Abstract
Background
Clinical decision-making involves a complex interaction between patients and caregivers. The medical knowledge and values of caregivers are essential for treatment recommendations. This study was undertaken to evaluate treatment recommendations by a group of Scandinavian neurosurgeons before and after an expert lecture on glioblastoma surgery.
Method
An interactive voting system was used to record responses to four questions regarding glioblastoma management before and after a 25-min lecture on the benefit of radical glioblastoma surgery.
Results
The majority of the audience aimed at radical surgery combined with radiotherapy before (76 %) and after (88 %) the lecture. The proportion who recommended immediate postoperative follow-up by MRI increased from 34 % to 75 %. Fourteen percent (before) and 45 % (after) recommended renewed surgery to remove small residuals in patients, while 52 % (before) and 60 % (after) would have wanted to be re-operated if they themselves had been patients.
Conclusion
The views on optimum management differed widely in a relatively homogeneous group of neurosurgeons. The lecture had a major impact on decision-making. A large proportion of the attendees recommended different management strategies for themselves and for their patients. The findings indicated the need to analyze the evaluation of medical knowledge, discuss the ethics of decision-making and encourage second opinions for serious neurosurgical decisions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Clinical decision-making involves a complex interaction of caregivers and patients. The caregiver needs to explain the diagnosis and treatment alternatives and is often expected to recommend “the best treatment.” The final decision is made by the patient, but the patient is utterly dependent on how caregivers perceive available medical knowledge and interpret the specific situation of each patient [1].
The caregivers have medical knowledge that comprises part of the prevailing medical paradigm but is individual since each caregiver has a personal set of experiences and a personal way of seeking and interpreting medical information. The individual medical knowledge is probably of essential importance for decision-making, and its inter-individual variation can be expected to lead to a big difference in treatment recommendations from different caregivers [2]. Lectures at conferences are a common means of continuous education. Improved technologies allow interactive sessions. The audience can respond to questions, with immediate recording of detailed responses. We expected that a lecture with medical contents that had some degree of novelty for a Scandinavian neurosurgical audience could influence attitudes toward glioma surgery.
We assessed whether attitudes toward decision-making were influenced by medical information delivered by an expert at a lecture. We specifically studied whether medical information would be valued differently when applied to an anonymous patient or to the caregivers themselves and whether the information given at the lecture could change the audience’s attitudes and thereby therapeutic traditions.
Methods
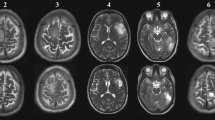
At the 59th annual Scandinavian Neurosurgical Meeting in Stockholm in 2008, an interactive wireless system for voting and responding was used to record replies to a set of questions before and after a lecture on the benefit of radical treatment of glioblastoma multiforme. The same questions (Figs. 1, 2, 3 and 4) were asked before and after the lecture. The 25-min lecture on the prognosis of glioblastoma with radical surgical treatment was given by Prof. Manfred Westphal, an international expert on glioblastoma treatment. The talk delivered recent data that allowed comparison of survival in relation to surgical radicality [3]. The audience comprised Scandinavian neurosurgeons: 50 at the vote before the lecture and 53 at the vote after. Three attendees arrived during the lecture; nobody left.
The results were discussed informally with the attendees after the session.
Results
In each vote, 93–97 % of all attendees participated. The questions and votes are shown in Figs. 1, 2, 3 and 4.
Before the lecture already a majority (76 %) of the audience aimed at radical surgery with radiotherapy. Thirty-four percent of the audience recommended postoperative MRI, while 28 % considered postoperative imaging unnecessary. Fourteen percent of the audience recommended renewed surgery for the patients to remove any small residuals detected on postoperative imaging, while 52 % would have wanted to be re-operated if they had been operated on for GBM and found to have a small residual on postoperative imaging.
Following the lecture, responses changed dramatically. The majority of the audience aiming at radical surgery increased to 88 %. Seventy-five percent of the audience recommended postoperative MRI, while 13 % considered postoperative imaging unnecessary. Forty-five percent of the audience recommended renewed surgery for patients to remove any small residuals detected on postoperative imaging, and 60 % would have wanted to be re-operated if they had been operated on for GBM and found to have a small residual on postoperative imaging.
During the informal discussion, the attendees expressed surprise at how much their attitudes had changed during the lecture. Regarding specific questions, the reasons not to obtain imaging or to obtain imaging with CT rather than MRI were described as “futility,” “medical priorities” and “lack of resources.” The reasons not to suggest the same treatments for patients as for themselves were: “there is no evidence of benefit;” “ we lack resources to go back for every patient;” “the potential benefit is only marginal and does not make a big difference for the patients.”
