Abstract
Background
Peroneal nerve entrapment is the most common peripheral mononeuropathy of the lower limbs. Foot drop, a common presentation, leads to an impaired eversion and dorsiflexion of the foot. An intriguing observation is the occurrence of foot drop secondary to weight loss.
Methods
A retrospective study of patients surgically treated for peroneal nerve entrapment was performed between January 1, 1995 and December 31, 2016, at the Department of Neurosurgery, Genk, Belgium. Out of a total of 421 patients, 200 patients with foot drop secondary to weight loss were included. For each subject, motor and sensory outcomes after external neurolysis were investigated. As a primary objective, we examined the postoperative outcomes of external neurolysis as a treatment for foot drop in patients with peroneal nerve entrapment at the fibular head secondary to weight loss. As a secondary objective, we analyzed the correlation between patient characteristics and the success rate of external neurolysis.
Results
When defining success as a postoperative MRC score of 4 or 5, external neurolysis has a success rate of 85% in patients with foot drop secondary to weight loss. A significant difference (P = < 0.0001) between postoperative and preoperative MRC scores indicates that external neurolysis leads to significant improvement of motor function in patients with foot drop secondary to weight loss. A multiple logistic regression model showed that “preoperative MRC scores” and “duration of symptoms” were the only variables with an impact on postoperative MRC scores. Other variables such as “age,” “gender,” and “side of entrapment” had no significant impact on postoperative results.
Conclusions
Statistical analysis emphasizes the important role of external neurolysis in the treatment of peripheral peroneal nerve entrapment. Therefore, external neurolysis at the fibular head should be regarded as a very effective and safe procedure in patients with foot drop secondary to weight loss.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Peroneal nerve entrapment is the most common peripheral mononeuropathy of the lower limbs in humans. This can be explained partially by its anatomical course, running through the peroneal canal formed by the fibular neck and the aponeurotic arch of the peroneus longus and soleus muscle [13, 15, 19, 44, 54, 57]. After passing the peroneal canal, the common peroneal nerve splits into its two terminal branches: the superficial and deep peroneal nerve [44]. The former is responsible for motor control of the peroneal muscles, producing foot eversion, and cutaneous innervation of the anterolateral aspect of the distal lower leg and dorsum of the foot [2, 5, 11, 25, 32, 36, 42, 47, 54]. The latter is mainly involved in motor control of the tibialis anterior, extensor hallucis longus and brevis and extensor digitorum longus and brevis muscles, producing dorsiflexion of the foot and toes. In addition, it is responsible for cutaneous innervation of a small area between the first and second toe [2, 5, 11, 36, 47]. Besides loss of sensation and tingling, one of the most common presentations of peroneal nerve entrapment is foot drop, leading to an impaired eversion and dorsiflexion of the foot [19, 31, 36]. Therefore, foot drop has a major impact on quality of life. There are many other causes that could lead to the formation of foot drop [7, 23, 26, 27, 48].
An intriguing observation is the occurrence of foot drop secondary to weight loss in the short term [4, 18, 29, 41, 45, 46, 50, 52, 57]. Although quite some research has been performed about this topic, the exact underlying pathophysiological mechanisms remain mostly unclear [57]. Moreover, there still exists some controversy about the proper treatment of foot drop [39, 49, 53]. Until now, there are no relevant clinical studies performed comparing conservative (e.g., medication, physiotherapy, functional-electric-stimulation) [3, 9, 20] and surgical approaches (e.g., external neurolysis) [20, 21, 34, 37, 40, 57]. Therefore, in order to guide clinical practice, this retrospective study investigates the postoperative motor and sensory outcomes of external neurolysis in patients with peroneal nerve entrapment leading to foot drop.
During this study, we focused on those patients who developed foot drop secondary to weight loss. We also examined correlations between different patient characteristics and success rate of external neurolysis. To our knowledge, this is the first retrospective study containing this extended amount of patients with foot drop secondary to weight loss.
Materials and methods
Data
Between January 1, 1995 and December 31, 2016, as many as 421 patients were treated for peroneal nerve entrapment by a team of neurosurgeons at Ziekenhuis Oost-Limburg (ZOL), Belgium. Data was collected from the patients’ medical record files and databases. Missing data was retrieved by personally contacting patients by telephone or email.
