Abstract
Background
When superficial temporal artery-middle cerebral artery bypass is combined with indirect methods (e.g., revascularization surgery) to treat Moyamoya disease (MMD), antiplatelet treatment can impact bypass patency, infarction, or hemorrhage complications. Recently, heparin has been proposed as an anticoagulant treatment against white thrombus at the anastomosis site. The study aims to evaluate the effect of aspirin on the perioperative outcomes and investigate the results of heparin treatment for white thrombus.
Methods
This retrospective study included 74 procedures of combined revascularization surgery for MMD patients who either received or did not receive aspirin. Perioperative outcomes were compared between the two groups. In addition, the effects of heparin treatment for white thrombus were evaluated.
Results
The rate of white thrombus at the anastomosis site was significantly higher in the non-aspirin medication group (univariate: p = 0.032, multivariate: p = 0.044) and, accordingly, initial bypass patency was lower in the non-aspirin medication group (p = 0.049). Of the 17 patients with white thrombus development, five received heparin injections, and all white thrombi disappeared; however, there was one case of epidural hematoma and another of subdural hematoma. The risk of hemorrhagic complications was significantly higher in the surgical procedures that received heparin injections (p = 0.021).
Conclusions
In MMD patients who received combined revascularization surgery, aspirin medication lowered the occurrence of white thrombus. Heparin injections help to treat white thrombus but can enhance the risk of hemorrhagic complications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Moyamoya disease (MMD) is a rare cerebrovascular disease characterized by progressive stenosis of the internal carotid artery at its terminal portion and secondary formation of collateral vessels at the brain base. Pediatric patients usually present with ischemic symptoms, while adults suffer ischemic symptoms or intracranial hemorrhage. Superficial temporal artery (STA)-middle cerebral artery (MCA) bypass combined with various indirect methods (combined revascularization surgery) is widely performed to improve ischemic symptoms or prevent recurrence of intracerebral hemorrhage [2, 6, 9].
Antiplatelet treatment has been used in non-hemorrhagic MMD patients because it has been associated with good functional status on hospital admission [11], led to low recurrence of ischemic events in cases without cerebral misery perfusion [10], and reduced the potential risk of surgical complications [13]. Antiplatelet treatment may increase the risk of bleeding while decreasing the risk of thrombogenesis; it can thus influence perioperative outcomes of combined revascularization surgery, such as bypass patency, infarction, or hemorrhagic complications. However, the use of antiplatelet treatments varies among surgeons, clear guidelines remain unestablished [13, 16], and the influence of antiplatelet treatment on perioperative outcomes has not been fully elucidated.
Heparin intravenous injection during STA-MCA anastomoses might not be common, but in off-pump coronary artery bypass graft surgery, which is a similar procedure of arterial anastomosis, heparin is typically used to avoid clotting within the graft or attenuate the thrombin-mediated effect [5, 7, 12]. Recently, intravenous heparin injections have been proposed as a countermeasure against white thrombus, which sometimes occur at the anastomosis site during STA-MCA bypass in MMD patients (Fig. 1) [8]. Considering the novelty of this approach, its effects require further evaluation. Therefore, the current study aimed to evaluate the effects of aspirin on perioperative outcomes in MMD patients who underwent combined revascularization surgery and to investigate the influence of heparin on white thrombus.
Methods
Enrolled surgical procedures
From July 2014 to March 2020, 81 consecutive combined revascularization surgeries for MMD patients were performed in Nagoya University Hospital. MMD diagnosis was made according to guidelines proposed by the Ministry of Health and Welfare of Japan [14]. As for antiplatelet medication in the preoperative period, aspirin and cilostazol were used in 52 and seven surgical procedures, respectively. Cases with a full washout period for antiplatelet medication were considered as no antiplatelet treatment. None of the patients received either anticoagulant oral agents in preoperative periods or additional antiplatelet agents in the perioperative period. Because the mechanisms of action for aspirin and cilostazol are different, to assure accuracy in the evaluation of the antiplatelet treatment effect, we excluded seven cases who received cilostazol. Finally, 74 surgical procedures which received aspirin or no antiplatelet medication were retrospectively analyzed. A flow diagram of the enrolled surgical procedures is shown in Fig. 2.
