Abstract
Objectives
The aim of our study was to evaluate minimally invasive techniques for the treatment of anterior circulation aneurysms versus standard surgery, and to calculate the impact of these techniques on health resources, length of stay, and treatment costs.
Methods
A consecutive series of 24 patients with ruptured and 30 with unruptured anterior circulation aneurysms treated with minimally invasive microsurgery (MIM) by the same surgeon was compared with a matched series of standard microsurgeries (SM) conducted for 23 ruptured and 22 unruptured aneurysms. Complication rates, aneurysm obliteration, modified Rankin Scale (mRS) outcomes, length of stay, and treatment costs were assessed.
Results
Surgical complications, aneurysm obliteration rates and mRS outcomes were comparable between MIM and SM groups in ruptured and unruptured aneurysm cohorts. MIM resulted in shorter operative times both in unruptured (102.7 ± 4.35 vs 194.7 ± 10.26 min, p < 0.0001) and ruptured aneurysms (124.3 ± 827 vs 209 ± 13.84 min, p < 0.0001). Length of stay was reduced in patients with MIM for unruptured aneurysms (1.55 ± 24 vs 4.28 ± 0.71 days, p < 0.000,1) but not in those with ruptured aneurysms. MIM reduced treatment costs of unruptured aneurysm patients, mainly through reduced utilization of inpatient resources (non-acute bed costs in CAD: 371.2 ± 80.99 vs 1440 ± 224.1, p < 0.0001), whereas costs were comparable in patients with ruptured aneurysms.
Conclusion
Minimally invasive surgery is a safe and effective approach for the treatment of ruptured and unruptured aneurysms of the anterior circulation. In patients with unruptured aneurysms, reduced invasiveness and shorter operative times decreased length of stay, which reflects improved patient postoperative recovery. Overall, this translated into bed resource economy and cost reduction.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The evolution of intracranial aneurysm surgery includes the development of minimally invasive techniques, which are being increasingly reported [2, 4, 6, 9, 11, 13–21]. Minimally invasive microsurgery (MIM) for aneurysms involves aneurysm clipping through a keyhole craniotomy, a smaller opening of the dura and brain exposure and only focal opening of the basal arachnoid cisterns. However, despite the attractiveness of reduced surgical invasiveness, these techniques have not yet been widely accepted as a routine practice. This is mainly due to concerns about safety or lack of objective benefit as compared to standard surgery. In fact, there are few comparative data on the safety of minimally invasive microsurgery and on clinical as well as radiological outcomes of patients undergoing these procedures [16]. Moreover, there is no information about the impact on health and hospital resources such as bed utilization, length of stay, and treatment costs. In order to change practice, minimally invasive microsurgery for aneurysms must be safe, efficient, and cost effective compared to standard surgery by objective measures. Moreover, as minimally invasive techniques aim at reducing surgical trauma, improving postoperative recovery, and consequently, shortening length of stay, these facets should be evaluated as well in order to establish minimally invasive surgery as part of the routine surgical armamentarium.
To begin addressing these questions, we conducted a single surgeon analysis of a prospectively maintained surgical case database to compare the safety, clinical outcomes, length of stay, and costs of minimally invasive and standard surgery for ruptured and unruptured aneurysms of the anterior circulation.
Patients and methods
Patients characteristics and inclusion criteria
We followed the ethical guidelines of the University Health Network and the University of Toronto. All patients in this series were consecutive cases with ruptured and unruptured anterior circulation aneurysms (including posterior communicating artery aneurysms) where surgical clipping was deemed more appropriate than endovascular therapy after a multidisciplinary consensus. Recurrent, previously coiled aneurysms needing surgical intervention were among those included in the study. We excluded patients with posterior circulation aneurysms other than posterior communicating artery, patients with aneurysms requiring EC-IC bypass, patients with giant aneurysms (>24 mm), and patients with distal circulation aneurysms, as well as patients with large intracerebral hemorrhages with mass effect requiring larger osteotomies for clot evacuation. Patient populations were matched for age, aneurysm size and location, WNFS and Fisher grades (Tables 1 and 2). The senior surgeon (M.T.) switched to using minimally invasive methods in April 2007. The patient population in this study thus reflects the first 54 patients operated on by this technique, matched with consecutive matched patients operated on by the same surgeon prior to April 2007.
