00415-002-1301-4
Dick O, Tom Dieck S, Altrock WD et al (2003) The presynaptic active zone protein bassoon is essential for photoreceptor ribbon synapse formation in the retina. Neuron 37:775–786
Dorr J, Wernecke KD, Bock M et al (2011) Association of retinal and macular damage with brain atrophy in multiple sclerosis. PLoS ONE 6:e18132. doi:10.1371/journal.pone.0018132
Fischer MD, Synofzik M, Heidlauf R et al (2011) Retinal nerve fiber layer loss in multiple system atrophy. Mov Disord 26:914–916. doi:10.1002/mds.23523
Galetta KM, Calabresi PA, Frohman EM, Balcer LJ (2011) Optical coherence tomography (OCT): imaging the visual pathway as a model for neurodegeneration. Neurother J Am Soc Exp Neurother 8:117–132. doi:10.1007/s13311-010-0005-1
Gibb WR, Lees AJ (1988) The relevance of the Lewy body to the pathogenesis of idiopathic Parkinson’s disease. J Neurol Neurosurg Psychiatry 51:745–752
Ho W-L, Leung Y, Tsang AW-T et al (2012) Review: tauopathy in the retina and optic nerve: does it shadow pathological changes in the brain? Mol Vis 18:2700–2710
Hood DC, Lin CE, Lazow MA et al (2009) Thickness of receptor and post-receptor retinal layers in patients with retinitis pigmentosa measured with frequency-domain optical coherence tomography. Invest Ophthalmol Vis Sci 50:2328–2336. doi:10.1167/iovs.08-2936
Liets LC, Eliasieh K, van der List DA, Chalupa LM (2006) Dendrites of rod bipolar cells sprout in normal aging retina. Proc Natl Acad Sci USA 103:12156–12160. doi:10.1073/pnas.0605211103
Martínez-Navarrete GC, Martín-Nieto J, Esteve-Rudd J et al (2007) Alpha synuclein gene expression profile in the retina of vertebrates. Mol Vis 13:949–961
Messina D, Cerasa A, Condino F et al (2011) Patterns of brain atrophy in Parkinson’s disease, progressive supranuclear palsy and multiple system atrophy. Parkinsonism Relat Disord 17:172–176. doi:10.1016/j.parkreldis.2010.12.010
Muller HP, Unrath A, Ludolph AC, Kassubek J (2007) Preservation of diffusion tensor properties during spatial normalization by use of tensor imaging and fibre tracking on a normal brain database. Phys Med Biol 52:N99–N109. doi:10.1088/0031-9155/52/6/N01
Noval S, Contreras I, Munoz S et al (2011) Optical coherence tomography in multiple sclerosis and neuromyelitis optica: an update. Mult Scler Int 2011:472790. doi:10.1155/2011/472790
Payan CAM, Viallet F, Landwehrmeyer BG et al (2011) Disease severity and progression in progressive supranuclear palsy and multiple system atrophy: validation of the NNIPPS–Parkinson plus scale. PLoS ONE 6:e22293. doi:10.1371/journal.pone.0022293
Rohani M, Langroodi AS, Ghourchian S et al (2012) Retinal nerve changes in patients with tremor dominant and akinetic rigid Parkinson’s disease. Neurol Sci Off J Ital Neurol Soc Ital Soc Clin Neurophysiol 34:689–693. doi:10.1007/s10072-012-1125-7
Shrier EM, Adam CR, Spund B et al (2012) Interocular asymmetry of foveal thickness in Parkinson disease. J Ophthalmol 2012:728457.doi:10.1155/2012/728457
Spund B, Ding Y, Liu T et al (2012) Remodeling of the fovea in Parkinson disease. J Neural Transm 120:745–753. doi:10.1007/s00702-012-0909-5
Syc SB, Saidha S, Newsome SD et al (2012) Optical coherence tomography segmentation reveals ganglion cell layer pathology after optic neuritis. Brain J Neurol 135:521–533. doi:10.1093/brain/awr264
Conflict of interest
All authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
702_2013_1072_MOESM1_ESM.tif
Supplementary Fig. 1 Sample OCT of 6 mm cross section of the macula scans that consist of 4096 A-scans with an axial resolution of 5 µm. Parkinson’s Disease (PD), Multiple System Atrophy (MSA), Progressive Supranuclear Palsy (PSP), Control (TIFF 6000 kb)
Rights and permissions
About this article
Cite this article
Schneider, M., Müller, HP., Lauda, F. et al. Retinal single-layer analysis in Parkinsonian syndromes: an optical coherence tomography study. J Neural Transm 121, 41–47 (2014). https://doi.org/10.1007/s00702-013-1072-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-013-1072-3