Abstract
Background
This study was designed to detect and assess the frequency and severity of nonmotor symptoms (NMSs) in advanced Parkinson’s disease (PD) and to investigate the effects of subthalamic nucleus deep brain stimulation (STN-DBS) on NMSs.
Methods
We developed an online PC–based questionnaire program to assess NMSs in PD. Twenty-six PD patients who underwent bilateral STN-DBS were assessed. The NMS questionnaire consisted of 54 NMSs in three categories, based on Witjas et al. (2002). For each NMS, the patients were asked whether or not it was present, whether or not the fluctuating manifestations correlated with the timing of levodopa-induced motor fluctuations, and how severe the NMS was. Patients were assessed by this system before surgery and at the follow-up visit, 3 to 6 months after surgery. At the postoperative assessment, patients were also assessed on preoperative NMSs using recall.
Results
The most frequent preoperative NMSs were constipation and visual disorders, while the most frequent postoperative NMSs were difficulty in memorizing and pollakiuria. The ranking of most frequent NMSs changed from before to after surgery. NMSs of drenching sweats, dysphagia, and constipation were significantly ameliorated, while NMSs of dyspnea and slowness of thinking were significantly deteriorated after surgery. The preoperative assessment by postoperative recall gave very different results from that of the preoperative assessment.
Conclusion
An online questionnaire system to assess NMSs in patients with advanced PD suggested that STN-DBS might influence the frequencies of some kinds of NMSs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parkinson’s disease (PD) is one of the most common neurodegenerative disorders, with a prevalence generally estimated at 0.3% of the population in industrialized countries [7]. It is the second most common neurodegenerative disorder after Alzheimer’s disease, and its prevalence increases with age, reaching 1% in people over 60 years of age [7]. One of the main pathological features of PD is the degeneration of dopaminergic neurons in the substantia nigra pars compacta (SNc), which gives rise to the four major motor symptoms of this disease: bradykinesia, tremor at rest, rigidity, and postural instability [8].
There are also many nonmotor symptoms (NMSs) that are common features of PD [11], such as dysautonomic, psychiatric and cognitive, and sensory symptoms [28, 29]. These problems, together with the chronic and progressive nature of the illness itself, may seriously hamper patients’ physical and mental health [6]. Similar to the motor symptoms of PD, NMSs significantly disable daily activity and negatively affect quality of life in PD patients. Some NMSs are alleviated by dopaminergic treatment. Subthalamic nucleus deep brain stimulation (STN-DBS) is a well-established surgical option for motor symptoms in PD patients [15]. This surgery dramatically alleviates the cardinal motor symptoms and allows for a reduction in antiparkinsonian drugs. There are some previous reports about the effects of STN-DBS on NMSs. In a study by Witjas et al. [29], STN-DBS was effective against NMSs such as drenching sweats, anxiety, fatigue, akathisia, and slowness of thinking. However, a rapid development of extreme apathy or abulia shortly after surgery was also described, especially in patients with very high doses of dopaminergic drugs that were drastically reduced after surgery [14]. Transient confusion has also been observed in some patients, possibly as a result of the long duration of brain surgery and the withdrawal of dopaminergic drugs [18]. In another study, night sleep was reported to improve in all patients [20]. However, because there are many types of NMSs, it can be very difficult to categorize and evaluate these types of symptoms. Some NMSs are subjective only, and other NMSs may be influenced by the effects of either STN-DBS or medication levels. To detect and evaluate NMSs in PD patients, we developed an online questionnaire system for NMSs. Compared with other reports of NMSs, this study is novel in that the questionnaire was conducted to investigate not only the presence and severity of symptoms, but also the onset of symptoms. An online system is useful because the acquired data can be categorized and anonymized, and multiple researchers can then use the data simultaneously. We used this system when speech-language-hearing therapists (STs) performed higher brain function tests both before and after surgery, and assessed the changing NMSs in PD patients after STN-DBS.