Objectives
The primary objective of this study was to analyze postoperative motor and sensory outcomes of external neurolysis in patients with peripheral peroneal nerve entrapment leading to foot drop secondary to weight loss. As a secondary objective, we set out to determine the impact of important patient characteristics on the success rate of this surgical procedure.
Inclusion and exclusion criteria
Only patients who developed foot drop secondary to an entrapment at the fibular head were selected from the databases. Secondly, only patients with weight loss as the only known cause of foot drop were extracted. Thirdly, only patients who were approached by means of an external neurolysis were selected for further analysis. In this procedure, a longitudinal incision is made at the fibular neck, thereby decompressing the underlying peroneal nerve (Fig. 1) [12, 13, 33, 57]. We applied the following exclusion criteria: entrapment elsewhere the fibular head, multiple causes (e.g., weight loss and L5 radiculopathy) and causes other than weight loss (e.g., synovial cysts, fractures, muscle hypertrophy). Finally, no distinction was made between different causes of weight loss nor between operations performed by different neurosurgeons.
Intraoperative view after external neurolysis at the fibular head showing the two major branches of the common peroneal nerve: the superficial and deep peroneal nerve [57]
Data preparation
Starting from 421 patients who were initially selected, 216 patients presented themselves with peroneal nerve entrapment caused by weight loss. In these, weight loss was the only underlying cause in 213 cases. Loss to follow-up was present in 13 patients. Therefore, based on the inclusion criteria, a total of 200 patients were selected. Patients who were treated for a bilateral peroneal nerve entrapment were statistically analyzed as two individual patients. The flow chart of patient enrolment is illustrated in Fig. 2.
Statistical analysis
In order to obtain a primary image concerning the study population, a number of exploratory analyses were conducted (e.g., table analysis for single endpoints). Depending on the set-up of the corresponding data, a number of different statistical tests were performed. Possible differences in binary data were analyzed using the Fisher’s exact test. As appropriate, we used the chi-square (χ2) test, in particular, meaning that every expected cell frequency was at least five. Possible differences in continuous data were analyzed using a parametric t test. Differences in ordinal data were analyzed using a Wilcoxon-rank sum test.
Analyzing our primary endpoint was done by comparing the preoperative and postoperative motor scores. The same procedure was done for the sensory conditions. This comparison was made using a Wilcoxon-rank sum test. For our secondary endpoint, we used a multiple logistic regression model in combination with backward elimination. Following patient characteristics were used in the model: “gender,” “age at surgery,” “amount of weight loss,” “start of symptoms,” “performing neurosurgeon,” and “side of entrapment.” All statistical analyses were performed in SAS Enterprise Guide 9.4 and SAS Editor 13.1. For all tests performed, we used a cut-off value of 5%, meaning that (unless otherwise indicated) a P value less than 0.05 was considered to be statistically significant.
Results
Patient profile
Patient profiles are summarized in Table 1. One hundred and sixteen patients (58%) were male and 84 patients (42%) were female. The proportion of males and females was significantly different (P = 0.01), indicating that peroneal nerve entrapment caused by weight loss as a single cause seems to be more prevalent in males than females.
One hundred and four patients (52%) presented themselves with a peroneal nerve entrapment located on the right side, while 96 (48%) of the peroneal nerve entrapments were located on the left side. There was no significant difference in location of entrapment in the population as a whole (P = 0.3107), nor in males (P = 0.1546) and females (P = 0.3313) viewed separately. Therefore, although foot drop was more prevalent on the right side, peroneal nerve entrapment caused by weight loss as a single cause does not seem to have a side preference in these patients.
For the study population as a whole, the mean age at surgery was 55 years and 6 months (95% CI 53.1364–57.9681). The mean age at surgery in males was slightly higher than that in females, although there was no significant difference between both sexes (P = 0.1983).
In total, 9 out of 200 patients (4.5%) suffered from a mild or severe complication after external neurolysis. Of these, 7 patients had local wound problems: edema (1 patient), wound dehiscence (1 patient), bleeding (1 patient), wound infection (2 patients), and hematoma formation (2 patients). One patient had a relapse of peroneal nerve entrapment 3 months after surgery. Finally, abscess formation and subsequent staphylococcal aureus sepsis led to the dead of an 87-year-old female patient. She died 28 days after surgery. There was a highly significant difference in proportion of patients with and without postoperative complications, indicating that postoperative complications after external neurolysis are rather uncommon (P = < 0.0001).