Usage of aspirin medication and classification
The usage of aspirin medication was retrospectively reviewed. The initiation depended on the decisions of attending surgeons because of the absence of clear guidelines. Aspirin was administered at a dose of 100 mg per day for adult patients and at a decreased weight-dependent dose for pediatric patients.
The surgical procedures receiving aspirin medication in the preoperative period were classified as aspirin medication group. In addition, this group was classified into three subgroups based on the preoperative rest period: (1) continued aspirin medication even on surgery day, (2) stopped aspirin medication on surgery day, (3) stopped aspirin medication 3–4 days before surgery. In the postoperative period, aspirin was restarted 2 days after surgery in cases without hemorrhagic complications in head computed tomography images (CT).
Surgical procedures
Combined revascularization surgery for the MCA territory was performed. Specifically, single STA-MCA anastomosis was performed in an end-to-side fashion after a frontotemporal craniotomy to reveal the distal part of the Sylvian fissure. Bypass patency was evaluated by indocyanine green videoangiography or Doppler sound. Encephalo-duro-myo-synangiosis or encephalo-duro-myo-pericranial-synangiosis was performed for the indirect methods for the MCA territory. During general anesthesia, PaCo2 was maintained between 36 and 40 mmHg.
Rescue methods for white thrombus and heparin usage manner
When white thrombus developed at the anastomosis site and caused the bypass occlusion, we first tried mechanical tapping on the anastomosis site. In some cases where the white thrombus did not disappear after mechanical tapping, re-suture or heparin (Mochida Pharmaceutical, Co.) injection was performed. Between July 2014 and November 2018, we performed re-suture if possible, and between December 2018 and March 2020, we used heparin injection. For adult patients, heparin was first injected intravenously at a dose of 2000 units in a bolus; when the thrombus remained, an additional injection was performed. For pediatric patients, the dose was decreased in a weight-dependent manner.
Perioperative management
All patients were treated to avoid hypovolemia and anemia. Systolic blood pressure was maintained between 80 and 120% of the preoperative value, and fibrinogen was maintained over 200 mg/dl. For pediatric cases, to avoid severe crying, appropriate sedation using thiamylal sodium, diazepam, and/or dexmedetomidine were used for medical examination or medical procedures if necessary. CT was performed just after surgery and the day after. A 3.0-T or 1.5-T magnetic resonance imaging (MRI) including fluid-attenuated inversion recovery imaging, diffusion-weighted imaging, and MR angiography (MRA) was performed routinely 2–3 days after surgery. Additional CT or MRI was performed when patients showed neurological symptoms suspicious of infarction or hemorrhagic complications.
Evaluated outcomes and other variables
As baseline clinical characteristics, we collected the following parameters: sex, age, surgery side, stenosis or occlusion of the posterior cerebral artery (PCA involvement), hypertension, diabetes mellitus, hyperlipidemia, and symptoms for surgery. As potential outcomes were affected by the use of antiplatelets, we evaluated the following events: initial bypass patency (evaluated before the rescue methods for white thrombus), final bypass patency (evaluated after rescue methods for white thrombus), white thrombus development at the anastomosis site, perioperative infarction, and hemorrhagic complications. In addition, to investigate the effect of heparin injection, the disappearance of white thrombus and hemorrhagic complications was evaluated.
Statistical analysis
For group pair comparison, we used Fisher’s exact test for categorical variables and the t test for numerical variables. If appropriate, logistic regression analysis was employed to test the effect of multiple variables. Significance value was set at a p value < 0.05. Statistical analyses were performed in R 3.6.2 (R Foundation for Statistical Computing; https://www.r-project.org/).
