Abstract
Introduction
There is a clinical equipoise between burr hole drainage (BHD) or twist drill craniotomy (TDC) as initial surgical intervention in patients with chronic subdural hematoma (cSDH). Moreover, the impact of type of postoperative drainage is not well elucidated. We performed a systematic review and meta-analysis comparing outcomes following BHD and TDC for initial surgical management in cSDH and to understand the impact of negative suction drainage with TDC.
Methods
A literature search was conducted according to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines for studies that directly compared TDC and BHD. The following outcomes were compared between TDC and BHD: mortality, recurrence, reoperations, complications, and cure rates. Subgroup analysis was performed to determine impact of negative suction drainage with TDC.
Results
Sixteen articles (n = 1,235; TDC: 663; BHD: 591) met inclusion criteria. Although complications (OR: 0.68, 95% CI: 0.38–1.23, p = 0.21; I2 = 31%), recurrence (OR: 1.16, 95% CI: 0.84–1.62, p = 0.37; I2 = 28%), cure (OR: 1.11, 95% CI: 0.72–1.72, p = 0.64, I2 = 34%), and mortality rates (OR: 1.20, 95% CI: 0.60–2.41; p = 0.61; I2 = 0%) were not significantly different between the two groups, TDC was associated with a higher reoperations than BHD (OR: 1.48, 95% CI:1.01–2.16, p = 0.04; I2 = 41%). Subgroup analysis demonstrated that TDC with negative suction drainage conferred equivalent reoperation rates as BHD (OR: 0.75, 95% CI: 0.24–2.35; p = 0.62; I2 = 65%); however, TDC without negative suction was associated with higher reoperations (OR: 1.62, 95% CI: 1.08–2.42; p = 0.02; I2 = 40%).
Conclusion
A systematic review and meta-analysis of available literature directly comparing TDC and BHD for primary evacuation of cSDH did not demonstrate clear superiority of either technique, although reoperations may be higher following TDC. Use of negative suction drainage with TDC may lead to similar rates of reoperation as BHD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic subdural hematoma (cSDH) is a common neurological disease, with an overall population incidence ranging from 1.72 to 20.6 per 100,000 persons per year and an even higher incidence in the elderly. [24, 36] Morbidity and mortality in patients with cSDH may range anywhere between 0–25 and 0–32%, respectively. [7] Neurological outcomes are often poor in up to 20% of patients, resulting in significant disability. [3] Although surgical evacuation is the mainstay of treatment in symptomatic cases, consensus for an optimal surgical strategy is commonly debated. [36] Perioperative mortality may range anywhere between 1.2 and 11%; a common complication is reaccumulation which may be as high as 70%, although reaccumulation requiring reoperation is usually only 10–20%. [3, 6, 9, 13, 16, 20, 30]
Being less invasive, burr hole drainage (BHD) and twist drill craniostomy (TDC) are commonly utilized for initial hematoma evacuation, with open craniotomy reserved as a second-line surgical strategy. Although TDC offers advantages such as being minimally invasive and able to be performed at the bedside which may be helpful in elderly patients with comorbidities, BHC is traditionally preferred and more commonly performed due to some evidence of superior safety and efficacy [33]. However, recent evidence-based systematic reviews by Ducruet et al. [6] and Almenawer et al. [1] have brought TDC back into the fold, demonstrating non-inferiority in morbidity, mortality, and recurrence rates. Due to variability in TDC technique and availability of more studies directly comparing outcomes between the two approaches, an updated comparison is warranted. Also, the impact of the type of subdural drainage utilized with TDC has not been well elucidated. In this study, we performed an updated systematic review and meta-analysis comparing outcomes following BHD and TDC for initial surgical management in patients with cSDH. We further aimed to compare any difference in outcomes between BHD and TDC based on the type of drainage system used with TDC. Our working hypothesis was that a negative suction drainage system would lead to equivalence in outcomes between TDC and BHD, while BHD would be superior to TDC with conventional closed drainage.