The mean amount of weight loss could be retrieved for all 200 patients included in our study. The mean amount of weight loss was 19.43 kg (95% CI 17.324–21.531), with a minimum of 2 kg and a maximum of 74 kg. In total, 69 patients (34.5%) showed a weight reduction of 10 kg or less, while 27 patients (13.5%) showed a weight reduction of at least 40 kg. Most patients with a significant weight reduction were those who underwent bariatric surgery.
Start of symptoms was defined as the time span between beginning of motor and/or sensory symptoms and the day of surgery. This variable gave us some information about the amount of time patients suffered from their symptoms before undergoing surgery. The mean duration of symptoms was 111 days or about 4 months (95% CI 30.000–182.022). Seventy-five patients (37.5%) were treated within the first month after presentation of symptoms, while 80 patients (40%) were treated after 3 months of having symptoms. Finally, there was no significant difference between both sexes concerning the start of symptoms (P = 0.2497).
Electrodiagnostic tests are critical in the evaluation of peroneal nerve lesions [6, 8, 14, 23, 24, 27, 35]. Because lesions located elsewhere the fibular head formed an exclusion criterion, we had to verify that the lesion was indeed located near this critical region. Therefore, motor conduction studies were performed by an electrophysiologist. It is generally accepted that a nerve conduction velocity (NCV) across the fibular head of less than 40 m/s can be interpreted as being aberrant [5, 6, 8, 14, 22, 24, 35, 36].
In total, electrodiagnostic data could be retrieved for 191 out of 200 patients (95.5%). Of these, 61 patients (30.5%) had an abnormal NCV. Paradoxically, 2 patients (1%) showed a normal NCV, while 1 patient (0.5%) showed an increased NCV. The mean NCV amounts to 31.14 m/s (95% CI 29.101–33.180). Finally, there was a significant difference between both sexes (P = 0.0326), in which the mean NCV across the fibular head was significantly lower in males in comparison with females.
Imaging studies were performed by the department of radiology at ZOL (Genk–Belgium) to detect underlying causes of foot drop. High-resolution sonography at the fibular head was performed as a screening tool for structural nerve abnormalities and space-occupying lesions, such as schwannomas and synovial cysts [51, 56]. Magnetic resonance imaging (MRI) was performed when sonographic abnormalities were present [1, 16, 28]. In total, MRI was performed in 69 patients (34.5%). Of these, 22 patients showed no abnormalities, while 27 patients showed direct or indirect signs of peroneal nerve abnormalities; 10 patients showed intraneural edema, 15 patients showed denervation edema of the tibialis anterior muscle, 1 patient showed a loss of fat in the fat pad around the peroneal nerve, and 1 patient showed neuritis of the peroneal nerve. Furthermore, 17 patients showed spinal abnormalities. Of these, 10 patients showed disc herniation, while spinal stenosis was present in 2 patients. Four patients had degenerative abnormalities of the vertebral column. One patient presented with spinal metastasis in the context of lung cancer. Finally, 2 patients had cystic lesions around the peroneal nerve, in which 1 patient had a Baker’s cyst, and 1 patient showed a proximal tibiofibular joint synovial cyst.
Presence of Tinel’s sign could be retrieved from the medical record files in 142 patients (71%). There was a highly significant difference in proportion between patients with and without a Tinel’s sign (P = < 0.0001), indicating that this clinical feature is critical in the physical evaluation of patients with foot drop. Finally, there was no significant difference concerning the occurrence of a Tinel’s sign in both sexes, indicating the presence of this sign is highly predictive for peripheral peroneal nerve entrapment in both sexes (P = 0.4680).
Time for maximal recovery was expressed as the time after surgery at which maximal recovery of motor symptoms was seen. The mean time for maximal recovery was 83 days or about 3 months (95% CI 63.463–103.167). Ninety-five percent of patients had their maximal recovery within the first 6 months after surgery. Finally, there was no significant difference between both sexes concerning the time for maximal recovery (P = 0.0694).
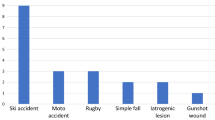
Finally, there were a variety of causes leading to weight loss in our study population (Table 2). In total, 19 different categories could be determined. The category “stress” was defined as all patients who suffered from physical or emotional stress (e.g., mourning, divorce, psychiatric illness), while the category “organ dysfunction” included all patients with organ malfunction (e.g., diabetes, kidney failure, heart failure, hyperthyroidism). Most patients included in our study presented themselves with weight loss of unknown origin.
