Abstract
Sepsis is characterized by systemic biochemical alterations including the central nervous system in the early times and cognitive impairment at later times after sepsis induction in the animal model. Recent studies have shown that, besides its hematological activity, erythropoietin (EPO) has cytoprotective effects on various cells and tissues. In order to corroborate elucidating the effects of alternative drugs for sepsis treatment, we evaluated the effects of both acute and chronic EPO treatment on oxidative stress and energetic metabolism in the hippocampus, and cognitive impairment, respectively, after sepsis induction by cecal ligation and perforation (CLP). To this aim, male Wistar rats underwent CLP with “basic support” or sham operation. In the acute treatment, EPO was administered once immediately after CLP induction. The rats were then killed after 6 and 24 h, and the hippocampus was removed for analysis of oxidative stress and energetic metabolism, respectively. Regarding the chronic treatment, EPO was administered once daily until the 4th day after induction. Aversive memory was tested on the 10th day after surgery. It was observed that the acute use of EPO (a single dose) alters the oxidative parameters and energetic metabolism. Chronic use (4 days) reversed cognitive impairment in the sepsis animal model. Mortality rates were attenuated only during chronic treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sepsis is characterized by a systemic inflammatory response to an insult (Vandijck et al. 2006) and is considered one of the most frequent causes of morbidity and mortality in intensive care units (ICU) (Sands et al. 1997). There are approximately 750,000 cases per year with 10–50% of deaths in North America (Angus et al. 2001) and around 400,000 new cases each year in Brazil (Marshall et al. 2005).
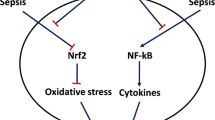
An essential feature of sepsis is the rapid production of cytokines, chemokines, prostaglandins and nitric oxide (Chao et al. 1995; Rietschel et al. 1996; Hu et al. 1997). At a macroscopic level, the systemic inflammatory response of sepsis causes significant hematological, hemodynamical and constitutional instability. At a microscopic level, there is impairment in the relationship between oxygen delivery and consumption, mainly related to defects in microcirculatory perfusion and disturbances in cellular metabolic pathways (Nelson et al. 1988; Cain and Curtis 1991). These changes, together with disruption of the brain blood barrier (BBB), may result in oxidative stress (Barichello et al. 2006; Comim et al. 2011), impairment of energetic metabolism (Comim et al. 2008, 2011) and apoptosis (Messaris et al. 2004; Semmler et al. 2005; Kafa et al. 2010) in the central nervous system (CNS), associated with depressive-like parameters (Comim et al. 2010) and cognitive damage (Barichello et al. 2005; Tuon et al. 2008). Thus, brain dysfunction caused by sepsis is known as septic encephalopathy (SE) and has been reported to occur in 8–70% of septic patients, depending on the inclusion criteria employed, and may be a poor outcome predictor (Sprung et al. 1990; Young et al. 1990).
Erythropoietin (EPO) is a 31-kDa glycoprotein that stimulates the proliferation, differentiation and survival of erythroid progenitor cells through an antiapoptotic mechanism (Jelkmann 1992). Recent studies have shown that, in addition to its hematological activity, EPO has cytoprotective effects on various cells and tissues. Although EPO is mainly produced by the fetal liver and adult kidneys, its receptors are also expressed in the brain, heart, lung, liver, kidneys, vascular endothelium and lymphoid tissues, and are even more pronounced in situations of hypoxia (Digicaylioglu et al. 1995; Westenfelder et al. 1999; Farrell and Lee 2004). Studies showed that the administration of exogenous EPO in animal models attenuated cerebral ischemia, spinal cord injury (Maiese et al. 2004), acute renal failure (Sharples and Yaqoob 2006) and myocardial ischemia (Abdelrahman et al. 2004). Paradoxically, it may induce lung injury by ischemia–reperfusion (Wu et al. 2006). In addition to its innumerous mechanisms of action, EPO has shown inhibitory effects on the activity of nitric oxide synthase (iNOS) (Squadrito et al. 1999; Akimoto et al. 1999), which produces large amounts of nitric oxide (NO), an important cause of hypotension, hypoperfusion and cell damage during sepsis (Chandra et al. 2006). Nitric oxide has direct deleterious effect on cells and becomes potentially pro-inflammatory and cytotoxic when it reacts with the hydroxyl radical (O2 −) to form peroxynitrite (ONOO−), a powerful free radical (Chandra et al. 2006).