Methods and materials
We used the questionnaire proposed by Witjas et al. [28] because this classification includes many NMSs in detail in each category, and we wanted to cover as many NMSs as possible in our study. The NMS questionnaire consisted of 54 NMSs in three categories (26 dysautonomic, 21 psychiatric/cognitive, and 7 sensory symptoms), and was used with some modifications to adapt the questionnaire to the Japanese language. For the patients’ comfort, the questionnaire was completed during “on-time” (on-drug condition preoperatively, and on-stimulation and on-drug conditions postoperatively). The initial postoperative DBS programming in all patients was performed using unipolar stimulation of the contact located at the dorsal STN. The stimulation parameters were reevaluated and adjusted as required during hospital visits to achieve maximal therapeutic effect against Parkinson’s disease symptoms.
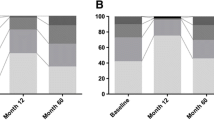
The questionnaire program was administrated on a PC to reduce the burden on patients and raters, to shorten the interview time, and to ensure the same questionnaire for all symptoms. The questionnaire program ran on a web browser and had graphical interfaces (Fig. 1). The patients were able to select the answer of the question by clicking on it, and their data were encrypted and password-locked to protect personal data. Figure 1 a shows the start page. On the second page (Fig. 1b), for each NMS, patients were asked if the symptom was present or absent. On the third page (Fig. 1c), for each NMS, patients were asked whether the fluctuating manifestations were correlated with the timing of “just before on-drug” (“just before on-time”), “on-drug” (“on-time”), “just before off-drug” (“just before off-time”), “off-drug” (“off-time”), “dyskinetic state,” or “unrelated to either on- or off-drug” (“on/off-unrelated time”). Before the questionnaire began, the definitions of “on,” “off,” and “dyskinetic state” were explained to patients. At the end of each NMS questionnaire (Fig. 1d), the patients were asked to rate the severity of each NMS with a scale ranging from 0 to 4 (0: no discomfort, 1: slight, 2: moderate, 3: marked, 4: maximum disability).
The online questionnaire program system. The questionnaire program was administrated on a PC and ran on a web browser. It had graphical interfaces, and patients were able to select the answer to the question by clicking on it. a Start page. b Second page: the patients were asked if each NMS was present or absent. c Third page: for each NMS, the patients were asked whether the fluctuating manifestations correlated with the timing of “just before on-drug” (“just before on-time”), “on-drug” (“on-time”), “just before off-drug” (“just before off-time”), “off-drug” (“off-time”), “dyskinetic state,” or not with motor symptoms (“on/off-unrelated time”). d Last page: the patients were asked to rate the severity of each NMS on a scale ranging from 0 to 4 (0: no discomfort, 1: slight, 2: moderate, 3: marked, 4: maximum disability
Twenty-six PD patients (seven men and nineteen women) who underwent bilateral STN-DBS in Kyushu University Hospital between June 2006 and May 2010 were assessed by this program. All patients were assessed before and after surgery and gave written informed consent for the collection and publication of their data. All experimental procedures were approved by the Ethics Committee of the Kyushu University Hospital. Inclusion criteria were responsiveness to levodopa and disabling motor fluctuations and/or levodopa-induced dyskinesia that was refractory to the adjustment of antiparkinsonian medication. Exclusion criteria were atypical parkinsonism, noticeable brain atrophy, age (> 75 years), dementia (MMSE < 20), or unstable psychiatric impairments. Subjects underwent contemporaneous bilateral STN-DBS implantation using MRI-guided indirect targeting and a multitrack microrecording method [32]. Using our online questionnaire, we investigated which symptoms were ranked highest before and after surgery, and the changes in severity of each NMS. The severity of symptoms in each parameter was evaluated using five levels (from 0 to 4) both before surgery and at 3 to 6 months after surgery. Statistical analysis was performed using a Wilcoxon signed-rank test to determine the relative difference between the preoperative and postoperative states. We used correlation coefficients and regression analysis to measure the strengths of the relationships between LEDD reduction after surgery and symptom improvement or worsening. P values < 0.05 were considered significant. We interpreted correlation coefficient sizes