Abstract
Background
We used [F-18] FDG microPET imaging as part of a longitudinal study to investigate changes in the brain.
Methods
Glucose metabolism during the development of neuropathic pain after tibial and sural nerve transection (TST) model rats. MicroPET images were obtained 1 week before operation and then weekly for 8 weeks post-operation.
Results
The behavioral test was performed immediately after the every FDG administration. After TST modeling, neuropathic pain rats showed increased mechanical sensitivity of the injured hind paw. The withdrawal response to mechanical pain stimulation by von Frey filaments was observed within the first week (3.8 ± 0.73), and it rapidly increased in the third week (7.13 ± 0.82). This response reached a peak in the fourth week after surgery (9.0 ± 0.53), which persisted until the eighth week. In microPET scan imaging, cerebellum, which initially started from the ansiform lobule, was activated gradually to all part from the third week in all image acquisitions through the eighth week.
Conclusions
The longitudinal microPET scan study of brains from neuropathic pain rat models showed sequential cerebellar activity that was in accordance with results from behavioral test responses, thus supporting a role for the cerebellum in the development of neuropathic pain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neuropathic pain is a neurodegenerative disease caused by lesions or dysfunction of the central or peripheral nervous system, and it is one of the most difficult pains to control because it is a multidimensional clinical entity mediated by many different pathophysiological mechanisms [2, 8, 15, 48].
Recently, there have been a number of studies evaluating the processing of pain in the brain by positron emission tomography (PET) or functional magnetic resonance imaging (fMRI), and these studies have shown changes in brain activity indicating the network of brain areas involved in forming a pain matrix [3, 27, 30, 31, 33, 41, 47]. The primary and secondary somatosensory cortices, insular cortex, anterior cingulate cortex, thalamus, and prefrontal cortex were the sites that were consistently activated in response to pain [1, 10, 32, 46]. In addition to these lateral and medial pain systems, the brainstem, amygdale, basal ganglia, and cerebellum are also related to the processing of nociceptive information and pain perception, but the details of their roles have not been clearly demonstrated yet [6]. Further, imaging studies for neuropathic pain have been reported using a resting state as well as stimulus-induced state, but these studies also only reflect the static states of the brain activities related to neuropathic pain. Although there have been few imaging studies based on the longitudinal acquisition of data on nociceptive pain processing, imaging studies during the development of neuropathic pain are lacking [35, 42]. Therefore, we performed a longitudinal study with [F-18] FDG microPET imaging to investigate changes in brain glucose metabolism during development of neuropathic pain.
Materials and methods
Animals and surgical procedures
A total of 15 male Sprague–Dawley rats (6 weeks old, weighing approximately 180–200 g) were used in this experiment. All 15 rats were operated on to induce neuropathic pain, but only 13 were confirmed to have neuropathic pain based on behavioral test results. Therefore, 13 rats were included for PET scans.
The rats were housed in groups of five per cage with food and water available ad libitum under a 12-h light/dark cycle. To induce peripheral neuropathic pain, we anesthetized the rats using pentobarbital sodium (50 mg/kg) and a segment of the left sciatic nerve was exposed. For the TST (tibial and sural transection) model, the left tibial and sural nerves were tightly ligated and completely transected, leaving the common peroneal nerve intact.
This study was conducted according to the guideline of the Ethical Committee of International Association for the Study of Pain [49] and the Institution Animal Care and Use Committee of Yonsei University. Every effort was made to minimize animal suffering, to reduce the number of animals used, and to utilize alternatives to in vivo techniques.
Mechanical hyperalgesia by von Frey test
To measure mechanical hyperalgesia, rats were placed on a metal mesh floor under a custom-made transparent plastic dome (8 × 8 × 18 cm) and innocuous mechanical stimuli were applied with a von Frey filament (8 mN bending force) ten times (once every 3–4 s) to the sensitive area of each hind paw. The frequency of foot withdrawal was expressed as a percentage that was used as the index of mechanical hyperalgesia.