Methods
Literature search strategy and selection criteria
This systematic review was conducted in accordance with PRISMA (Preferred Reporting Items for Systematic Review and Meta-analysis) guidelines [19]. The literature search strategy was designed around the PICO format: Is there a difference in surgical outcomes (outcome) between patients undergoing TDC (intervention) and BHD (comparator) among patients with cSDH (population of interest)? A detailed electronic search using Ovid Medline/PubMed, Ovid Embase, Ovid Scopus and Cochrane Central Register of Controlled Trials, and Cochrane Database of Systematic Reviews was performed using keywords “Chronic Subdural Hematoma” or “Subdural Hematoma” or “Subdural Hemorrhage” or “Subdural Bleeding,” “ Burr Hole” or “Twist Drill” or “ Burr Hole” and “Twist Drill,” or “Craniotomy” or “Craniectomy” or “Craniostomy” or “Evacuation” or “Evacuation” or “Trepan” or “Trephine,” from their dates of inception to August 14, 2020. The search strategy was designed by a master’s level librarian with input from the study’s principal investigator (Supplement 1 ). Title and abstract screening followed by full-text evaluation was performed independently by two study co-authors (K.Y. and A.G.). The following were used as inclusion criteria: (1) cohort studies or clinical trials directly comparing outcomes following primary TDC and BHD among patients with cSDH and (2) studies reporting one or more of the following outcomes following drainage: mortality, morbidity (complications), reoperations, cure, and recurrence rates. Studies using non-human species, case reports or series with ≤ 5 patients, reviews, and letters to the editor were excluded.
Definition of TDC and BHD
Twist drill craniostomy was defined as a percutaneous bedside procedure performed with a hand-held manual twist drill to create a bony opening for evacuation. In the TDC arm, the size of the opening is usually < 1 cm. [5, 10, 11, 17, 21, 23, 26, 27, 31] Burr hole drainage was defined as drainage with wider openings (of size ≥ 1 cm) created with larger operating room drills.
Outcomes of interest
Morbidity was defined as any complication with the exception of recurrence. Mortality was defined as death during or following surgery. Both mortality and morbidity were determined from time of surgery to last follow-up (although length of follow-up was variable, with minimum being 2–4 weeks). All hematoma reaccumulations were defined as recurrence, while reoperations were specifically defined as only those reaccumulations that warranted further evacuation due to symptoms or clinical worsening. Cure was defined as attainment of full autonomy at last follow-up (grade 0 or 1 in Markwalder [18] classification or grade 5 on Glasgow Coma Scale [14]).
Data extraction and critical appraisal
In addition to above mentioned outcomes, the following data were extracted from included studies: author, year of publication, study design (prospective or retrospective, observational study vs clinical trial), country, number of institutions and surgeons, surgical technique for TDC and BHD (size of needle or port system, type of anesthesia, drainage system, etc.), number of patients, mean age of the cohort, sex distribution, and follow-up period. Risk of bias was evaluated using the Newcastle–Ottawa Scale (NOS) for observational studies and Cochrane Risk-of-bias tool for randomized controlled trials. [12, 22] Publication bias was determined using funnel plots. The grade of recommendation, assessment, development, and evaluation (GRADE) approach was used to assess limitations in study design, consistency, evidence directness, the precision of results, and publication bias. [2] The GRADEpro guideline development tool was used to create a summary of findings (SoF) table (http://gradepro.org/).
Statistical analysis
All data analyses were performed using Review Manager 5.4.1. Odds ratios (ORs) were used to pool effect estimates for binary outcomes using the Mantel–Haenszel summary statistics and the results visualized as forest plots. Heterogeneity was estimated using the I2 statistic, with substantial heterogeneity defined as I2 > 50%. A fixed-effects model was applied with I2 < 50%. Based on the type of drainage system utilized with TDC (negative suction vs other closed drainage system), we introduced subgroups to assess variation in effect size between TDC and BHD. All p-values were 2-sided with statistical significance defined as p ≤ 0.05.
