Abstract
Background
Meningiomas are more prevalent in elderly individuals; however, the surgical outcome and prognostic factors in this age group are unclear. This retrospective study aimed to identify the prognostic factors of elderly patients with intracranial meningiomas who underwent surgical resection.
Methods
Eighty-six patients (aged ≥65) diagnosed with an intracranial meningioma were surgically treated at our department. The clinical, radiological, and follow-up data were retrospectively reviewed. Univariate and multivariate logistic analyses were performed to identify relationships between factors [age, sex, neurological condition, concomitant disease, American Society of Anesthesiology (ASA) classification, preoperative Karnofsky Performance Scale (KPS) score, tumor location and size, peritumoral edema, and Simpson resection grade] and outcome.
Results
One patient (1.2 %) died within 30 days of surgery. The morbidity rate was 37.2 %. Postoperative morbidities occurred more frequently in the patients with preoperative neurological deficits than in those without (p = 0.049). Univariate analysis identified significant relationships between a low KPS score (≤70) at discharge and preoperative neurological deficits, low preoperative KPS score (≤70), and critical tumor location (p < 0.001, p < 0.001, and p = 0.04, respectively). In the multivariate logistic analysis, only the preoperative KPS score remained significant for the KPS score at discharge (p = 0.005); there was no significant association with the most recent KPS score.
Conclusion
The outcome of intracranial meningioma resection in elderly individuals is favorable if the preoperative KPS score is >70 and no neurological deficits are present. Treatment decisions should be patient-specific, and additional factors should be considered when operations are performed in patients with a low preoperative KPS score or neurological deficits.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Meningiomas are the most common benign intracranial neoplasms and account for 13–26 % of all intracranial tumors [21]. Meningiomas may occur at any age; however, the prevalence increases with age, and the peak incidence rate occurs in the 6th and 7th decades of life [8, 37]. With the availability of advanced diagnostic imaging modalities, increasing human life expectancy, and an improvement in medical care insurance, an increasing number of meningiomas has been identified in elderly patients [2, 3, 8, 18, 19, 21, 26, 37].
Despite the current era of advanced microneurosurgery, surgical decisions for elderly patients remain difficult. As a result of increased surgical mortality and poor outcome in this age group, a more accurate and safe surgical intervention is required. Some authors have previously attempted to identify prognostic factors for surgical outcomes in elderly patients. Several factors were predictive of outcome, including patient factors, such as the neurological conditions and the preoperative Karnofsky Performance Scale (KPS) score, and tumor parameters, such as size and location [1, 7, 9–13, 27, 33]. However, other authors did not replicate these findings [2–4, 23].
Various grading score systems [1, 9, 15, 33] have been established for patient selection, such as the Clinical-Radiological Grading System (CRGS) [1], the Sex, KPS, ASA, Location of Tumor, and Peritumoral Edema (SKALE) grading system [33], and the Geriatric Scoring System (GSS) [9]. These grading score systems are reasonable and effective, and some systems have been validated [16, 34]. Because of the retrospective or small sample sizes of the currently available series, prospective, multicenter, and large sample studies are required to validate these grading systems.
There is no common consensus regarding the surgical interventions for meningiomas in elderly individuals. Furthermore, the prognostic factors of meningiomas in surgically treated elderly patients remain controversial.
The aim of this retrospective study was to identify prognostic factors for intracranial meningiomas in elderly patients older than 65 years of age who underwent surgical resection. The clinical data, radiological findings, and follow-up records were reviewed and evaluated.
Patients and methods
This study was approved by the institutional review board of Guangxi Medical University, and written informed consent was provided by the patients or their relatives.
Inclusion criteria
This retrospective study included 86 patients aged 65 years or older who were newly diagnosed with meningiomas. The patients underwent surgery between January 2007 and December 2013 in the Department of Neurosurgery of The First Affiliated Hospital of Guangxi Medical University.
Exclusion criteria
We excluded patients who received radiosurgery or surgical resection for tumor recurrence, as well as patients with multiple tumors.
Patient population
Eighty-six patients were included in the data analyses. There was a female bias with 55 females and 31 males (ages ranged from 65 to 86 years; mean age, 70 years). All patients were symptomatic at admission, with the exception of five who were incidentally identified. The most common symptom was headache, followed by dizziness and limb weakness. The average illness history duration was 16 months (range: 1 day to 240 months).