Considering that there is a lack of information in the literature regarding the use of EPO in sepsis, even more in SE, the present study proposed to evaluate the effects of EPO on oxidative stress and energetic metabolism in the brain as well as cognitive deficits in septic rats submitted to sepsis by cecal ligation and perforation (CLP).
Materials and methods
Animals
Male Wistar rats (3–4 months old, 220–310 g) were obtained from our breeding colony (UNESC). The animals were housed five to a cage with food and water available ad libitum and maintained on a 12-h light/dark cycle (lights on at 7:00 a.m.). All experimental procedures involving animals were performed in accordance with the NIH Guide for the Care and Use of Laboratory Animals and the Brazilian Society for Neuroscience and Behavior (SBNeC) recommendations for animal care. All protocols performed were approved by the ethics committee at UNESC (protocol number 88/2011).
Experimental procedures
Under general anesthesia (ketamine at 80 mg kg−1 and xylazine at 10 mg kg−1), 24 and 15 male Wistar rats underwent CLP (sepsis group, single 14-G perforation) and sham operation (control group), respectively, as previously described. After surgery, the sepsis group received basic support (saline at 50 mL kg−1 immediately and 12 h after CLP plus ceftriaxone at 30 mg kg−1 and clindamycin at 25 mg kg−1 every 6 h for a total of 3 days). The sham-operated group received only saline at 50 mL kg−1, immediately and 12 h after surgery (volume of saline corresponded to antibiotic volume administered). The animals were divided into five groups: acute treatment: sham = 10 animals; CLP 6 h = 5 animals; CLP 24 h = 5 animals; chronic treatment: sham 10 days = 10 animals and CLP 10 days = 10 animals. All animals presented signs of encephalopathy 6 h after sepsis (lethargy, mild ataxia, lack of spontaneous movement and loss of righting reflex) and gradually returned to their normal awakened status 24–36 h after CLP. To minimize the possibility that the animals did not truly develop sepsis, the CLP procedure was performed by the same investigators at all times. In addition, all animals were observed after CLP to determine signs of infection (piloerection, lethargy, tachypnea and weight loss), and the number of animals that survived was in accordance with our previous reports (Barichello et al. 2005, 2006; Tuon et al. 2008; Comim et al. 2008, 2010, 2011).
Regarding the acute treatment, the animals received either a single systemic injection of EPO at 1,200 UI kg−1 administered subcutaneously, or saline solution immediately after the induction. The animals were killed after 6 h (oxidative stress evaluation) (Barichello et al. 2006) and 24 h (energetic metabolism evaluation) (Comim et al. 2008) of sepsis induction and had the hippocampus removed and immediately stored at −80°C for posterior analyses. With regard to chronic treatment, the animals received four doses (immediately, and 24, 48 and 72 h after surgery) of EPO at 300 UI kg−1—the final dose was the same as for acute treatment. The animals were then submitted to the step-down inhibitory avoidance task 10 days after surgery. Mortality was also evaluated during chronic treatment.
Behavior test
The step-down inhibitory avoidance test evaluates aversive memory. Briefly, the training apparatus was a 50 × 25 × 25-cm acrylic box (Albarsch, Porto Alegre, Brazil) with a floor consisting of parallel caliber stainless steel bars (1-mm diameter) spaced 1-cm apart. A 7-cm wide, 2.5-cm high platform was placed on the floor of the box against the left wall. During the training trial, the animals were placed on the platform and their latency to step down on the grid with all four paws was measured with an automatic device. Immediately after stepping down on the grid, the animals received a 0.4-mA, 2.0-s foot shock and were returned to their home cage. A retention test trial was performed 24 h after training. The retention test trial was procedurally identical to training, except that no foot shock was performed. The retention test step-down latency (maximum, 180 s) was used as a measure of inhibitory avoidance retention (Quevedo et al. 1999).
Biochemical analyses
Mitochondrial respiratory chain enzyme activities
Brain structures were homogenized (1:10, w/v) in SETH buffer (250 mM sucrose, 2 mM EDTA, 10 mM Trizma base, 50 IU mL−1 heparin, pH 7.4) for determination of mitochondrial respiratory chain enzyme activities (complexes I, II, II–III and IV). NADH dehydrogenase (complex I) was evaluated according to the method described by Cassina and Radi (1996) by the rate of NADH-dependent ferricyanide reduction at 420 nm (Cassina and Radi 1996). The activities of succinate–DCIP oxidoreductase (complex II) and succinate–cytochrome c oxidoreductase (complex II–III) were determined according to the method of Fischer et al. (1985). Complex II activity was measured by following the decrease in absorbance due to the reduction of 2,6-DCIP at 600 nm. Complex II–III activity was measured by cytochrome c reduction from succinate. The activity of cytochrome c oxidase (complex IV) was assayed by following the decrease in absorbance due to the oxidation of previously reduced cytochrome c at 550 nm (Miro et al. 1998). The activities of the mitochondrial respiratory chain complexes were expressed as nmol/min mg protein (Miro et al. 1998).