as follows: 0.0 ≤ |r| < 0.2: almost no correlation; 0.2 ≤ |r| < 0.4: weak correlation; 0.4 ≤ |r| < 0.7: moderately strong correlation; and 0.7 ≤ |r| ≤ 1.0: strong correlation. At the postoperative examination, patients were asked to recall which symptoms existed before surgery. In the recall study, one case was excluded because of insufficient data (n = 25). Patients also completed the unified Parkinson’s disease rating scale (UPDRS) with activity of daily living score (UPDRS part II) and motor score (UPDRS part III), and the Mini-Mental State Examination (MMSE), both before and after surgery. The levodopa-equivalent daily dose (LEDD) was calculated according to the conversion formula proposed by Tomlinson et al. [26]
Results
Mean patient age was 61.9 years, mean age at disease onset was 48.3 years, and mean disease duration was 13.7 years. The maximum age of the patients was 74 years and the lowest MMSE score was 21. The mean interview duration was 20 min. Using an online questionnaire program, all patients were able to answer questions without any problems. Table 1 summarizes patient profiles and surgical outcomes. All patients had some NMSs. After surgery, UPDRS part II and III scores in “off-time” significantly improved by 64% and 74%, respectively (p < 0.01). In addition, the LEDD and LDD (levodopa daily dose) were significantly reduced by 59.3% and 70.0%, respectively (p < 0.01). Table 2 gives the ten most frequent NMSs. Preoperatively, the most frequent NMSs were constipation (88%), visual disorders (69%), flatulence (65%), and difficulty in memorizing (65%), which all fall into the categories of dysautonomic or psychiatric and cognitive symptoms. Postoperatively, the most frequent NMSs were difficulty in memorizing (58%), pollakiuria (46%), visual disorders (42%), oral dryness (38%), flatulence (38%), anxiety (38%), irritability (38%), and slowness of thinking (38%). These also fall into the categories of dysautonomic or psychiatric and cognitive symptoms. There were no sensory symptoms in the top 10 most frequent preoperative and postoperative NMSs.
Next, we investigated the changes in severity of each NMS after surgery in the “off-time” and “on/off-unrelated time.” NMSs in the “just before on-time,” “on-time,” “just before off-time,” and “dyskinetic state” were excluded because they were very rarely reported. The NMSs that were ameliorated or deteriorated in the postoperative state were examined further. Tables 3, 4, and 5 show the p values for postoperative changes in severity in three categories (Table 3: dysautonomic symptoms; Table 4: psychiatric and cognitive symptoms; Table 5: sensory symptoms). In the dysautonomic symptom category in Table 3, drenching sweats (p = 0.026) and dysphagia (p = 0.031) during “off-time,” and constipation (p = 0.010) during “on/off-unrelated time,” were ameliorated following STN-DBS. In contrast, dyspnea (p = 0.032) during “on/off-unrelated time” was deteriorated postoperatively. For psychiatric and cognitive symptoms (Table 4), only slowness of thinking (p = 0.029) was significantly deteriorated during “on/off-unrelated time.” No sensory symptoms showed significant changes between preoperative and postoperative states (Table 5). From the correlation analysis between LEDD reduction after surgery and the improvement or worsening of symptoms, “dysphagia” was weakly correlated with LEDD reduction after surgery, but this result did not reach statistical significance (r = 0.384, p = 0.052). No other symptoms showed any correlation with LEDD reduction after surgery.
Table 6 shows the reported preoperative NMSs before and after surgery. Table 6 (A) gives the 10 most frequent preoperative NMSs by recall after surgery, while Table 6 (B) shows the top 10 preoperative NMSs that the patients stated they did not have when asked to recall preoperative NMSs after surgery. Pollakiuria (36%), flatulence (32%), facial flushing (28%), and constipation (28%) were the top-ranked symptoms in Table 6 (B). Moreover, many dysautonomic NMSs were ranked highly. Table 6 (C) shows the top 10 NMSs that the patients reported as preoperative symptoms by recall after surgery, but that they did not report before surgery. Drenching sweats (32%), fatigue (32%), akathisia (32%), and mental hyperactivity (28%) were ranked top in Table 6 (C). Some sensory and psychiatric and cognitive symptoms were ranked highly here, as well as dysautonomic symptoms. Importantly, the results were quite different depending on the time of evaluation; that is, preoperative NMSs reported by recall after surgery were quite different from the preoperative NMSs that were reported prior to surgery.
