Abstract
Background
Thalamopeduncular tumors arise at the junction of the inferior thalamus and cerebral peduncle, and present with a common clinical syndrome of progressive spastic hemiparesis.
Method
Formal preoperative magnetic resonance imaging (MRI) and diffusion tensor imaging (DTI) were performed. Postoperative MRI was obtained to evaluate the extent of tumor resection. A prospective analysis of clinical outcomes was then conducted by the senior author.
Conclusions
Preoperative tractography is a useful adjunct to surgical planning in tumors that displace motor pathways. Gross total resection of pilocytic astrocytomas usually results in cure, and therefore should be entertained when developing treatment strategies for thalamopeduncular tumors of childhood.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Relevant surgical anatomy
The thalamopeduncular syndrome is a common clinical presentation of progressive spastic hemiparesis exhibited by children harboring a tumor of the cerebral peduncle just underneath the thalamus (Fig. 1). They typically present in the first 2 decades of life and are pilocytic astrocytomas. As these pilocytic tumors grow, they cross the ambient cistern to enter the temporal horn of the lateral ventricle through the choroidal fissure (Fig. 2). As they enlarge, the unilateral motor symptoms most commonly lead to diagnosis. The displacement of the corticospinal tract (CST) can be variable, but in the majority of cases they are anterolateral (Fig. 3). The ispilateral optic tract is often stretched around the lateral aspect of the tumor and can usually be identified on the preoperative magnetic resonance imaging (MRI), as well as at surgery. This structure should be identified and spared. It can be easily identified as it runs parallel to the basal vein of Rosenthal as it courses around the brain stem. If the tumor extends below the tentorial edge, it may also involve the third or fourth cranial nerve. In one of our cases, the third nerve was thinned and not identifiable within the tumor capsule until after it had been transected.
Left thalamopeduncular pilocytic astrocytoma. a Composite of three axial T1-weighted Gd-enhanced MRIs demonstrates that the tumor arises from the lateral aspect of the peduncle underneath the thalamus, pushing the normal thalamus superiorly. The thalamic displacement made a transcallosal approach to the tumor a poor choice, because the surgeon would have violated the normal thalamus to reach the tumor. b The optic tract, a structure that must be carefully avoided in removing the tumor, is deviated superior and lateral to the tumor. The arrow designates the CST. ) An axial DTI of the same tumor shows the CSTs deviated anteriorly and laterally (arrow; CSTs are in blue); this was the most common pattern of CST displacement in this series, noted in seven of ten patients. This pattern of tract displacement made a transsylvian approach unattractive; one would have to transect the tracts to reach the tumor. d Coronal DTI. e The authors chose an approach through the middle temporal gyrus by using frameless stereotactic navigation to approach the tumor just posterior to the CSTs [1]
Left thalamopeduncular cystic and solid pilocytic astrocytoma. a A coronal fluid-attenuated inversion recovery (FLAIR) MRI demonstrating that the tumor grows from the thalamopeduncular junction, across the ambient cistern, and through the choroidal fissure of the temporal horn of the lateral ventricle to invade the middle fossa. b Coronal DTI showing that the CSTs are displaced medial to the tumor. Medial tract displacement made an image-guided approach through the middle temporal gyrus optimal to reach both the superior and inferior extent of the neoplasm. c A coronal T2-weighted MRI obtained the day after surgery, demonstrating the approach through the temporal lobe and a gross total resection of the tumor, sparing the CSTs
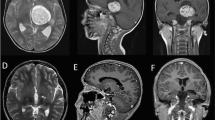
Pilocytic tumor in a 3-year-old child presenting with spastic hemiparesis. a Axial T2-weighted MRI showing displacement of the thalamus anterior and posterior to the tumor. b A DTI color map. The arrows (tracts in blue) designate the CST. c A fractional anisotropy map demonstrating that in this case the CSTs (arrows) were draped around the lateral aspect of the tumor, which made a lateral approach unattractive. d, e Sagittal T1-weighted MRI showing previous biopsy tract; note enhancement of the tract. f The authors chose to use the previous biopsy tract, a transfrontal corticotomy, to remove the tumor; the patient’s hemiparesis improved postoperatively
Description of the technique
We have found that a transtemporal transchoroidal approach through the temporal horn allows a complete resection in the majority of children with this disease. However, we have seen cases in which the CSTs are completely lateral or completely medial. In the lateral case, a transcortical middle frontal gyrus approach allowed a curative resection. In other cases, the tumor may extend into the posterior fossa. In such cases, a staged transtemporal approach followed by a supracerebellar infratentorial approach has allowed complete resection of these larger tumors. The points are that the CSTs can be identified by MRI and the specific approach tailored to spare these tracts and the ipsilateral optic tract. Secondly, these tumors generally extend superiorly enough that a subtemporal or supracerebellar approach alone will not allow access to the superior portion of the tumor. The transchoroidal approach will allow that access.
Indications
Subsequently we have utilized MRI tractography to define the displacement of the CSTs and to tailor the approach based upon these findings. In the majority of patients, the CSTs have been displaced anterolaterally. Prior authors have attempted resection of these through a subtemporal approach, but have been able to accomplish a complete resection in only a minority of children [2, 3].
Limitations
In our first experience with this tumor, prior to the development of MRI tractography, a transsylvian approach was used to resect such a tumor where it invaded the temporal horn of the lateral ventricle. A complete resection was accomplished; however, the patient’s hemiparesis was worsened by the resection, without a clear-cut explanation from his postoperative MRI. We now know that in 80% of these children, the CSTs are displaced anterolaterally by the tumor, in which case a transsylvian approach leads to their violation and subsequent hemiplegia.