Creatine kinase activity
Creatine kinase (CK) activity was measured in brain homogenates pre-treated with 0.625 mM lauryl maltoside. The reaction mixture consisted of 60 mM Tris–HCl, pH 7.5, containing 7 mM phosphocreatine, 9 mM MgSO4 and approximately 0.4–1.2 lg protein in a final volume of 100 lL. After 15 min of pre-incubation at 37°C, the reaction was started by the addition of 0.3 lmol of ADP plus 0.08 lmol of reduced glutathione. The reaction was stopped after 10 min by the addition of 1 lmol of p-hydroxymercuribenzoic acid. The creatine formed was estimated according to the colorimetric method of Hughes (1962). The color was developed by the addition of 100 lL 2% α-naphthol and 100 lL 0.05% diacetyl in a final volume of 1 mL and read spectrophotometrically after 20 min at 540 nm. Results were expressed as U/min mg protein.
Citrate synthase activity
The method of citrate synthase (CS) activity has been described by Srere (1969). The reaction mix contained 100 mM Tris, pH 8.0, 0.1 mM acetyl-CoA, 0.1 mM 5,5′-ditiobis-(2 nitrobenzoic acid), 0.1% Triton X-100, 2–4 μg supernatant protein and initial oxaloacetate of 0.2 mM that was monitored with 412 nm for 3 min at 25°C.
Oxidative stress
In order to assess oxidative damage, the formation of thiobarbituric acid reactive species (TBARS) was measured during an acid-heating reaction, as previously described (Esterbauer and Cheeseman 1990). The samples were mixed with 1 mL of 10% trichloroacetic acid (TCA) and 1 mL of 0.67% thiobarbituric acid and were then heated in a boiling water bath for 15 min. Thiobarbituric acid reactive species was determined by the absorbance at 535 nm. Oxidative damage to proteins was measured by the quantification of carbonyl groups based on the reaction with dinitrophenylhydrazine (DNPH), as previously described (Levine et al. 1994). Proteins were precipitated by the addition of 20% TCA and redissolved in DNPH; the absorbance was read at 370 nm. To determine catalase (CAT) activity, the brain tissue was sonicated in 50 mmol/L phosphate buffer (pH 7.0), and the resulting suspension was centrifuged at 3,000g for 10 min. The supernatant was used for enzyme assay. Catalase activity was measured by the rate of decrease in hydrogen peroxide absorbance at 240 nm (Aebi 1984). Superoxide dismutase (SOD) activity was assayed by measuring the inhibition of adrenaline auto-oxidation, as previously described (Bannister and Calabrese 1987). All biochemical measures were normalized to the protein content, with bovine albumin as standard (Lowry et al. 1951).
Statistical analysis
Data from biochemical analyses are presented as mean ± SD. Data were analyzed by one-way analysis of variance (ANOVA) and multiple comparisons were performed by Tukey test. Data from inhibitory avoidance are presented as the median (interquartile range) of retention test latencies. Differences between training and test session latencies within each group were determined using the Wilcoxon test. Comparisons among groups were performed using Mann–Whitney U test. Mortality was assessed by Kaplan–Meier survival analysis and log rank test. Values of p < 0.05 were considered to be significant.
Results
The mortality rates are shown in Fig. 1. There were statistical differences in the mortality rates between CLP and sham groups 24 h after induction. The use of EPO prevented mortality during the first 4 days after CLP (time of treatment). Then, mortality rates were higher when compared with sham group and similar to the CLP group.
Figure 2 shows the oxidative and antioxidant activity in the hippocampus after acute treatment with EPO (6 h after surgery). We observed that there was an increase in lipid peroxidation in the CLP group when compared with the sham group. A decrease in TBARS levels was observed after acute treatment with EPO when compared with the sham and CLP groups (a). Regarding protein peroxidation, no differences between groups were observed (b). Regarding antioxidant activity, there was an increase in both CAT (c) and SOD (d) activities in the CLP group when compared with the sham group. Such increases were attenuated by acute treatment with EPO when compared with the CLP group.