[F-18] FDG microPET acquisition
[F-18] FDG was used to reveal brain glucose metabolism. One week before the induction of neuropathic pain, baseline [F-18] FDG PET scans were performed in all 13 rats as a control. Each rat was in a cage at 30 °C for 30 min before [F-18] FDG injection for adaptation. [F-18] FDG (0.5 mCi/100 g) was administrated via the lateral vein of the tail. After administration, the rat was in the conscious state inside the cage for 60 min, and during that period, we performed a behavioral test to encourage glucose uptake. Following FDG uptake, the rat was initially anesthetized with 5 % isoflurane (O2: 1.5 l/min, with vacuum). Then, we fixed the head to minimize the motion artifacts. Under a maintenance dose of 2 % isoflurane (O2: 1.0 l/min, with vacuum), the microPET scanning was performed for 60 min. While the scanning image was taken by using microPET, the body temperature was maintained with a heating pad using a warm sensor. Every week until the eighth week after the induction of neuropathic pain through operation, behavioral tests were performed and [F-18] FDG PET scans were done.
[F-18] FDG microPET data analysis
In order to improve the accuracy for anatomical locations, the MRI scan was co-registered on [F-18] FDG microPET scan. [F-18] FDG microPET images were reconstructed using the ordered subset expectation maximization (OSEM) algorithm with ten iterations. The nominal pixel size was 0.43 × 0.43 × 0.81 mm3. For statistical analysis, only the brain regions within the [F-18] FDG microPET images were manually extracted. To make the [F-18] FDG rat brain templates, baseline images (n = 12) were coregistered to the respective images and resliced with trilinear interpolation (0.4 × 0.4 × 0.4 mm3) using SPM5 (http://www.fil.ion.ucl.ac.uk/spm). Individual images were averaged to create a [F-18] FDG rat brain template. Then, the template was normalized to the MRI template for accurate anatomical information, which was placed in stereotaxic space [40]. All individual images were normalized using the [F-18] FDG rat brain template. To increase the statistical power, all the individual normalized images were smoothed with an isotropic Gaussian kernel (2 mm FWHM). Voxel-based statistical analyses were carried out with statistical parametric mapping. Proportional scaling was used for global normalization. The statistical threshold was set at p < 0.05 (family-wise error correction) with an extent threshold of 100 contiguous voxels. T-value maps of results were overlaid on transverse views of the MRI template to define voxels that showed significant change. For the analysis of correlations among the brain areas with significant metabolic changes, average glucose metabolism in each activated or deactivated brain region was calculated with all voxels within 1 mm at the Paxinos position of each region. Pearson’s correlation coefficients among regions of interest were calculated (p < 0.01, two-tailed).
The baseline images from before the induction of neuropathic pain operation and the images from each week after operation were compared.
Results
Behavioral test after TST model
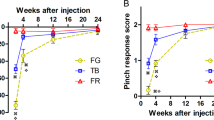
After TST modeling, neuropathic pain rats showed increased mechanical sensitivity of the injured hind paw. The withdrawal response to mechanical pain stimulation by von Frey filaments was observed within the before surgery to neuropathic pain (0.62 ± 0.14) in pain group, and it rapidly increased in the third week (5.24 ± 0.56). This response reached a peak in the seventh week after surgery (6.63 ± 0.64), and persisted until the eighth week. Conversely, in the normal group, the behavioral results from before surgery (0.61 ± 0.21), and it persisted until the eighth week (Figs. 1 and 2). The withdrawal responses confirmed the induction of neuropathic pain.
a Primary motor cortex was activated from the first to third week after operation, but primary sensory cortex and whole cerebellum, which initially started from the ansiform lobule, were activated in all the image acquisitions through the eighth week. The inferior colliculus showed activation in the second week that was maintained until the eighth week. The ventral posteromedial thalamic nucleus was activated from the sixth to the eighth week
[F-18] FDG microPET scan
Primary motor cortex (AP: 0.4 mm; ML: 2.2 mm; DV: 2.0 mm) was revealed as an active area from the first to third week after operation, whereas the primary sensory cortex (AP: 1.0 mm; ML: −4.0 mm; DV: 2.0 mm) and whole cerebellum, which initially started from the ansiform lobule (AP: −13.6 mm; ML: 2.4 mm; DV: 3.2 mm), were activated in all the image acquisitions through the eighth week. The cerebellar uptake gradually increased in the third week, and after the forth week, the whole cerebellum was activated. The inferior colliculus (AP: −9.0 mm; ML: ±1.8 mm; DV: 4.0 mm) showed activation in the second week that was maintained into the eighth week. The ventral posteromedial thalamic nucleus (AP: −3.6 mm; ML: 2.6 mm; DV: 6.6 mm) was activated from the sixth to eighth week (Figs. 3a, c and 4).
