Abstract
Recent results suggest that cytokine and glutamate receptors can interact directly and form receptor heteromers. Due to such heteromers, cytokines can act not only as classical neuromediators but also directly enhance glutamate gated ion channel activity via allosteric mechanisms. Our opinion is that such heteromers may lead to enhanced glutamate neurotoxicity in pathogenic processes of multiple sclerosis. Thus, agents targeting evolutionary conserved leucine-rich motifs responsible for such dimerization of receptors may represent a useful strategy to inhibit excitotoxicity in multiple sclerosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Human brain and immune system appear to have at least three deep similarities in their functional organization: cytokine networks (Goncharova and Tarakanov 2007), receptor mosaics (Agnati et al. 2008; Fuxe et al. 2007), and nanotubes at neural and immune synapses (Goncharova and Tarakanov 2008a) including ligand-gated ion channels (ionotropic glutamate receptors GluRs). A common feature of all these mechanisms of intercellular communications seems to be the related receptor assemblies which are formed by direct receptor–receptor interactions and provide a novel principle in molecular medicine (Fuxe et al. 2007, 2008). Chemokines, cytokines, and their receptors play important roles in such communications between neural and immune cells. Chemotactic cytokines (chemokines) are the only members of the cytokine family that act on G-protein coupled receptor (GPCR) superfamily where metabotropic glutamate receptors (mGluRs) also belong to the GPCR family. The possible common architecture of GPCRs and cytokine receptors (Goncharova and Tarakanov 2008b) suggests that they may act as molecular switches similar to the prototypical innate immune receptors: toll-like receptors (Gay et al. 2006). Thus, receptor heteromers can be formed by direct receptor–receptor interactions due to their evolutionary conserved leucine-rich motifs (Bell et al. 2005). We suppose that such heteromers may also lead to microglia-mediated excitotoxicity (Takeuchi et al. 2006) and neuroinflammatory responses (Fuxe et al. 2008), including multiple sclerosis.
Microglia
Microglia has been linked to pathology and disease progression in several neurodegenerative disorders including multiple sclerosis (MS). Excitotoxicity in general is linked to excessive glutamate activation of receptors, particularly the N-methyl-d-aspartate (NMDA) receptor (Pickering et al. 2005). Cell death resulting from excessive levels of glutamate and overstimulation of glutamate receptors can inter alia be caused by impaired uptake of glutamate by glial cells. Microglia can become overactivated or deregulated by two types of signals: (1) the direct stimulation of microglia by environmental toxins or endogenous proteins and (2) neuronal damage and consequent reactive microgliosis (Block et al. 2007). Overactivated microglia can induce significant and highly detrimental neurotoxic effects by the excess production of a large array of cytotoxic factors such as superoxide, nitric oxide (NO), proinflammatory prostaglandins (Aguirre et al. 2008) and cytokines.
Considerable research has been devoted to the role of the adaptive immune system in the pathogenesis of autoimmune inflammatory demyelination (AID) (O’Brien et al. 2008). AID is thought to occur spontaneously in patients with MS, a common cause of neurological disability. AID is also observed in the best characterized animal model of MS, experimental autoimmune encephalomyelitis (EAE). The adaptive immune system recognizes and responds to antigens via highly specific T-cell receptors. Myelin-reactive T-cells may initiate pathological immune responses that lead to central nervous system damage in MS and EAE. By contrast, the innate immune system recognizes evolutionarily conserved structures that are common to invading pathogens with high efficiency for rapid recognition and elimination of viruses, bacteria, and fungi. This recognition is mediated by pattern-recognition receptors such as toll-like receptors (TLRs) expressed on cells of the innate immune system (dendritic cells and CNS-resident cells, such as microglia) that have the potential to activate autoimmune responses by inducing the production of inflammatory cytokines and chemokines. Conversely, the innate immune system can also reduce autoimmune inflammation by inducing the production of immunoregulatory molecules such as type I interferons, which are currently used in the treatment of MS and block immune factors of class II MHC molecules (Boggild 2006). For example, O’Brien et al. (2008) review the evidence that TLRs can exacerbate or regulate AID and discuss the therapeutic potential of targeting either process.