Surgical technique (Fig. 1)
Illustrations of the minimally invasive supraorbital craniotomy and minipterional approaches. a 3D reconstruction of a postoperative CT after a supraorbital craniotomy showing the location and size of the bone flap. c Exposure of the frontal lobe after supraorbital craniotomy and opening of the dura. e Subfrontal microsurgical exposure of an anterior communicating artery aneurysm through a supraorbital approach. b 3D reconstruction of a postoperative CT after a right minipterional craniotomy. d Exposure of the lateral aspect of the right frontal lobe and superficial sylvian fissure after a minipterional craniotomy and opening of the dura. f Transsylvian microsurgical exposure of a MCA bifurcation aneurysm through a minipterional craniotomy
Standard aneurysm microsurgery consisted of a curved, fronto-temporal incision behind the hairline, interfascial dissection and deinsertion of the temporal muscle, standard fronto-temporal (pterional) craniotomy (8–12 × 6–8 cm), drilling of the lesser wing of the sphenoid bone until the upper limit of the superior orbital fissure, wide splitting of the sylvian fissure and basal arachnoid cisterns, proximal artery control and further standard microsurgical clipping of the aneurysm. For selected aneurysms of the anterior communicating artery, an orbito-zygomatic osteotomy was added to the standard pterional craniotomy. Minimally invasive microsurgery consisted of a curved, fronto-temporal incision behind the hairline or an eyebrow incision in bald patients or patients with a receding hairline. A small keyhole craniotomy (3–4 cm × 2–3 cm) was placed depending on the aneurysm location and configuration. For anterior communicating artery (AComA) aneurysms, ophtalmic artery (OphtA) aneurysms. and most posterior communicating artery (PComA) aneurysms, the craniotomy was done in the lateral supraorbital region with no deinsertion of the temporalis muscle (Fig. 1a, c, e). For aneurysms of the carotid bifurcation (ICAbif), PComA and AChorA aneurysms with a posterior retrocarotid projection and aneurysms of the middle cerebral artery (MCA), a keyhole opening was placed more laterally, either to expose the sylvian fissure and/or to allow a more lateral trajectory to the internal carotid artery (ICA) (Fig. 1b, d, f). Arachnoid cisterns (basal and sylvian fissure) were opened only focally to release sufficient CSF and expose the aneurysm. Retractors were placed as needed to expose the aneurysm after CSF was released and the brain relaxed. If needed, a ventricular catheter was placed in the frontal horn to maximize CSF drainage. Proximal control was achieved and the aneurysm was clipped using a standard microsurgical technique, but with special, single-shafted clip appliers (Aesculap) allowing a better view during co-axial work in the smaller working space.
Length of stay and outpatient surgeries
Length of stay data were retrieved from administrative hospital databases and patients charts. The typical unruptured aneurysm patient itinerary was a same day admission before transfer to the operating room. After the surgery, patients were admitted to the post-anesthesia critical unit (PACU) before their transfer to a neuro step-down unit (neuro-critical care unit: NCCU) where they spent one night. If they were not discharged the day after surgery, patients were transferred to the ward until their discharge. Aneurysm obliteration and vessel patency was checked either with a conventional DSA or with a postoperative CT angiogram during the patient stay.
Aneursym surgery outpatients were admitted to a dedicated day surgery unit (DSU) after surgery and a 2–4 h stay in the PACU. They underwent a CT angiogram 4–6 h postoperatively to check for aneurysm obliteration, vessel patency, and absence of hematoma or significant brain edema. They were typically discharged 8 h after surgery once they met the DSU discharge criteria.
Patients with ruptured aneurysms were admitted to the intensive care unit (ICU) or the NCCU according to their condition until surgery. After surgery, patients that did not require ICU care were typically observed for vasospasm and delayed ischemia in the NCCU for 12–14 days before being transferred to the ward or discharged home.
Data analysis
Clinical data were abstracted from a prospectively maintained aneurysm database, and from patients charts including clinical notes, operative reports, discharge summaries and follow-up reports. Modified Rankin Scale (mRS) outcomes were collected prospectively and entered in the aneurysm database during follow-up visits by a multidisciplinary team of neurosurgeons and interventional neuroradiologists, and not solely by the operating surgeon. mRS scores were verified for consistency by reviewing follow-up reports. Radiological data was collected by retrospectively reviewing all patients’ radiological imaging and radiological reports.
Treatment costs
All costs are in Canadian dollars (CAD) and were obtained from the hospital case-costing department. Costs included all expenses occurring during each inpatient or outpatient stay for surgical treatment within the Division of Neurosurgery. The cost breakdown consisted of operative room (including personnel and material), acute bed (PACU, NCCU, and ICU or for outpatient, DSU) and ward bed costs, medical imaging (diagnostic digital subtraction angiography, CT and MRI scans) costs, pharmacy and food, core labs, and finally, costs of allied health (physiotherapy and occupational therapy) utilization. Physician fees, treatment costs of supplementary hospitalization in other institutions or inpatient rehabilitation, or the costs of potential further procedures were not included. As outpatients followed a different clinical itinerary in an organized institutional setting, we calculated their costs separately, as we were interested in gauging the further impact on costs of switching from inpatient to outpatient minimally invasive aneurysm surgery.