a Primary motor cortex (AP: 0.4 mm; ML: 2.2 mm; DV: 2.0 mm) was active from the first to third week after operation, but primary sensory cortex (AP: 1.0 mm; ML: −4.0 mm; DV: 2.0 mm) and whole cerebellum, which initially started from the ansiform lobule (AP: −13.6 mm; ML: 2.4 mm; DV: 3.2 mm), were activated in all the image acquisitions through the eighth week. The inferior colliculus (AP: −9.0 mm; ML: ±1.8 mm; DV: 4.0 mm) showed activation in the second week that was maintained until the eighth week. The ventral posteromedial thalamic nucleus (AP: −3.6 mm; ML: 2.6 mm; DV: 6.6 mm) was activated from the sixth week to the eighth week. b Primary and secondary motor cortex of the contralateral side (AP: 4.2 mm; ML: ±2.4 mm; DV: 2.0 mm) and substantia nigra (AP: −6.4 mm; ML: −2.0 mm; DV: 8.0 mm) were gradually deactivated from the first through eighth week. The fornix (AP: −0.4 mm; ML: 0.6 mm; DV: 6.4 mm) and insula cortex (AP: 3.2 mm, ML: −3.8 mm, DV: 5.8 mm) were deactivated in the third and forth weeks, respectively. After the fifth week, the hippocampus (AP: −4.4 mm; ML: 0.6 mm; DV: 3.8) was deactivated, and after the sixth week, the nucleus accumbens (AP: 1.0 mm; ML: 0.8 mm; DV: 7.0 mm) and retrosplenial cortex (AP: −5.4 mm; ML: ±0.4 mm; DV: 2.6 mm) were deactivated. c Glucose metabolism changes in the cerebellum of the neuropathic pain rat model. The cerebellum showed significantly progressive activation in glucose metabolism compared with baseline (p < 0.001)
The primary and secondary motor cortex of the contralateral side (AP: 4.2 mm; ML: ±2.4 mm; DV: 2.0 mm) and substantia nigra (AP: −6.4 mm; ML: −2.0 mm; DV: 8.0 mm) were gradually deactivated from the first through the eighth week. The fornix (AP: −0.4 mm; ML: 0.6 mm; DV: 6.4 mm) and insular cortex (AP: 3.2 mm, ML: −3.8 mm, DV: 5.8 mm) began to deactivate from the third and forth week, respectively. After the fifth week, the hippocampus (AP: −4.4 mm; ML: 0.6 mm; DV: 3.8) was deactivated, and after the sixth week, the nucleus accumbens (AP: 1.0 mm; ML: 0.8 mm; DV: 7.0 mm) and retrosplenial cortex (AP: −5.4 mm; ML: ±0.4 mm; DV: 2.6 mm) were deactivated (Fig. 3b).
