Abstract
Rivastigmine is a potent acetyl- and butyrylcholinesterase inhibitor widely used for cognitive improvement in Alzheimer’s disease (AD) therapy. However, dose-limiting adverse effects restrict its tolerability and clinical outcomes. This study explored new combined therapy, in which peripheral cholinergic adverse effects and central cognitive amelioration of rivastigmine were differentiated by a peripheral cholinoceptor antagonist anisodamine. The results demonstrated that rivastigmine (0.75 and 2.0 mg/kg) could significantly reverse the scopolamine-induced cognitive deficit in mice through passive avoidance test. Nevertheless, a high dose of rivastigmine (3.25 mg/kg) would compromise cognitive amelioration and produce obvious adverse effects, including hypersalivation, intestinal hyperperistalsis and muscle cramp. Interestingly, concomitant administration of anisodamine (10 mg/kg) effectively counteracted both the muscarinergic and nicotinergic adverse effects, while facilitating cognitive amelioration of rivastigmine (3.25 mg/kg). These findings provide an insight into the feasibility of combined therapy with cholinesterase inhibitors and peripheral cholinoceptor antagonists for the treatment of AD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
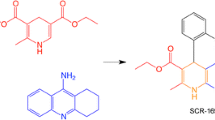
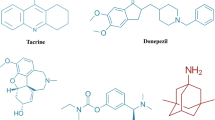
Alzheimer’s disease (AD) is characterized by the presence of neuritic amyloid plaques and neurofibrillary tangles in the brain, together with pathologic changes associated with cholinergic denervation. Its clinical symptoms are progressive disturbance of multiple cortical functions including memory, judgment, orientation, comprehension, learning capacity and language. Although most of the major neurotransmitter systems have been implicated in the etiology of AD, the loss of forebrain cholinergic function is the most dramatic and consistent neurobiological abnormality. The relatively unaffected impact on post-synaptic muscarinic receptors of the disease supports the ideas that direct- or indirect-acting muscarinic receptor agonists would be effective for cognitive improvement in AD therapy (Holzgrabe et al. 2007). Therefore, cholinesterase inhibitors, such as rivastigmine, galantamine, donepezil and huperzine A, have been successfully explored for treatment of the cognitive deficits in their early stage through maintaining synaptic levels of acetylcholine.
Among the well-established cholinesterase inhibitors, rivastigmine is a carbamate-type dual inhibitor of brain acetyl- and butyrylcholinesterase. In clinical trials, its beneficial effects on standard measures of cognitive and global function have been observed at 6–12 mg/day in patients with mild to moderate AD (Gauthier et al. 2006). Subsequent trials allowing increased dosage showed improvement in cognitive performance, but were still modest in outcome partly due to dose-limiting adverse effects including nausea, vomiting, gastrointestinal disturbances, agitation, headache, fainting and muscle cramp, etc (Frankfort et al. 2005; Siddiqui and Wagstaff 2006; Pavlis et al. 2007). It has been reported that inhibition of butyrylcholinesterase may correlate with peripheral toxicity, such as gastrointestinal disturbances and muscle cramp. However, exploring new compounds with high selectivity for acetylcholinesterase, donepezil, for example, hardly improved the tolerability profile of agents (Liston et al. 2004). More recent evidence indicates that in AD, butyrylcholinesterase activity progressively increases as the severity of dementia advances, while acetylcholinesterase activity declines. Both acetyl- and butyrylcholinesterase play important roles in the pathogenesis of AD and are legitimate targets when managing the disease. Therefore, inhibition of butyrylcholinesterase may provide additional benefits (Lane et al. 2006). Accordingly, despite similar peripheral adverse effects as with selective acetylcholinesterase inhibitors, rivastigmine has specific benefits in late-stage AD (Stahl 2000). Thus, it is of great importance to find other therapeutic strategies in which both acetyl- and butyrylcholinesterase could be inhibited by rivastigmine to ameliorate cognition, while the unfavorable peripheral cholinergic adverse effects could be avoided.