Statistical analysis
Statistical analysis was done using the Prism software (Graphpad). Differences between groups, except patient’s mean age, and clinical outcomes were calculated using chi-squared contingency table analysis. The mean age of patients per group was calculated using a Student’s t-test. Aneurysm locations were compared with a Fisher's exact test and aneurysm size distribution was compared with a Mann-Whitney rank-sum test. Length of stay was compared with a Student’s t-test. Costs between two groups were compared using a two-tailed Student’s t-test and costs between three groups were compared using one-way ANOVA analysis with a Bonferroni multiple comparison test. Costs are represented in scatter dot plot graphs with means and standard errors of the mean.
Results
Pre-treatment comparison of standard surgery and minimally invasive surgery groups
Standard microsurgery and minimally invasive microsurgery groups were comparable for both ruptured and unruptured aneurysms cohorts. There was no significant difference in age, aneurysm size distribution, and location (Tables 1 and 2). There were more recurrent, previously coiled aneurysms in the elective group treated with minimally invasive surgery, although this did not reach significance. In the ruptured aneurysm group, Fisher and WFNS grade were comparable between the standard and minimally invasive groups (Table 1).
Surgical safety and efficacy (Table 3)
Unruptured aneurysms
There were no perioperative mortalities in either of the two groups. Overall perioperative complications were low in both groups. In the standard microsurgery group there was one clinically eloquent perforator stroke in the basal ganglia (4.5 %) in a patient with a middle cerebral artery bifurcation aneurysm, one transient third nerve palsy (4.5 %), and one wound infection (4.5 %) requiring intravenous (IV) antibiotics. In the minimally invasive microsurgery group, one patient had a permanent anosmia (3.3 %), one had a single postoperative seizure (3.3 %), one had an infection requiring IV antibiotics (3.3 %), and one had a CSF leak that needed surgical repair (3.3 %). No patient had a severe permanent complication such as a clinically eloquent stroke. Overall, the total complication rate was similar in both groups (13.5 % vs. 13.2 %). No intraoperative rupture was encountered in any patients treated for unruptured aneurysms. In one patient operated on with a standard approach for a paraophthalmic aneurysm, the aneurysm was considered not clippable after intraoperative exploration and was wrapped. All aneurysms operated with minimally invasive microsurgery were completely obliterated.
On available postoperative CTs obtained from 0 to 3 days postoperatively, silent ischemia (defined as a sharply demarcated hypodensity in an arterial territory but without detectable postoperative deficits) was detected in two out of 13 standard surgeries (15.4 %) and four out of 28 (14.2 %) minimally invasive surgeries (Fig. 2a, b, c, f and Table 3). Diffuse frontal or temporal hypodensity on postoperative CT scans, which were interpreted either as retraction induced or as venous compromise during dissection, was seen in three out of 13 cases of standard surgery (23.1 %) and one out of 28 cases of minimally invasive surgery (3.6 %) (Fig. 2d, e, c, f and Table 3). This was significant (χ2 = 3.837 with 1 df, p = 0.05).
Postoperative CT scans illustrating postoperative hypodensities. a and b silent ischemia (asterisk) after clipping of a MCA bifurcation aneurysm through a minipterional craniotomy (a) and after clipping of an AComA aneurysm through a standard pterional craniotomy (b). d and e diffuse “retraction” changes (asterisk) after clipping of a MCA bifurcation aneurysm through a minipterional craniotomy (d) and after clipping of an AComA aneurysm through a standard pterional craniotomy (e). c and f postoperative CT scans without obvious hypodensities after a minipterional (c) and a standard pterional craniotomy d
Ruptured aneurysms
The postoperative mortality rate was 0 % in both groups. There were no permanent treatment-induced complications in the standard surgery group. One patient (4.3 %) had transient third nerve palsy and one patient had a wound infection that required IV antibiotics (4.3 %). In the minimally invasive surgery group, one patient (4 %) with an MCA aneurysm who presented with a sylvian-fissure hematoma and pre-operative hemiparesis matured to a clinically eloquent stroke, resulting in hemiplegia. One patient with an AComA aneurysm (4 %) had a monocular vision loss, possibly due to compromise of the vasculature of the optic nerve or thermal injury with bipolar coagulation. One patient (4 %) had a permanent anosmia. One patient (4 %) had a temporary CSF leak that resolved with lumbar drainage and one patient (4 %) had a small, asymptomatic subdural collection that resolved spontaneously. Finally, one patient (4 %) treated for an AChoA showed loss of SSEPs at the end of the wound closure and woke up hemiplegic; in this case, the craniotomy was immediately reopened and the clip repositioned, with a complete recovery of the deficit. Overall, there were no statistical differences in total complication rates between the two groups (χ2 = 0.8653 with 1 df, p = 0.3523).