Motor outcomes
During our study, we used the Medical Research Council (MRC) Scale for Muscle Strength (Table 3). Thereby, foot drop can be classified into five different grades based on the severity of motor deficits, ranging from 0 (no movement is observed) to 5 (normal muscle movement) [38]. MRC scores were checked before and after external neurolysis for each individual patient. By comparing preoperative and postoperative MRC scores, improvement in motor control after surgery could be analyzed. Outcomes are summarized in Fig. 3 and Table 4.
Left figure (a) showing the preoperative MRC scores ranging from zero to four. Right figure (b) showing the postoperative MRC scores ranging from 0 to 5. A MRC score of 0 indicates a total foot drop, while a MRC score of 5 indicates normal muscle strength. Note that one patient died shortly after surgery
Before external neurolysis, 97 patients (48.5%) had the lowest MRC score, meaning that these patients suffered from a complete foot drop. Furthermore, 24 patients (12%), 39 patients (19.5%), 26 patients (13%), and 14 patients (7%) had a MRC score of 1, 2, 3, and 4 respectively. In conclusion, most patients with foot drop presented themselves with a complete foot drop.
However, after external neurolysis, 96 patients (48.24%) had the highest MRC score and therefore had a complete recovery. Only 3 patients (1.51%) maintained a complete foot drop despite external neurolysis. One (0.5%), 11 (5.53%), 15 (7.54%), and 73 (36.68%) patients had a postoperative MRC score of 1, 2, 3, and 4 respectively. There was one loss to follow-up caused by mortality shortly after surgery. Therefore, when defining success as a postoperative MRC score of at least 4, external neurolysis as a treatment for foot drop secondary to weight loss as a single cause has a success rate of 85%.
From a clinical point of view, we were also interested in the gain of MRC score after external neurolysis. Therefore, success rates were expressed as the increase in MRC score after surgery in respect to the preoperative MRC score. Forty-two (21.1%) and 39 (19.6%) patients had a gain of motor function of 4 and 5 respectively. Moreover, 24 patients (12.1%), 44 patients (22%), and 43 patients (21.61%) had a gain of motor function of 1, 2, and 3 respectively, while 7 patients (3.5%) had no improvement after surgery. There was one loss to follow-up caused by mortality shortly after surgery.
Finally, we see that success rate increases as the preoperative MRC score increases. No individual patient had a decrease in MRC score after surgery. Statistical analysis showed a significant difference in postoperative MRC score compared with preoperative MRC score (P = < 0.0001). Therefore, external neurolysis leads to a significant improvement in motor function in patients with foot drop secondary to weight loss.
Sensory outcomes
During physical examination, each individual patient included in our study was asked for sensory deficits. Symptoms qualified as sensory included the presence of hypoesthesia and/or paresthesia. The absence of any postoperative sensory symptoms was considered as “complete recovered,” while those patients with a minimum of sensory symptoms were classified as “partial recovered.” Finally, those patients with no improvement in preoperative state were said to have “no recovery.”
Before external neurolysis, 159 patients (79.5%) mentioned sensory deficits. There was a highly significant difference in the proportion of patients with and without sensory deficits (P = < 0.0001), indicating that foot drop secondary to weight loss is mostly accompanied by sensory symptoms. Of these, 121 patients (76.6%) showed complete recovery after surgery, while 34 patients (21.38%) had a partial recovery.
Finally, only 3 patients (1.89%) had no recovery of their sensory symptoms (Fig. 4). Therefore, external neurolysis secondary to weight loss can be seen as an appropriate treatment option for patients with corresponding sensory deficits, since 98.11% of patients had an improvement of sensory symptoms after surgery.
Multiple logistic regression
A multiple logistic regression model was performed for evaluating which patient characteristics had a significant impact on postoperative MRC score. MRC score of at least 4 was chosen as dependent variable in the model. The following 14 patient characteristics were fitted in the regression model as dependent variables: “age,” “gender,” “performing neurosurgeon,” “preoperative MRC score,” “preoperative sensory symptoms,” “side of entrapment,” “start of symptoms,” “amount of weight loss,” “cause of weight loss,” “year of surgery,” “time for maximal recovery,” “motor conduction study,” “Tinel’s sign,” and “MRI findings.”