One kind of rational choice is that a combination of cholinoceptor antagonist with cholinesterase inhibitor might reserve central cognitive amelioration, but counteract peripheral adverse effects of cholinesterase inhibitor. Anisodamine, a peripheral cholinoceptor antagonist widely used in China, was originally isolated from scopolia tangutica, a Chinese traditional medicinal herb primarily found in the Tibet region (Poupko et al. 2007). Anisodamine also possesses other diverse beneficial actions besides its cholinoceptor antagonism. For example, it is reported that anisodamine can improve the deficits of learning and memory in avoidance response of rats after medial frontal cortex damage or acute cerebral ischemia and reperfusion by reducing calcium overload in the brain (Zhang et al. 1995). The high safety of anisodamine has been well documented in the treatment of numerous serious toxic shocks, thrombosis and neuralgia (Yang et al. 2007). Our previous study demonstrated that anisodamine hardly influenced cognition at normal doses due to its extremely low blood–brain barrier permeability (Zhang et al. 2008). When combined with non-selective muscarinic agonist pilocarpine, anisodamine could separate the peripheral cholinergic adverse effects from central cognitive amelioration of pilocarpine (Wang et al. 2003). In the present investigation, anisodamine was explored to differentiate peripheral cholinergic adverse effects and central cognitive amelioration of the commonly used acetyl- and butyrylcholinesterase inhibitor rivastigmine. The study presents experimental evidences for the feasibility of the combined therapy with cholinesterase inhibitors and peripheral cholinoceptor antagonists in the treatment of AD.
Materials and methods
Chemicals
Anisodamine hydrochloride was obtained from Shanghai Number One Chemical Pharmaceutical Co. Ltd. Activated charcoal was from Shanghai Chemicals Company of Chinese medicinal bloc. Carboxymethylcellulose was purchased from Shanghai Lengxin Chemicals Co. Ltd (-)-Scopolamine hydrobromide was from Sigma Chemical Company, St Louis, MO, USA. Hexamethonium bromide was from Acros Organics, NJ, USA. Rivastigmine was generously presented by Professor Zhui-Bai Qiu from the School of Pharmacy, Fudan University, Shanghai, China.
Animals
Kunming mice, regardless of gender, weighing 22–26 g were supplied by an experimental animal center of Shanghai Jiao Tong University School of Medicine. All animals were housed in plastic cages with food and water ad libitum and maintained on a 12/12 h light/dark cycle at 22 ± 1°C. All the procedures were in accordance with the Regulations of Experimental Animal Administration issued by the State Committee of Science and Technology of the People’s Republic of China.
Passive avoidance test
Mice were randomly assigned to ten groups, 12 mice per group. All drugs were diluted in normal saline and given intraperitoneally in a volume of 0.1 ml/10 g body weight. Control and model animals were given the same volume of normal saline. Rivastigmine-treated groups (0.75, 2.0 and 3.25 mg/kg) were used to delineate cognitive amelioration as well as the dose-limiting effects of rivastigmine. Anisodamine (1 or 10 mg/kg) was given 10 min preceding rivastigmine (3.25 mg/kg) to see whether anisodamine could influence central cognitive effects of rivastigmine. At 1 h after the administration of rivastigmine or saline, a single dose of 0.25 mg/kg scopolamine was given intraperitoneally to impair the memory of mice and thus provide animal models for AD. Anisodamine at 1 or 10 mg/kg, alone or followed 70 min later by scopolamine (0.25 mg/kg), respectively, was administered to study whether anisodamine had any influence on the central nervous system or could interfere with the amnesic effects of scopolamine at the present dosages in the passive avoidance test.
Training in the passive avoidance test was performed using a conventional two-compartment box. The experiment was performed 20 min after the injection of scopolamine by placing the mouse into the light compartment and maintaining them there for 1 min. Then, after opening the gate between the two compartments, inescapable electric shock at 33 V was given automatically once the mouse went into the dark room. When the shock ceased, the mice were immediately removed from the box and replaced in their cages. Retention was measured 24 h after training and expressed as error latency to enter the dark compartment within 300 s. Error latency for each drug group was compared with that in the scopolamine model group.
Measurement of salivary secretion and intestinal propulsion rate
Additional mice were given anisodamine (1 or 10 mg/kg) with or without rivastigmine (2.0 or 3.25 mg/kg). Rivastigmine (3.25 mg/kg) was also given 10 min after the injection of anisodamine (1 or 10 mg/kg). At 10 min after the injection of rivastigmine, a pre-weighed cotton ball was inserted into the mouse’s oral cavity and saliva was collected for 5 min. Difference between the initial weight and the weight after use of the cotton ball represented the salivary secretion (Wang et al. 2003). Following another 5 min, mice were treated by gavages with test meal consisting of 5% activated charcoal and 1% carboxymethylcellulose and killed 20 min later. The small intestines were removed and the longest distance traveled by the test meal and the total length from the pyloric sphincter to the ileo-caecal junction was measured. The ratio between these represented the intestinal propulsion rate.