Results
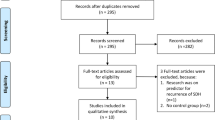
A total of 675 results were obtained from the initial electronic search. Following initial title, abstract screening, and full-text evaluation, 4 RCTs [10, 11, 21, 33] and 12 observational studies [4, 5, 8, 15, 17, 23, 25,26,27, 29, 31, 35] with a total of 1235 patients (TDC: n = 663; BHD: n = 591) were included for qualitative and quantitative comparison. Figure 1 demonstrates the PRISMA search strategy. Follow-up was variable and ranged between 2 weeks and 2 years. The mean (SD) age for TDC and BHD cohorts was 69 (5.5) and 67 (5.4) years, respectively. Study characteristics are presented in Tables 1, 2, 3. Within the TDC group, mean (± SD) duration of drainage was 2.6 ± 0.8 days (13 studies, n = 544) vs 2.5 ± 1.2 days for BHD (12 studies, n = 407). Size of bone opening ranged from 3 to 5.8 mm for TDC (9 studies, n = 323) vs 10 to 25 mm for BHD. Two studies (n = 88) reported using a negative suction drainage system in the TDC arm, [21, 26] while passive drainage was utilized with BHD across all studies. Nine studies (n = 490) reported on use of active irrigation with TDC, of which 6 (n = 336) reported it to be used as part of their protocol, while 3 studies (n = 154) reported it as not being used. For the BHD cohort, use of active irrigation was reported by 11 studies, of which 10 (n = 347) reported it as part of the protocol, while 1 study (n = 18) reported it to be not used. Ten studies (n = 362) reported using single burr hole in the BHD arm, and two (n = 107) reported using double burr holes, while two studies (n = 77) failed to clarify usage of single or double burr hole technique. Two reported (n = 45) usage of both single or double burr hole techniques used in BHD arm.
Mortality
Following analysis of 9 studies (n = 558; 249 in TDC and 309 in BHD), we did not observe a statistically significant difference in mortality between TDC and BHD (OR: 1.20, 95% CI: 0.60–2.41; p = 0.61; I2 = 0%) (Fig. 2A).
Subgroup analysis for usage of negative suction with TDC did not reveal any statistically significant differences in mortality for the two subgroups (negative suction: OR: 1.05, 95% CI: 0.20–5.50; p = 0.96; I2 = 0%; closed drainage: OR: 1.24, 95% CI: 0.57–2.66; p = 0.59; I2 = 0%).
Meta-analysis of 4 RCTs (n = 196; 100 in TDC and 96 in BHD) did not demonstrate a statistically significant difference in mortality between TDC and BHD (OR: 0.81, 95% CI: 0.27–2.41; p = 0.70; I2 = 0%) (Fig. 4A).
Complications
From an analysis of 8 studies (n = 576; 279 in TDC and 297 in BHD), we did not observe a statistically significant difference in overall recurrence (OR: 0.68, 95% CI: 0.38–1.23, p = 0.21; I2 = 31%) (Fig. 2B).
Cure rate
From an analysis of 12 studies (n = 940; 530 in TDC and 410 in BHD), we did not observe a statistically significant difference in overall cure rate (OR: 0.99, 95% CI: 0.66–1.49, p = 0.98, I2 = 35%) (Fig. 2C).
Meta-analysis of 4 RCTs (n = 196; 100 in TDC and 96 in BHD) did not demonstrate a statistically significant difference in between TDC and BHD (OR: 1.34, 95% CI: 0.64–2.79; p = 0.44; I2 = 47%) (Fig. 4B).
Recurrence
From an analysis of 16 studies (n = 1235; 663 in TDC and 591 in BHD), we did not observe a statistically significant difference in overall recurrence (OR: 1.16, 95% CI: 0.84–1.62, p = 0.37; I2 = 28%) (Fig. 3A).
Further subgroup analysis confirmed these findings and did not reveal any statistically significant differences in outcomes for the two subgroups (negative suction: OR: 0.64, 95% CI: 0.21–1.99; p = 0.44; I2 = 54%; closed drainage: OR: 1.23, 95% CI: 0.87–1.75; p = 0.24; I2 = 28%).
Meta-analysis of 4 RCTs (n = 196; 100 in TDC and 96 in BHD) did not demonstrate a statistically significant difference in recurrence between TDC and BHD (OR: 0.89, 95% CI: 0.40–1.98; p = 0.77; I2 = 17%) (Fig. 4C).
Reoperations
From an analysis of 14 studies (n = 1012; 499 in TDC and 532 in BHD), TDC was associated with a slightly higher rate of reoperations performed for reaccumulation as compared to BHD (16.23% vs 11.46%; OR: 1.48, 95% CI: 1.01–2.16, p = 0.04; I2 = 41%) (Fig. 3B).