All included patient characteristics showed a P value of more than 0.05, except for the variables “start of symptoms” and “preoperative MRC score.” Therefore, only these characteristics had a significant impact on the postoperative MRC score. “Start of symptoms” was proven to be inversely related to postoperative MRC score, meaning that postoperative MRC score deteriorates as the duration of symptoms before surgery increases. Patient characteristics and corresponding P values fitted in the multiple logistic regression model are listed in Table 5.
Discussion
To our knowledge, this is the first retrospective study containing this extended amount of patients with foot drop secondary to weight loss. Although there exist some interesting hypotheses, it still remains unclear how weight loss gives rise to the occurrence of peroneal nerve entrapment. The first observations took place right after World War II, where foot drop was observed in prisoners of war (Kaminsky F. 1947; Denny-Brown D. 1947) [10]. In 1991, Wadström et al. believed that foot drop could be explained by a shortage of vital nutrients and vitamins [46, 55]. Furthermore, foot drop was seen in cancer patients [17, 29, 43] and in patients following a strict diet or those who underwent bariatric surgery [4, 7, 29, 43, 45, 46, 50]. The underlying cause in all of these cases might be explained by the associated weight loss. Nevertheless, weight loss plays an important role in the development of foot drop, occurring in about half of our patients (216 out of 421 patients). This is comparable with previous research conducted by Weyns et al., in which weight loss occurred in 43.5% of patients [57].
There still remains some controversy about the proper treatment of patients with foot drop, especially in those who develop foot drop secondary to weight loss. This is encouraged by a lack of scientific agreement concerning this topic. For example, it remains unclear whether to choose a conservative treatment or a surgical approach right away. In 1976, Sorell et al. performed a retrospective study in which patients with peroneal nerve entrapment were treated conservatively only. Five out of 26 patients (25%) had a complete recovery. Seven patients (35%) showed a partial recovery [49]. This is comparable with the observation made by Krakow et al., where none out of five patients who received a conservative treatment for peroneal nerve entrapment made a full recovery. After performing external neurolysis on the very same patients, four out of five cases (80%) experienced a full recovery [30]. Moreover, there are some studies reinforcing the important role of external neurolysis in the treatment of peroneal nerve entrapment. For example, the study of Thoma et al., in which 19 out of 20 patients (95%) experienced a full recovery [53]. This is comparable with a study conducted by Fabre et al., in which the success rate was 87% after external neurolysis [13]. Despite these good results, we have to take into consideration the small sample size that was encountered in all of these studies. Therefore, the analysis that we made, involving 200 patients, should yield an important contribution in the discussion whether external neurolysis is useful or not in the treatment of patients with peroneal nerve entrapment caused by weight loss.
Data in our study suggests that the moment of surgery is crucial in obtaining excellent postoperative results. Like other studies, the shorter the duration of symptoms before surgery, the better the results [58].
In contrast to earlier studies, we demonstrated that some patient characteristics are important in predicting the benefit of external neurolysis in patients with foot drop secondary to weight loss. Unlike Mont et al., we were able to find an association between the amount of preoperative loss of muscle strength and postoperative recovery [37]. This denotes the fact that a higher preoperative muscle strength is associated with a postoperative outcome that is more satisfactory. Unlike Waldström et al., we found a highly significant association between duration of symptoms and postoperative outcomes after external neurolysis. Therefore, better results can be obtained when patients are treated as soon as possible in the progression of foot drop.
There are some limitations concerning our study. Firstly, we were only able to analyze data from patients admitted to the team of neurosurgeons at ZOL. Because the lack of access to databases from other hospitals in the country, we were not able to follow those patients that were admitted or transferred to another hospital after surgery. However, the statistical methods used in our study did take into account the possibility of potential loss to follow-up. Secondly, it is important to underline the subjective nature of sensory symptoms. It is very hard for patients to precisely describe the exact symptoms that they experience, making detection of these symptoms very difficult. Thirdly, due to lack of relevant research concerning the conservative approach of peroneal nerve entrapment, it is nearly impossible to compare surgical and conservative outcomes. Therefore, further analysis is necessary to assess differences in outcomes between conservative and surgical approaches. Fourthly, the influence of regaining weight on peroneal nerve abnormalities was not considered an objective in our study. However, this could have an added value in current literature. Therefore, this should be further evaluated, leading to a better understanding of the underlying pathophysiology of peripheral nerve abnormalities. Finally, there still exists some operation bias in our study, since patients having symptoms lasting for more than 6 months that are rarely surgically approached at ZOL.