Clinical data
The preoperative performance status was retrospectively evaluated according to the KPS score. When the KPS score was >70, the patient’s neurological condition was rated as good. We chose a score of 70 as the cutoff because the patient was unable to perform normal activities or work, with a KPS score ≤70. During the neurological examination, different neurological deficits, such as visual impairment and muscle weakness, were identified in 49 patients. The general health conditions were assessed according to the American Society of Anesthesiology (ASA) classification. Elderly patients typically suffer from various systemic diseases; thus, we were not surprised to determine that approximately half of the study participants (46.5 %) exhibited other systemic diseases. Hypertension and diabetes mellitus were the most common diseases. Twenty-nine patients could control their concomitant diseases by medical treatment, whereas 11 did not have their concomitant diseases under control. The preoperative neurological and general health conditions of the patients are listed in Table 1. For statistical purposes, the neurological condition was divided into deficits and no deficits; concomitant diseases were divided into present and absent, and the ASA was divided into grades I or II and grades III or IV.
Imaging findings
All patients were evaluated via contrast-enhanced computed tomography (CT) or magnetic resonance imaging (MRI) prior to surgery. According to the classification of Caroli et al. [7], the tumor location was graded as critical if the lesion was located on an eloquent area and the brainstem or was next to major cerebral vessels or cranial nerves. The tumor size was defined as the maximum diameter on the contrast-enhanced MRI or CT scans. For statistical purposes, the lesion was divided into two types: <4 and ≥4 cm. Peritumoral edema was simplified into two categories: edema and without edema. All tumors were postoperatively confirmed by histological examination (according to the 2007 World Health Organization Classification [22]). Table 2 lists the distributions of tumor location; Table 3 summarizes the tumor characteristics.
Follow-up
All patients received their first follow-up at 3 months after surgery, which included a contrast-enhanced MRI. If the patients did not return for re-examination, we contacted them or their relatives by telephone. Mortality within 30 days was considered perioperative mortality.
Statistical analysis
Statistical analysis was performed using SPSS version 17 software (SPSS, Chicago, IL, USA). A univariate logistic regression analysis was utilized to correlate factors (sex, age, neurological condition, concomitant disease, ASA classification, preoperative KPS score, tumor location and size, peritumoral edema, and Simpson resection grade) with outcomes (mortality, morbidity, KPS score at discharge, and most recent KPS score). The KPS values before and after surgery were compared using a t-test. Differences in the length of stay among different groups were analyzed using a Mann-Whitney U test. Significance was defined as p < 0.05.
The potential prognostic variables associated with outcome (p < 0.1) in the univariate analysis were included in a multivariate logistic regression model.
Results
Extension of tumor removal
The extent of tumor removal was graded according to the Simpson classification [35]. Gross total resection was achieved in 67 patients (Simpson I in 43 patients and Simpson II in 24 patients), which comprised 77.9 % of the patients. Simpson grade III was achieved in 12 patients (14.0 %), whereas grade IV was achieved in seven patients (8.1 %).
Mortality
One patient died on the first day after the operation. Thus, the perioperative mortality was 1.2 %. The deceased patient was a 70-year-old male who exhibited a meningioma located on the falx with severe peritumoral edema. He died of diffuse cerebral edema and intracerebral hematoma. There were no other patients who died within 3 months after surgery (Table 4 displays information regarding all deceased patients).
Morbidity
Thirty-two of the patients (37.2 %) suffered from different complications, including surgical and medical complications (Table 5). Intracranial hematomas were the most frequent surgical morbidity (intracerebral hematoma in 9 cases and epidural hematoma in 1 case). Of the ten patients, two patients required a craniotomy to remove the intracranial hematomas. Most postoperative complications were non-fatal and ultimately improved via conservative management or rehabilitation.
Length of stay and place of discharge
The mean length of stay was 24.2 ± 10.3 days (range: 11–64 days). The mean lengths of stay for the patients with ASA I, II, and III/IV were 22.9, 23.1, and 27.8 days, respectively. The average length of stay was 26.8 days for the patients with concomitant diseases and 21.9 days for the patients without concomitant diseases. The patients with a high ASA or concomitant diseases required a significantly longer length of hospital stay (p = 0.032 and p = 0.01, respectively).
Most patients were discharged from the Neurosurgery Department after recovery, whereas only seven were discharged from other departments that provided rehabilitation (three patients were discharged from the Rehabilitation Department, three patients were discharged from the Department of Traditional Chinese Medicine, and one patient was discharged from the Department of Psychiatry).