Further, subgroup analysis revealed that the reoperation rate was similar between TDC with negative suction and BHD (OR: 0.75, 95% CI: 0.24–2.35; p = 0.62; I2 = 65%) but was significantly higher for TDC without negative suction when compared to burr hole drainage (OR: 1.62, 95% CI: 1.08–2.42; p = 0.02; I2 = 40%).
Meta-analysis of 4 RCTs (n = 196; 100 in TDC and 96 in BHD) did not demonstrate a statistically significant difference in reoperations between TDC and BHD (OR: 0.78, 95% CI: 0.32–1.90; p = 0.59; I2 = 32%) (Fig. 4D).
Critical appraisal
Study quality assessment using the Newcastle–Ottawa Scale (NOS) revealed high quality/low risk of bias for most observational studies with the exception of two studies which were of moderate quality. A low risk of bias was found for RCTs using the Cochrane tool (Supplement 2, Tables 1–2). Funnel plots were generated for publication bias, and no apparent asymmetry was found on visual inspection. Strength of evidence, assessed using the GRADE approach, was low for recurrence and cure and very low for mortality, reoperation, and complication. The GRADE summary of findings are summarized in Table 4.
Discussion
The present systematic review and meta-analysis did not demonstrate a significantly different outcome profiles between TDC and BHD, with the exception of a possibly higher reoperation rate with TDC. A higher complication rate was observed with BHD, but this was not found to be statistically significant. As opposed to previously conducted meta-analyses, it is important to note that only studies with direct comparisons were included in our study and subgroup analysis was performed to determine the effect of type of postoperative drainage. [1, 6] Further, only primary evacuations were included, and efficacy for drainage of recurrent hematomas was not evaluated. While the overall rate of recurrence was not significantly different, reaccumulations requiring reoperation as perceived by the groups reporting their results were higher with TDC. These findings point to the possible existence of a potential trade-off between inadequate drainage and greater surgical invasiveness, as determined by the size of the bone opening. Previous meta-analyses by Almenawer et al. and Teles et al. have suggested that drain usage following evacuation was associated with a significantly lower recurrence rate. [1, 28] Recurrence was also found to be lower with the utilization of a two-burr hole technique as opposed to a single burr hole. [19] Therefore, an adequate decompression supplemented with postoperative drainage may be the cornerstone of a good clinical outcome, as opposed to choice between different surgical techniques, which may be dictated by patient age, baseline functional status, and comorbidities. Another postulated reason for higher recurrence with TDC or single burr hole drainage is suggested to be challenges with drainage of multiloculated cSDH. [6]
Although the overall results demonstrated a higher rate of re-evacuation with TDC, subgroup analysis demonstrated that TDC with negative suction was associated with similar reoperation rates as BHD. Therefore, given that TDC may be performed at the bedside as opposed to BHD and may offer similar outcomes when used with negative suction, it may be a reasonable option to consider for elderly patients with comorbidities who may be less suitable surgical candidates. For the same reason, it may also be important to consider from a cost-saving perspective. With the exception of recurrence requiring reoperation, our findings are consistent with findings from previous meta-analyses by Almenawer et al. and Ducruet et al. which demonstrated no significant difference in outcomes such as mortality, morbidity, cure, and recurrence (reaccumulation) rates following BHD or TDC for cSDH evacuation. [1, 6] However, a systematic review published in 2003 that pooled data indirectly from 48 studies followed by a decision analysis study also suggested a higher recurrence rate with percutaneous drainage, which is consistent with our findings. [32]
The lack of uniform outcomes reporting in patients undergoing surgical evacuation of cSDH is important to consider. [34] For instance, many studies within our meta-analysis defined recurrence as a clinically significant hematoma reaccumulation that warranted re-evacuation [8, 10, 11, 17, 27, 29], while others measured any reaccumulations as a recurrence. [4, 5, 21, 23, 25, 26, 31, 33] Heterogeneity in outcomes reporting was also significant due to highly variable duration of postoperative follow-up ranging from 4 weeks to 4 years.