Discussion
In our microPET images acquired after stimulus, we observed longitudinal metabolic changes in the rat brain occurring in parallel with induced neuropathic pain for eight sequential weeks. Images from between the first and second week, compared with images of normal phase, showed that brain metabolic activity increased in the contralateral side of the primary motor cortex, primary sensory cortex, posterior thalamic nuclear group and crus II of the ansiform lobule of cerebellum. Cerebellar uptake is expected in the early phase because it is part of the pain matrix, including the thalamus, primary somatosensory cortex/primary motor cortex, secondary somatosensory cortex, midbrain, anterior insula, anterior cingulate cortex, and ventrolateral prefrontal cortex [10, 18, 32], and the uptakes in these sites, which are known as the lateral pain system, may be the result of nociceptive pain evoked by operation. From the third week, the central nucleus of the inferior colliculus and almost all of the cerebellum showed increased activity whereas the periaqueductal gray matter and primary and secondary motor cortex activity decreased. Interestingly, a good correlation was observed between the metabolic increase in the cerebellum on microPET and withdrawal rate of behavioral tests after peripheral nerve injury. The rate of the withdrawal response to mechanical allodynia of the ipsilateral hind paw slowly increased, and after the third week, the increment reached a maximal point that persisted for the length of the study (8 weeks). These findings suggest that changes in metabolic activity over time could reflect the development of surgery-induced neuroplastic adaptive modification, shifting to pain modulation of the cerebellum in response to nociceptive and neuropathic pain. From the sixth week, the nuclei of the brainstem also showed gradual uptake. The nuclei of the brainstem, such as the pons and the medulla oblongata, are known to participate in the descending modulation of nociception [25]. This finding indicates that the descending pain modulation process is also activated after neuropathic pain.
The spinothalamic system is known as the major route for transmitting nociceptive information to the cerebral cortex [9]. Still, the cortical targets of this system are unclear. A recent study showed that the spinothalamic system targets mainly the insula [13], and the appearance of deactivation in the insula on the forth week of our stimulus-evoked study may be the result of the advent of neuropathic pain. Near completion of the neuropathic pain model showed some changes from the sixth-week image studies. With regards to both affective and sensory aspects of altered pain perception, anatomical changes in the brain regions after chronic neuropathic pain have been reported [42]. The posterior cingulate cortex, which does not exist in rats, and retrosplenial cortex, showed important roles in pain processing in several studies, and the volume of the cortex decreased with chronic pain from other etiologies [4, 23]. Deactivation of the retrosplenial cortex after the sixth week in our study is in accordance with these results. The ascending nociceptive control pathway mediates pain-induced analgesia, and the nucleus accumbens is one of the structures that has specific mechanisms related to this pathway [37–39]. The role of the nucleus accumbens in the pain modulation pathway, such as antinociception or functional defensive behavior, has been studied [26, 44]. We observed deactivation of the nucleus accumbens and retrosplenial cortex in the sixth week after neuropathic pain induction. This deactivation is thought to be similar to the relative decrease in thalamic regional cerebral blood flow given the compensatory mechanism for inhibiting excessive nociceptive input after a behavioral test [17, 27].
The cerebellum is thought to be involved in a wide range of tasks, including sensorimotor control, language, spatial, and executive functions. Recent studies have consistently shown that the cerebellum may have a role in sensory processing including nociception [5, 28, 36] but its significance for pain processing largely remains unknown. From animal and human studies, it is known that peripheral afferent sensory inputs may activate the cerebellum. The input from stimulation of A-delta and C fiber nociceptors passes via climbing and mossy fibers to reach Purkinje cells in the cerebellum [14, 19]. Early cerebellar uptake in our images is due to the nociceptive signal from spontaneous pain induced by operation. With advances in technology, recent studies have revealed functional topography of the cerebellum as the presence of sensorimotor homunculi and association area projection in cerebellar lobules [16, 20, 43]. In the first and second weeks of the study, the crus II of the cerebellum was activated, which is in accordance with the sensory input pathway to the cerebellum, but after the third week, almost all cerebellar uptake was noted, which is in contrast to results from previous studies. It is well known that cerebellar activity from motor withdrawal and nociceptive sensory processing is indistinguishable by functional imaging [11, 24]. One of the different points of our study is that we acquired the images from the resting state, while previous studies obtained their results under noxious or non-noxious stimulation.
