Abstract
Background
There is still no clear guideline for surgical treatment for patients with medically refractory trigeminal neuralgia (TN). When it comes to which surgical treatment to choose, microvascular decompression (MVD) or Gamma Knife surgery (GKS), we should know the long-term outcome of each treatment.
Methods
We analyzed 179 patients undergoing MVD and 52 patients undergoing GKS followed for 1 year or longer. We evaluated the patient’s neurological status including pain relief, complications and recurrence. Results were assessed with Barrow Neurological Institute (BNI) pain intensity and facial numbness scores. Overall outcomes were compared between the two groups based on pain relief and complications.
Results
BNI pain intensity and facial numbness scores at the final visit were significantly lower in the MVD group than in the GKS group (P < 0.001, P = 0.04, respectively). Overall outcomes were superior following MVD than following GKS (P < 0.001). Following whichever treatment, there were initially high rates of pain-free status “without medication”: 96.6% in the MVD group and 96.2% in the GKS group. However, 6.1% in the MVD group and 51.9% in the GKS group fell into a “with medication” state within median periods of 1.83 and 3.92 years, respectively (P < 0.001). Kaplan-Meier analysis revealed that pain recurred more often and later in the GKS group than in the MVD group (P < 0.001).
Conclusions
Considering the long-term outcomes, MVD should be chosen as the initial surgical treatment for patients with medically refractory TN.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Trigeminal neuralgia (TN) is a common neurovascular compression syndrome characterized by paroxysmal unilateral facial pain. At early stages of the disease, most patients can control their pain with medication alone [1, 20, 23]. However, the efficacy of medication often declines over time. Some patients become unable to continue medication because of adverse effects, including dizziness, a floating sensation, skin rash and liver dysfunction. For such patients, surgical options are considered.
Various treatments are currently available for intractable TN, including microvascular decompression (MVD), Gamma Knife surgery (GKS), radiofrequency thermocoagulation, glycerol rhizotomy and balloon compression [1, 6, 20, 21, 23]. At our institution, MVD and GKS are available for patients with medically refractory TN. We initially started treatment of TN with GKS in 2005 and subsequently introduced MVD for recurrent cases after GKS. However, our preliminary observations showed that MVD could offer superior pain control with fewer recurrences than GKS. Consequently, MVD is now the first treatment of choice for TN at our institution.
There are several reports on long-term outcomes for MVD and GKS, respectively [1, 13, 17, 20, 23, 27]. However, studies comparing the two treatments are limited [3, 4, 6, 12, 16, 18, 26]. Both treatments are reported to be safe and effective, but concrete guidelines outlining which treatment is recommended after failure of medical therapy do not exist. Surgeons frequently choose treatments with consideration of the patient’s preference. We conducted a retrospective study to compare long-term outcomes (pain relief, recurrence and complications) following MVD or GKS as the initial surgical treatment for medically refractory patients with TN.
Materials and methods
Patient population
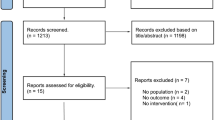
Between April 2005 and September 2016, we treated 372 consecutive patients with medically refractory TN. Patients were predominantly treated with GKS before 2010. Since then, MVD has become the first treatment of choice to date. Only one patient who was medically unfit for MVD was treated with GKS after 2010. As a result, 72 patients were treated with GKS and 300 with MVD during this period (Fig. 1). To exclusively compare the effect of each treatment as the first surgical modality, we excluded patients who had undergone previous surgical treatment, MVD and/or GKS. We also excluded patients with atypical or secondary TN because these cohorts tend to show different postoperative courses than those with typical TN [24]. We were interested in long-term outcomes, so those with follow-up periods of less than 1 year were excluded. Consequently, 179 and 52 patients were enrolled in MVD group and GKS group, respectively (Fig. 1). Written informed consent was obtained from all patients prior to each procedure, and the ethics committee of our hospital approved the study.