KPS score at discharge
After surgical treatment, the number of patients with a KPS score of at least 80 at discharge was 65 (75.6 %). The mean KPS score at discharge was 79.4 ± 15.3 (range: 0–100). There was no significant difference between the mean preoperative and discharge KPS scores (p = 0.25).
Follow-up and most recent KPS score
During a mean follow-up period of 38.3 months (range: 3.2–86.2 months), 79 patients remained alive, 2 died of unrelated diseases, and 4 were lost to follow-up. The reason for the loss to follow-up was that the relatives of the elderly patients changed their telephone numbers.
We rated the quality of life as good when the most recent KPS score was >70, namely, the patients obtained a satisfactory quality of life. In contrast, the outcome was rated poor if the most recent KPS score was ≤70. The results were as follows: 65 patients (82.3 %) were rated as good (which included 13 patients rated 100, 35 rated 90, and 17 rated 80), whereas 14 patients (17.7 %) were rated as poor (which included 2 patients rated 70, 7 rated 60, 3 rated 50, 1 rated 40, and 1 rated 30).
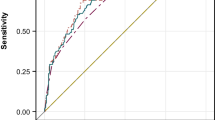
In the 79 living patients, the mean recent KPS score was 83.4 ± 15.0 (range: 30–100), which was significantly different from the mean preoperative KPS score (p = 0.005). We also compared the mean discharge and most recent KPS scores, and there was no significant difference between the two groups (p = 0.07). The KPS scores of the patients at admission, discharge, and the most recent follow-up are shown in Fig. 1.
Factors and outcomes
There was no significant relationship between mortality within 30 days and the preoperative factors or extension of tumor removal. According to the univariate analysis, a significant relationship between preoperative neurological deficits and morbidity was identified [odds ratio (OR) = 3.480, 95 % confidence interval (CI) = 1.329–9.111, p = 0.009]. There was no significant difference between the patients with low (≤70) versus high (>70) preoperative KPS scores (OR = 2.294, 95 % CI = 0.919–5.726, p = 0.072). When a multivariate logistic regression model was performed (which included the neurological condition and preoperative KPS score), the preoperative neurological deficits remained significant for morbidity (OR = 3.051, 95 % CI = 1.007–9.244, p = 0.049). The other factors, however, did not exhibit a significant contribution (the results of the univariate analysis and multivariate logistic regression are shown in Tables 6 and 7, respectively).
Preoperative neurological deficits and low KPS scores were associated with a low KPS score (≤70) at discharge (OR = 11.038, 95 % CI = 2.384–51.517, p < 0.001 and OR = 11.657, 95 % CI = 3.635–37.386, p < 0.001, respectively). The KPS score at discharge was lower in the patients who exhibited a lesion located on a critical region compared with the patients who exhibited a lesion located on a non-critical region (OR = 3.750, 95 % CI = 1.001–14.044, p = 0.04). The multivariate logistic regression indicated that only the preoperative KPS score remained significant (OR = 6.634, 95 % CI = 1.784–24.669, p = 0.005).
Regarding the most recent KPS score, no factors exhibited a significant contribution. It is worth noting that the patients with a high preoperative KPS score were likely to obtain a satisfactory quality of life (OR = 3.228, 95 % CI = 0.986–10.566, p = 0.092).
Discussion
Meningiomas are more frequently identified in elderly individuals. According to data from the Central Brain Tumor Registry of the US, the meningioma incidence rate is 8 per 100,000 individuals, and approximately 49 % of these individuals are older than 65 years of age [8]. Similarly, nationwide epidemiologic data from Korea in 2005 indicated the incidence of meningiomas increased with age and peaked in the 7th decade [19]. Thus, neurosurgeons will be more likely to encounter meningiomas in elderly patients, including patients who are asymptomatic. It is critical to develop criteria that can identify the patients who require surgical treatment, conservative management, or simple follow-up.
Mortality
According to published reports [1–7, 9–13, 15–17, 20, 23, 25, 27–34, 36], there are wide variations in surgical mortality, which have ranged from 0 to 45 % (Table 8 reviews an intracranial meningioma surgery series in elderly patients).