Small neck remnants were intentionally left to preserve parent artery or branches in four (17.4 %) patients undergoing standard surgery and two (8.7 %) patients operated on with minimally invasive approaches.
On available postoperative CT scans, silent ischemia was found in two (8.7 %) patients with standard and four (17.4 %) patients with minimally invasive approaches, whereas diffuse hypodensity due to retraction injury or venous compromise was found in 14 (60.1 %) patients with standard and nine (39.1 %) patients with minimally invasive surgeries (Table 3). These differences were not significant (χ2 = 2.174 with 1 df, p = 0.1404).
Clinical postoperative outcomes (Table 4)
Unruptured aneurysms
At the first follow-up visit (6–12 weeks) and 6 months postoperatively, all patients achieved a good outcome (0–2) on a modified Rankin scale (mRS) (Table 3). One patient in the standard surgery group who had a perioperative stroke was lost to follow-up before the first follow-up visit. At discharge, this patient had slowly improving expressive dysphasia and hemiparesis. Of the 21 remaining patients followed in the standard group, 18 (86 %) had an mRS of 0 at the first follow-up visit and three (14 %) had an mRS of 1. At 6 months, 19 (90.4 %) patients had an mRS of 0 and two (9.6 %) remained with an mRS of 1. The latter two patients’ disability was present preoperatively, and consisted of progressive visual deficits due to optic nerve compression by paraophthalmic aneurysms that persisted postoperatively; despite these symptoms, the patients were able to resume their normal activity. One patient had a transient, third nerve palsy that resolved by the 6-month follow-up visit. In the minimally invasive group, 26 (92.8 %) out of 28 patients had an mRS of 0 at first follow-up, one (3.6 %) had an mRS of 1 and one (3.6 %) had an mRS of 2. The latter patients’ disability was present preoperatively, and consisted of moderate memory problems from a previous subarachnoid hemorrhage, which remained at an mRS of 2 postoperatively. One patient who complained of transient memory problems at the first follow-up returned to full-time work by the 6-month visit. Overall, there was no statistical difference in mRS at first follow-up (χ2 = 0.1032 with 1 df, p = 0.748) or at 6 months (χ2 = 0.05875 with 1 df, p = 0.8085) between the standard and minimally invasive groups.
Ruptured aneurysms
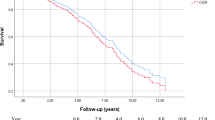
At first follow-up (6–12 weeks after discharge), 19 (82.6 %) patients treated with standard surgery were independent (mRS 0-2) and four (17.4 %) were dependent with an mRS of 3. At 6 months, 20 (86.9 %) patients were independent (mRS 0-2), two patients (8.6 %) were dependent (mRS 3), and one patient (4.3 %) was lost to follow-up. Among patients operated on with a minimally invasive approach, 20 patients (83.3 %) were independent (mRS 0-2) at 6–12 weeks, three (12.5 %) patients were dependent (mRS 3-5), and one patient (4.2 %) was lost to follow-up. At 6 months, 22 (91.7 %) patients were independent (mRS 0-2), one patient (4.2 %) was dependent (mRS 5), and one patient remained lost to follow up. There were no mortalities in either group. Of all the patients with poor outcomes (mRS 3-5), one patient treated with a minimally invasive approach had a bad outcome due to the surgery, and all the others had complications due to their initial condition, multiple medical complications, and/or delayed cerebral ischemia due to vasospasm. Overall, there was no difference in outcome at 6–12 weeks (χ2 = 0.3141 with 1 df, p = 0.5752) or at 6 months (χ2 = 0.02449 with 1 df, p = 0.8757) between the standard or minimally invasive surgery groups.
Length of surgery (Table 5)
In patients treated for unruptured aneurysms, the mean operative time (skin-to-skin) was 194.7 ± 10.3 min with standard surgery and 102.7 ± 4.3 min with minimally invasive surgery, the latter of which was very significantly shorter (p < 0.0001). Minimally invasive surgery similarly reduced operative times in patients with ruptured aneurysms (209 ± 13.84 min for standard surgery vs. 124 ± 8.275 min for minimally invasive surgery, p < 0.0001). All surgeries included in this series of standard and minimally invasive approaches were entirely performed by the senior author (MT).