Romero et al. showed cerebellar activation in their microPET study of a rat model of surgery-induced latent pain sensitization, and it was nociceptive pain that reflected the slow development of surgery-induced neuroplastic adaptative modification [35]. However, our microPET study showed activation of the cerebellum as time passed after nerve injury, and the uptake was correlated with the results of the behavioral test for neuropathic pain. The glucose metabolism of the cerebellum increased until 3 weeks and reached steady state from 4 to 8 weeks. These longitudinal metabolic changes without external stimulation could be the result of an adaptive or modulating process, especially in the cerebellum. Borsook et al. reported that painful external stimuli in chronic neuropathic pain patients activated cerebellar areas related to cognitive processing as well as sensory-motor integration and secondary sensory processing [7]. Our whole cerebellar uptake suggests that the cerebellar response to neuropathic pain is not only encoding pain modulation, but also cognitive modulation, and the whole cerebellar activation could be the result of rhythmic sensorimotor synchronization, although there is still no consensus on the cerebellar timekeeping function. After the cessation of neuropathic pain, the peripheral nerve-injured rat, in ordinary time, may experience pain and adapt to produce a sequential or coincidence motor response to such pain. Although resting state of our study, the cerebellum, as a pain modulation region, could be activated, and this finding persisted into the eighth week of our investigation. Though there has not been thorough research into the putative comparative role of the cerebellum in anticipation of pain, the difference in spatial locations of the anticipatory and pain activation, as reported by Restuccia et al., suggests that multiple parts of the cerebellum respond to pain in different ways [21, 29, 34, 45].
From our behavioral tests of mechanical stimulation, the withdrawal response rate manifested within with the first week and reached a maximum after 4 weeks, and this rapid peripheral nerve injury-specific remodeling of cortical circuit responses was verified as being associated with neuropathic pain development.
Our study has some limitations. Specifically, we used an anesthetic material that could affect the uptake of neurons, and we did not get any images after the eighth week. In animal models used for neuropathic pain study, neuropathic pain established by transection or partial crush of peripheral nerve maintained for over or less than 8 weeks [12]. It is different from neuropathic pain in human patients. Generally, patients with neuropathic pain suffer from pain for their entire lives, but animal models of neuropathic pain cannot mimic this long-lasting feature, even though those animal models are well mimicking algesia and allodynia [12, 22]. We suppose that this could have resulted from artificial manipulation of the animal’s nervous system. Therefore, we performed our microPET study for 8 weeks.
Even with these limitations, the longitudinal microPET scans of peripheral nerve-injured rat brains showed sequential cerebellar uptake that was in accordance with behavioral test responses. In conclusion, the cerebellum, an integrator of multiple effector systems related to pain, is thought to be involved not only in sensorimotor processing but also affective processing and pain modulation. Our longitudinal microPET scan study of peripheral nerve-injured rat brains showed sequential cerebellar activity that was in concordance with behavioral test responses, thus supporting a role of the cerebellum in the processing of neuropathic pain.
References
Apkarian AV, Bushnell MC, Treede RD, Zubieta JK (2005) Human brain mechanisms of pain perception and regulation in health and disease. Eur J Pain 9:463–484
Baron R (2006) Mechanisms of disease: neuropathic pain–a clinical perspective. Nat Clin Pract Neurol 2:95–106