How to avoid complications
In utilizing a transtemporal approach through the middle temporal gyrus, care should be taken to minimize the use of fixed retractors as these seem to cause more ischemic changes on postoperative imaging than is seen following dynamic retraction (Fig. 4). In opening the choroidal fissure above the alveus of the hippocampus, the hippocampus should be protected with cottonoids. Within the cistern, branches of the posterior communicating artery and anterior choroidal artery should be protected. The optic tract is often found just above the opening into the cistern and can generally be identified on high-resolution MRI preoperatively. Injury to the tract causes homonymous hemianopsia. In cases with larger tumors, we have seen the third nerve thinned out and indistinguishable from the tumor capsule. In one case the third nerve was cut inadvertently and in another case the optic tract was cut inadvertently, as those structures appeared to be fibrous capsular tissue rather than neural tissue. Whether or not stimulation and monitoring is helpful is an unanswered question. The pilocytic tumors are usually gray fleshy tumors, which are clearly different from the subjacent white matter tracts of the brain stem. Postoperatively, most patients are initially weaker on the contralateral side, but with physical therapy will generally ambulate and become more functional than they were preoperatively. We have not seen postoperative seizures in our series to date.
A 6-year-old, right-handed boy with a 4-month history of progressive right hemiparesis; recent onset of headaches; functional spastic hemiparesis on exam with thalamic hand. a Tumor invading temporal horn of lateral ventricle. b Gross total resection accomplished; patient developed dense contralateral hemiparesis postoperatively secondary to probable violation of the descending motor tracts
Specific perioperative considerations
While resection of these lesions is generally curative, diffusion tensor imaging (DTI) is a valuable tool for preoperative planning (Fig. 5). Given their growth patterns, thalamopeduncular tumors tend to encroach on the ipsilateral optic tract, basal vein of Rosenthal, and ipsilateral third cranial nerve. An approach should be tailored to avoid these delicate neural structures, with the goal of gross total resection. In this series, the tumors that had been treated with low-grade chemotherapy had all progressed, suggesting that perhaps conventional chemotherapy is of marginal benefit in the management of these neoplasms [1].
A 5-year-old child presenting with a 3-week history of progressive hemiparesis, arm worse than leg; a several-day history of headache, nausea, and vomiting. a Preoperative images. b Axial DTI. c Sagittal DTI. d Postoperative axial image. e T1 + Gd coronal image 1 year postoperative showing complete tumor resection. Out of 14 children, so far only two have recurred, and one has required chemotherapy and radiotherapy. The others have not required additional treatment
Specific information to give to the patient about surgery and potential risks
Patients should be informed that the hemiparesis will likely be worse immediately postoperatively, but should improve over time with physical therapy. Most patients do not return to normal but are functional. All ambulate but tend to have some residual spasticity in either an arm or a leg. At risk is a homonymous hemianopsia, possible double vision or ptosis if the third nerve is injured, and possible tumor recurrence. Although a theoretical risk, we have not seen postoperative seizures to date.
References
Broadway SJ, Ogg RJ, Scoggins MA, Sanford R, Patay Z, Boop FA (2011) Surgical management of tumors producing the thalamopeduncular syndrome of childhood. J Neurosurg Pediatr 7:589–595. doi:10.3171/2011.4.PEDS119
Puget S, Crimmins DW, Garnett MR, Grill J, Oliveira R, Boddaert N, Wray A, Lelouch-Tubiana A, Roujeau T, Di Rocco F, Zerah M, Sainte-Rose C (2007) Thalamic tumors in children: a reappraisal. J Neurosurg 106:354–362. doi:10.3171/ped.2007.106.5.354
Tomita T, Cortes RF (2002) Astrocytomas of the cerebral peduncle in children: surgical experience in seven patients. Childs Nerv Syst 18:225–230. doi:10.1007/s00381-002-0576-1
Acknowledgements
The authors wish to thank Andrew J. Gienapp, BA (Department of Medical Education, Methodist University Hospital, Memphis, TN and Department of Neurosurgery, University of Tennessee Health Science Center, Memphis, TN) for technical and copyediting, and preparation of the manuscript and figures for publishing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research.
Conflict of interest
Dr. Boop declares that he has worked as a consultant for Medtronic. Mr. Foley declares that he has no conflict of interest to disclose.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Informed consent
Informed consent was obtained from all individual participants included in the study. Additional informed consent was obtained from all individual participants for whom identifying information is included in this article.
Additional information
Key points
1. These tumors are usually of benign pathology
2. They usually occur in children in the first 2 decades of life
3. The children present with progressive spastic hemiparesis, and if the tumor continues to enlarge, will develop hydrocephalus
4. Following resection, the patient’s hemiparesis is usually worsened immediately, but will improve over time and with therapy
5. There is risk of damage to the optic tract and subsequent homonymous hemianopsia
6. There is risk of damage to the third cranial nerve which could prevent opening of the ipsilateral eye or cause diplopia
Electronic supplementary material
Navigated trans-temporal trans-choroidal microsurgical resection of thalamo-peduncular tumor. (MP4 341,468 kb)
Rights and permissions
About this article
Cite this article
Foley, R., Boop, F. Tractography guides the approach for resection of thalamopeduncular tumors. Acta Neurochir 159, 1597–1601 (2017). https://doi.org/10.1007/s00701-017-3257-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-017-3257-2