Preoperative radiological examinations
To identify any vascular involvement and exclude any implication of tumors, patients underwent two sequences of magnetic resonance imaging (MRI): fast imaging employing steady-state acquisition (FIESTA) and contrast-enhanced T1 spoiled gradient recalled (SPGR). The anatomical data including the compressing vessels and severity of neurovascular compression (NVC) were collected based on MRI findings. Severity of NVC was rated on a degree scale according to Sindou et al. [22] as follows: (1) the vessel in contact with the root without any visible indentation to the root, (2) displacement and/or distortion of the root and (3) a marked indentation in the root.
Microsurgical procedures
In the MVD group, 3D images of the craniotomy site were obtained with contrast-enhanced CT scans to identify the exact site of the transverse-sigmoid junction. Additionally, 3D images of the trigeminal nerve and adjacent structures were created using GammaPlan® (ELEKTA, Stockholm, Sweden) to determine the anatomical relations between the nerve and vessels [7] (Fig. 2). MVD was performed with the retrosigmoid approach under general anesthesia. Transposition of the culprit arteries and sacrifice of small adherent veins were frequently applied. However, interposition was applied in limited cases in which the vertebrobasilar artery or large vein were the compromising vessels [8]. In cases of arachnoid adhesion, the nerve was dissected free from the arachnoid.
Radiosurgical procedures
In the GKS group, CT scans with bone window levels were performed to detect and correct the distortion of MRI and determine the accurate target [5]. A Leksell frame was firmly fixed to the patient’s head under local anesthesia. GammaPlan® was used to accurately determine the retrogasserian target by the patient’s CT and MR images [5, 19] (Fig. 3). Irradiation was performed with a single isocenter at the maximum dose of 85–92 Gy (median, 88 Gy) via a 4-mm collimator helmet.
Assessment of outcomes
Questionnaires or telephone interviews were used to assess the neurological status of patients (pain relief, complications and recurrence) at 1 year or longer after surgery (median, 3.3 years; range, 1–11.1 years). For those who had any additional surgical treatment, their neurological status immediately before the additional treatment was recorded as the final evaluation.
The treatment outcome was evaluated by assessing pain relief in conjunction with recurrence and complications [10]. Treatment outcome was assessed with the Barrow Neurological Institute (BNI) pain intensity score (P) and BNI facial numbness score (N), respectively [21]. The total of both scores (T = P + N) was defined as excellent (T: 2), good (T: 3), fair (T: 4) or poor (T ≥ 5) (Table 1). Complications other than facial numbness were documented separately.
We focused on pain-free status without medication after treatment, as patients tend to find being medication-free more desirable than taking medication. “Recurrence” was defined as any degree of recurrent pain requiring medication and/or additional surgical procedures after reaching a medication-free status.
Statistical analysis
We analyzed data with two-tailed Fisher exact tests for nominal data and Student’s t-tests for continuous data. A P-value less than 0.05 was considered statistically significant. The probability of a pain-free period without medication was assessed with Kaplan-Meier analyses. Analyses were conducted with commercially available software (JMP®, SAS, Cary, NC, USA).
Results
Patient characteristics
In this study, 231 patients with TN were initially treated with either MVD (n = 179; female/male, 114/65; mean age, 62 years; age range, 19–97 years) or GKS (n = 52; female/male, 35/17; mean age, 71; age range, 45–89 years) (Table 2). All patients had medically intractable TN (P-4, P-5; Table 2), which affected the face unilaterally. The right side was affected in 101 patients (56.4%) undergoing MVD and in 30 patients (57.7%) undergoing GKS.
The V2 division of the trigeminal nerve was most frequently involved (MVD: 64 patients, 35.8%; GKS: 18 patients, 34.6%) followed by the V3 division (MVD: 42 patients, 23.5%; GKS: 13 patients, 25.0%). Multiple division involvement was recognized in both groups (MVD: 65 patients, 36.3%; GKS: 20 patients, 38.4%). Involvement of solely V1 division was rare in both groups (MVD: 8 patients, 4.5%; GKS: 1 patients, 1.9%).