Becerra L, Morris S, Bazes S, Gostic R, Sherman S, Gostic J, Pendse G, Moulton E, Scrivani S, Keith D, Chizh B, Borsook D (2006) Trigeminal neuropathic pain alters responses in CNS circuits to mechanical (brush) and thermal (cold and heat) stimuli. J Neurosci 26:10646–10657
Bentley DE, Derbyshire SW, Youell PD, Jones AK (2003) Caudal cingulate cortex involvement in pain processing: an inter-individual laser evoked potential source localisation study using realistic head models. Pain 102:265–271
Bingel U, Quante M, Knab R, Bromm B, Weiller C, Buchel C (2002) Subcortical structures involved in pain processing: evidence from single-trial fMRI. Pain 99:313–321
Bingel U, Tracey I (2008) Imaging CNS modulation of pain in humans. Physiology (Bethesda) 23:371–380
Borsook D, Moulton EA, Tully S, Schmahmann JD, Becerra L (2008) Human cerebellar responses to brush and heat stimuli in healthy and neuropathic pain subjects. Cerebellum 7:252–272
Bouhassira D, Attal N, Fermanian J, Alchaar H, Gautron M, Masquelier E, Rostaing S, Lanteri-Minet M, Collin E, Grisart J, Boureau F (2004) Development and validation of the Neuropathic Pain Symptom Inventory. Pain 108:248–257
Craig AD (2003) Pain mechanisms: labeled lines versus convergence in central processing. Annu Rev Neurosci 26:1–30
Davis KD (2000) The neural circuitry of pain as explored with functional MRI. Neurol Res 22:313–317
Dimitrova A, Kolb FP, Elles HG, Maschke M, Forsting M, Diener HC, Timmann D (2003) Cerebellar responses evoked by nociceptive leg withdrawal reflex as revealed by event-related FMRI. J Neurophysiol 90:1877–1886
Dowdall T, Robinson I, Meert TF (2005) Comparison of five different rat models of peripheral nerve injury. Pharmacol Biochem Behav 80:93–108
Dum RP, Levinthal DJ, Strick PL (2009) The spinothalamic system targets motor and sensory areas in the cerebral cortex of monkeys. J Neurosci 29:14223–14235
Ekerot CF, Garwicz M, Schouenborg J (1991) The postsynaptic dorsal column pathway mediates cutaneous nociceptive information to cerebellar climbing fibres in the cat. J Physiol 441:275–284
Finnerup NB, Otto M, McQuay HJ, Jensen TS, Sindrup SH (2005) Algorithm for neuropathic pain treatment: an evidence based proposal. Pain 118:289–305
Grodd W, Hulsmann E, Ackermann H (2005) Functional MRI localizing in the cerebellum. Neurosurg Clin N Am 16:77–99, v
Iadarola MJ, Max MB, Berman KF, Byas-Smith MG, Coghill RC, Gracely RH, Bennett GJ (1995) Unilateral decrease in thalamic activity observed with positron emission tomography in patients with chronic neuropathic pain. Pain 63:55–64
Ingvar M (1999) Pain and functional imaging. Philos Trans R Soc Lond B Biol Sci 354:1347–1358
Jie W, Pei-Xi C (1992) Discharge response of cerebellar Purkinje cells to stimulation of C-fiber in cat saphenous nerve. Brain Res 581:269–272
Kelly RM, Strick PL (2003) Cerebellar loops with motor cortex and prefrontal cortex of a nonhuman primate. J Neurosci 23:8432–8444
Keltner JR, Furst A, Fan C, Redfern R, Inglis B, Fields HL (2006) Isolating the modulatory effect of expectation on pain transmission: a functional magnetic resonance imaging study. J Neurosci 26:4437–4443
Lee BH, Won R, Baik EJ, Lee SH, Moon CH (2000) An animal model of neuropathic pain employing injury to the sciatic nerve branches. Neuroreport 11:657–661
Lenz FA, Rios M, Zirh A, Chau D, Krauss G, Lesser RP (1998) Painful stimuli evoke potentials recorded over the human anterior cingulate gyrus. J Neurophysiol 79:2231–2234
Maschke M, Erichsen M, Drepper J, Jentzen W, Muller SP, Kolb FP, Diener HC, Timmann D (2002) Limb flexion reflex-related areas in human cerebellum. Neuroreport 13:2325–2330
Mason P (2005) Ventromedial medulla: pain modulation and beyond. J Comp Neurol 493:2–8
Meyer ME, Cottrell GA, Van Hartesveldt C (1993) Intracerebral haloperidol potentiates the dorsal immobility response in the rat. Pharmacol Biochem Behav 44:157–160
Moisset X, Bouhassira D (2007) Brain imaging of neuropathic pain. Neuroimage 37(Suppl 1):S80–S88
Moulton EA, Schmahmann JD, Becerra L, Borsook D (2010) The cerebellum and pain: passive integrator or active participator? Brain Res Rev 65:14–27
Ohyama T, Nores WL, Murphy M, Mauk MD (2003) What the cerebellum computes. Trends Neurosci 26:222–227