Conclusions
Statistical analysis performed during this study emphasizes the important role of external neurolysis in the treatment of peripheral peroneal nerve entrapment secondary to weight loss. When defining success as a postoperative MRC score of at least 4, external neurolysis has a success rate of 85%. A significant difference (P = < 0.0001) between postoperative and preoperative MRC scores indicates external neurolysis leads to significant improvement of motor function in patients with foot drop secondary to weight loss.
A multiple logistic regression model showed that “preoperative MRC score” and “duration of symptoms” were the only variables with an influence on postoperative MRC score. Other variables such as “age”, “gender,” and “side of entrapment” had no significant impact on postoperative results. Finally, postoperative complications were fairly uncommon and mostly mild. Therefore, external neurolysis can be seen as an effective and safe procedure in patients with foot drop secondary to weight loss. The size of the study population makes this research highly relevant for clinical practice, in particular, because at the moment there are no other studies in medical literature with a comparable population size.
References
Aagaard BD, Lazar DA, Lankerovich L, Andrus K, Hayes CE, Maravilla K, Kliot M (2003) High-resolution magnetic resonance imaging is a noninvasive method of observing injury and recovery in the peripheral nervous system. Neurosurgery 53:199–203 discussion 203-194
Agur AMRDA (2012) Grant’s atlas of anatomy, 13th edn. Lippincott Williams & Wilkins, Philadelphia
Alam M, Choudhury IA, Bin Mamat A (2014) Mechanism and design analysis of articulated ankle foot orthoses for drop-foot. TheScientificWorldJournal 2014:867869. https://doi.org/10.1155/2014/867869
Aprile I, Padua L, Padua R, D'Amico P, Meloni A, Caliandro P, Pauri F, Tonali P (2000) Peroneal mononeuropathy: predisposing factors, and clinical and neurophysiological relationships. Neurol Sci 21:367–371
Baima J, Krivickas L (2008) Evaluation and treatment of peroneal neuropathy. Curr Rev Musculoskelet Med 1:147–153. https://doi.org/10.1007/s12178-008-9023-6
Buschbacher RM PN (2006) Superficial peroneal sensory nerve. Manual of nerve conduction studies (2nd edition):p. 222–226
Cruz-Martinez A, Bort S, Arpa J, Palau F (1997) Hereditary neuropathy with liability to pressure palsies (HNPP) revealed after weight loss. Eur Neurol 37:257–260
Daube JR, Rubin DI (2009) Needle electromyography. Muscle Nerve 39:244–270. https://doi.org/10.1002/mus.21180
De Labachelerie CACC, Pelissier J, Laffont I, Froger J (2013) A new approach to treatment of foot-drop syndrome with functional electrical stimulation in chronic stroke patients. Ann Phys Rehabil Med:56–e384. https://doi.org/10.1016/j.rehab.2013.07.987
Denny-Brown D (1947) Neurological conditions resulting from prolonged and severe dietary restriction; case reports in prisoners-of-war, and general review. Medicine 26:41–113
Drake LRVA, Mitchell AWM (2014) Gray’s anatomy for students, 3d edn. Elsevier, Philadelphia
Ducic I, Felder JM 3rd (2012) Minimally invasive peripheral nerve surgery: peroneal nerve neurolysis. Microsurgery 32:26–30. https://doi.org/10.1002/micr.20959
Fabre T, Piton C, Andre D, Lasseur E, Durandeau A (1998) Peroneal nerve entrapment. J Bone Joint Surg Am 80:47–53
Ghugare BW, Singh RK, Patond KR, Joshi MU (2013) Assessment of nerve conduction study to establish most common electrophysiological predictor of lumbosacral radiculopathy among radiologically diagnosed L5S1 neural foramina compression cases. Indian J Physiol Pharmacol 57(2):209–213
Gloobe H, Chain D (1973) Fibular fibrous arch—anatomical considerations in fibular tunnel syndrome. Acta Anat 85:84–87
Grant GA, Britz GW, Goodkin R, Jarvik JG, Maravilla K, Kliot M (2002) The utility of magnetic resonance imaging in evaluating peripheral nerve disorders. Muscle Nerve 25:314–331