Evaluation of muscle cramp
Blind methods were used for evaluation of muscle cramp. All drugs were given as in the observations of peripheral muscarinergic adverse effects. Hexamethonium (1.0 mg/kg) was given 10 min before rivastigmine (3.25 mg/kg) to discriminate its peripheral nicotinic antagonism for inhibition of muscle cramp. All observations were made by five observers who were unaware of the pretreatment received by the mice. They observed mice independently and then marked the extent of muscle cramp as follows: no muscle cramp = 0, occasional muscle twitches or slight muscle cramp = 1, moderate intermittent muscle cramp = 2, gross muscle cramp, but with occasional quiescent periods = 3. Assessments were made 15 min after rivastigmine injection and at 5-min intervals for 15 min thereafter.
Statistics
Data were expressed as mean ± SEM. One-way ANOVAs followed by post hoc Dunnett’s multiple comparison tests were used for statistical evaluation of differences between groups during passive avoidance test and observations of peripheral muscarinergic adverse effects. Values of P < 0.05 were considered to be statistically significant. The markers of muscle cramp were subjected to Kruskal–Wallis test, a non-parametric test and a P value of less than 0.01 was considered to be statistically significant.
Results
Effect of rivastigmine on scopolamine-induced cognitive deficit
In passive avoidance test, control mice avoided entering the dark compartment in the retention session 24 h after training, so that their error latency at 278 ± 22 s was over four times than that of the scopolamine model group at 65 ± 16 s (P < 0.01). Simultaneously, pre-administration of rivastigmine (0.75 and 2.0 mg/kg) significantly reversed the scopolamine-induced cognitive deficit with an increase in error latency to 217 ± 36 and 231 ± 33 s, respectively (P < 0.01). But, rivastigmine at higher dosage (3.25 mg/kg) compromised the ameliorating effect on scopolamine-induced cognitive deficit with error latency at only 106 ± 35 s (P > 0.05; Fig. 1a).
Influence of rivastigmine alone on scopolamine-induced cognitive deficit and its adverse effects. a Effect of rivastigmine on scopolamine-induced cognitive deficit in passive avoidance test. b Adverse effects of rivastigmine on salivary secretion and intestinal propulsion rate. Data were expressed as mean ± S.E.M. *P < 0.05, **P < 0.01, significantly different from the scopolamine 0.25 mg/kg model group. a P < 0.05, b P < 0.01, significant difference from control; c P < 0.05, d P < 0.01, significant difference from the rivastigmine 3.25 mg/kg group
Adverse effects of rivastigmine at high dose
The salivary secretion in the rivastigmine 2.0 and 3.25 mg/kg group increased by twofold (P < 0.05) and fourfold (P < 0.01) than the control, while the intestinal propulsion rate increased to 52 ± 4% for 2.0 mg/kg and 65 ± 6% for 3.25 mg/kg (P < 0.01) versus 39 ± 2% for the control (Fig. 1b).
Combined effect of anisodamine and rivastigmine on scopolamine-induced cognitive deficit
Anisodamine (1 or 10 mg/kg) did not impair the cognitive function of normal mice (P > 0.05 versus control) nor aggravate the cognitive deficit induced by scopolamine (P > 0.05 versus scopolamine group) (Fig. 2a). However, the cognitive amelioration of rivastigmine (3.25 mg/kg) was largely facilitated in the scopolamine-induced cognitive deficit mice through concomitant administration of anisodamine (1 or 10 mg/kg). For anisodamine (10 mg/kg) in combination with rivastigmine (3.25 mg/kg) group, error latency to enter the dark room increased to 187 ± 28 s (P < 0.05 versus scopolamine model group; Fig. 2b).
Combined effect of anisodamine and rivastigmine on salivary secretion and intestinal propulsion rate
Anisodamine alone at 1 or 10 mg/kg could also inhibit salivary secretion significantly (P < 0.05 and P < 0.01 versus control, respectively), while at 10 mg/kg tended to decrease intestinal propulsion rate without reaching significance (Fig. 3a). But in combined therapy with anisodamine and rivastigmine, both the hypersalivation and intestinal hyperperistalsis induced by rivastigmine (3.25 mg/kg) were significantly inhibited to similar level as the control (Fig. 3b). The salivary secretion and intestinal peristalsis were muscarinergic effects in nature. Here, anisodamine significantly counteracted peripheral muscarinergic adverse effects of rivastigmine.