Figure 3 demonstrates the effect of the acute treatment of EPO on energetic metabolism (24 h after surgery) in the hippocampus. No statistical differences were observed between groups regarding Complex I (a), Complex II (b), Complex III (c) and Complex IV (d). We believe that the significance was not possible in Fig. 1a due to the high standard deviation. The CK activity was decreased in comparison with the sham; the acute treatment with EPO also decreased CK activity when compared with the CLP and sham groups (e). Finally, there were no alterations in the CS activity between groups (f).
The results of the behavior test are shown in Fig. 4. The aversive memory was evaluated 10 days after surgery. Sepsis induction by CLP caused cognitive damage in the aversive memory; the chronic treatment with EPO was able to reverse the cognitive impairment observed in the CLP group.
Discussion
In this study, we observed that (1) the acute treatment with EPO (a single dose) did not attenuate oxidative stress or the energetic metabolism 6 and 24 h, respectively, after induction by CLP; (2) the chronic treatment (four doses) reversed the cognitive damage 10 days after sepsis induction by CLP; and (3) the use of EPO prevented mortality only in the first 4 days (during the EPO treatment) after induction.
Erythropoietin has been used in the treatment of certain types of anemia inhibiting apoptosis of erythrocyte progenitor cells and increasing formation of new red blood cells. Recently, EPO has also been recognized as a multifunctional cytokine with anti-inflammatory, anti-oxidative, and anti-apoptotic properties (Sharples et al. 2004; Ates et al. 2005; Cuzzocrea et al. 2006). Additionally, some reports have demonstrated the beneficial effects of EPO in animal models of acute inflammation (Cuzzocrea et al. 2006; Mitra et al. 2007; Aoshiba et al. 2009). The protective effects have been extensively investigated in animal models of ischemia–reperfusion injury as well. In these models, EPO effectively attenuated acute renal dysfunction by anti-apoptotic, anti-inflammatory and anti-oxidative mechanisms (Vesey et al. 2004; Sharples et al. 2004; Ates et al. 2005; Cuzzocrea et al. 2006). However, the issue of EPO transport across the BBB in vivo is complicated by the fact that endothelial cells synthesize a soluble EPO receptor (which is readily detected in humans) that would sequester EPO, neutralizing its biological activity (Yamaji et al. 1996; Harris and Winkelmann 1996).
In this regard, a great number of studies failed to demonstrate the beneficial effects of treatment using EPO. In a recent study, it was observed that acute treatment with EPO did not attenuate renal dysfunction or inflammation in a porcine model of endotoxemia (Sølling et al. 2011a). This same group showed in this study that the protective effect of EPO was against ischemia–reperfusion injury, but not against endotoxemia. In a randomized, double-masked, single-center trial study with preterm infants in Switzerland, it was observed that there were no significant effects of early high-dose EPO treatment in preterm infants on blood pressure, cerebral oxygenation, hemoglobin, leukocyte and platelet count (Fauchère et al. 2008). A previous report using pigs showed that the endotoxemia increased the number of apoptotic cell in the blood and the spleen, and EPO did not modify this alteration (Sølling et al. 2011b). This study does not support that EPO confers protection against lymphocyte apoptosis. The lymphocyte apoptosis may be crucial to the development of sepsis-induced immunosuppression. In vivo, microdialysis of hippocampal neurons reveals that NO production is elevated after EPO (Yamamoto et al. 2004). International guidelines do not recommend the use of EPO as a specific treatment for anemia associated with severe sepsis, although no specific information regarding its use in septic shock patients is currently available (Dellinger et al. 2008). The fact is that there are not many data in the literature regarding the benefits of the use of EPO in the septic brain, and there is still no consensus on the benefits of its use in many diseases.
The brain is particularly sensitive to oxidative damage due to its relative high content of peroxidizable fatty acids and limited antioxidant capacity (Floyd 1999). In our study, the use of EPO decreased the TBARS levels and also the levels of CAT and SOD. Similarly, Calapai et al. (2000) have demonstrated in a brain ischemic injury that EPO causes a decrease in malondialdehyde (MDA) levels during brain ischemia. Malondialdehyde is the end product of major reactions leading to significant oxidation of polyunsaturated fatty acids in cellular membranes and thus serves as a reliable marker of oxidative stress. The major intracellular antioxidant enzyme, SOD, rapidly and specifically reduces superoxide radicals (O2−) to hydrogen peroxide (H2O2). As the level of oxidative stress progresses, the level of SOD activity decreases (Floyd 1999). The decomposition of H2O2 to form water and oxygen is accomplished in the cell by CAT. One reason for the increase in MDA is the H2O2 in the medium (Floyd 1999). Both CAT and SOD enzymes break down the H2O2 formed in the tissues. However, the activities of these enzymes were increased by sepsis and decreased by EPO in our study. Therefore, we suggest that EPO may be acting by preventing oxidative damage before 6 h and, as oxidative stress progresses, the levels of SOD and CAT activity decrease.