Length of stay (Table 5)
The patients undergoing minimally invasive surgery for unruptured aneurysms stayed a mean of 1.552 ± 0.246 days. This included seven outpatients who, by definition, had a length of stay of 0 days, as they did not spend the night in the hospital. When outpatients are excluded from the analysis, LOS was 2.045 ± 0.2415 days. Patients treated with standard surgery stayed significantly longer, with an LOS of 4.285 ± 0.7109 days (p < 0.0001 for comparison with the minimally invasive group with or without outpatients).
In patients with subarachnoid hemorrhage, length of stay was determined by an obligatory observation period for delayed cerebral ischemia due to vasospasm of at least 12–14 days even in good grade patients or by the complicated medical and neurological conditions due to subarachnoid hemorrhage in poor grade patients. The length of stay was not different in minimally invasive or standard surgery groups (19 ± 2.067 days for standard surgery and 18.19 ± 2.048 days for patients with minimally invasive surgery, p = 0.3914).
Costs
Total costs per unruptured aneurysm patient were significantly different between standard surgery, inpatient, and outpatient minimally invasive surgery using a one-way ANOVA analysis (p = 0.0014) (Fig. 3a). To measure the sole impact of surgical technique on total costs, we have also compared standard surgery and minimally invasive surgery inpatients only with a two-tailed t-test, excluding outpatients. The decreased costs in minimally invasive patients was statistically significant (p = 0.0419). A breakdown of costs showed that there was no significant difference in OR or acute bed costs between the three groups (Fig. 3b and c). However, the cost of ward beds was significantly lower in minimally invasive surgery inpatients, as expected from their shorter length of stay, and was understandably null for outpatients who did not utilize ward beds (Fig. 3d). In addition, the costs of medical imaging were very significantly lower in the minimally invasive inpatient group compared to standard surgery and further decreased in the outpatient group (Fig. 4a). This is due to the routine use of postoperative DSA in the time frame where patients were undergoing standard surgery and a progressive transition to postoperative CT angiogram; only more recently in the time frame were most of the minimally invasive surgeries done. Therefore, a progressive reduction in medical imaging costs, which is not a direct consequence of the surgical approach, has, in addition to bed expense reduction, also contributed to a decrease in total costs.
Breakdown of treatment costs in unruptured aneurysms. a Total costs, b Operating room costs, c Acute bed costs and d Ward bed costs. Comparisons are made between standard surgeries, minimally invasive surgeries on inpatients (Mini) and minimally invasive surgeries in outpatients (Mini-Op). Groups were compared with a one-way ANOVA analysis and a post-test Bonferroni multiple comparison between groups. p values are shown. **: p values <0.01, *** : p values <0.001
Further breakdown of treatment costs in unruptured aneurysms. a Imaging costs, b Core labs costs, c Pharmacy and Nutrition costs and d Allied health (physiotherapy, speech therapy, occupational therapy) costs. Comparisons are made between standard surgeries, minimally invasive surgeries on inpatients (Mini) and minimally invasive surgeries in outpatients (Mini-Op). Groups were compared with a one-way ANOVA analysis and a post-test Bonferroni multiple comparison between groups. p values are shown. **: p values <0.01, *** : p values < 0.001. NS: non-significant p values >0.05
As imaging costs introduce a bias in the total cost analysis, we recalculated total costs after excluding imaging costs. Total costs without imaging were still significantly different between standard surgery patients, minimally invasive surgery inpatients, and minimally invasive surgery outpatients using a one-way ANOVA analysis (p < 0.034), but when comparing only standard and minimally invasive surgery inpatients, there was no significant difference in total costs (two-tailed t-test, p = 0.079). Further cost evaluation included comparable costs of laboratory tests (Fig. 4b), a significant decrease in costs for pharmacy and nutrition (though for relatively inconsequential amounts; Fig. 4c) and no differences in allied health costs, which includes physiotherapy, speech and language therapy, as well as occupational therapy (Fig. 4d).
Total treatment costs were not different between standard and minimally invasive groups in ruptured aneurysms (Fig. 5).
Discussion
Over the last 15 years, many surgeons have reported their experience with minimally invasive keyhole craniotomies for the treatment of anterior skull base lesions and aneurysms. The potential advantages often cited by supporters of minimally invasive techniques are that smaller openings not only reduce postoperative morbidity due to soft tissue, muscle, and bone trauma, but in fact also decrease the manipulation of the brain itself as only targeted and necessary intracranial structures are exposed and dissected. Moreover, under optimal relaxation with CSF release, brain retraction is actually described by several authors to be minimal, while others have combined keyhole craniotomies with skull base surgery techniques by adding the removal of the orbital ridge to obtain a more basal trajectory and therefore less retraction [17, 20, 22].