Discussion
Regarding the development of an online questionnaire program for NMSs, two points should be noted. The first point is that recall is not reliable; our results were quite different depending on the timing of the evaluation. Reporting of NMSs in PD is easily influenced by feelings at the timing of the questionnaire. In Table 6, the preoperative NMSs are completely different from those that were recalled postoperatively. It is therefore impossible to obtain accurate results if patients are not assessed preoperatively. The second point is that a long examination time might exhaust patients [12]. Our interview system addressed this point by enabling us to relatively easily evaluate NMSs in PD patients with minimum stress for the subjects involved. However, because the preoperative questionnaire was completed during “on-time,” the “on” medication state might have meant that patients were more optimistic (or hypomanic), and this may have affected or compromised the subjective evaluation of NMSs.
Several questionnaires have been developed for the assessment of NMSs observed in PD, including the nonmotor symptom scale (NMSS) [4], NMSQuest [3, 19], and PDQ-39 [21]. Our questionnaire system had a graphical interface, meaning that even older patients and hearing-impaired patients could operate the program, and the mean duration for the interview was only 20 min. In the present study, STs used this system to efficiently assess NMSs, but we believe that accurate test results can be obtained even if this system is used by clinicians and other medical staff who do not regularly perform this kind of questionnaire. There is, however, one potential problem when considering the generalization of this questionnaire: the meaning of words may change depending on the language that is used. Translating questions into different languages may affect the results of the study. Although we referred to Witjas et al. [28, 29] in this study, it may not have always been possible to ask questions with exactly the same nuances, because we did not verify the back translations of the questions. It is therefore not appropriate to directly compare the results of the current study with the results of studies by Witjas et al.
With regard to the results from the present study, there is also a possibility that STN-DBS influences NMSs. In Table 2, there is a difference between the highest ranked NMSs before and after surgery. There are two possible factors that may influence changes in NMSs after an STN-DBS operation. One is that STN-DBS directly influences NMSs, and the other is that the reduction in LEDD, caused by the positive effects of STN-DBS on motor symptoms, has a modulatory effect on NMSs. The aforementioned reports suggest that STN-DBS affects some parts of NMSs, but it is not clear whether symptom changes are a direct or indirect effect of chronic stimulation of the STN. Our study had similar findings to a previous study by Witjas [29] in that the most frequent preoperative NMSs were anxiety, slowness of thinking, and irritability, and that many dysautonomic NMSs, especially drenching sweats, were markedly improved by STN-DBS. In addition, to ensure the reliability of results, it was necessary to ask patients to evaluate their symptoms at the present time, and not to recall symptoms that existed at a previous time point.
In the current study, drenching sweats and dysphagia during “off-time” and constipation during “on/off-unrelated time” were ameliorated following STN-DBS, and dyspnea and slowness of thinking were significantly deteriorated postoperatively during “on/off-unrelated time.” Using correlation analysis, no symptoms were significantly correlated with postoperative LEDD reduction; however, the low number of patients in the present study may have affected these results. Constipation was one of the most common preoperative symptoms, reported in 88% of patients before surgery, but just 31% of patients reported this symptom after surgery (Table 2). There are three possibilities to explain the amelioration of constipation in the current study. The first possibility involves the postoperative LEDD reduction that occurs as a result of STN-DBS. Zibetti et al. first suggested this mechanism [33]. Dopaminergic medications are known to influence anorectal function, with an improvement in manometric and electromyographic measures of anorectal function during “on” periods and a deterioration during “off” episodes [2]. The second possibility to explain the improvement in constipation is that STN-DBS has a direct effect on extrapyramidal motor dysfunction. For example, Abott et al. [1] suggested that increased colonic transit time may be a manifestation of the same processes that cause the motor symptoms of PD. The third possibility relates to the increase in physical activity of PD patients after STN-DBS. Studies focusing on the general population and on older patients have shown that immobility or insufficient physical activity is linked to constipation [9, 24]. An amelioration of motor symptoms in PD patients after surgery might improve their mobility and physical activity levels, thus improving their constipation. For these reasons, STN-DBS might improve constipation both directly and indirectly. Drenching sweats were also reported by more than 87% of preoperative patients [25, 28]. Krack et al. reported that the alleviation of drenching sweats after STN-DBS is because of stimulation of the descending sympathetic fibers in the zona incerta [14], while Witjas et al. [29] reported that this alleviation is probably due to STN-DBS-induced improvements in motor complications. Although the relationship between drenching sweats and dyskinesia was not clear in our study, STN-DBS treatment resulted in a significant improvement of drenching sweats. Dysphagia during “off-time” was also significantly improved in the present study. Although clinically significant improvements in swallowing function were not identified in one previous report [27], many reports have shown functional improvement in the tongue, pharynx, and larynx after STN-DBS [5, 13, 16, 17, 23, 31, 33]; therefore, STN-DBS may be related to the improvement in this symptom.