With regard to mortality rates after treatment with EPO, this study observed that the administration of EPO prevented mortality only during chronic treatment—the first 4 days after surgery. Recent studies have raised important issues about the safety of EPO administration: (1) the treatment with EPO resulted in increased mortality in patients with acute stroke (Ehrenreich et al. 2009); (2) recent meta-analyses demonstrated that correcting anemia with EPO in patients with cancer may worsen survival (Tonelli et al. 2009; Bohlius et al. 2009); and (3) EPO increases the risk of thrombosis; so, caution should be taken when used in patients who are already at an increased risk of thrombosis, such as in critically ill patients.
Cognitive deficits are one of the alterations described in both humans (Iwashyna et al. 2010) and rats (Barichello et al. 2005a, b; Tuon et al. 2008) that survive sepsis. In this study, we showed that the use of EPO (divided into four doses) reversed the cognitive damage 10 days after induction. Although sufficient studies have not been done to assess a possible role for EPO in learning and memory, some authors have shown that the administration of EPO in healthy mice markedly increases conditioned taste aversion (Ehrenreich et al. 2004). We believe that EPO had effect on cognition by different pathways, because EPO did not increase CK activity and decreased the antioxidant activity in the hippocampus. Apparently, the beneficial effect observed with EPO administration was with regard to the level of lipid peroxidation and cognitive damage. The neurobiology of cognitive impairment in sepsis is still not entirely clear, but a number of studies have shown that oxidative stress may be involved in this complex process (for review see: Streck et al. 2008; Comim et al. 2009). We believe that the effects of EPO on learning and memory are likely to be an especially new area for future investigation, since no clear mechanism can be elucidated at this point.
In conclusion, this study observed that the acute use of EPO (a single dose) did not attenuate oxidative stress or energetic metabolism, but the chronic use (4 days) reversed the cognitive impairment in sepsis animal model. Also, mortality rate was decreased only during the first 4 days after induction (chronic treatment). Thus, further investigations are necessary to assess the effects of EPO treatment on CNS, memory, and learning to provide a solid mechanistic explanation for the beneficial effect of EPO in the animal model of sepsis.
References
Abdelrahman M, Rafi A, Ghacha R, Qayyum T, Karkar A (2004) Post-transplant erythrocytosis: a review of 47 renal transplant recipients. Saudi J Kidney Dis Transpl (an official publication of the Saudi Center for Organ Transplantation, Saudi Arabia) 4:433–439
Aebi H (1984) Catalase in vitro. Methods Enzymol 105:121–126
Akimoto T, Kusano E, Muto S, Fujita N, Okada K, Saito T, Komatsu N, Ono S, Ebata S, Ando Y, Homma S, Asano Y (1999) The effect of erythropoietin on interleukin-1beta mediated increase in nitric oxide synthesis in vascular smooth muscle cells. J hypertens 9:1249–1256
Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR (2001) Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med 29:1303–1310
Aoshiba K, Onizawa S, Tsuji T, Nagai A (2009) Therapeutic effects of erythropoietin in murine models of endotoxin shock. Crit Care Med 37:889–898
Ates E, Yalcin AU, Yilmaz S, Koken T, Tokyol C (2005) Protective effect of erythropoietin on renal ischemia and reperfusion injury. ANZ J Surg 75:1100–1105
Bannister JV, Calabrese L (1987) Assays for superoxide dismutase. Methods Biochem Anal 32:279–312
Barichello T, Martins MR, Reinke A, Feier G, Ritter C, Quevedo J, Dal-Pizzol F (2005) Cognitive impairment in sepsis survivors from cecal ligation and perforation. Crit Care Med 33:221–223