Graus F, Ferrer I, Lamarca J (1983) Mixed carcinomatous neuropathy in patients with lung cancer and lymphoma. Acta Neurol Scand 68:40–48
Harrison MJ (1984) Peroneal neuropathy during weight reduction. J Neurol Neurosurg Psychiatry 47:1260
Hirose CB, McGarvey WC (2004) Peripheral nerve entrapments. Foot Ankle Clin 9:255–269. https://doi.org/10.1016/j.fcl.2004.02.001
Ho B, Khan Z, Switaj PJ, Ochenjele G, Fuchs D, Dahl W, Cederna P, Kung TA, Kadakia AR (2014) Treatment of peroneal nerve injuries with simultaneous tendon transfer and nerve exploration. J Orthop Surg Res 9:67. https://doi.org/10.1186/s13018-014-0067-6
Humphreys DB, Novak CB, Mackinnon SE (2007) Patient outcome after common peroneal nerve decompression. J Neurosurg 107:314–318. https://doi.org/10.3171/jns-07/08/0314
Huynh W, Kiernan MC (2011) Nerve conduction studies. Aust Fam Physician 40:693–697
Ja S (2013) The common fibular nerve. In: Ultrasound Evaluation of Focal Neuropathies: Correlation with Electrodiagnosis. Demos Medical, New York, pp 349–365
Kane NM, Oware A (2012) Nerve conduction and electromyography studies. J Neurol 259:1502–1508. https://doi.org/10.1007/s00415-012-6497-3
Kang PB, Preston DC, Raynor EM (2005) Involvement of superficial peroneal sensory nerve in common peroneal neuropathy. Muscle Nerve 31:725–729. https://doi.org/10.1002/mus.20329
Katirji B (1999) Peroneal neuropathy. Neurol Clin 17:567–591 vii
Katirji MB, Wilbourn AJ (1988) Common peroneal mononeuropathy: a clinical and electrophysiologic study of 116 lesions. Neurology 38:1723–1728
Kim JY, Ihn YK, Kim JS, Chun KA, Sung MS, Cho KH (2007) Non-traumatic peroneal nerve palsy: MRI findings. Clin Radiol 62:58–64. https://doi.org/10.1016/j.crad.2006.07.013
Koehler PJ, Buscher M, Rozeman CA, Leffers P, Twijnstra A (1997) Peroneal nerve neuropathy in cancer patients: a paraneoplastic syndrome? J Neurol 244:328–332
Krackow KA, Maar DC, Mont MA, Carroll C (1993) Surgical decompression for peroneal nerve palsy after total knee arthroplasty. Clin Orthop Relat Res (292):223–228. https://doi.org/10.1097/00003086-199307000-00028
Kuks JBM (2012) Mononeuropathieën van het been: Leerboek Klinische Neurologie 17th edition
Lee JH, Lee BN, An X, Chung RH, Kwon SO, Han SH (2011) Anatomic localization of motor entry point of superficial peroneal nerve to peroneus longus and brevis muscles. Clin Anat 24:232–236. https://doi.org/10.1002/ca.21076
Maalla R, Youssef M, Ben Lassoued N, Sebai MA, Essadam H (2013) Peroneal nerve entrapment at the fibular head: outcomes of neurolysis. Orthop Traumatol Surg Res 99:719–722. https://doi.org/10.1016/j.otsr.2013.05.004
Mackinnon S, Dellon A (1988) Surgery of the peripheral nerve 1st Edition. George Thieme Verlag, p 638
Marciniak C (2013) Fibular (peroneal) neuropathy: electrodiagnostic features and clinical correlates. Phys Med Rehabil Clin N Am 24:121–137. https://doi.org/10.1016/j.pmr.2012.08.016
Masakado Y, Kawakami M, Suzuki K, Abe L, Ota T, Kimura A (2008) Clinical neurophysiology in the diagnosis of peroneal nerve palsy. The Keio journal of medicine 57:84–89
Mont MA, Dellon AL, Chen F, Hungerford MW, Krackow KA, Hungerford DS (1996) The operative treatment of peroneal nerve palsy. J Bone Joint Surg Am 78:863–869
Paternostro-Sluga T, Grim-Stieger M, Posch M, Schuhfried O, Vacariu G, Mittermaier C, Bittner C, Fialka-Moser V (2008) Reliability and validity of the Medical Research Council (MRC) scale and a modified scale for testing muscle strength in patients with radial palsy. J Rehabil Med 40:665–671. https://doi.org/10.2340/16501977-0235
Price BA, Miller G (1992) Internal neurolysis. J Foot Surg 31:250–259
Ramanan M, Chandran KN (2011) Common peroneal nerve decompression. ANZ J Surg 81:707–712
Ramos-Levi AM, Matias-Guiu JA, Guerrero A, Sanchez-Pernaute A, Rubio MA (2013) Peroneal palsy after bariatric surgery; is nerve decompresion always necessary? Nutr Hosp 28:1330–1332. https://doi.org/10.3305/nh.2013.28.4.6495