Because dyspnea and slowness of thinking deteriorated postoperatively during “on/off-unrelated time” in the present study, these symptoms may be affected not only by stimulation parameters but also by other factors such as drug treatment or disease progression. The effect of STN-DBS on dyspnea has not been previously reported and requires further clinical study. Regarding slowness of thinking, there are reports that cognitive tasks that rely on working memory are ameliorated by STN-DBS, whereas performance in other cognitive tasks is deteriorated [10, 22]. STN-DBS did not reduce overall cognition, but there was a selective postoperative decrease in frontal cognitive functions [30]. However, because slowness of thinking is a subjective symptom, it may be difficult to identify the damaged subfunction in detail and to understand how it affects patients’ quality of life.
There are several important possible outcomes from the results of this study. If it becomes clear how STN-DBS affects NMSs, a new research field may be developed that pursues the physiological and pathological mechanisms of the interactions between brain stimulation and systemic responses that are derived from peripheral autonomic nerves or other nonmotor neural networks. In addition, the effect of DBS methodology, such as proximity to limbic part of STN, caudate involvement in lead trajectory, and stimulation frequencies may be explored. There is also a possibility that drug reduction methods will be able to be customized depending on individual patients and their specific NMSs. In addition, information about possible worsening or amelioration of NMSs can be disclosed to patients who are considering DBS and other device-aided therapies.
Study limitations
This study has some limitations. Because only a small number of patients were included in this study, the statistical power was low. We must also acknowledge that this questionnaire program only states a preliminary measurement, and that it is difficult to test the reliability and construct validity of this questionnaire program because there were a limited number of cases available.
Conclusion
We presented an online questionnaire system for NMSs in patients with advanced PD. This interview system enabled us to evaluate NMSs in PD patients easily, in detail, and with minimum stress for patients. With this program, comprehensive test results can be obtained not only by STs but also by people who are not used to performing desk inspections. It should be noted that STN-DBS affects not only motor symptoms but also some NMSs. Questionnaire studies should be performed at the time that symptoms are present, because answer by recall is not reliable.
References
Abbott RD, Petrovitch H, White LR, Masaki KH, Tanner CM, Curb JD, Grandinetti A, Blanchette PL, Popper JS, Ross GW (2001) Frequency of bowel movements and the future risk of Parkinson’s disease. Neurology 57:456–462
Ashraf W, Wszolek ZK, Pfeiffer RF, Normand M, Maurer K, Srb F, Edwards LL, Quigley EM (1995) Anorectal function in fluctuating (on-off) Parkinson’s disease: evaluation by combined anorectal manometry and electromyography. Mov Disord 10:650–657
Chaudhuri KR, Martinez-Martin P, Schapira AH, Stocchi F, Sethi K, Odin P, Brown RG, Koller W, Barone P, MacPhee G, Kelly L, Rabey M, MacMahon D, Thomas S, Ondo W, Rye D, Forbes A, Tluk S, Dhawan V, Bowron A, Williams AJ, Olanow CW (2006) International multicenter pilot study of the first comprehensive self-completed nonmotor symptoms questionnaire for Parkinson’s disease: the NMSQuest study. Mov Disord 21:916–923