Discussion
We found that a lecture on the benefit of radical surgery for glioblastoma dramatically increased the number of neurosurgeons who expressed a positive attitude toward radical surgery, resection evaluation by postoperative MRI and aggressive surgical management. In spite of a large difference in attitudes to radiology and renewed operation before and after, consensus was not reached. The strong impact was surprising considering that the data were largely available in published literature and had also been widely discussed at several international meetings. We can only speculate about why the impact was so strong. It is possible that new data, although accessible, fail to affect the neurosurgical community fully unless presented in a specific context, such as a lecture by a renowned expert. The latter may transfer trust and make the audience confident that the data presented are relevant and reliable. The finding indicates that a conference format with invited experts can be a highly effective means of postgraduate education and that the personal interaction with a lecturer may have an additional pedagogic value. Although the majority of the audience expressed a favorable attitude toward radical surgery with radiotherapy for glioblastomas, only a small fraction expressed willingness to carry out aggressive radiological postoperative follow-up and readiness to increase the radicality by immediate reoperation.
The findings cannot be generalized to any combination of experts, topics or audiences. The compilation of a scientific program requires knowledge and evaluation of these factors. The results vary and can be more or less successful. Our findings are only proof of the concept that a lecture can under certain circumstances be a highly effective means of changing attitudes and provide relevant information on factors that affect medical decision-making. We emphasize, however, that a reported change in attitudes does not necessarily lead to a change in behavior. Peer pressure and the influence of irrational factors may have affected how the audience reported their attitudes. In order to corroborate the findings, this study could be repeated with an extended protocol including analysis of scanning practices and surgical indications “before and after.”
The audience was asked to make very serious therapeutic decisions that would have an impact on the expected length of survival. The audience comprised an all-Scandinavian group of neurosurgeons, reflecting similar neurosurgical training and a relatively homogeneous set of values in the Scandinavian countries [4]. The group can be considered to comprise competent decision-makers. Still, the group diverged significantly from any consensus regarding the recommended radiological and surgical measures. The individual therapeutic differences reflect differences in values and differences in evaluation of medical knowledge. Different opinions regarding individual treatment are probable, also regarding other cases. Our finding identifies a need to assess the quality and value contents of recommendations from consensus conferences on individual patient care. It is also obvious that individual patients may benefit from the opportunity to consult more than one specialist before deciding upon treatment.
It was surprising that the audience did not recommend the same treatment for their patients that they would have chosen for themselves. Before the lecture, 14 % recommended a second operation to increase the radicality for their patients, while 52 % stated that they would want to have additional surgery if they were the patient in question. Again, we can only speculate as to why a large fraction of the neurosurgeons recommended different treatment for themselves than for their patients. A decision to go back in for a second surgery can only be justified if reoperation can be expected to give benefit: extended survival without increasing the risk. The condition for the question was that the added surgical risk was neglible. The critical issue is thus whether extended survival could be expected. It is commonly stated that additional measures can only extend survival marginally (reviewed in [3]). Another common argument is that we lack reliable data to judge the survival benefit [5]. Both arguments contain an element of evaluation. A “marginal benefit” may be evaluated differently by the person who will be affected by the benefit and by outsiders who provide or pay for the “marginal benefit.” Again, the evaluation of which data are sufficiently reliable to influence surgical treatment is subjective. Both logical empiricists (reviewed in [6]) and members of the EBM movement [7–10] have tried to provide tools to judge scientific quality. They have attempted to construct systems to evaluate science independently of the scientific content; the attempts have been futile. The evaluation of which data are relevant at a given time requires expertise in the field [1, 11, 12].
The surprising finding was, however, that so many potential caregivers evaluated scientific data or value of extended life differently for their patients than for themselves. “Lack of evidence” was cited as a cause not to perform surgery in patients. These participants viewed the “scientific facts” as individual pieces of information that needed experimental verification, a perspective that is sometimes expressed in evidence-based medicine [13–15]. This view is in strong disagreement with two more common views in philosophy: first, the paradigm concept, which holds that our scientific fields comprise a multitude of overlapping and interlocking observations, beliefs and practices that provide a unified idea of accepted truth. This “truth” is a function of the interdependence of the elements of the paradigm and is not established by experimental verification of each observation. Originally, Thomas Kuhn described how science works and how scientific facts, theories, observations and beliefs form a paradigm [16]. The second view was actually presented earlier, originally by Karl Popper [17]. Science comprises theories, not individual observations or experimental facts. The theories are tested experimentally, and the theory must be changed if thoroughly falsified by experimental observations. In our case, it could be argued that our paradigm and theories suggested radical surgery if at all possible. The fact that nobody has experimentally verified whether renewed surgery under these circumstances is beneficial is not relevant. The lack of experimental “verification” is not sufficient to disregard what we already accept as part of the neurosurgical paradigm, and “lack of evidence” is not an epistemologically acceptable reason [18] to withhold surgery or radiological examinations. It is neither rational nor intellectually honest to use a set of medical “knowledge” for decisions that affect oneself and a different set of “medical evidence” that applies to patients.