In the current study, one patient died perioperatively; thus, the surgical mortality was 1.2 %. Compared with other reports, this rate is relatively low regarding mortality but higher regarding morbidity. The inconsistency can be explained by the following reasons: (1) our patients were younger. The mean age of other reports was at least 70 years [1, 4, 6, 7, 12, 27, 33, 36], whereas the mean age in this group was 70 years. In general, younger individuals have an increased likelihood of survival because physiological function and operation tolerance are better compared with elderly patients. (2) Most complications were not fatal. Serious complications, such as pulmonary embolism or cardiorespiratory failure, did not occur in our patients. (3) Most patients were in good general condition preoperatively, and comorbidity could be controlled in 72 % of the patients; 76.7 % of the patients had an ASA I or II status.
Furthermore, the excellent surgical outcomes also depended on advances in microneurosurgical techniques, improvements in anesthesia management, and intensive care development.
Morbidity
The most common surgical complication was intracranial hematoma (11.7 %), followed by motor deficits (9.3 %). Postoperative morbidities occurred more frequently in the patients with neurological deficits. Forty-nine patients had preoperative neurological deficits to various degrees, including 24 patients who experienced postoperative complications. Only eight patients experienced complications in the absence of neurological deficits. Although we did not identify a significant relationship between morbidity and the preoperative KPS score, the morbidity was increased in the individuals with a preoperative KPS score ≤70 compared with >70. Previous studies [1, 7, 11–13, 27] have demonstrated an increase in mortality is associated with a low preoperative KPS score; however, the relationship between morbidity and preoperative KPS scores has rarely been addressed.
It is worth noting that intracranial hematomas are common after resection in elderly patients. According to previous studies, the occurrence rate ranged from 2.7 to 16 % [1, 11, 16, 33]. Gerlach et al. [14] retrospectively identified the risk factors for postoperative hematoma after the surgical resection of intracranial meningiomas. The authors demonstrated patients aged 65 years or older had an increased risk for postoperative hemorrhage and concluded that thrombocytopenia and platelet dysfunction were associated with postoperative hemorrhage after meningioma surgery. This finding was not surprising because elderly patients often exhibit cardiovascular diseases and are often chronically treated with antiplatelet agents.
Factors and outcome
Aging is often considered a factor that increases operative risks [9, 15, 20, 29, 33]; however, the majority of studies suggest that age is not a surgical contraindication [1, 6, 7, 25, 27, 33]. Our results also support this viewpoint.
Some authors [7, 9, 33] have reported females have an increased probability of survival. Although the deceased patients were male in our group, we could not confirm that females have a greater likelihood of survival because of the small sample size in our series.
Several published studies have demonstrated that poor preoperative neurological conditions were associated with poor surgical outcomes [11–13, 36]. Djindjian et al. [13] demonstrated that when patients underwent operations with a preoperative KPS score ≤40, the operative failure rate was 100 %; in their study, six patients died and two experienced severe disabilities. Cohen-Inbar et al. [9] emphasized a poor outcome was related to a poor preoperative neurological condition (KPS score ≤70). In our group, 56 patients exhibited a preoperative KPS score >70, and 51 of these patients continued to exhibit a KPS score >70 at discharge. However, only 14 patients with a preoperative KPS score ≤70 also exhibited a KPS score ≥70 at discharge. Furthermore, the neurological condition was associated with short-term outcome (KPS score at discharge) via univariate analysis. When a multivariate analysis was performed, no significant relationship between neurological condition and KPS score at discharge was identified. Because the preoperative KPS score and neurological condition are not independent, the KPS score may reflect the neurological condition to some extent.
Before a decision is made to perform an operation in patients, the tumor characteristics should be taken into account. The tumor parameters that affect the surgical outcome include peritumoral edema, size, and location [1, 4, 6, 7, 9–13, 33, 34]. Cornu et al. [11] reported that a tumor location on the base or in the posterior fossa was related to a poor outcome. In Sacko’s study [33], a critical location was associated with increased mortality in the first year after surgery, and more morbidities occurred in the patients with a critical tumor location. According to our data, 31.4 % of the tumors were located on the base and 67.6 % were located in a critical region. D’Andrea et al. [12] demonstrated an increased postoperative morbidity associated with a larger maximum tumor diameter. This relationship was also confirmed by Sacko [33]. However, the tumor location and size were not associated with outcome in our patients. Many conflicting results regarding the prognostic value of peritumoral edema have been presented [1, 6, 12, 13, 27, 28, 33, 36]. Various classifications have been utilized to define the edema extent [1, 33]; thus, we could not select the most predictive classification for our study. Therefore, we divided the peritumoral edema into those with and without edema. However, we failed to identify a significant prognostic value of peritumoral edema. A comprehensive evaluation of these tumor factors will enable clinicians to more precisely evaluate the risk of surgery and the predictive value.