Receptors
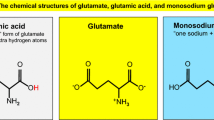
TLRs play an important role not only in innate but also in adaptive immunity, including the brain (Block et al. 2007). These receptors share a conserved modular structure (Fig. 1) with extracellular domain (ectodomain ECD), single transmembrane (TM) α-helix, and C-terminal homology motif called the Toll/Interleukin receptor (TIR) domain (Xu et al. 2000). The ECD contains block of repeats of a 24-amino acid motif, called a leucine-rich repeat (LRR), usually with cysteine-rich capping structures at the amino and carboxyl termini of each block (Bell et al. 2005). The LRR domains are found in a very large and diverse group of proteins and have been inferred to be responsible for molecular recognition (Matsushima et al. 2007). The LRR units fold into a curved, solenoidal structure (“horseshoe”), and the sequence conservation reflects the requirements for this structural scaffold, with the conserved residues forming the hydrophobic core of each LRR. Specific molecular recognition by LRR containing proteins is often achieved by interactions with the side chains of variable residues that protrude from the short parallel β-strand of each LRR and form the inner (concave) surface of the horseshoe. The arrangement of these side chains can be viewed as a combinatorial code that is able to bind specific ligands (Gay et al. 2006). According to Radons et al. (2003), a principal function of the TIR domain is also mediating homotypic protein–protein interactions in the signal transduction pathway.
Possible common architecture of toll-like receptor (TLR), cytokine receptor (CyR), ionotropic glutatamte receptor (GluR), and metabotropic glutamate receptor (mGluR). Extracellular binding pocket (“horseshoe”) can be formed by leucine-rich repeats (LRRs) of ectodomain (ECD) of TLR, β-sheets of Immunoglobulin (Ig) domains of CyR, and N-terminal of GluR and mGluR (TM transmembrane α-helix; TIR toll/interleukin receptor domain)
Gay et al. (2006) propose a molecular mechanism for signaling by TLRs that involves a series of protein conformational changes initiated by dimerization of their ECDs. The initial dimerization event, which is triggered by the interaction of the receptor with its ligand, might disrupt a pre-formed but non-functional dimer. Formation of a stable receptor-ligand complex then relieves constitutive autoinhibition, enabling receptor–receptor association of the extracellular juxtamembrane regions and cytoplasmic signaling domains. This activation process constitutes a tightly regulated, unidirectional molecular switch. The emerging picture of the molecular mechanism for TLR signaling has striking parallels with other receptors. For example, signaling by both the epidermal growth factor receptor which is a tyrosine kinase receptor (Uings and Farrow 2000) and the erythropoietin receptor which is a cytokine receptor (Watovich et al. 1996) involves binding of ligand to the ECD. This binding is followed by a conformational rearrangement of the juxtamembrane regions, causing stable receptor–receptor interactions (Gay et al. 2006). Possible common architecture (Fig. 1) also suggests that cytokine and glutamate receptors might all act as molecular switches similar to the TLRs (Goncharova and Tarakanov 2008b). Fuxe et al. (2008) propose that incorrect dimerization of such receptors may lead to neuroinflammation.
Receptor heteromers and glutamate excitotoxicity
Tumor necrosis factor alpha (TNFα) is a proinflammatory cytokine, the receptors for which (TNFR1, TNFR2) are expressed on both neurons and glial cells. It plays a facilitatory role in glutamate excitotoxicity, both directly and indirectly by inhibiting glial glutamate transporters on astrocytes. Additionally, TNFα has direct effects on glutamate transmission, for example increasing expression of alpha-amino-3hydroxy-5-methyl-4isoxazolepropionic (AMPA) receptors on synapses. Brain TNFα levels are typically increased in a wide range of neural disorders, including MS (Pickering et al. 2005).
Interferon gamma (IFNγ) also enhances the production of TNFα, NO and superoxide by surrounding micorglia in MS lesions and exacerbates the microglial reaction to neuronal degeneration. Mizuno et al. (2008) have reported for the first time that IFNγ directly induces neuronal damage in mouse cortical neurons through a unique neuron-specific receptor complex (receptor heteromer) containing the IFNγ receptor (IFNGR) and AMPA GluR1 receptor. Moreover, IFNγ phosphorylates GluR1 at the serine 845 position by the JAK/STAT pathway, increases Ca2+ influx and thereafter NO production, and subsequently decreases ATP production, leading to the dendritic bead formation. They also demonstrate that IFNγ synergistically enhances glutamate neurotoxicity mediated by AMPA receptors but not NMDA receptors. These findings provide novel mechanisms of neuronal excitotoxicity based on direct and specific cytokine–glutamate receptor interactions, which may occur in MS. Other excitotoxic mechanisms may also possibly exist in MS since epitopes of autoantibodies to NMDA heteromers exist in paraneoplastic limbic encephalitis (Takahashi 2008) as well as in certain forms of epilepsy (Takahashi et al. 2003).