Limitations
There were some important limitations to the present systematic review and meta-analysis. Due to the observational nature of most included studies, we observed a low strength of evidence for all outcomes on GRADE evaluation. As mentioned previously, we observed heterogeneity in outcomes reporting, and all outcomes of interest were not reported consistently in all included studies. Many outcomes were also difficult to interpret due to the highly variable length of follow-up across studies. Hospital and procedure costs, as well as resource utilization, were not evaluated in included studies. It was also not possible to exclude the effect of heterogeneity in surgical technique on outcomes, as the size of TDC opening reported was also variable. Cure rates across studies were reported using multiple different functional assessment scales. In addition, given that this was a meta-analysis, the effect of confounders such as age, sex, anticoagulation, steroid use, and other comorbidities could not be adjusted via multivariable analysis. Only two studies (n = 88) reported usage of a negative suction device with TDC, which limits the strength and generalizability of findings obtained from subgroup analysis. Furthermore, we could not able to find studies reporting BHC with active drainage (negative suction) that fit in our inclusion criteria; therefore, we were not able to do BHC with active drainage vs TDC with or without active drainage subgroup meta-analysis.
Conclusion
An updated systematic review and meta-analysis of available literature directly comparing TDC and BHD for initial evacuation of cSDH did not demonstrate clear superiority of either technique, although reoperations may be higher following TDC. Usage of negative suction drainage with TDC may lead to similar rates of reoperation as BHD. Further improvement in TDC techniques may improve overall drainage and prevent clinically significant reaccumulation warranting reoperation.
Data availability
Supplemental data included.
Code availability
Not applicable.
References
Almenawer SA, Farrokhyar F, Hong C, Alhazzani W, Manoranjan B, Yarascavitch B et al (2014) Chronic subdural hematoma management: a systematic review and meta-analysis of 34,829 patients. Ann Surg 259:449–457. https://doi.org/10.1097/SLA.0000000000000255
Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S et al (2004) Grading quality of evidence and strength of recommendations. BMJ 328:1490. https://doi.org/10.1136/bmj.328.7454.1490
Balser D, Farooq S, Mehmood T, Reyes M, Samadani U (2015) Actual and projected incidence rates for chronic subdural hematomas in United States Veterans Administration and civilian populations. J Neurosurg 123:1209–1215. https://doi.org/10.3171/2014.9.JNS141550
Bhatty GB: Subdural haematoma: an evaluation of treatment methods. J Indian Med Assoc 94:7–10, 1996 Available: https://www.ncbi.nlm.nih.gov/pubmed/8776032.
Certo F, Maione M, Altieri R, Garozzo M, Toccaceli G, Peschillo S et al (2019) Pros and cons of a minimally invasive percutaneous subdural drainage system for evacuation of chronic subdural hematoma under local anesthesia. Clin Neurol Neurosurg 187:105559. https://doi.org/10.1016/j.clineuro.2019.105559
Ducruet AF, Grobelny BT, Zacharia BE, Hickman ZL, DeRosa PL, Andersen KN et al (2012) The surgical management of chronic subdural hematoma. Neurosurg Rev 35:155–69. https://doi.org/10.1007/s10143-011-0349-y (discussion 169)
Feghali J, Yang W, Huang J (2020) Updates in chronic subdural hematoma: epidemiology, etiology, pathogenesis, treatment, and outcome. World Neurosurg 141:339–345. https://doi.org/10.1016/j.wneu.2020.06.140
Garber S, McCaffrey J, Quigley EP, MacDonald JD (2016) Bedside treatment of chronic subdural hematoma: using radiographic characteristics to revisit the twist drill. J Neurol Surg A Cent Eur Neurosurg 77:233–238. https://doi.org/10.1055/s-0035-1570128
Gelabert-González M, Iglesias-Pais M, García-Allut A, Martínez-Rumbo R (2005) Chronic subdural haematoma: surgical treatment and outcome in 1000 cases. Clin Neurol Neurosurg 107:223–229. https://doi.org/10.1016/j.clineuro.2004.09.015
Gökmen M, Sucu HK, Ergin A, Gökmen A, Bezircio LuH (2008) Randomized comparative study of burr-hole craniostomy versus twist drill craniostomy; surgical management of unilateral hemispheric chronic subdural hematomas. Zentralbl Neurochir 69:129–133. https://doi.org/10.1055/s-2007-1004587
Goyal R, Nayak B, Maharshi R, Bidhar D, Panchal S, Pathak H (2018) Management of chronic subdural hematoma: burr hole versus twist drill – a prospective study. Asian Journal of Neurosurgery 13:319. https://doi.org/10.4103/ajns.ajns_99_16
Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928. https://doi.org/10.1136/bmj.d5928
Ivamoto HS, Lemos HP Jr, Atallah AN (2016) Surgical treatments for chronic subdural hematomas: a comprehensive systematic review. World Neurosurg 86:399–418. https://doi.org/10.1016/j.wneu.2015.10.025
Jennett B, Bond M: Assessment of outcome after severe brain damage: a practical scale. Lancet 305:480–484, 1975 Available: http://www.sciencedirect.com/science/article/pii/S0140673675928305.