Results
Effect of aspirin on perioperative outcomes
Baseline clinical characteristics, including sex, surgery side, PCA involvement, hypertension, diabetes mellitus, and hyperlipidemia, did not differ significantly between the aspirin and not-aspirin medication groups. In the aspirin medication group, the mean age was significantly smaller, and the rate of ischemic symptoms was higher (Table 1).
Comparing the perioperative outcomes between aspirin and not-aspirin medication groups, initial bypass patency was significantly lower in the non-aspirin medication group (p = 0.049). Similarly, rates of white thrombus development at the anastomosis site, which contribute to the initial bypass failure, were significantly higher in the non-aspirin medication group (p = 0.032). Final bypass patency, infarction, and hemorrhagic complications did not show significant differences (Table 2). Additionally, we investigated possible confounders with respect to white thrombus development (Table 3). Because PCA involvement also showed a significant association with white thrombus development (p = 0.002) in univariate analysis, we performed logistic regression analysis using these two explanatory variables. In multivariate analysis, both aspirin medication and PCA involvement showed significant correlations to white thrombus development (aspirin medication, p = 0.044; PCA involvement, p = 0.004).
As a supplementary analysis, we evaluated whether differences in preoperative rest periods of aspirin medication influenced the outcomes. Comparing the subgroups of aspirin medication, perioperative outcomes, including bypass patency, development of white thrombus, infarction, and hemorrhagic complications, did not significantly differ (Table 4).
Effect of heparin injections on white thrombus
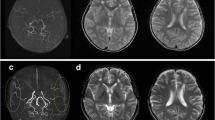
In 17 cases of the 74 surgical procedures, white thrombi developed at the anastomosis site. Results on the rescue methods are summarized in Table 5. Twelve cases received mechanical tapping and/or re-suture, but white thrombi remained in four cases. Five cases underwent tapping and heparin intravenous injection. White thrombi disappeared in all cases: four cases needed 2000 units heparin, while one needed 7000 units. However, in the five surgical procedures that received heparin injections, there was one case of epidural hematoma and another of subdural hematoma (Fig. 3). Neither patient received aspirin medication. In all enrolled surgical procedures, hemorrhagic complication rates were significantly higher in surgical procedures that received heparin injections (p = 0.021) in contrast to those with aspirin medication (Tables 6 and 7). Multivariate analysis was not applied because the number of heparin injections was small.
Postoperative images of computed tomography (CT) in cases with hemorrhagic complications. a A 48-year-old female who suffered from hemorrhagic Moyamoya disease (MMD) underwent combined revascularization surgery. She did not receive antiplatelet treatment preoperatively, but received a 7000-unit heparin injection for white thrombus treatment. Two days after surgery, her consciousness level declined, and CT showed thick acute subdural hematoma under the encephalo-duro-myo-synangiosis. Emergency craniotomy to remove the intracranial hematoma was needed, and after that, she recovered her consciousness level. b Thirteen-year-old female suffering from MMD-related headache underwent combined revascularization surgery. She did not receive antiplatelet treatment preoperatively, but received a 2000-unit heparin injection for white thrombus treatment. Just after surgery, she did not show any symptoms, but CT showed an acute epidural hematoma near the craniotomy area. A conservative treatment was initiated, which stopped hematoma growth
Discussion
We investigated the effects of aspirin medication and heparin injection on perioperative outcomes in MMD patients who underwent combined revascularization surgery. Use of aspirin before surgery lowered the occurrence of white thrombus, and PCA involvement was identified a risk factor for white thrombus. Our results show that while heparin intravenous injection might help to treat white thrombus at the anastomosis site, it may elevate the risk of hemorrhagic complications.
Both aspirin and heparin treatments were found to be useful in preventing white thrombus. The mechanism of the rapid development of white thrombus during the anastomosis procedure is considered as follows [1]. First, the incised arterial wall exposes collagen and tissue factors to blood flow, and collagen triggers platelet accumulation and activation. Meanwhile, tissue factors initiate thrombin generation, which converts fibrinogen to fibrin and activates platelets. Aspirin and heparin may prevent thrombus development by decreasing platelet function and blocking thrombin effects in this cascade. Referring to the literature on the risk of white thrombus, Mikami et al. reported that high MRA scores correlated with thrombus development [8]. The MRA score is higher in cases of PCA involvement [4]; thus, our result was consistent with the past report.