Chaudhuri KR, Martinez-Martin P, Brown RG, Sethi K, Stocchi F, Odin P, Ondo W, Abe K, Macphee G, Macmahon D, Barone P, Rabey M, Forbes A, Breen K, Tluk S, Naidu Y, Olanow W, Williams AJ, Thomas S, Rye D, Tsuboi Y, Hand A, Schapira AH (2007) The metric properties of a novel non-motor symptoms scale for Parkinson’s disease: results from an international pilot study. Mov Disord 22:1901–1911
Ciucci MR, Barkmeier-Kraemer JM, Sherman SJ (2008) Subthalamic nucleus deep brain stimulation improves deglutition in Parkinson’s disease. Mov Disord 23:676–683
Cronin-Golomb A (2013) Emergence of nonmotor symptoms as the focus of research and treatment of Parkinson’s disease: introduction to the special section on nonmotor dysfunctions in Parkinson’s disease. Behav Neurosci 127:135–138
de Lau LML, Breteler MMB (2006) Epidemiology of Parkinson’s disease. Lancet Neurol 5:525–535
Dickson DW (2018) Neuropathology of Parkinson disease. Parkinsonism Relat Disord 46(Suppl 1):S30–S33
Dukas L, Willett WC, Giovannucci EL (2003) Association between physical activity, fiber intake, and other lifestyle variables and constipation in a study of women. Am J Gastroenterol 98:1790–1796
Jahanshahi M, Ardouin CM, Brown RG, Rothwell JC, Obeso J, Albanese A, Rodriguez-Oroz MC, Moro E, Benabid AL, Pollak P, Limousin-Dowsey P (2000) The impact of deep brain stimulation on executive function in Parkinson’s disease. Brain. 123:1142–1154
Jankovic J (2008) Parkinson’s disease: clinical features and diagnosis. J Neurol Neurosurg Psychiatry 79:368–376
Katsarou Z, Bostantjopoulou S, Peto V, Kafantari A, Apostolidou E, Peitsidou E (2004) Assessing quality of life in Parkinson’s disease: can a short-form questionnaire be useful? Mov Disord 19:308–312
Kitashima A, Umemoto G, Tsuboi Y, Higuchi MA, Baba Y, Kikuta T (2013) Effects of subthalamic nucleus deep brain stimulation on the swallowing function of patients with Parkinson’s disease. Parkinsonism Relat Disord 19:480–482
Krack P, Fraix V, Mendes A, Benabid AL, Pollak P (2002) Postoperative management of subthalamic nucleus stimulation for Parkinson’s disease. Mov Disord 17(Suppl 3):S188–S197 Review
Krack P, Batir A, Van Blercom N, Chabardes S, Fraix V, Ardouin C, Koudsie A, Limousin PD, Benazzouz A, LeBas JF, Benabid AL, Pollak P (2003) Five-year follow-up of bilateral stimulation of the subthalamic nucleus in advanced Parkinson’s disease. N Engl J Med 349:1925–1934
Kulneff L, Sundstedt S, Olofsson K, van Doorn J, Linder J, Nordh E, Blomstedt P (2013) Deep brain stimulation - effects on swallowing function in Parkinson’s disease. Acta Neurol Scand 127:329–336
Lengerer S, Kipping J, Rommel N, Weiss D, Breit S, Gasser T, Plewnia C, Krüger R, Wächter T (2012) Deep-brain-stimulation does not impair deglutition in Parkinson’s disease. Parkinsonism Relat Disord 18:847–853
Limousin P, Krack P, Pollak P, Benazzouz A, Ardouin C, Hoffmann D, Benabid AL (1998) Electrical stimulation of the subthalamic nucleus in advanced Parkinson’s disease. N Engl J Med 339:1105–1111
Martinez-Martin P, Schapira AH, Stocchi F, Sethi K, Odin P, MacPhee G, Brown RG, Naidu Y, Clayton L, Abe K, Tsuboi Y, MacMahon D, Barone P, Rabey M, Bonuccelli U, Forbes A, Breen K, Tluk S, Olanow CW, Thomas S, Rye D, Hand A, Williams AJ, Ondo W, Chaudhuri KR (2007) Prevalence of nonmotor symptoms in Parkinson’s disease in an international setting; study using nonmotor symptoms questionnaire in 545 patients. Mov Disord 22:1623–1629
Moro E, Scerrati M, Romito LM, Roselli R, Tonali P, Albanese A (1999) Chronic subthalamic nucleus stimulation reduces medication requirements in Parkinson’s disease. Neurology 53:85–90
Peto V, Jenkinson C, Fitzpatrick R, Greenhall R (1995) The development and validation of a short measure of functioning and well being for individuals with Parkinson’s disease. Qual Life Res 4:241–248