How these widely debated technical concepts translate into patient’s safety, outcomes, and treatment efficacy is less clear. Reisch and Perneczky reported a pioneering series of 450 supraorbital craniotomies performed through eyebrow incisions for various intracranial lesions, including 229 aneurysms with low complications [18], and later updated to comprise 793 aneurysms. They found an mRS of 1–2 in 96 % of cases in unruptured aneurysms, and compared to 150 pterional craniotomies, there was a tendency toward better outcomes in the minicraniotomy group [7]. Neurological outcomes or aneurysm obliteration rates were not provided in several other studies that focused more on technical issues of keyhole approaches [5, 17, 21]. Glasgow outcome scale (GOS)-based outcomes were provided by Brydon et al., who analyzed their experience with 50 cases of supraorbital minicraniotomies for ruptured aneurysms of the anterior circulation. They describe overall new and immediate postoperative deficits in 12 % of their patients and new deficits at discharge of 24 %, whereas their reported 18 % mortality and poor outcomes (GOS 1-3) and 82 % of favorable outcome (GOS 4 and 5) are confounded by morbidity due to subarachnoid hemorrhage [2]. Mitchell et al. reported 47 cases of supraorbital minicraniotomies in 40 elective and seven subarachnoid hemorrhage patients with seven early complications, overall good outcomes (45 patients had GOS of 5) and clipping of the aneurysms judged successful in all cases [11]. Lan et al. have operated on 100 patients, mainly with ruptured aneurysms with minimally invasive keyhole approaches with 92 % good GOS outcomes [9]. Paladino et al. compared a large series of 482 patients with ruptured and unruptured aneurysms of the anterior circulation operated on with minimally invasive approaches, with a series of 146 patients operated on through a standard approach by another surgical team [16]. Glasgow outcome scores were comparably favorable in standard and keyhole surgeries, but no detailed data is shown on complications and radiological results. These series provide encouraging data on the safety of minimally invasive aneurysm surgery, but fail to provide comprehensive and complete information to adequately compare minimally invasive and standard surgery.
Our series is a comparative study that captured the transition from standard to minimally invasive surgery at a single institution and in a single-surgeon practice, and provides detailed clinical and radiological outcomes. Although comparing consecutive and not contemporaneous treatment groups (Pre-and post-April 2007), we believe our study provides value by describing a real change in surgical practice and the corresponding learning curve in a homogenous and prospectively followed patient population. First, we have found that minimally invasive surgery was comparably safe to standard approaches and overall the complication rate was low. Our experience also shows that minimally invasive surgery is effective in obliterating anterior circulation aneurysms (overall obliteration rate 52/54, 96.3 %) without increasing perioperative aneurysm rupture rates.
We have reviewed all available postoperative scans and recorded the presence of postoperative changes either in the form of hemorrhagic complications or hypodensities due to silent ischemia or due to the surgical approach. We have not found hemorrhagic contusions of brain parenchyma in either of the two approaches and silent arterial ischemia was comparable in both series. Diffuse hypodensities, which are often labeled as “retraction” injuries, were lower in the minimally invasive group, and statistically significantly less in unruptured aneurysms. This suggests that, contrary to what is often assumed, the risk of parenchymal brain injury with small craniotomies is not increased and in fact might be lower than in standard approaches. This can be explained by the fact that limited exposure reduces manipulation of the brain and that limited cisternal dissection prevents the sacrifices of draining veins that are often divided during a standard dissection of the sylvian fissure, resulting in hypodensities on postoperative scans. Second, this also shows that with adequate brain relaxation using osmotic agents, ventilation control, and CSF release, the retraction needed to expose the working area is not detrimental to the brain.
We have prospectively collected modified Rankin scale outcomes at the occasion of the first two follow-up visits at 6–12 weeks and at 6 months, showing that these were equally good in standard and minimally invasive surgeries both in unruptured and ruptured aneuryms. Together, low complication rates, efficient aneurysm obliteration, minimal postoperative radiological changes and excellent mRS outcomes objectively support minimally invasive surgery as a safe and efficient procedure.
More difficult to quantify, postsurgical morbidity and functional limitations such as pain, time to independent mobilization, and return to full autonomy were not directly measured in this study. However, length of stay is a valid surrogate measure of postsurgical recovery, as patients are always cleared by the surgical team as well as by the physiotherapy and occupational therapy team for independent mobilization, adequate pain management, and safety at home before authorizing discharge. The length of stay under the same discharge criteria—that are independent of the operating surgeon—throughout the two series dropped very significantly in the elective minimally invasive surgery group, showing that patients undergoing minimally invasive procedures have a shorter recovery from surgery and anesthesia. Although we cannot formally exclude a bias in discharge policy between the standard and minimally invasive inpatient groups, we believe that shorter length of stay may be imputable to reduced surgical trauma and might also be influenced by significantly shorter length of surgeries and therefore anesthesia.