Heparin intravenous injection during revascularization surgery for MMD patients was significantly associated with hemorrhagic complications. This finding implies that the anticoagulant function of heparin outweighed the hemostatic effects of surgical procedures. During cardiac surgery using heparin intravenous injection, drains are placed in the pericardial, mediastinum, and pleural cavity for preventing hemorrhagic complications [3, 15]. However, in combined revascularization surgery, drains are generally not placed in the epidural or subdural space. Even if drains are placed, they will not remove bleeding effectively because an acute epidural or subdural hematoma is solid and requires a craniotomy. Therefore, the risk of hemorrhagic complications by heparin injection for white thrombus remains an outstanding issue, and other approaches are needed.
This study is subject to several limitations. First, age and symptom distribution differed between the aspirin and not-aspirin medication groups, which may have led to selection bias. This finding may be attributable to the tendency of ischemic patients to take aspirin medication and the differences in clinical presentation between pediatric and adult patients. Second, the rates of PCA involvement, aspirin medication, and symptom distribution differed between heparin and not-heparin-injected groups. However, these factors were not significantly associated with hemorrhagic complications in the present study, and also no previous report supported the hemorrhagic risk of these factors. Third, the level of platelet function affected by aspirin medication was not measured: aspirin resistance and its functional differences in the preoperative rest period were not quantitatively assessed. Lastly, the incidence of white thrombi in this study (23.0%) was relatively high. The development of white thrombi may be one of the main causes of bypass failure, and it also presented a challenge in this study. Identifying the causes or risk factors for developing white thrombi is important; however, only few reports have attempted to address this issue [8]. Although the causes underlying the high incidence of white thrombi have not been fully identified, the present study identified the factors for decreasing the rate of white thrombi or the treatment thereof.
Conclusions
In MMD patients who underwent combined revascularization surgery, use of aspirin medication resulted in a lower occurrence of white thrombus. Despite heparin injections having potential to treat white thrombus, they may elevate the risk of hemorrhagic complications.
Abbreviations
- CT:
-
Computed tomography
- ICH:
-
Intracranial hemorrhage
- MCA:
-
Middle cerebral artery
- MMD:
-
Moyamoya disease
- MRA:
-
Magnetic resonance angiography
- MRI:
-
Magnetic resonance imaging
- PCA:
-
Posterior cerebral artery
- SD:
-
Standard deviation
- STA:
-
Superficial temporal artery
- TIA:
-
Transient ischemic attack
References
Furie B, Furie BC (2008) Mechanisms of thrombus formation. N Engl J Med 359(9):938–949
Golby AJ, Marks MP, Thompson RC, Steinberg GK (1999) Direct and combined revascularization in pediatric moyamoya disease. Neurosurgery 45(1):50–60
Gozdek M, Pawliszak W, Hagner W, Zalewski P, Kowalewski J, Paparella D, Carrel T, Anisimowicz L, Kowalewski M (2017) Systematic review and meta-analysis of randomized controlled trials assessing safety and efficacy of posterior pericardial drainage in patients undergoing heart surgery. J Thorac Cardiovasc Surg 153(4):865-875.e12
Houkin K, Nakayama N, Kuroda S, Nonaka T, Shonai T, Yoshimoto T (2005) Novel magnetic resonance angiography stage grading for Moyamoya disease. Cerebrovasc Dis 20(5):347–354