Regardless of how knowledge, evidence and values affect treatment recommendations, one would, for ethical reasons, expect doctors to recommend the same treatment for their patients and themselves. The idea of treating oneself and others equally is fundamental in Kantian ethics, agrees with Aristotelian ethics and is found in most religious codes of ethics (reviewed in [19]). Modern versions of contract theory require a “veil of ignorance”: moral choices should be made without the knowledge of whether you yourself or someone else will be affected by the choice. The exception is utilitarian ethics, which require empirical inquiry into the consequences of the actions before choosing the best action. Still, it is difficult to believe that instances of treating others differently than one would, prima facie, lead to better consequences than equality of treatment. Finally, it would be difficult to defend the fairness of utilizing more resources for one’s own benefit than for the patient's. The findings remind us how easy it is to neglect our primary duties to our patients. Our medical interventions affect the lives of patients profoundly.
When interpreting findings, we must remember that our observations reflected a relatively small investigational group, and we cannot know whether the findings of a reported change in attitude translated into practice. Still, we provide a serious reminder that we need to make earnest therapeutic evaluations concerning what benefits our patients; also, what benefits patients should not be different from what benefits ourselves. We should also encourage patients to seek second opinions since our own evaluation of the therapeutic optimum may differ from that of others because of different values and different evaluations of knowledge.
References
Sackett DL, Rosenberg WC, Muir Gray JA, Haynes RB, Richardson WS (1996) Evidence based medicine: what it is and what it isn’t. BMJ 312:70–72
Bate L, Hutchinson A, Underhill J, Maskrey N (2012) How clinical decisions are made. Br J Clin Pharmacol 74:614–620
Kanu OO, Mehta A, Di C, Lin N, Bortoff K, Bigner DD, Yan H, Adamson DC (2009) Glioblastoma multiforme: a review of therapeutic agents. Expert Opin Ther Targets 13:701–718
World Value Survey (1998) In: Inglehart R, Basañez M, Moreno A (eds) Human values and beliefs—source book. University of Michigan Press, Chicago
Metcalfe SE, Grant R (2001) Biopsy versus resection for malignant glioma. Cochrane Database Syst Rev 2001(3), CD002034
Haack S (2003) Defending science—within reason. Prometheus Books, New York
British Medical Association (1995) Report of the working party on medical education. BMA, London
Marshall T (1995) Evidence based medicine. Lancet 346:1171–1172
Editorial, no authors listed (1995) Evidence based medicine; in its place. Lancet 346:785
Sackett DL (1995) Surveys of self-reported reading times of consultants in Oxford, Birmingham, Milton-Keynes, Bristol, Leicester, and Glasgow. In: Rosenberg WMC, Richardson WS, Haynes RB, Sackett DL (eds) Evidence-based medicine. Churchill Livingstone, London
Cohen AM, Hersh WR (2004) Criticisms of evidence—based medicine. Evid Based Cardiovasc Med 8:197–198
Popper K (1962) Conjectures and refutations. Routledge and Keagan Paul, London
Davidoff F, Haynes B, Sackett D, Smith R (1995) Evidence based medicine: a new joumal to help doctors identify the information they need. BMJ 310:1085–1086
Goldenberg MJ (2006) On evidence and evidence-based medicine: lessons from the philosophy of science. Soc Sci Med 62:2621–2632
Weatherall DJ (1994) The inhumanity of medicine. BMJ 309:1671–1672
Kuhn T (1996) The structure of scientific revolutions, 3rd edn. University of Chicago Press, Chicago
Popper K (1959) The logic of scientific discovery. Routledge, London
Worrall J (2007) Evidence in medicine and evidence-based medicine. Philos Compass 2/6:981–1022
Tännsjö T (2002) Understanding ethics. An introduction to moral theory. Edinburgh University Press, Edinburgh
Acknowledgment
We acknowledge the expert lecture given by Prof. Manfred Westphal, which was indispensible for our study.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mathiesen, T. To operate or not—the impact of a lecture on radical glioblastoma surgery and different treatment options on decision-making for oneself and patients. Acta Neurochir 155, 1425–1429 (2013). https://doi.org/10.1007/s00701-013-1796-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-013-1796-8