As a result of advances in anesthetic techniques, we performed operations on patients who exhibited a strong desire to undergo an operation, regardless of an ASA IV or V. In contrast, Nakamura et al. [25] did not perform surgery for patients with ASA IV–V. Some neurosurgeons have suggested the ASA assessment prior to surgery is necessary [4, 11, 12, 25, 33]. A higher ASA is typically associated with a poor outcome. In Sacko et al. [33], 70.2 % of the patients exhibited an ASA III-IV status, and the 1-year mortality rate was 11.5 %. We failed to identify similar results compared with this study. In our study, the morbidity and short- and long-term outcomes were not affected by a high ASA status or concomitant diseases. However, patients with a high ASA or uncontrolled concomitant diseases required additional recovery time and an increased length of hospital stay.
The aggressive resection of meningiomas in elderly individuals can increase morbidity and mortality and is thought to be risky. D’Andrea et al. [12] affirmed that radical resection could increase morbidity. In their series, a gross total resection was performed in 30 patients, and 5 patients died during the postoperative period. To date, an increasingly greater number of neurosurgeons agree with the philosophy that it is not essential to attain total tumor removal. We should attempt to remove tumors with the greatest extent of nerve function preservation to maintain the ability of patients to pursue a satisfactory quality of life post-surgery. The life expectancy of elderly individuals is less than that of young individuals; in addition to the slow-growing feature of meningiomas, it is critical to preserve nerve function in elderly individuals. Nakamura et al. [24] identified 41 meningiomas in asymptomatic patients via imaging. The findings indicated tumor growth was associated with patient age, and the annual growth rates tended to be lower in elderly individuals. We advocate the primary aim of an operation for elderly individuals is to alleviate symptoms and improve their quality of life. Our gross total resection rate is not high compared with previous studies; however, the long-term outcome was favorable. Thus, it appears that “survival with residual tumor” is acceptable in this age population.
Limitations
This study used retrospective data collection. We did not follow up regarding the patients who were treated conservatively or received radiosurgery to assess their outcomes. Unfortunately, we cannot provide data regarding the patients who refused surgery; therefore, there is an element of bias within the cohort, i.e., self-selection. The decision to operate was subjective, and we did not apply a protocol or criteria. Prospective and large sample studies must be performed to identify prognostic factors and surgical selection criteria for elderly patients with intracranial meningioma.
Conclusion
Age is not a contraindication to surgery in elderly individuals. The outcome of intracranial meningioma resection in the aged population is favorable when patients have no neurological deficits and a preoperative KPS score >70. When a decision regarding surgery is made for patients with a low preoperative KPS score or neurological deficits, we should consider additional factors, such as the preoperative general health condition, tumor characteristics, and patient perspectives. Thus, the decision-making should be tailored to the individual patient.