The most common compressing vessel was the superior cerebellar artery (SCA), followed by both the SCA and anterior inferior cerebellar artery (AICA), AICA, vein and vertebrobasilar arteries (VB). Regarding severity of NVC, degree 1 was most common, followed by degrees 2 and 3. There were no significant differences between the two groups in the affected division, compressing vessel and NVC severity (Table 2).
The period from pain onset to treatment ranged from 0.1 to 40 years (median, 4 years) in the MVD group and 0.5 to 24 years (median, 4.5 years) in the GKS group. Follow-up duration ranged from 1 to 9.6 years (median, 3.25 years) in the MVD group and 1 to 11.1 years (median, 5.0 years) in the GKS group. Patient characteristics did not significantly differ between the groups except age at treatment and follow-up period. Those undergoing GKS had longer follow-up periods than those undergoing MVD because our institution initially started to treat TN only with GKS (Table 2).
Pain relief (P)
We compared pain relief at the final assessment between the two groups using the BNI pain intensity scores (Table 3). In the MVD group, 144 patients (80.4%) were graded P-1 (no pain, no medication), 17 (9.5%) were graded P-2 (occasional pain, not requiring medication), 15 (8.4%) were graded P-3 (some pain, adequately controlled with medication), and 3 (1.7%) were graded P-4/5 (some pain, not adequately controlled with medication/severe pain/no pain relief). In the GKS group, the number of patients graded P-1, P-2, P-3 and P-4/5 was 20 (38.5%), 3 (5.8%), 12 (23.1%) and 17 (32.7%), respectively. The groups statistically differed from each other (P < 0.001), suggesting greater pain relief was achieved following MVD than following GKS.
Numbness (N)
Postoperative numbness was assessed with the BNI facial numbness scores (Table 3). In the MVD group, 144 patients (80.4%) were graded N-1 (no facial numbness), 25 (14.0%) were graded N-2 (mild facial numbness, not bothersome), and 10 (5.6%) were graded N-3/4 (facial numbness, somewhat bothersome/very bothersome). In the GKS group, the number of patients graded N-1, N-2 and N-3/4 was 33 (63.5%), 13 (25.0%) and 6 (11.5%), respectively. The groups differed significantly from each other (P = 0.04), suggesting patients undergoing GKS more frequently experienced postoperative numbness than did those undergoing MVD.
Aside from numbness, severe dry eye requiring periodical care by ophthalmology was found in both groups at the final assessment. However, hearing disturbance (dysfunction of the eighth nerve), masticatory weakness (dysfunction of trigeminal motor root) and cerebellar dysfunction were only noted in the MVD group (Table 3). However, there were no significant differences between the groups for rates of complications besides facial numbness.
Overall outcome
The overall outcome at the final follow-up was evaluated by summing the BNI pain intensity score and the BNI facial numbness score (Table 3, Fig. 4). In the MVD group, 122 patients (68.2%) were graded “excellent,” 28 patients (15.6%) “good,” 19 patients (10.6%) “fair” and 10 patients (5.6%) “poor.” In the GKS group, 13 patients (25.0%) were graded “excellent,” 5 patients (9.6%) “good,” 11 patients (21.2%) “fair” and 23 patients (44.2%) “poor.” As such, MVD provides a significantly superior long-term outcome compared with GKS (P < 0.001).
Long-term efficacy
There were 173 (96.6%) and 50 (96.2%) medication-free patients (P-1/P-2) at 1-year post-operation in the MVD and GKS groups, respectively. Recurrence (≥ P-3) over time was found in 11 patients (6.1%) undergoing MVD and 27 patients (51.9%) undergoing GKS (P < 0.001). The time to recurrence ranged from 1.17 to 8 years (median, 1.83 years) in the MVD group and 1.08 to 10.83 years (median, 3.92 years) in the GKS group (P = 0.001) (Table 4). The long-term efficacy of treatment (patients remaining medication-free, P-1/P-2) was evaluated with Kaplan-Meier analysis. The GKS group lost medication-free status faster than the MVD group (P < 0.001) (Fig. 5).