Barichello T, Fortunato JJ, Vitali AM, Feier G, Reinke A, Moreira JC, Quevedo J, Dal-Pizzol F (2006) Oxidative variables in the brain after sepsis induced by cecal ligation and perforation. Crit Care Med 34:886–889
Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, Zwahlen M, Clarke M, Weingart O, Kluge S, Piper M, Rades D, Steensma DP, Djulbegovic B, Fey MF, Ray-Coquard I, Machtay M, Moebus V, Thomas G, Untch M, Schumacher M, Egger M, Engert A (2009) Recombinant human erythropoiesis-stimulating agents and mortality in patients with cancer: a meta-analysis of randomized trials. Lancet 373:1532–1542
Cain SM, Curtis SE (1991) Experimental models of pathologic oxygen supply dependency. Crit Care Med 19:603–612
Calapai G, Marciano MC, Corica F, Allegra A, Parisi A, Frisina N, Caputi AP, Buemi M (2000) Erythropoietin protects against brain ischemic injury by inhibition of nitric oxide formation. Eur J Pharmacol 401:349–356
Cassina A, Radi R (1996) Differential inhibitory action of nitric oxide and peroxynitrite on mitochondrial electron transport. Arch Biochem Biophys 328:309–316
Chandra V, Pandav R, Laxminarayan R, Tanner C, Manyam B, Rajkumar S, Silberberg D, Brayne C, Chow J, Herman S, Hourihan F, Kasner S, Morillo L, Ogunniyi A, Theodore W, Zhang ZX (2006) Neurological disorders. In: Jamison DT, Breman JG, Measham AR, Alleyne G, Claeson M, Evans DB, Jha P, Mills A, Musgrove P (eds) Disease control priorities in developing countries, 2nd edn. World Bank, Washington, DC
Chao CC, Hu S, Peterson PK (1995) Glia, cytokines, and neurotoxicity. Crit Rev Neurobiol 9:189–205
Comim CM, Rezin GT, Scaini G, Di-Pietro PB, Cardoso MR, Petronilho FC, Ritter C, Streck EL, Quevedo J, Dal-Pizzol F (2008) Mitochondrial respiratory chain and creatine kinase activities in rat brain after sepsis induced by cecal ligation and perforation. Mitochondrion 8:313–318
Comim CM, Constantino LC, Barichello T, Streck EL, Quevedo J, Dal-Pizzol F (2009) Cognitive impairment in the septic brain. Curr Neurovasc Res 6:194–203
Comim CM, Cassol-Jr OJ, Constantino LC, Petronilho F, Constantino LS, Stertz L, Kapczinski F, Barichello T, Quevedo J, Dal-Pizzol F (2010) Depressive-like parameters in sepsis survivor rats. Neurotoxic Res 17:279–286
Comim CM, Cassol-Jr OJ, Constantino LS, Felisberto F, Petronilho F, Rezin GT, Scaini G, Daufenbach JF, Streck EL, Quevedo J, Dal-Pizzol F (2011) Alterations in inflammatory mediators, oxidative stress parameters and energetic metabolism in the brain of sepsis survivor rats. Neurochem Res 36:304–311
Cuzzocrea S, Di PR, Mazzon E, Patel NS, Genovese T, Muia C, Crisafulli C, Caputi AP, Thiemermann C (2006) Erythropoietin reduces the development of nonseptic shock induced by zymosan in mice. Crit Care Med 34:1168–1177
Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, Reinhart K, Angus DC, Brun-Buisson C, Beale R, Calandra T, Dhainaut JF, Gerlach H, Harvey M, Marini JJ, Marshall J, Ranieri M, Ramsay G, Sevransky J, Thompson BT, Townsend S, Vender JS, Zimmerman JL, Vincent JL (2008) Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med 36:296–327
Digicaylioglu M, Bichet S, Marti HH, Wenger RH, Rivas LA, Bauer C, Gassmann M (1995) Localization of specific erythropoietin binding sites in defined areas of the mouse brain. Proc Natl Acad Sci USA 9:3717–3720
Ehrenreich H, Degner D, Meller J, Brines M, Béhé M, Hasselblatt M, Woldt H, Falkai P, Knerlich F, Jacob S, von Ahsen N, Maier W, Brück W, Rüther E, Cerami A, Becker W, Sirén AL (2004) Erythropoietin: a candidate compound for neuroprotection in schizophrenia. Mol Psychiatry 9:42–54
Ehrenreich H, Weissenborn K, Prange H, Schneider D, Weimar C, Wartenberg K, Schellinger PD, Bohn M, Becker H, Wegrzyn M, Jähnig P, Herrmann M, Knauth M, Bähr M, Heide W, Wagner A, Schwab S, Reichmann H, Schwendemann G, Dengler R, Kastrup A, Bartels C, EPO Stroke Trial Group (2009) Recombinant human erythropoietin in the treatment of acute ischemic stroke. Stroke 40:e647–e656