Counteracting effect of anisodamine on muscle cramp induced by rivastigmine
Rivastigmine (3.25 mg/kg) could also induce time-dependent muscle cramp as shown in Fig. 4. Hexamethonium (1.0 mg/kg), the peripheral nicotinic acetylcholine receptor antagonist, significantly decreased the extent of muscle cramp 20 and 25 min after injection of rivastigmine, suggesting the nicotinergic activation of rivastigmine in peripheral neuromuscular junction (P < 0.05 compared with rivastigmine 3.25 mg/kg group). Likewise, anisodamine (10 mg/kg) counteracted the nicotinergic muscle cramp induced by rivastigmine (3.25 mg/kg) more effectively than hexamethonium.
Counteracting effect of anisodamine on muscle cramp induced by rivastigmine. Peripheral nicotinic receptor antagonist of ganglia blocker hexamethonium at 1.0 mg/kg was given 10 min before rivastigmine (3.25 mg/kg). Assessments were made by five observers 15 min after rivastigmine injection and at 5-min intervals for 15 min thereafter. Data were expressed as mean ± S.E.M. d P < 0.01 versus 3.25 mg/kg rivastigmine at the respective time point
Discussion
Although cholinesterase inhibitors are the current mainstays of medical therapy for AD, their clinical outcomes are still far from satisfactory, partly due to their dose-limiting adverse effects. The recent clinical study in USA demonstrated that larger dosage (400 μg b.i.d) of the cholinesterase inhibitor huperzine A was needed for effective cognitive improvement instead of its usual dosage of 200 μg b.i.d (Wang et al. 2009). However, long-term and large-dose regime of huperzine A might be hampered by the dose-limiting cholinergic adverse effects. New approaches are needed to improve the effectiveness and relief from adverse effects of the currently approved cholinesterase inhibitors. Some preliminary studies suggested that cholinesterase inhibitors in combination with memantine could ameliorate cognition synergistically, whereas cholinesterase inhibitors with antipsychotic could benefit patients with behavior disturbances (Schmitt et al. 2004). Recently, Jackish et al. (2009) reported that at least some of the clinically used cholinesterase inhibitors have unwanted indirect effects on acetylcholine release, due to autoinhibition of presynaptic acetylcholine release via the muscarinic M2 autoreceptor. So, the combined therapy with centrally acting muscarinic antagonists and cholinesterase inhibitors or inhibitors with centrally acting M2 muscarinic antagonism may also benefit AD patients. In addition, symptomatic medications were proposed to improve several cholinergic symptoms of cholinesterase inhibitors. For example, patients with nausea and/or vomiting were given domperidone or metoclopramide to relieve the gastrointestinal adverse effects and improve the tolerability of rivastigmine temporally (Forette et al. 1999; Scarzella et al. 2007).
In this report, we proposed a new combined therapy with rivastigmine and anisodamine to counteract peripheral cholinergic adverse effects and facilitate central cognitive amelioration of rivastigmine. So far, there are not sound animal models for AD, largely because of the poor understanding of the pathogenesis of AD. Both transgenic mice and animal models induced by pharmacological manipulations are commonly used for AD studies. The classical and acceptable AD model induced by scopolamine was applied here to simulate the cholinergic hypofunction in AD patients’ brain (Dodart and May 2005). The experimental results showed that rivastigmine at 2.0 mg/kg had better ameliorating effects on scopolamine-induced cognitive deficit than that of rivastigmine 0.75 mg/kg. Also, the peripheral adverse effects of mice at 2.0 mg/kg were more obvious than that at 0.75 mg/kg. The low dose and the middle dose used for rivastigmine at 0.75–2.0 mg/kg were nearly comparable to the commonly used dose at 6–12 mg/kg in clinic, on the basis of dose transformation formula. With the high dose at 3.25 mg/kg, we intended to obviously mimic the peripheral adverse effects of rivastigmine through animal models. In this study, we tried to prove the reasonability of a new combined therapy with cholinesterase inhibitors and brain-restricted cholinoceptor antagonists. Our experiments demonstrated that rivastigmine at the used high dose (3.25 mg/kg) had much less ameliorating effects on scopolamine-induced cognitive deficit than rivastigmine at lower doses (0.75 or 2.0 mg/kg; Fig. 1a). Otherwise, rivastigmine at 3.25 mg/kg produced obvious adverse effects including hypersalivation, intestinal hyperperistalsis and muscle cramp (Figs. 1b, 4). More interestingly, concurrent administration of the cholinoceptor antagonist anisodamine (10 mg/kg) could facilitate cognitive amelioration, which was compromised by rivastigmine (3.25 mg/kg) alone, and at the same time counteracted the adverse effects of rivastigmine (3.25 mg/kg; Figs. 2b, 3b, 4). In theory, concomitant use of medications with anticholinergic properties and cholinesterase inhibitors could potentially impact on cognitive and physical functioning in AD patients (Felder et al. 2000). The extremely low blood–brain barrier permeability and peripheral anticholinergic properties of anisodamine might contribute to its differential effects on the peripheral cholinergic adverse effects and central cognitive amelioration of rivastigmine. Alleviation of the adverse effects may improve the cognitive performance in animal models.