Discussion
The goal of treatment for TN is to achieve a complete and permanent cure without any postoperative complications [10]. It is widely accepted that the etiology of typical TN is caused by vascular compression or conflict of the trigeminal nerve, generating ephaptic transmission between neurons [1, 20, 23].
The advantage of MVD, the only non-ablative technique, is that it theoretically eliminates the cause of pain. However, MVD is associated with a greater potential of surgical risk than other procedures, including trigeminal dysfunction, and impairment of other cranial nerves, cerebellum and brainstem function [1, 23]. Other procedures, e.g., GKS, radiofrequency rhizotomy, glycerol postgasserian rhizolysis and balloon microcompression of the gasserian ganglion, are ablative techniques that rely on controlled injury to part of the nerve to generate neuromodulation without intracranial manipulation and are expected to possess fewer risks than MVD [2, 6, 12, 17, 18, 20]. It is crucial that patients should be provided detailed information regarding both surgery-related risks and long-term outcomes for each treatment.
Barker et al. [1] reported postoperative outcomes of 1185 patients who underwent MVD during a 20-year period. In their series, 70% of patients remained pain free without medication for 10 years, 30% had recurrence, and 11% underwent a second operation for recurrence. Sindou et al. [22] investigated long-term outcome of 362 patients who underwent MVD in which decompression of the root was performed without any additional lesioning or cutting of the adjacent rootlets. According to Kaplan-Meier analysis, the pain-free rate without any medication was 91% at 1 year and 73.38% after 15 years of follow-up. Although MVD is considered safe and effective in treating medically intractable TN, complications such as facial numbness, brainstem infarction, ipsilateral hearing loss and death were reported in their MVD series. Aggressive dissection may achieve more pain relief while increasing the risk of complications. Later reports indicated that thorough decompression of the whole cisternal portion of the nerve, transposition rather than interposition, and adequate management of veins are also crucial to obtain better surgical outcomes with fewer complications and recurrences [8, 15, 23]. Therefore, the outcome of MVD is largely attributable to the surgeon’s skills and decision-making during surgery.
In contrast, technical differences in GKS, such as the target site and prescribed dose, may affect outcomes. Kondziolka et al. [11] reported that lower prescription doses decrease pain relief rates, while a higher dose induces more postoperative complications. They concluded that the optimal radiation dose is between 70 Gy and 90 Gy. Matsuda et al. [14] compared the results of two targeting methods, the retrogasserian target and the root entry zone target. Although pain control rates at the final follow-up were similar between the two targets, patients treated with the retrogasserian target had a higher incidence of trigeminal dysfunction. Thus, they recommended using the root entry zone target and 80 Gy for treatment of TN in GKS. Recently, Régis et al. [20] reported the long-term outcomes of 497 patients initially treated with GKS (median maximum dose: 85 Gy). Although 456 patients (91.75%) were pain free in a median of 10 days, their actuarial probabilities of continuing to be pain free without medication at 3, 5, 7 and 10 years were 71.8%, 64.9%, 59.7% and 45.3%, respectively. Our long-term outcome of GKS for medication-free status showed a similar tendency to their report. They report the actuarial rate of hypesthesia was 20.4% at 5 years and reached 21.1% at 7 years, including very bothersome facial hypesthesia in three patients (0.6%). Numbness in the GKS group in our study was more than in their report, which may have been caused by the higher prescribed dosage (median maximum dose: 88 Gy). Initial pain relief is satisfactory, but shorter durability and a higher chance of facial numbness are common following GKS compared with MVD [1, 9].