Kim GH, Kim B-T, Im S-B, Hwang S-C, Jeong JH, Shin D-S (2014) Comparison of the Indications and treatment results of burr-hole drainage at the maximal thickness area versus twist-drill craniostomy at the pre-coronal point for the evacuation of symptomatic chronic subdural hematomas. J Korean Neurosurg Soc 56:243. https://doi.org/10.3340/jkns.2014.56.3.243
Kolias AG, Chari A, Santarius T, Hutchinson PJ (2014) Chronic subdural haematoma: modern management and emerging therapies. Nat Rev Neurol 10:570–578. https://doi.org/10.1038/nrneurol.2014.163
Lee S-J, Hwang S-C, Im SB (2016) Twist-drill or burr hole craniostomy for draining chronic subdural hematomas: how to choose it for chronic subdural hematoma drainage. Korean J Neurotrauma 12:107–111. https://doi.org/10.13004/kjnt.2016.12.2.107
Markwalder T-M, Steinsiepe KF, Rohner M, Reichenbach W, Markwalder H (1981) The course of chronic subdural hematomas after burr-hole craniostomy and closed-system drainage. J Neurosurg 55:390–396. https://doi.org/10.3171/jns.1981.55.3.0390
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2010) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 8:336–341. https://doi.org/10.1016/j.ijsu.2010.02.007
Mori K, Maeda M (2001) Surgical treatment of chronic subdural hematoma in 500 consecutive cases: clinical characteristics, surgical outcome, complications, and recurrence rate. Neurol Med Chir 41:371–381. https://doi.org/10.2176/nmc.41.371
Muzii VF, Bistazzoni S, Zalaffi A, Carangelo B, Others: Chronic subdural hematoma: comparison of two surgical techniques: preliminary results of a prospective randomized study/Comments. J Neurosurg Sci 49:41, 2005 Available: http://search.proquest.com/openview/81b23273a359f8b052e60765f8334f9e/1?pq-origsite=gscholar&cbl=49236.
Ottawa Hospital Research Institute: Available: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 22 January 2021
[PDF] A prospective comparative study of twist drill ..: Available: https://www.semanticscholar.org/paper/A-Prospective-Comparative-Study-of-Twist-Drill-Burr-Wang-Chen/ec66db560fc02cf113018205e1a5d41892d0f12b.
Rauhala M, Luoto TM, Huhtala H, Iverson GL, Niskakangas T, Öhman J, et al: The incidence of chronic subdural hematomas from 1990 to 2015 in a defined Finnish population. J Neurosurg:1–11, 2019 https://doi.org/10.3171/2018.12.JNS183035.
Ray Williams G, Baskaya MK, Menendez J, Polin R, Willis B, Nanda A: Burr-hole versus twist-drill drainage for theevacuation of chronic subdural haematoma:a comparison of clinical results. J Clin Neurosci 8:551–554, 2001 Available: http://www.sciencedirect.com/science/article/pii/S0967586800909263.