Houlind K, Fenger-Grøn M, Holme SJ et al (2014) Graft patency after off-pump coronary artery bypass surgery is inferior even with identical heparinization protocols: results from the Danish On-pump Versus Off-pump Randomization Study (DOORS). J Thorac Cardiovasc Surg 148(5):1812-1819.e2
Kuroda S, Houkin K (2008) Moyamoya disease: current concepts and future perspectives. Lancet Neurol 7(11):1056–1066
Martorell L, Martínez-González J, Rodríguez C, Gentile M, Calvayrac O, Badimon L (2008) Thrombin and protease-activated receptors (PARs) in atherothrombosis. Thromb Haemost 99(2):305–315
Mikami T, Suzuki H, Ukai R, Komatsu K, Akiyama Y, Wanibuchi M, Houkin K, Mikuni N (2019) Predictive factors for acute thrombogenesis occurring immediately after bypass procedure for moyamoya disease. Neurosurg Rev:609–617
Miyamoto S, Yoshimoto T, Hashimoto N et al (2014) Effects of extracranial-intracranial bypass for patients with hemorrhagic moyamoya disease: results of the Japan adult moyamoya trial. Stroke 45(5):1415–1421
Miyoshi K, Chida K, Kobayashi M, Kubo Y, Yoshida K, Terasaki K, Ogasawara K (2019) Two-year clinical, cerebral hemodynamic, and cognitive outcomes of adult patients undergoing medication alone for symptomatically ischemic Moyamoya disease without cerebral misery perfusion: a prospective cohort study. Clin Neurosurg 84(6):1233–1241
Onozuka D, Hagihara A, Nishimura K et al (2016) Prehospital antiplatelet use and functional status on admission of patients with non-haemorrhagic moyamoya disease: a nationwide retrospective cohort study ( J-ASPECT study). BMJ Open. https://doi.org/10.1136/bmjopen-2015-009942
Paparella D, Semeraro F, Scrascia G, Galeone A, Ammollo CT, Kounakis G, de Luca Tupputi Schinosa L, Semeraro N, Colucci M (2010) Coagulation-fibrinolysis changes during off-pump bypass: effect of two heparin doses. Ann Thorac Surg 89(2):421–427
Rashad S, Fujimura M, Niizuma K, Endo H, Tominaga T (2016) Long-term follow-up of pediatric moyamoya disease treated by combined direct–indirect revascularization surgery: single institute experience with surgical and perioperative management. Neurosurg Rev 39(4):615–623
Research Committee on the Pathology and Treatment of Spontaneous Occlusion of the Circle of Willis (2012) Guidelines for diagnosis and treatment of Moyamoya disease (spontaneous occlusion of the circle of willis). Neurol Med Chir (Tokyo) 52(5):245–266
Roberts N, Boehm M, Bates M, Braidley PC, Cooper GJ, Spyt TJ (2006) Two-center prospective randomized controlled trial of Blake versus Portex drains after cardiac surgery. J Thorac Cardiovasc Surg 132(5):1042–1046
Zhao Y, Zhang Q, Zhang D, Zhao Y (2017) Effect of aspirin in postoperative management of adult ischemic Moyamoya disease. World Neurosurg 105:728–731
Author information
Authors and Affiliations
Contributions
Conceptualization: Fumiaki Kanamori, Yoshio Araki. Methodology: Fumiaki Kanamori, Kinya Yokoyama. Formal analysis and investigation: Fumiaki Kanamori, Kenji Uda, Takashi Mamiya, Masahiro Hishihori, Takashi Izumi. Writing—original draft preparation: Fumiaki Kanamori; Supervision: Sho Okamoro, Atsushi Natsume.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Institutional Review Board of the Nagoya University Graduate School of Medicine (No. 2016-0327).
Consent to participate/publish
Informed consent was obtained from all study participants or their legal guardians.
The participants provided informed consent regarding publishing their data and photographs.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Vascular Neurosurgery - Other
Rights and permissions
About this article
Cite this article
Kanamori, F., Araki, Y., Yokoyama, K. et al. Effects of aspirin and heparin treatment on perioperative outcomes in patients with Moyamoya disease. Acta Neurochir 163, 1485–1491 (2021). https://doi.org/10.1007/s00701-020-04668-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-020-04668-0