The muscarinic receptor antagonism of anisodamine has been well documented since its discovery in 1965. However, in our experiment, anisodamine counteracted not only muscarinergic adverse effects such as hypersalivation and intestinal hyperperistalsis, but also nicotinergic adverse effects of muscle cramp. The nicotinic receptor antagonist hexamethonium significantly decreased the extent of muscle cramp suggesting the indirect peripheral nicotinic activation of rivastigmine through maintaining acetylcholine levels at neuromuscular junctions (Inglis 2002). Therefore, the action of anisodamine on muscle cramp was obviously not mediated by its muscarinic antagonism. The nicotinic receptor antagonism of anisodamine (Zhao et al. 1993) may explain the counteracting effect of anisodamine on muscular abnormality induced by rivastigmine.
Indeed, in humans and, in particular, in subjects with AD, the primary dose-limiting actions are nausea and vomiting, which are generally considered to be mediated both centrally (Birks et al. 2009) and peripherally (Gottwald and Rozanski 1999). Nausea and vomiting induced by cholinesterase inhibitors-stimulated gastrointestinal motility are related to potentiation of peripheral cholinergic pathways by cholinesterase inhibitors (Jarvie et al. 2008). Although nausea and vomiting could not be imitated in mice, the cholinesterase inhibitors-induced gastrointestinal hyperperistalsis (cholinergic action in nature) could be reflected by the increased intestinal propulsion rate, as we measured. Therefore, our data suggested that anisodamine may also counteract the cholinesterase inhibitors-induced nausea and vomiting through its inhibition of gastrointestinal peristalsis.
Other brain-restricted cholinoceptor antagonists, such as quaternary scopolamine, may also antagonize peripheral adverse effects of cholinesterase inhibitors and are worth a trial. Among other agents, anisodamine has the profile of high safety that was well documented in its 40 years of clinical use in China. Moreover, anisodamine antagonized not only the muscarinergic adverse effects, but also the nicotinergic adverse effects of rivastigmine, besides other beneficial actions. Our findings may provide an insight that the combined therapy with peripheral cholinoceptor antagonist and the commonly used cholinesterase inhibitors might provide alternative therapeutic strategies for AD.
References
Birks J, Grimley Evans J, Iakovidou V, Tsolaki M, Holt FE (2009) Rivastigmine for Alzheimer's disease. Cochrane Database Syst Rev, CD001191
Dodart JC, May P (2005) Overview on rodent models of Alzheimer’s disease. Curr Protoc Neurosci 9:9.22.1–9.22.16
Felder CC, Bymaster FP, Ward J, DeLapp N (2000) Therapeutic opportunities for muscarinic receptors in the central nervous system. J Med Chem 43:4333–4353
Forette F, Anand R, Gharabawi G (1999) A phase II study in patients with Alzheimer’s disease to assess the preliminary efficacy and maximum tolerated dose of rivastigmine (Exelon). Eur J Neurol 6:423–429
Frankfort SV, Appels BA, de Boer A, Tulner LR, van Campen JP, Koks CH, Beijnen JH (2005) Discontinuation of rivastigmine in routine clinical practice. Int J Geriatr Psychiatry 20:1167–1171
Gauthier S, Juby A, Morelli L, Rehel B, Schecter R et al (2006) A large, naturalistic, community-based study of rivastigmine in mild-to-moderate AD: the EXTEND Study. Curr Med Res Opin 22:2251–2265
Gottwald MD, Rozanski RI (1999) Rivastigmine, a brain-region selective acetylcholinesterase inhibitor for treating Alzheimer's disease: review and current status. Expert Opin Investig Drugs 8:1673–1682
Holzgrabe U, Kapková P, Alptüzün V, Scheiber J, Kugelmann E (2007) Targeting acetylcholinesterase to treat neurodegeneration. Expert Opin Ther Targets 11:161–179