Shorter length of stay and improved postoperative recovery were what clearly prompted us to consider treating patients with unruptured aneurysms as outpatients. Our department has a long-lasting and large experience with outpatient surgery for intracranial lesions, mainly brain tumors [1], and has therefore a well-established outpatient infrastructure and protocol [3]. Moreover, qualitative studies have shown that patient satisfaction was high in patient;s undergoing outpatient brain tumor surgery [8]. In our limited initial experience, we did not experience complications or readmissions in any of the seven outpatients. From this small initial series, we conclude that outpatient aneurysm surgery warrants further exploration in well-selected patients and is rendered possible only by minimally invasive surgery in an organized setting and with proper patient information. However, further follow-up and larger case series are required prior to drawing conclusions about this practice.
Finally, in an era of increased scrutiny of health costs by health authorities and hospitals, we have analyzed the impact of switching to minimally invasive aneurysm surgery on treatment costs. The incremental decrease in costs between standard surgery, minimally invasive inpatient surgery, and outpatient surgery shows that minimally invasive surgery decreases costs mainly by shortening the length of stay and therefore bed resource utilization. Further cost reduction during this period is also due to a progressive decline in postoperative digital subtraction angiography and increased use of CT angiograms, which is not related to the surgical technique per se. This introduces a bias in the total cost comparison, and cost reduction selectively induced by minimally invasive approaches is clearly only due to shorter ward bed utilization. The impact of minimally invasive surgery on total costs is therefore moderate. Furthermore, in a ruptured aneurysm population the length of stay and thus the costs are dictated by the severity of the subarachnoid hemorrhage and consequent complications, therefore, understandably the surgical technique has no impact in this context.
Overall, our initial experience shows that for most anterior circulation aneurysms, minimally invasive surgery is a valid alternative to standard approaches in both ruptured and unruptured aneurysms. In unruptured aneurysms, it may have objective and measurable advantages that consist mainly of shorter postoperative recovery times translating into shorter length of stay and some impact on overall costs. Minimally invasive aneurysm surgery may represent a significant progress of open aneurysm microsurgery that remains an essential modality in the standard of care of cerebral aneurysms, even in the post-ISUA (International Study of Unruptured Intracranial Aneurysms), post-ISAT (International Subarachnoid Aneurysm Trial) [12, 23]. Although our series consisted of patients deemed unsuitable for endovascular therapy, the improvement of aneurysm microsurgery through reduced invasiveness may serve to help match the perceived lower invasiveness of endovascular therapy. Furthermore, microsurgery, associated with longer durability and lower rebleeding rates [10, 12, 23], may be advantageous in younger patients that are eligible for both treatments. In this context, further refinement and efforts to reduce invasiveness of microsurgery remain a justifiable and important goal.
Conclusion
Minimally invasive microsurgery for cerebral aneurysms is part of an ongoing effort to reduce surgical disruption of tissue and surgical brain trauma, which translates to shorter operative times, and shorter postoperative recovery and length of stay, therefore possibly augmenting patient satisfaction and improving their perception of surgery. Altogether, our experience shows that minimally invasive surgery is an important evolution towards minimization of surgical trauma, and at the same time provides the safety and durability of standard aneurysm surgery.