Guyon and Nahon (2007) have preliminary data suggesting that chemokine receptor CXCR4 for stromal cell-derived factor SDF-1α should interact with gamma-amino butyric acid GABAB receptors (GABARs). As SDF-1α influences presynaptic GABA release, this could be another way to explain how different SDF-1α concentrations lead to different effects. Furthermore, CXCR4 and CCR2 (the receptor for the chemokine monocyte chemoattractant protein MCP-1) have been shown to form heterodimers (Percherancier et al. 2005) which is true also for CCR5 (receptor for macrophage inflammatory protein MIP-1) and CCR2b receptors colocated in CD4+ T-cells, the heterodimers of which exhibited reciprocal antagonistic receptor–receptor interactions at the recognition level via allosteric mechanisms (El-Asmar et al. 2005; Springael et al. 2006). Thus, chemokine receptor subtypes strongly interact in receptor heterodimers and SDF-1α can modulate the activity of neurons by multiple regulatory pathways involving possibly different types of CXCR4 containing heteromers including and often combining modulation of voltage-dependent channels and increase in neurotransmitter release (GABA, glutamate, dopamine), often through Ca-dependent mechanisms.
Following SDF-1α interaction, CXCR4 undergoes a dimerization which is necessary for its functionality and signaling (Mellado et al. 2001). Dimerization is accompanied by receptor phosphorylation as well as changes in signal transduction processes (Rodriguez-Frade et al. 2001). This dimerization enables the activation of the JAK/STAT pathway, which allows the subsequent triggering of G-protein dependent signaling events (Vila-Coro et al. 1999). Furthermore, SDF-1α itself can form a dimeric structure in solution at non-acidic pH. It is therefore possible that, depending on the concentration, SDF-1α would act as a monomer or oligomer on CXCR4 monomers or homodimers, leading to different responses. Heterodimerization is known to play a role in signal transduction of other metabotropic receptors. For example, GABAB receptors interact with mGluRs (Hirono et al. 2001). CXCR4 could also form heterodimers with other GPCRs, which could lead to complex responses according to the chemokines/peptides/neuromediator environment present in the extracellular medium.
Several proinflammatory cytokines have been reported to modulate glutamate excitotoxicity (Tables 1, 2). Interleukin-1beta (IL-1β) also enhances NMDA-mediated neurotoxicity and NMDA-induced Ca2+ influx (Viviani et al. 2003). Also IL-6 treatment of developing cerebellar granule neurons increases the excitotoxicity of NMDA (Qiu et al. 1998). We propose that these cytokines may function through a cytokine/glutamate receptor heteromer like IFNGR/GluR1 (Mizuno et al. 2008). Agents targeting such complexes of receptor heteromers may represent a useful strategy to inhibit excitotoxicity in MS.
Leucine-rich motifs as potential therapeutic targets
Generally, protein aggregation correlates with the development of several deleterious human disorders such as Alzheimer’s disease, Parkinson’s disease, prion-associated transmissible spongiform encephalopathies and type II diabetes (Fernandez-Busquets et al. 2008). The polypeptides involved in these disorders may be globular proteins with a defined 3D-structure or natively unfolded proteins in their soluble conformations. In either case, proteins associated with these pathogeneses all aggregate into amyloid fibrils sharing a common structure, in which β-strands of polypeptide chains are perpendicular to the fibril axis. Because of the prominence of amyloid deposits in many of these diseases, much effort has gone into elucidating the structural basis of protein aggregation. A number of recent experimental and theoretical studies have significantly increased our understanding of the process. On the one hand, solid-state NMR, X-ray crystallography and single molecule methods have provided us with the first high-resolution 3D structures of amyloids, showing that they exhibit conformational plasticity and are able to adopt different stable tertiary folds. On the other hand, several computational approaches have identified regions prone to aggregation in disease-linked polypeptides, predicted the differential aggregation propensities of their genetic variants, and simulated the early, crucial steps in protein self-assembly. Review of Fernandez-Busquets et al. (2008) summarizes these findings and their therapeutic relevance, as by uncovering specific structural or sequential targets they may provide us with a means to tackle the debilitating diseases linked to protein aggregation. For example, “hot spots” of such aggregation in TLR in comparison with cytokine and glutamate receptors have been predicted by (AGGRESCAN 2008) and shown in Fig. 2 together with corresponding LRRs. Amino acid codes of the receptors have been obtained from (NCBI 2008; PDB 2008).