Seven studies compared the outcomes for MVD and GKS at a single institution (Table 5) [3, 4, 6, 12, 16, 18, 26]. Although follow-up periods and definitions of numbness and recurrence differ in each report, the majority indicate that MVD provides superior efficacy for long-term pain relief and less facial paresthesia than GKS. This is consistent with our results. Linskey et al. [12] compared 36 patients treated with MVD and 44 patients with GKS. They observed 5-year actuarial pain-free rates of 80% for MVD and 33% for GKS (P = 0.002). The relative risk of losing pain-free status after 5 years was 3.35-fold higher for those treated with GKS compared with MVD. Both procedures ensured a high degree of early patient satisfaction (95–100%). While MVD maintained a high rate of patient satisfaction, satisfaction with GKS decreased to 75% as pain control waned. A recent study by Dai et al. [4] showed that pain reduction 2 years after treatment is significantly greater for MVD (95.4%) than for GKS (88.7%) (P < 0.01). There was also significantly greater corneal reflection loss in GKS (21.7%) than in MVD (5.7%) (P = 0.002). There was also more facial numbness in GKS (17.4%) than in MVD (14.9%). However, the GKS complication rate was lower than ours, which might reflect a lower prescription dose and a different target.
Berger et al. [2] collated articles on MVD or stereotactic radiosurgery (SRS) for TN published between 2000 and 2015. They used decision-analytic modeling to compare a large cohort undergoing MVD (3697 patients, mean follow-up: 43.2 months) with those undergoing SRS (3477 patients, mean follow-up: 31.7 months). Their results suggest pain is significantly more likely to be cured (BNI score P-1) after MVD. In addition to better pain control, MVD was associated with significantly lower complications and recurrences than SRS, suggesting that MVD provides more favorable outcomes than SRS for the treatment of TN. Another literature review [25] investigated long-term outcomes for various TN treatments, including MVD, SRS, glycerol rhizotomy, partial sensory rhizotomy, percutaneous balloon microcompression and radiofrequency thermorhizotomy. The study compared 4884 patients treated with MVD with 107 treated with SRS. Of those undergoing MVD, 76.6% were pain free and 18.4% experienced recurrence 6.7 years after surgery, while in those undergoing SRS 58% were pain free and 25% experienced recurrence 5 years after treatment. Thus, MVD was associated with the highest rate of long-term patient satisfaction and the lowest rate of pain recurrence among several treatment methods. Although differing targets and doses may affect outcomes after GKS, uniform procedures for the treatment are used at each institution. Nonetheless, outcomes for MVD are influenced more by the surgeon’s skills and experiences [9]. In experienced hands, surgery-related complications are uncommon. Therefore, MVD might be considered as the first-line treatment for an experienced team when the patient’s condition allows [25].
Treatment choice generally depends on patient’s preference. Due to lower surgery risks than MVD, GKS is generally considered desirable. Surgery-related complications may occur following surgery even conducted by experienced neurosurgeons. Nonetheless, these complications are uncommon and rates are lower than for other common neurosurgical procedures such as aneurysmal clipping or brain tumor excision [12]. In our study, there was a low rate of complications and no significant difference between MVD and GKS groups. Therefore, patients should not only consider surgery-related risk but also long-term outcomes for each treatment, because satisfaction will reduce as pain control wanes. In case of recurrence of pain, patients eventually visit a physician regularly for medication and may live in constant fear of a painful attack. Even if pain is controlled, facial numbness, which is usually difficult to cure, has negative implications for a patient’s quality of life. When making surgical decisions, physicians should provide patients with detailed information about various TN treatments.
Limitations
This is a retrospective study at a single institute, and patients were not randomized. Although patients were given detailed information about MVD and GKS, their treatment choice was subject to bias. We could not exclude the possibility that differences observed in this study may have been caused by differences in baseline characteristics between the two groups. We acknowledge that this is an institutional result of MVD and GKS offered as the first surgical treatment for TN. Therefore, our results may not be applicable for patients with other types of TN, such as recurrent TN, atypical TN, secondary TN or patients who previously underwent surgical procedures.