Petrovic P, Ingvar M, Stone-Elander S, Petersson KM, Hansson P (1999) A PET activation study of dynamic mechanical allodynia in patients with mononeuropathy. Pain 83:459–470
Peyron R, Garcia-Larrea L, Gregoire MC, Convers P, Lavenne F, Veyre L, Froment JC, Mauguiere F, Michel D, Laurent B (1998) Allodynia after lateral-medullary (Wallenberg) infarct. A PET study. Brain 121(Pt 2):345–356
Peyron R, Laurent B, Garcia-Larrea L (2000) Functional imaging of brain responses to pain. A review and meta-analysis (2000). Neurophysiol Clin 30:263–288
Peyron R, Schneider F, Faillenot I, Convers P, Barral FG, Garcia-Larrea L, Laurent B (2004) An fMRI study of cortical representation of mechanical allodynia in patients with neuropathic pain. Neurology 63:1838–1846
Restuccia D, Della Marca G, Valeriani M, Leggio MG, Molinari M (2007) Cerebellar damage impairs detection of somatosensory input changes. A somatosensory mismatch-negativity study. Brain 130:276–287
Romero A, Rojas S, Cabanero D, Gispert JD, Herance JR, Campillo A, Puig MM (2011) A (1)(8)F-fluorodeoxyglucose MicroPET imaging study to assess changes in brain glucose metabolism in a rat model of surgery-induced latent pain sensitization. Anesthesiology 115:1072–1083
Saab CY, Willis WD (2001) Nociceptive visceral stimulation modulates the activity of cerebellar Purkinje cells. Exp Brain Res 140:122–126
Schmidt BL, Tambeli CH, Barletta J, Luo L, Green P, Levine JD, Gear RW (2002) Altered nucleus accumbens circuitry mediates pain-induced antinociception in morphine-tolerant rats. J Neurosci 22:6773–6780
Schmidt BL, Tambeli CH, Gear RW, Levine JD (2001) Nicotine withdrawal hyperalgesia and opioid-mediated analgesia depend on nicotine receptors in nucleus accumbens. Neuroscience 106:129–136
Schmidt BL, Tambeli CH, Levine JD, Gear RW (2002) mu/delta cooperativity and opposing kappa-opioid effects in nucleus accumbens-mediated antinociception in the rat. Eur J Neurosci 15:861–868
Schweinhardt P, Fransson P, Olson L, Spenger C, Andersson JL (2003) A template for spatial normalisation of MR images of the rat brain. J Neurosci Methods 129:105–113
Schweinhardt P, Glynn C, Brooks J, McQuay H, Jack T, Chessell I, Bountra C, Tracey I (2006) An fMRI study of cerebral processing of brush-evoked allodynia in neuropathic pain patients. Neuroimage 32:256–265
Seminowicz DA, Laferriere AL, Millecamps M, Yu JS, Coderre TJ, Bushnell MC (2009) MRI structural brain changes associated with sensory and emotional function in a rat model of long-term neuropathic pain. Neuroimage 47:1007–1014
Stoodley CJ, Schmahmann JD (2010) Evidence for topographic organization in the cerebellum of motor control versus cognitive and affective processing. Cortex 46:831–844
Tambeli CH, Fischer L, Monaliza SL, Menescal-de-Oliveira L, Parada CA (2012) The functional role of ascending nociceptive control in defensive behavior. Brain Res 1464:24–29
Tesche CD, Karhu JJ (2000) Anticipatory cerebellar responses during somatosensory omission in man. Hum Brain Mapp 9:119–142
Tracey I (2005) Nociceptive processing in the human brain. Curr Opin Neurobiol 15:478–487
Witting N, Kupers RC, Svensson P, Jensen TS (2006) A PET activation study of brush-evoked allodynia in patients with nerve injury pain. Pain 120:145–154
Woolf CJ, Mannion RJ (1999) Neuropathic pain: aetiology, symptoms, mechanisms, and management. Lancet 353:1959–1964
Zimmermann M (1983) Ethical guidelines for investigations of experimental pain in conscious animals. Pain 16:109–110
Acknowledgments
This study was financially supported by a grant from the Industrial Source Technology Development Program (no.10033812) of the Ministry of Knowledge Economy (MKE).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Jinhyung Kim and Jaewoo Shin contributed equally to this work.
Rights and permissions
About this article
Cite this article
Kim, J., Shin, J., Oh, JH. et al. Longitudinal FDG microPET imaging of neuropathic pain: does cerebellar activity correlate with neuropathic pain development in a rat model?. Acta Neurochir 157, 1051–1057 (2015). https://doi.org/10.1007/s00701-015-2415-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-015-2415-7