References
Arienta C, Caroli M, Crotti F, Villani R (1990) Treatment of intracranial meningiomas in patients over 70 years old. Acta Neurochir 107:47–55
Awad IA, Kalfas I, Hahn JF, Little JR (1989) Intracranial meningiomas in the aged: surgical outcome in the era of computed tomography. Neurosurgery 24:557–560
Bateman BT, Pile-Spellman J, Gutin PH, Berman MF (2005) Meningioma resection in the elderly: nationwide inpatient sample, 1998–2002. Neurosurgery 57:866–872, discussion 866–872
Black P, Kathiresan S, Chung W (1998) Meningioma surgery in the elderly: a case–control study assessing morbidity and mortality. Acta Neurochir 140:1013–1016, discussion 1016–1017
Boviatsis EJ, Bouras TI, Kouyialis AT, Themistocleous MS, Sakas DE (2007) Impact of age on complications and outcome in meningioma surgery. Surg Neurol 68:407–411, discussion 411
Buhl R, Hasan A, Behnke A, Mehdorn HM (2000) Results in the operative treatment of elderly patients with intracranial meningioma. Neurosurg Rev 23:25–29
Caroli M, Locatelli M, Prada F, Beretta F, Martinelli-Boneschi F, Campanella R, Arienta C (2005) Surgery for intracranial meningiomas in the elderly: a clinical-radiological grading system as a predictor of outcome. J Neurosurg 102:290–294
Claus EB, Bondy ML, Schildkraut JM, Wiemels JL, Wrensch M, Black PM (2005) Epidemiology of intracranial meningioma. Neurosurgery 57:1088–1095, discussion 1088–1095
Cohen-Inbar O, Soustiel JF, Zaaroor M (2010) Meningiomas in the elderly, the surgical benefit and a new scoring system. Acta Neurochir 152:87–97, discussion 97
Cohen-Inbar O, Sviri GE, Soustiel JF, Zaaroor M (2011) The Geriatric Scoring System (GSS) in meningioma patients—validation. Acta Neurochir 153:1501–1508, discussion 1508
Cornu P, Chatellier G, Dagreou F, Clemenceau S, Foncin JF, Rivierez M, Philippon J (1990) Intracranial meningiomas in elderly patients. Postoperative morbidity and mortality. Factors predictive of outcome. Acta Neurochir 102:98–102
D’Andrea G, Roperto R, Caroli E, Crispo F, Ferrante L (2005) Thirty-seven cases of intracranial meningiomas in the ninth decade of life: our experience and review of the literature. Neurosurgery 56:956–961, discussion 956–961
Djindjian M, Caron JP, Athayde AA, Fevrier MJ (1988) Intracranial meningiomas in the elderly (over 70 years old). A retrospective study of 30 surgical cases. Acta Neurochir 90:121–123
Gerlach R, Raabe A, Scharrer I, Meixensberger J, Seifert V (2004) Post-operative hematoma after surgery for intracranial meningiomas: causes, avoidable risk factors and clinical outcome. Neurol Res 26:61–66
Grossman R, Mukherjee D, Chang DC, Bennett R, Brem H, Olivi A, Quinones-Hinojosa A (2011) Preoperative charlson comorbidity score predicts postoperative outcomes among older intracranial meningioma patients. World Neurosurg 75:279–285
Konglund A, Rogne SG, Helseth E, Meling TR (2013) Meningioma surgery in the very old—validating prognostic scoring systems. Acta Neurochir 155:2263–2271, discussion 2271
Konglund A, Rogne SG, Lund-Johansen M, Scheie D, Helseth E, Meling TR (2013) Outcome following surgery for intracranial meningiomas in the aging. Acta Neurol Scand 127:161–169
Kuratsu J, Ushio Y (1997) Epidemiological study of primary intracranial tumours in elderly people. J Neurol Neurosur Psychiatr 63:116–118
Lee CH, Jung KW, Yoo H, Park S, Lee SH (2010) Epidemiology of primary brain and central nervous system tumors in Korea. J Korean Neurosurg Soc 48:145–152
Lieu AS, Howng SL (1998) Surgical treatment of intracranial meningiomas in geriatric patients. Kaohsiung J Med Sci 14:498–503
Louis DN, Scheithauer BW, Budka H, von Deimling A, Kepes JJ (2000) Meningiomas. In: Kleihues P, Cavenee WK (eds) Pathology and genetics of tumours of the nervous system: World Health Organisation classification of tumours. IARC Press, Lyon, pp 176–184
Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, Scheithauer BW, Kleihues P (2007) The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol 114:97–109
Mastronardi L, Ferrante L, Qasho R, Ferrari V, Tatarelli R, Fortuna A (1995) Intracranial meningiomas in the 9th decade of life: a retrospective study of 17 surgical cases. Neurosurgery 36:270–274
Nakamura M, Roser F, Michel J, Jacobs C, Samii M (2003) The natural history of incidental meningiomas. Neurosurgery 53:62–70, discussion 70–61
Nakamura M, Roser F, Dormiani M, Vorkapic P, Samii M (2005) Surgical treatment of cerebellopontine angle meningiomas in elderly patients. Acta Neurochir 147:603–609, discussion 609–610
Niiro M, Yatsushiro K, Nakamura K, Kawahara Y, Kuratsu J (2000) Natural history of elderly patients with asymptomatic meningiomas. J Neurol Neurosur Psychiatr 68:25–28