Conclusions
As MVD provides superior outcomes compared to GKS, it should be considered the initial surgical treatment for patients with TN. However, when it comes to which surgical treatment to choose, the patient’s condition and the surgeon’s skill should be taken into consideration.
References
Barker FG 2nd, Jannetta PJ, Bissonette DJ, Larkins MV, Jho HD (1996) The long-term outcome of microvascular decompression for trigeminal neuralgia. N Engl J Med 334:1077–1083
Berger I, Nayak N, Schuster J, Lee J, Stein S, Malhotra NR (2017) Microvascular decompression versus stereotactic radiosurgery for trigeminal neuralgia: a decision analysis. Cureus 9:e1000
Brisman R (2007) Microvascular decompression vs. Gamma Knife radiosurgery for typical trigeminal neuralgia: preliminary findings. Stereotact Funct Neurosurg 85:94–98
Dai ZF, Huang QL, Liu HP, Zhang W (2016) Efficacy of stereotactic Gamma Knife surgery and microvascular decompression in the treatment of primary trigeminal neuralgia: a retrospective study of 220 cases from a single center. J Pain Res 26:535–542
Hayashi M, Chernov M, Tamura N, Taira T, Izawa M, Yomo S, Nagai M, Chang CS, Ivanov P, Tamura M, Muragaki Y, Okada Y, Iseki H, Takakura K (2011) Stereotactic radiosurgery of essential trigeminal neuralgia using Leksell Gamma Knife model C with automatic positioning system: technical nuances and evaluation of outcome in 130 patients with at least 2 years follow-up after treatment. Neurosurg Rev 34:497–508
Hitchon PW, Holland M, Noeller J, Smith MC, Moritani T, Jerath N, He W (2016) Options in treating trigeminal neuralgia: experience with 195 patients. Clin Neurol Neurosurg 149:166–170
Inoue T, Hirai H, Shimizu T, Tsuji M, Shima A, Suzuki F, Matsuda M (2012) Ocular neuromyotonia treated by microvascular decompression: usefulness of preoperative 3D imaging: case report. J Neurosurg 117:1166–1169
Inoue T, Hirai H, Shima A, Suzuki F, Fukushima T, Matsuda M (2017) Diagnosis and management for trigeminal neuralgia caused solely by venous compression. Acta Neurochir 159:681–688
Kalkanis SN, Eskandar EN, Carter BS, Barker FG 2nd (2003) Microvascular decompression surgery in the United States, 1996 to 2000: mortality rates, morbidity rates, and the effects of hospital and surgeon volumes. Neurosurgery 52:1251–1261
Kondo A, Date I, Endo S, Fujii K, Fujii Y, Fujimaki T, Hasegawa M, Hatayama T, Hongo K, Inoue T, Ishikawa M, Ito M, Kayama T, Kohmura E, Matsushima T, Munemoto S, Nagahiro S, Ohno K, Okamura T, Ryu H, Shigeno T, Shirane R, Tagusagawa Y, Tanabe H, Yamada K, Yamakami I (2012) A proposal for standardized analysis of the results of microvascular decompression for trigeminal neuralgia and hemifacial spasm. Acta Neurochir 154:773–778
Kondziolka D, Lunsford LD, Flickinger JC, Young RF, Vermeulen S, Duma CM, Jacques DB, Rand RW, Regis J, Peragut JC, Manera L, Epstein MH, Lindquist C (1996) Stereotactic radiosurgery for trigeminal neuralgia: a multiinstitutional study using the gamma unit. J Neurosurg 84:940–945
Linskey ME, Ratanatharathorn V, Peñagaricano J (2008) A prospective cohort study of microvascular decompression and Gamma Knife surgery in patients with trigeminal neuralgia. J Neurosurg 109:160–172
Martínez Moreno NE, Gutiérrez-Sárraga J, Rey-Portolés G, Jiménez-Huete A, Martínez Álvarez R (2016) Long-term outcomes in the treatment of classical trigeminal neuralgia by Gamma Knife radiosurgery: a retrospective study in patients with minimum 2-year follow-up. Neurosurgery 79:879–888