Pillon B, Ardouin C, Damier P, Krack P, Houeto JL, Klinger H, Bonnet AM, Pollak P, Benabid AL, Agid Y (2000) Neuropsychological changes between “off” and “on” STN or GPi stimulation in Parkinson’s disease. Neurology. 55:411–418
Silbergleit AK, LeWitt P, Junn F, Schultz LR, Collins D, Beardsley T, Hubert M, Trosch R, Schwalb JM (2012) Comparison of dysphagia before and after deep brain stimulation in Parkinson’s disease. Mov Disord 27:1763–1768
Södergren M, McNaughton SA, Salmon J, Ball K, Crawford DA (2012) Associations between fruit and vegetable intake, leisure-time physical activity, sitting time and self-rated health among older adults: cross-sectional data from the WELL study. BMC Public Health 12:551
Swinn L, Schrag A, Viswanathan R, Bloem BR, Lees A, Quinn N (2003) Sweating dysfunction in Parkinson’s disease. Mov Disord 18:1459–1463
Tomlinson CL, Stowe R, Patel S, Rick C, Gray R, Clarke CE (2010) Systematic review of levodopa dose equivalency reporting in Parkinson’s disease. Mov Disord 25:2649–2653
Troche MS, Brandimore AE, Foote KD, Okun MS (2013) Swallowing and deep brain stimulation in Parkinson’s disease: a systematic review. Parkinsonism Relat Disord 19:783–788
Witjas T, Kaphan E, Azulay JP, Blin O, Ceccaldi M, Pouget J, Poncet M, Chérif AA (2002) Nonmotor fluctuations in Parkinson’s disease: frequent and disabling. Neurology 59:408–413
Witjas T, Kaphan E, Régis J, Jouve E, Chérif AA, Péragut JC, Azulay JP (2007) Effects of chronic subthalamic stimulation on nonmotor fluctuations in Parkinson’s disease. Mov Disord 22:1729–1734
Witt K, Pulkowski U, Herzog J, Lorenz D, Hamel W, Deuschl G, Krack P (2004) Deep brain stimulation of the subthalamic nucleus improves cognitive flexibility but impairs response inhibition in Parkinson disease. Arch Neurol 61:697–700
Wolz M, Hauschild J, Koy J, Fauser M, Klingelhöfer L, Schackert G, Reichmann H, Storch A (2012) Immediate effects of deep brain stimulation of the subthalamic nucleus on nonmotor symptoms in Parkinson’s disease. Parkinsonism Relat Disord 18:994–997
Yoshida F, Miyagi Y, Morioka T, Hashiguchi K, Murakami N, Matsumoto K, Nagata S, Sasaki T (2008) Assessment of contact location in subthalamic stimulation for Parkinson’s disease by co-registration of computed tomography images. Stereotact Funct Neurosurg 86:162–166
Zibetti M, Torre E, Cinquepalmi A, Rosso M, Ducati A, Bergamasco B, Lanotte M, Lopiano L (2007) Motor and nonmotor symptom follow-up in parkinsonian patients after deep brain stimulation of the subthalamic nucleus. Eur Neurol 58:218–223
Acknowledgments
We thank Bronwen Gardner, PhD, from Edanz Group (www.edanzediting.com/ac) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was conducted in accordance with the Declaration of Helsinki. This study design was approved by the Ethics Committee of Kyushu University (30-388).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Comments
This is a very practical work showing how the internet can be used to ease the fulfilment of clinical questionnaires. Although some issues related to the self-administration of tests still hold, it improves the easiness to obtain preoperative data at the preoperative stage, and highlights the possible bias of retrieving preoperative data postoperatively.
Juan Barcia
Madrid, Spain
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Functional Neurosurgery - Movement disorders
Rights and permissions
About this article
Cite this article
Kawaguchi, M., Samura, K., Miyagi, Y. et al. The effects of chronic subthalamic stimulation on nonmotor symptoms in advanced Parkinson’s disease, revealed by an online questionnaire program. Acta Neurochir 162, 247–255 (2020). https://doi.org/10.1007/s00701-019-04182-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-019-04182-y