According to Matsushima et al. (2007), all LRRs in TLRs include the highly conserved segment, LxxLxLxxNxL, in which “L” is Leu (shown by bold skew L in Figs. 2, 3, 4), Ile, Val, or Phe (bold I, V, or F) and “N” is Asn, Thr, Ser, or Cys (bold N, T, S, or C), and “x” is any amino acid. There are seven classes of LRRs including “typical” and “bacterial”. All known domain structures adopt an arc or “horseshoe” shape (ECD in Fig. 1). Vertebrate TLRs form six major families. The repeat numbers of LRRs and their “phasing” in TLRs differ with isoforms and species; they are aligned differently in various databases. Each of the six major TLR families is characterized by their constituent LRR motifs, their repeat numbers, and their patterns of cysteine clusters. For example, the central parts of the TLR1, TLR4, and TLR7 families have more irregular or longer LRR motifs. These central parts are inferred to play a key role in the structure and/or function of their TLRs. Furthermore, the super-repeat in the TLR7 family suggests strongly that “bacterial” and “typical” LRRs evolved from a common precursor (Matsushima et al. 2007). Traces of LxxLxLxxNxL can be found also in cytokine and glutamate receptors (Fig. 2). Note that “hot spots” of aggregation seem to be located at corresponding LRRs.
Four ECD motifs seem to be mostly cited directly by glutamate and cytokine receptors (Fig. 3). These motifs generalize the all 5- and 4-letter (amino acids) homologies of ECD of TLR3 with the glutamate receptors GluR1, mGluR5 and the cytokine receptors IFNGR, TNFR, IL1R. These homologies have been computed using our original software for comparing and visualization of protein structures together with nanotubes (Goncharova and Tarakanov 2008a). Note that at least three of the four mostly cited motifs in Fig. 3 are leucine-rich motifs. Moreover, these mostly cited motifs seem to be located between “hot spots” of aggregation but at leucine-rich motifs (Fig. 4). These results (Figs. 2, 3, 4) suggest that such leucine-rich motifs might be useful therapeutic targets to prevent incorrect dimerization of receptors.
Concluding remarks
Mizuno et al. (2008) have reported for the first time a unique neuron-specific receptor heteromer containing the cytokine and glutamate receptors. Our hypothesis is that direct cytokine receptor—ionotropic glutamate receptor interactions may generally take place in MS due to the formation of specific cytokine-glutamate receptor heteromers upon the increased activation of the cytokine receptors by their ligands formed in the neuroinflammatory process in MS. This may enhance the neurodegeneration process to which also the formation of chemokine receptor containing GPCR heteromers may contribute by indirectly increasing glutamate neurotoxicity. A novel treatment strategy of MS to help counteract the appearance of the relapsing-remitting type of MS and supplement the present treatment with corticosteroids and type-1 interferons may therefore be to target such receptor heteromers in drug development. A combined treatment with specific cytokine and glutamate receptor antagonists targeting these receptor heteromers allowing low doses to be used may counteract the development of glutamate excitotoxicity and thus reduce disease progression in MS. Our opinion also suggests evolutionary conserved leucine-rich motifs as potential therapeutic targets to prevent incorrect dimerization of receptors in MS.
References
AGGRESCAN (2008) Prediction of “hot spots” of aggregation in polypeptides. http://bioinf.uab.es/aggrescan/
Agnati LF, Fuxe KG, Goncharova LB, Tarakanov AO (2008) Receptor mosaics of neural and immune communication: possible implications for basal ganglia functions. Brain Res Rev 58:400–414
Aguirre JA et al (2008) The novel cyclooxygenase-2 inhibitor GW637185X protects against MPTP-toxicity. NeuroReport 19:657–660
Bell JK et al (2005) The molecular structure of the Toll-like receptor 3 ligand-binding domain. Proc Natl Acad Sci USA 102:10976–10980
Block ML, Zecca L, Hong J-S (2007) Microglia-mediated neurotoxicity: uncovering the molecular mechanisms. Nat Rev Neurosci 8:57–59
Boggild M (2006) Rationale and experience with combination therapies in multiple sclerosis. J Neurol 253(Suppl 6):vi45–vi51
Conchillo-Sole O et al (2007) AGGRESCAN: a server for the prediction and evaluation of “hot spots” of aggregation in polypeptides. BMC Bioinformatics 8:65