Esterbauer H, Cheeseman KH (1990) Determination of aldehydic lipid peroxidation products: malonaldehyde and 4-hydroxynonenal. Methods Enzymol 186:407–421
Farrell F, Lee A (2004) The erythropoietin receptor and its expression in tumor cells and other tissues. Oncologist 5:18–30
Fauchère JC, Dame C, Vonthein R, Koller B, Arri S, Wolf M, Bucher HU (2008) An approach to using recombinant erythropoietin for neuroprotection in very preterm infants. Pediatrics 122:375–382
Fischer JC, Ruitenbeek W, Berden JA, Trijbels JM, Veerkamp JH, Stadhouders AM, Sengers RC, Janssen AJ (1985) Differential investigation of the capacity of succinate oxidation in human skeletal muscle. Clin Chim Acta 153:23–36
Floyd RA (1999) Antioxidants, oxidative stress, and degenerative neurological disorders. Proc Soc Exp Biol Med 222:236–245
Harris KW, Winkelmann JC (1996) Enzyme-linked immunosorbent assay detects a potential soluble form of the erythropoietin receptor in human plasma. Am J Hematol 52:8–13
Hu S, Peterson PK, Chao CC (1997) Cytokine-mediated neuronal apoptosis. Neurochem Int 30:427–431
Hughes BP (1962) A method for the estimation of serum creatine kinase and its use in comparing creatine kinase and aldolase activity in normal and pathological sera. Clin Chim Acta 7:597–603
Iwashyna TJ, Ely EW, Smith DM, Langa KM (2010) Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA 304:1787–1794
Jelkmann W (1992) Erythropoietin: structure, control of production, and function. Physiol Rev 2:449–489
Kafa IM, Uysal M, Bakirci S, Ayberk Kurt M (2010) Sepsis induces apoptotic cell death in different regions of the brain in a rat model of sepsis. Acta Neurobiol Exp 70:246–260
Levine RL, Williams JA, Stadtman ER, Shacter E (1994) Carbonyl assays for determination of oxidatively modified proteins. Methods Enzymol 233:346–357
Lowry OH, Rosebrough NJ, Farr AL, Randall RJ (1951) Protein measurement with the folin phenol reagent. J Biol Chem 193:265–275
Maiese K, Li F, Chong ZZ (2004) Erythropoietin in the brain: can the promise to protect be fulfilled? Trends Pharmacol Sci 11:577–583
Marshall JC, Deitch C, Moldawer LL, Opal S, Redl H, Van der Poll T (2005) Preclinical models of shock and sepsis: what can they tell us? Shock 24:1–6
Messaris E, Memos N, Chatzigianni E, Konstadoulakis MM, Menenakos E, Katsaragakis S, Voumvourakis C, Androulakis G (2004) Time-dependent mitochondrial-mediated programmed neuronal cell death prolongs survival in sepsis. Crit Care Med 32:1764–1770
Miro O, Cardellach F, Barrientos A, Casademont J, Rotig A, Rustin P (1998) Cytochrome c oxidase assay in minute amounts of human skeletal muscle using single wavelength spectrophotometers. J Neurosci Methods 80:107–111
Mitra A, Bansal S, Wang W, Falk S, Zolty E, Schrier RW (2007) Erythropoietin ameliorates renal dysfunction during endotoxaemia. Nephrol Dial Transplant 22:2349–2353
Nelson DP, Samsel RW, Wood LDH, Schumacker PT (1988) Pathological supply dependence of systemic and intestinal O2 uptake during endotoxemia. J Appl Physiol 64:2410–2419
Quevedo J, Vianna MR, Roesler R, Izquierdo I (1999) Two time windows of anisomycin-induced amnesia for inhibitory avoidance training in rats: protection from amnesia by pretraining but not pre-exposure to the task apparatus. Learn Mem 6:600–607
Rietschel ET, Brade H, Holst O, Brade L, Müller-Loennies S, Mamat U, Zähringer U, Beckmann F, Seydel U, Brandenburg K, Ulmer AJ, Mattern T, Heine H, Schletter J, Loppnow H, Schönbeck U, Flad HD, Hauschildt S, Schade UF, Di Padova F, Kusumoto S, Schumann RR (1996) Bacterial endotoxin: chemical constitution, biological recognition, host response, and immunological detoxification. Curr Top Microbiol Immunol 216:39–81
Sands KE, Bates DW, Lanken PN, Graman PS, Hibberd PL, Kahn KL, Parsonnet J, Panzer R, Orav EJ, Snydman DR, Black E, Schwartz JS, Moore R, Johnson BL, Platt R (1997) Academic Medical Center Consortium Sepsis Project Working Group: epidemiology of sepsis syndrome in 8 academic medical centers. JAMA 278:234–238