RE H (1996) Peroneal nerve entrapment at the knee. Oper Tech Sports Med 4(1):46–53
Rubin DI, Kimmel DW, Cascino TL (1998) Outcome of peroneal neuropathies in patients with systemic malignant disease. Cancer 83:1602–1606
Ryan W, Mahony N, Delaney M, O'Brien M, Murray P (2003) Relationship of the common peroneal nerve and its branches to the head and neck of the fibula. Clin Anat 16:501–505. https://doi.org/10.1002/ca.10155
Shahar E, Landau E, Genizi J (2007) Adolescence peroneal neuropathy associated with rapid marked weight reduction: case report and literature review. Eur J Paediatr Neurol 11:50–54. https://doi.org/10.1016/j.ejpn.2006.10.008
Sherman DG, Easton JD (1977) Dieting and peroneal nerve palsy. Jama 238:230–231
Russell S (2006) Examination of peripheral nerve injuries: an anatomical approach. Thieme Medical Publishers, New York, pp 6–30 36-32
Sommer C (2001) Pain in peripheral nerve diseases. Karger. https://doi.org/10.1159/isbn.978-3-318-00741-1
Sorell DA, Hinterbuchner C, Green RF, Kalisky Z (1976) Traumatic common peroneal nerve palsy: a retrospective study. Arch Phys Med Rehabil 57:361–365
Sotaniemi KA (1984) Slimmer’s paralysis—peroneal neuropathy during weight reduction. J Neurol Neurosurg Psychiatry 47:564–566
Spinner RJ, Puffer RC, Skinner JA, Amrami KK (2011) The MRI appearance and importance of the “very” terminal branches of the recurrent articular branch in fibular intraneural ganglion cysts. Clin Anat 24:268–272. https://doi.org/10.1002/ca.21109
Streib E (1993) Weight loss and foot drop. J Iowa Med Soc 83:224–225
Thoma A, Fawcett S, Ginty M, Veltri K (2001) Decompression of the common peroneal nerve: experience with 20 consecutive cases. Plast Reconstr Surg 107:1183–1189
Van den Bergh FR, Vanhoenacker FM, De Smet E, Huysse W, Verstraete KL (2013) Peroneal nerve: normal anatomy and pathologic findings on routine MRI of the knee. Insights Imaging 4:287–299. https://doi.org/10.1007/s13244-013-0255-7
Wadstrom C, Backman L, Persson HE, Reizenstein P (1991) The effect of excessive weight reduction on peripheral and central nervous functions. A study in obese patients treated by gastric banding. Eur J Surg 157:39–44
Weyns F, Bringmans T, Vandevenne J, Daenekindt T, Van Goethem A, Wuyts J, Vanormelingen L, Vandersteen M (2012) Peripheral neuropathy caused by joint-related cysts: a review of 17 cases. Acta Neurochir 154:1741–1753. https://doi.org/10.1007/s00701-012-1444-8
Weyns FJ, Beckers F, Vanormelingen L, Vandersteen M, Niville E (2007) Foot drop as a complication of weight loss after bariatric surgery: is it preventable? Obes Surg 17:1209–1212
Wilkinson MC, Birch R (1995) Repair of the common peroneal nerve. J Bone Joint Surg Br 77:501–503
Acknowledgments
We would like to thank the Department of Neurosurgery at Ziekenhuis Oost-Limburg for providing the required data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
For this type of study, formal consent is not required.
Informed consent
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Comments
An interesting article with results that are not surprising, namely that: Decompressing the common peroneal nerve following the development of a weight loss associated neuropathy has a high success rate; patients with a higher preoperative MRC score and shorter duration of symptoms did better following surgical decompression. The relatively large number of patients studied makes it a useful addition to the literature.
Michel Kliot
CA, USA
This article is part of the Topical Collection on Peripheral Nerves
Rights and permissions
About this article
Cite this article
Broekx, S., Weyns, F. External neurolysis as a treatment for foot drop secondary to weight loss: a retrospective analysis of 200 cases. Acta Neurochir 160, 1847–1856 (2018). https://doi.org/10.1007/s00701-018-3614-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-018-3614-9