El-Asmar L et al (2005) Evidence for negative binding cooperativity within CCR5–CCR2b heterodimers. Mol Pharmacol 67:460–469
Fernandez-Busquets X et al (2008) Recent structural and computational insights into conformational diseases. Curr Med Chem 15:1336–1349
Fuxe K et al (2007) Intramembrane receptor–receptor interactions: a novel principle in molecular medicine. J Neural Trans 114:49–75
Fuxe KG, Tarakanov AO, Goncharova LB, Agnati LF (2008) A new road to neuroinflammation in Parkinson’s disease? Brain Res Rev 58:453–458
Gay NJ, Gangloff M, Weber ANR (2006) Toll-like receptors as molecular switches. Nat Rev Immunol 6:693–698
Goncharova LB, Tarakanov AO (2007) Molecular networks of brain and immunity. Brain Res Rev 55:155–166
Goncharova LB, Tarakanov AO (2008a) Nanotubes at neural and immune synapses. Curr Med Chem 15:210–218
Goncharova LB, Tarakanov AO (2008b) Why chemokines are cytokines while their receptors are not cytokine ones? Curr Med Chem 15:1297–1304
Guyon A, Nahon J-L (2007) Multiple actions of the chemokine stromal cell-derived factor-1α on neuronal activity. J Mol Endocrinol 38:365–376
Hirono M, Yoshioka T, Konishi S (2001) GABA(B) receptor activation enhances mGluR-mediated responses at cerebellar excitatory synapses. Nat Neurosci 4:1207–1216
Matsushima N et al (2007) Comparative sequence analysis of leucine-rich repeats (LRRs) within vertebrate toll-like receptors. BMC Genomics 8:124–145
Mellado M et al (2001) Chemokine receptor homo or heterodomerization activates distinct signaling pathways. EMBO J 20:2497–2507
Mizuno T et al (2008) Interferon-γ directly induces neurotoxicity through a neuron specific, calcium-permeable complex of IFN-γ receptor and AMPA GluR1 receptor. FASEB J 22:1797–1806
NCBI (2008) National center for biotechnology information. http://www.ncbi.nlm.nih.gov
O’Brien K, Fitzgerald DC, Naiken K, Alugupalli KR, Rostami AM, Gran B (2008) Role of the innate immune system in autoimmune inflammatory demyelation. Curr Med Chem 15:1105–1115
PDB (2008) Protein data bank. http://www.rcsb.org/pdb
Percherancier Y et al (2005) Bioluminescence resonance energy transfer reveals ligand-induced conformational changes in CXCR4 homo and heterodimers. J Biol Chem 280:9895–9903
Pickering M, Cumiskey D, O’Connor JJ (2005) Actions of TNF-α on glutamatergic synaptic transmission in the central nervous system. Exp Physiol 90:663–670
Qiu Z, Sweeney DD, Netzeband JG, Gruol DL (1998) Chronic interleukin-6 alters NMDA receptor-mediated membrane responses and enhances neurotoxicity in developing CNS neurons. J Neurosci 18:10445–10456
Radons J et al (2003) The interleukin 1 (IL-1) receptor accessory protein Toll/IL-1 receptor domain. J Biol Chem 278:49145–49153
Rodriguez-Frade JM, Mellado M, Martinez AC (2001) Chemokine receptor dimerization: two are better than one. Trends Immunol 22:612–617
Springael JY et al (2006) Allosteric modulation of binding properties between units of chemokine receptor homo- and hetero-oligomers. Mol Pharmacol 69:1652–1661
Takahashi Y (2008) Epitope of autoantibodies to N-methyl-d-asparate receptor heteromers in paraneoplastic limbic encephalitis. Ann Neurol 64:110–111
Takahashi Y et al (2003) Autoantibodies to NMDA receptor in patients with chronic forms of epilepsia partialis continua. Neurol 61:891–896
Takeuchi H et al (2006) Tumor necrosis factor-α induces neurotoxicity via glutamate release from hemichannels of activated microglia in an autocrine manner. J Biol Chem 281:21362–21368
Uings IJ, Farrow SN (2000) Cell receptors and cell signalling. J Clin Pathol Mol Pathol 53:295–299
Vila-Coro AJ et al (1999) The chemokine SDF-1alpha triggers CXCR4 receptor dimerization and activates the JAK/STAT pathway. FASEB J 13:1699–1710
Viviani B et al (2003) Interleukin-1beta enhances NMDA receptor-mediated intracellular calcium increase through activation of the Src family of kinases. J Neurosci 23:8692–8700
Watovich SS et al (1996) Cytokine receptor signal transduction and the control of hematopoietic cell development. Annu Rev Cell Dev Biol 12:91–128
Xu Y et al (2000) Structural basis for signal transduction by the Toll/interleukin-1 receptor domains. Nature 408:111–115
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tarakanov, A.O., Fuxe, K.G., Agnati, L.F. et al. Possible role of receptor heteromers in multiple sclerosis. J Neural Transm 116, 989–994 (2009). https://doi.org/10.1007/s00702-009-0197-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-009-0197-x