Inglis F (2002) The tolerability and safety of cholinesterase inhibitors in the treatment of dementia. Int J Clin Pract 127:45–63
Jackisch R, Förster S, Kammerer M, Rothmaier AK, Ehret A, Zentner J, Feuerstein TJ (2009) Inhibitory potency of choline esterase inhibitors on acetylcholine release and choline esterase activity in fresh specimens of human and rat neocortex. J Alzheimers Dis 16:635–647
Jarvie EM, Cellek S, Sanger GJ (2008) Potentiation by cholinesterase inhibitors of cholinergic activity in rat isolated stomach and colon. Pharmacol Res 58:297–301
Lane RM, Potkin SG, Enz A (2006) Targeting acetylcholinesterase and butyrylcholinesterase in dementia. Int J Neuropsychopharmacol 9:101–124
Liston DR, Nielsen JA, Villalobos A, Chapin D, Jones SB, Hubbard ST, Shalaby IA, Ramirez A, Nason D, White WF (2004) Pharmacology of selective acetylcholinesterase inhibitors: implications for use in Alzheimer’s disease. Eur J Pharmacol 486:9–17
Pavlis CJ, Kutscher EC, Carnahan RM, Kennedy WK, Van Gerpen S, Schlenker E (2007) Rivastigmine-induced dystonia. Am J Health Syst Pharm 64:2468–2470
Poupko JM, Baskin SI, Moore E (2007) The pharmacological properties of anisodamine. J Appl Toxicol 27:116–121
Scarzella L, Costanza A, Vastola K (2007) Domperidone is effective in the prevention of rivastigmine-related gastrointestinal disturbances. Funct Neurol 22:101–104
Schmitt B, Bernhardt T, Moeller HJ, Heuser I, Frölich L (2004) Combination therapy in Alzheimer’s disease: a review of current evidence. CNS Drugs 18:827–844
Siddiqui MA, Wagstaff AJ (2006) Rivastigmine: in Parkinson’s disease dementia. CNS Drugs 20:739–747
Stahl SM (2000) The new cholinesterase inhibitors for Alzheimer’s disease, Part 1: their similarities are different. J Clin Psychiatry 61:710–711
Wang H, Lu Y, Chen HZ (2003) Differentiating effects of anisodamine on cognitive amelioration and peripheral muscarinic adverse effects induced by pilocarpine in mice. Neurosci Lett 344:173–176
Wang BS, Wang H, Wei ZH, Song YY, Zhang L, Chen HZ (2009) Efficacy and safety of natural acetylcholinesterase inhibitor huperzine A in the treatment of Alzheimer’s disease: an updated meta-analysis. J Neural Transm 116:457–465
Yang LM, Xie YF, Chen HZ, Lu Y (2007) Diastereomeric and enantiomeric high-performance liquid chromatographic separation of synthetic anisodamine. J Pharm Biomed Anal 43:905–909
Zhang S, Liu J, He L (1995) Anisodamine (654–2) improves impaired cognitive function induced by experimental brain damage. Zhongguo Yi Xue Ke Xue Yuan Xue Bao 17:254–258
Zhang WW, Song MK, Cui YY, Wang H, Zhu L, Niu YY, Yang LM, Lu Y, Chen HZ (2008) Differential neuropsychopharmacological influences of naturally occurring tropane alkaloids anisodamine versus scopolamine. Neurosci Lett 443:241–245
Zhao CL, Ron S, Liu CG, He XP, Xie ZP (1993) Blocking effect of anisodamine on acetylcholine receptor channels. Zhongguo Yao Li Xue Bao 14:190–192
Acknowledgments
This study was sponsored by the National Natural Science Foundation of China (No. 30772553 and 30701018), the Major Basic Research Project of Shanghai Municipal Science and Technology Commission (07DJ14005) and Research Fund for the Doctoral Program of China Education Ministry (200802480058). We thank Ting Zhang, Yan Qin, Jing-Xia Chen, Yi-Qing Shi and Yan Zhou for their contribution to the experiment on muscle cramp evaluation.
Author information
Authors and Affiliations
Corresponding author
Additional information
W.-W. Zhang and Z.-P. Xu contributed equally to this work.
Rights and permissions
About this article
Cite this article
Zhang, WW., Xu, ZP., Cui, YY. et al. Peripheral cholinoceptor antagonist anisodamine counteracts cholinergic adverse effects and facilitates cognitive amelioration of rivastigmine. J Neural Transm 116, 1643–1649 (2009). https://doi.org/10.1007/s00702-009-0297-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-009-0297-7