References
Boulton M, Bernstein M (2008) Outpatient brain tumor surgery: innovation in surgical neurooncology. J Neurosurg 108:649–654
Brydon HL, Akil H, Ushewokunze S, Dhir JS, Taha A, Ahmed A (2008) Supraorbital microcraniotomy for acute aneurysmal subarachnoid haemorrhage: results of first 50 cases. Br J Neurosurg 22:40–45
Carrabba G, Venkatraghavan L, Bernstein M (2008) Day surgery awake craniotomy for removing brain tumours: technical note describing a simple protocol. Minim Invasive Neurosurg 51:208–210
Cheng WY, Lee HT, Sun MH, Shen CC (2006) A pterion keyhole approach for the treatment of anterior circulation aneurysms. Minim Invasive Neurosurg 49:257–262
Czirjak S, Nyary I, Futo J, Szeifert GT (2002) Bilateral supraorbital keyhole approach for multiple aneurysms via superciliary skin incisions. Surg Neurol 57:314–323, discussion 323–314
Dare AO, Landi MK, Lopes DK, Grand W (2001) Eyebrow incision for combined orbital osteotomy and supraorbital minicraniotomy: application to aneurysms of the anterior circulation. Technical note. J Neurosurg 95:714–718
Fischer G, Stadie A, Reisch R, Hopf NJ, Fries G, Bocher-Schwarz H, van Lindert E, Ungersbock K, Knosp E, Oertel J, Perneczky A (2011) The keyhole concept in aneurysm surgery: results of the past 20 years. Neurosurgery 68:45–51, discussion 51
Khu KJ, Doglietto F, Radovanovic I, Taleb F, Mendelsohn D, Zadeh G, Bernstein M (2010) Patients’ perceptions of awake and outpatient craniotomy for brain tumor: a qualitative study. J Neurosurg 112:1056–1060
Lan Q, Gong Z, Kang D, Zhang H, Qian Z, Chen J, Huang Q (2006) Microsurgical experience with keyhole operations on intracranial aneurysms. Surg Neurol 66(Suppl 1):S2–S9
Mitchell P, Kerr R, Mendelow AD, Molyneux A (2008) Could late rebleeding overturn the superiority of cranial aneurysm coil embolization over clip ligation seen in the International Subarachnoid Aneurysm Trial? J Neurosurg 108:437–442
Mitchell P, Vindlacheruvu RR, Mahmood K, Ashpole RD, Grivas A, Mendelow AD (2005) Supraorbital eyebrow minicraniotomy for anterior circulation aneurysms. Surg Neurol 63:47–51, discussion 51
Molyneux AJ, Kerr RS, Yu LM, Clarke M, Sneade M, Yarnold JA, Sandercock P (2005) International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet 366:809–817
Mori K, Osada H, Yamamoto T, Nakao Y, Maeda M (2007) Pterional keyhole approach to middle cerebral artery aneurysms through an outer canthal skin incision. Minim Invasive Neurosurg 50:195–201
Mori K, Yamamoto T, Nakao Y, Oyama K, Esaki T, Watanabe M, Nonaka S, Hara T, Honma K (2008) Lateral supraorbital keyhole approach to clip unruptured anterior communicating artery aneurysms. Minim Invasive Neurosurg 51:292–297
Niemela M, Koivisto T, Kivipelto L, Ishii K, Rinne J, Ronkainen A, Kivisaari R, Shen H, Karatas A, Lehecka M, Frosen J, Piippo A, Jaaskelainen J, Hernesniemi J (2005) Microsurgical clipping of cerebral aneurysms after the ISAT Study. Acta Neurochir Suppl 94:3–6
Paladino J, Mrak G, Miklic P, Jednacak H, Mihaljevic D (2005) The keyhole concept in aneurysm surgery—a comparative study: keyhole versus standard craniotomy. Minim Invasive Neurosurg 48:251–258
Ramos-Zuniga R, Velazquez H, Barajas MA, Lopez R, Sanchez E, Trejo S (2002) Trans-supraorbital approach to supratentorial aneurysms. Neurosurgery 51:125–130, discussion 130–121
Reisch R, Perneczky A (2005) Ten-year experience with the supraorbital subfrontal approach through an eyebrow skin incision. Neurosurgery 57:242–255, discussion 242–255
Reisch R, Perneczky A, Filippi R (2003) Surgical technique of the supraorbital key-hole craniotomy. Surg Neurol 59:223–227
Steiger HJ, Schmid-Elsaesser R, Stummer W, Uhl E (2001) Transorbital keyhole approach to anterior communicating artery aneurysms. Neurosurgery 48:347–351, discussion 351–342
van Lindert E, Perneczky A, Fries G, Pierangeli E (1998) The supraorbital keyhole approach to supratentorial aneurysms: concept and technique. Surg Neurol 49:481–489, discussion 489–490
Warren WL, Grant GA (2009) Transciliary orbitofrontozygomatic approach to lesions of the anterior cranial fossa. Neurosurgery 64:324–329, discussion 329–330
Wiebers DO, Whisnant JP, Huston J 3rd, Meissner I, Brown RD Jr, Piepgras DG, Forbes GS, Thielen K, Nichols D, O’Fallon WM, Peacock J, Jaeger L, Kassell NF, Kongable-Beckman GL, Torner JC (2003) Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet 362:103–110
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Radovanovic, I., Abou-Hamden, A., Bacigaluppi, S. et al. A safety, length of stay, and cost analysis of minimally invasive microsurgery for anterior circulation aneurysms. Acta Neurochir 156, 493–503 (2014). https://doi.org/10.1007/s00701-013-1980-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-013-1980-x