Semmler A, Okulla T, Sastre M, Dumitrescu-Ozimek L, Heneka MT (2005) Systemic inflammation induces apoptosis with variable vulnerability of different brain regions. J Chem Neuroanat 30:144–157
Sharples EJ, Yaqoob MM (2006) Erythropoietin and acute renal failure. Sem Nephrol 4:325–331
Sharples EJ, Patel N, Brown P, Stewart K, Mota-Philipe H, Sheaff M, Kieswich J, Allen D, Harwood S, Raftery M, Thiemermann C, Yaqoob MM (2004) Erythropoietin protects the kidney against the injury and dysfunction caused by ischemia–reperfusion. J Am Soc Nephrol 15:2115–2224
Sølling C, Christensen AT, Nygaard U, Krag S, Frøkiaer J, Wogensen L, Krog J, Tønnesen EK (2011a) Erythropoietin does not attenuate renal dysfunction or inflammation in a porcine model of endotoxemia. Acta Anaesthesiol Scand 55(4):411–421
Sølling C, Nygaard U, Christensen AT, Wogensen L, Krog J, Tønnesen EK (2011b) Lymphocyte apoptosis is resistant to erythropoietin in porcine endotoxemia. APMIS 119:143–154
Sprung CL, Peduzzi PN, Shatney CH, Schein RM, Wilson MF, Sheagren JN, Hinshaw LB (1990) Impact of encephalopathy on mortality in the sepsis syndrome. The Veterans Administration Systemic Sepsis Cooperative Study Group. Crit Care Med 18:801–806
Squadrito F, Altavilla D, Squadrito G, Campo GM, Arlotta M, Quartarone C, Saitta A, Caputi AP (1999) Recombinant human erythropoietin inhibits iNOS activity and reverts vascular dysfunction in splanchnic artery occlusion shock. Br J Pharmacol 2:482–488
Srere PA (1969) Citrate synthase. Methods Enzymol 13:3–11
Streck EL, Comim CM, Barichello T, Quevedo J (2008) The septic brain. Neurochem Res 33:2171–2177
Tonelli M, Hemmelgarn B, Reiman T, Manns B, Reaume MN, Lloyd A, Wiebe N, Klarenbach S (2009) Benefits and harms of erythropoiesis-stimulating agents for anemia related to cancer: a meta-analysis. CMAJ 180:E62–E71
Tuon L, Comim CM, Petronilho F, Barichello T, Izquierdo I, Quevedo J, Dal-Pizzol F (2008) Time-dependent behavioral recovery after sepsis in rats. Intensive Care Med 34:1724–1731
Vandijck D, Decruyenaere JM, Blot SI (2006) The value of sepsis definitions in daily ICU-practice. Acta Clin Belg 6:220–226
Vesey DA, Cheung C, Pat B, Endre Z, Gobe G, Johnson DW (2004) Erythropoietin protects against ischaemic acute renal injury. Nephrol Dial Transplant 19:348–355
Westenfelder C, Dl Biddle, Rl Baranowski (1999) Human, rat, and mouse kidney cells express functional erythropoietin receptors. Kidney Int 3:808–820
Wu ZS, Zhou GZ, Jiang JH, Shen GL, Yu RQ (2006) Gold colloid-bienzyme conjugates for glucose detection utilizing surface-enhanced Raman scattering. Talanta 3:533–539
Yamaji R, Okada T, Moriya M, Naito M, Tsuruo T, Miyatake K, Nakano Y (1996) Brain capillary endothelial cells express two forms of erythropoietin receptor mRNA. Eur J Biochem 239:494–500
Yamamoto M, Koshimura K, Sohmiya M, Murakami Y, Kato Y (2004) Effect of erythropoietin on nitric oxide production in the rat hippocampus using in vivo brain microdialysis. Neuroscience 128:163–168
Young GB, Bolton CF, Austin TW, Archibald YM, Gonder J, Wells GA (1990) The encephalopathy associated with septic illness. Clin Invest Med 13:297–304
Acknowledgments
This research was supported by grants from CNPq (ELS, JQ and FD-P), FAPESC (ELS, JQ and FD-P) and UNESC (ELS, JQ and FD-P). ELS, JQ and FD-P are CNPq Research Fellows. CMC is holder of a CNPq Studentship. LSC, FV and GS are holder of a CAPES Studentship.
Author information
Authors and Affiliations
Corresponding author
Additional information
C. M. Comim and O. J. Cassol Jr. collaborated in equal proportions.
Rights and permissions
About this article
Cite this article
Comim, C.M., Cassol, O.J., Abreu, I. et al. Erythropoietin reverts cognitive impairment and alters the oxidative parameters and energetic metabolism in sepsis animal model. J Neural Transm 119, 1267–1274 (2012). https://doi.org/10.1007/s00702-012-0774-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-012-0774-2