Rughani AI, Lin C, Dumont TM, Penar PL, Horgan MA, Tranmer BI (2010) A case-comparison study of the subdural evacuating port system in treating chronic subdural hematomas. J Neurosurg 113:609–614. https://doi.org/10.3171/2009.11.JNS091244
Smely C, Madlinger A, Scheremet R (1997) Chronic subdural haematoma ? a comparison of two different treatment modalities. Acta Neurochirurgica 139:818–826. https://doi.org/10.1007/bf01411399
Teles A, Falavigna A, Kraemer J (2016) Surgical treatment of chronic subdural hematoma: systematic review and meta-analysis of the literature. Arquivos Brasileiros de Neurocirurgia: Brazilian Neurosurgery 35:118–127. https://doi.org/10.1055/s-0035-1571270
Thavara BD, Kidangan GS, Rajagopalawarrier B (2019) Comparative study of single burr-hole craniostomy versus twist-drill craniostomy in patients with chronic subdural hematoma. Asian J Neurosurg 14:513–521. https://doi.org/10.4103/ajns.AJNS_37_19
Torihashi K, Sadamasa N, Yoshida K, Narumi O, Chin M, Yamagata S (2008) Independent predictors for recurrence of chronic subdural hematoma: a review of 343 consecutive surgical cases. Neurosurgery 63:1125–9. https://doi.org/10.1227/01.NEU.0000335782.60059.17 (discussion 1129)
Wang Q-F, Cheng C, You C (2016) A new modified twist drill craniostomy using a novel device to evacuate chronic subdural hematoma. Medicine 95:e3036. https://doi.org/10.1097/MD.0000000000003036
Weigel R (2003) Outcome of contemporary surgery for chronic subdural haematoma: evidence based review. J Neurol Neurosurg Psychiatry 74:937–943. https://doi.org/10.1136/jnnp.74.7.937
Xu C, Chen B, Xue L, Xia L, Yang X, Wei M, et al: Randomized controlled study on the curative effects of twist‑drill craniotomy and burr‑hole craniotomy in the treatment of chronic subdural hematoma. Exp Ther Med 16:959–965, 2018 Available: https://www.spandidos-publications.com/etm/16/2/959. Accessed 9 December 2020
Xu C-S, Lu M, Liu L-Y, Yao M-Y, Cheng G-L, Tian X-Y, et al: Chronic subdural hematoma management: clarifying the definitions of outcome measures to better understand treatment efficacy - a systematic review and meta-analysis. Eur Rev Med Pharmacol Sci 21:809–818, 2017 Available: https://www.ncbi.nlm.nih.gov/pubmed/28272701.
Xu M, Wang W-H, Zhu S-Q, Tan W-G, Jin X-G, Lu W et al (2020) Effects of minimally invasive approaches on chronic subdural hematoma by novel YL-1 puncture needle and burr-hole methods. Acta Neurol Belg 120:37–42. https://doi.org/10.1007/s13760-018-0914-z
Yang W, Huang J (2017) Chronic subdural hematoma: epidemiology and natural history. Neurosurg Clin N Am 28:205–210. https://doi.org/10.1016/j.nec.2016.11.002
Author information
Authors and Affiliations
Contributions
K.Y.: Conception and design, data collection, data analysis, and writing original draft.
A.G.: Conception and design, data collection, data analysis, and writing and revising original draft.
J.V.G.: Study supervision, revising, and approving final draft.
Corresponding authors
Ethics declarations
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Comments:
Chronic Subdural Hematoma (CSDH) is one of the most frequent neurosurgical diagnosis. Nevertheless, the optimal treatment regimen is yet to be defined. Twist-drill Craniostomy (TDC) and Burr-hole Drainage (BHD) are the two most frequently used surgical treatment techniques, with countless reports in literature as to the pros and cons of each of these. Nevertheless, there is currently no consensus as to which of these techniques is the superior.
I commend the authors for this systematic review and meta-analysis, providing solid data on the current evidence level in terms of BHD versus TDC in CSDH. Further, this work raises essential questions as to lack of evidence when it comes to the optimal drainage of patients with CSDH, highlighting the need for more research/evidence in the treatment of this patient category.
Jiri Bartek
Stockholm, Sweden
This publication describes a systematic review and meta-analysis of CSDH treatment using classical burr hole craniostomy vs twist drill technique. The study is methodologically sound and is a nicely performed study on a - for neurosurgeons - very important subject. It adds to the growing evidence that the way a CDSH is drained is less important as long as drainage is performed for a yet undetermined time period.
Frantz Poulsen
Denmark
This article is part of the Topical Collection on Brain trauma
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yagnik, K.J., Goyal, A. & Van Gompel, J.J. Twist drill craniostomy vs burr hole drainage of chronic subdural hematoma: a systematic review and meta-analysis. Acta Neurochir 163, 3229–3241 (2021). https://doi.org/10.1007/s00701-021-05019-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-021-05019-3