Matsuda S, Serizawa T, Nagano O, Ono J (2008) Comparison of the results of 2 targeting methods in Gamma Knife surgery for trigeminal neuralgia. J Neurosurg 109:185–189
Matsushima T, Yamaguchi T, Inoue TK, Matsukado K, Fukui M (2000) Recurrent trigeminal neuralgia after microvascular decompression using an interposing technique. Teflon felt adhesion and the sling retraction technique. Acta Neurochir 142:557–561
Nanda A, Javalkar V, Zhang S, Ahmed O (2015) Long term efficacy and patient satisfaction of microvascular decompression and Gamma Knife radiosurgery for trigeminal neuralgia. J Clin Neurosci 22:818–822
Oesman C, Mooij JJA (2011) Long-term follow-up of microvascular decompression for trigeminal neuralgia. Skull Base 21:313–322
Pollock BE, Schoeberl KA (2010) Prospective comparison of posterior fossa exploration and stereotactic radiosurgery dorsal root entry zone target as primary surgery for patients with idiopathic trigeminal neuralgia. Neurosurgery 67:633–638
Régis J, Metellus P, Hayashi M, Roussel P, Donnet A, Bille-Turc F (2006) Prospective controlled trial of Gamma Knife surgery for essential trigeminal neuralgia. J Neurosurg 104:913–924
Régis J, Tuleasca C, Resseguier N, Carron R, Donnet A, Gaudart J, Levivier M (2016) Long-term safety and efficacy of Gamma Knife surgery in classical trigeminal neuralgia: a 497-patient historical cohort study. J Neurosurg 124:1079–1087
Rogers CL, Shetter AG, Fiedler JA, Smith KA, Han PP, Speiser BL (2000) Gamma Knife radiosurgery for trigeminal neuralgia: the initial experience of the Barrow Neurological Institute. Int J Radiat Oncol Biol Phys 47:1013–1019
Sindou M, Leston J, Decullier E, Chapuis F (2007) Microvascular decompression for primary trigeminal neuralgia: long-term effectiveness and prognostic factors in a series of 362 consecutive patients with clear-cut neurovascular conflicts who underwent pure decompression. J Neurosurg 107:1144–1153
Sindou M, Leston JM, Decullier E, Chapuis F (2008) Microvascular decompression for trigeminal neuralgia: the importance of a noncompressive technique—Kaplan-Meier analysis in a consecutive series of 330 patients. Neurosurgery 63:341–350
Sindou M, Leston J, Howeidy T, Decullier E, Chapuis F (2006) Micro-vascular decompression for primary trigeminal neuralgia (typical or atypical). Long-term effectiveness on pain; prospective study with survival analysis in a consecutive series of 362 patients. Acta Neurochir 148:1235–1245
Tatli M, Satici O, Kanpolat Y, Sindou M (2008) Various surgical modalities for trigeminal neuralgia: literature study of respective long-term outcomes. Acta Neurochir 150:243–255
Wang DD, Raygor KP, Cage TA, Ward MM, Westcott S, Barbaro NM, Chang EF (2017) Prospective comparison of long-term pain relief rates after first-time microvascular decompression and stereotactic radiosurgery for trigeminal neuralgia. J Neurosurg 24:1–10
Zhang H, Lei D, You C, Mao BY, Wu B, Fang Y (2013) The long-term outcome predictors of pure microvascular decompression for primary trigeminal neuralgia. World Neurosurg 79:756–762
Acknowledgments
We thank Ms. Satomi Fujimura and Ms. Lori Radcliffe for assistance with data collection and English language editing.
Funding
No funding was received for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Inoue, T., Hirai, H., Shima, A. et al. Long-term outcomes of microvascular decompression and Gamma Knife surgery for trigeminal neuralgia: a retrospective comparison study. Acta Neurochir 159, 2127–2135 (2017). https://doi.org/10.1007/s00701-017-3325-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-017-3325-7