Nishizaki T, Kamiryo T, Fujisawa H, Ohshita N, Ishihara H, Ito H, Aoki H (1994) Prognostic implications of meningiomas in the elderly (over 70 years old) in the era of magnetic resonance imaging. Acta Neurochir 126:59–62
Papo I (1983) Intracranial meningiomas in the elderly in the CT scan era. Acta Neurochir 67:195–204
Patil CG, Veeravagu A, Lad SP, Boakye M (2010) Craniotomy for resection of meningioma in the elderly: a multicentre, prospective analysis from the national surgical quality improvement program. J Neurol Neurosur Psyciatr 81:502–505
Poon MT, Fung LH, Pu JK, Leung GK (2013) Outcome comparison between younger and older patients undergoing intracranial meningioma resections. J Neuro-Oncol 114:219–227
Poon MT, Fung LH, Pu JK, Leung GK (2014) Outcome of elderly patients undergoing intracranial meningioma resection—a systematic review and meta-analysis. Br J Neurosurg 28:303–309
Proust F, Verdure L, Toussaint P, Bellow F, Callonec F, Menard JF, Freger P (1997) Intracranial meningioma in the elderly. Postoperative mortality, morbidity and quality of life in a series of 39 patients over 70 years of age. Neurochirurgie 43:15–20
Sacko O, Sesay M, Roux FE, Riem T, Grenier B, Liguoro D, Loiseau H (2007) Intracranial meningioma surgery in the ninth decade of life. Neurosurgery 61:950–954, discussion 955
Schul DB, Wolf S, Krammer MJ, Landscheidt JF, Tomasino A, Lumenta CB (2012) Meningioma surgery in the elderly: outcome and validation of 2 proposed grading score systems. Neurosurgery 70:555–565
Simpson D (1957) The recurrence of intracranial meningiomas after surgical treatment. J Neurol Neurosur Psychiatr 20:22–39
Umansky F, Ashkenazi E, Gertel M, Shalit MN (1992) Surgical outcome in an elderly population with intracranial meningioma. J Neurol Neurosur Psychiatr 55:481–485
Wiemels J, Wrensch M, Claus EB (2010) Epidemiology and etiology of meningioma. J Neuro-Oncol 99:307–314
Acknowledgments
We would like to thank the neurosurgeons and staff of The First Affiliated Hospital of Guangxi Medical University for their excellent work. We thank Medjaden Bioscience, Ltd., for assisting in the preparation of this manuscript.
Patient consent
The patients or their relatives consented to study participation and the use of their data for research purposes.
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Our Chinese colleaques retrospectively analyzed prognostic factors for the outcome in 86 elderly (≥65 years) patients after a microsurgical removal of an intracranial meningioma. But their task was impossible—only one variable in the cohort was rather constant, i.e., modern microneurosurgery in advanced services, but two were highly variable, i.e., intracranial meningiomas (size/site/adherence to adjacent structures) and elderly patients (neurological deficits/concomitant diseases and medications/previous neurocardiovascular events)—at least in unselected population-based services.
Let's try an Individual Risk Calculator of Operative 12-month Mortality and Morbidity of Intracranial Meningiomas in the Elderly based on the authors’ multivariate analysis data. What would the risk of operative 1- or 12-month mortality be for this 70-year-old female, a retired cardiologist, with treated hypertension and anticoagulation because of atrial fibrillation, now presenting with a suprasellar meningioma and rapidly reduced visual acuity not allowing an independent life any more? This is not possible because there are only seven tuberculum sellae meningiomas in their series, etc. The individual risk calculator would require 8600 rather than 86 patients. The authors conclude that ‘prospective and large sample studies must be performed to identify prognostic factors and surgical selection criteria for elderly patients with intracranial meningioma.’ I don't think so because that effort would exceed our combined capacity. But I totally agree that ‘treatment decisions should be patient-specific.’
Who then is elderly? My official retirement age is 68 years. If I then had a 5-cm falcine meningioma with focal seizures in the left foot, what would my neurosurgeon, orginally trained by me, tell me, and in what tone, about my possible outcome and complications?—Professor, considering your age, I am sorry to tell that your left foot will most probably remain weaker than it is now and the risk of venous infarctions from occlusion of bridging veins…
Juha E Jääskeläinen
Kuopio Finland
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 228 kb)
Rights and permissions
About this article
Cite this article
Chen, ZY., Zheng, CH., Tang Li et al. Intracranial meningioma surgery in the elderly (over 65 years): prognostic factors and outcome. Acta Neurochir 157, 1549–1557 (2015). https://doi.org/10.1007/s00701-015-2502-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-015-2502-9