Abstract
Background
Fenestrations of intracranial arteries are variants resulting from incomplete fusion of vessels during development with unknown clinical significance. They are best visualised with 3D rotational angiography (3DRA).
Objective
In a prospective consecutive series of patients with suspected aneurysms, 3DRA was performed to identify not only the potential bleeding source but also to assess the frequency and location of any fenestrations of intracranial arteries.
Methods
In 287 consecutive patients with possible intracranial aneurysms (accidental discovery or previous history of SAH), 3DRAs were prospectively performed, and the location of subarachnoid haemorrhage was assessed by CT.
Results
Of 174 patients presenting with SAH, 153 had saccular aneurysms, and in 21 cases (12.1 %), no source of bleeding was found. In 20 of these 21 patients with "unexplained SAH" (95.2 %) an arterial fenestration was detected in the neighbourhood of the clot. The incidence of fenestration in the 153 aneurysmal SAH patients was 22.9 %, and it was 23.3 % in 266 patients with intracranial aneurysms (113 accidental and 153 ruptured).
Conclusions
Arterial fenestration was detected in 22.9 % of ruptured cerebral aneurysms, in contrast with 95.2 % in patients with unexplained SAH, the difference being statisctically significant (p < 0.01). Fenestration is a developmental defect, a structural wall weakness possibly making the vessel prone to rupture. Its incidence of nearly 100 % may suggest a connection with idiopathic SAH. The presented data indicate that arterial fenestrations are generally overlooked, and they can be considered as one of the candidates for the source of idiopathic SAH.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Arterial fenestrations are vascular anomalies in which the parent artery divides into two distinct endothelium-lined channels over a certain section of its length [1]. Fenestrations are rare findings on traditional 2D angiography, but are observed more frequently in autopsy studies or surgical investigations. The frequency of arterial fenestrations detected by traditional 2D angiography was 0.7 % in a retrospective survey of more than 5,000 angiographic examinations, whereas fenestrations in the anterior communicating artery (ACoA) complex alone were present in 20 to 40 % of autopsy cases and in 20 % of a surgical series [2–4]. Despite their probably common prevalence as indicated by anatomical studies, the relative scarcity of fenestrations discovered by traditional diagnostic modalities has until recently hindered their detailed examination. They were widely considered to be rare, and accordingly, most papers on fenestrations were case reports.
However, the improvement achieved in the resolution of imaging modalities and the possibility of 3D reconstruction has now made it possible to detect fenestrations more effectively. Most fenestrations are visible from only one specific viewing angle, which is probably not present among the limited available projections of conventional angiography. With 3D imaging, any desired viewing angle can be reconstructed. Hence, the reported proportions of fenestrations detected with recent diagnostic procedures are currently approaching those reported from anatomical studies. With the use of this technique, the occurrence of fenestrations in the ACoA complex was first reported in 2008 as 5.3 % [5]. Then, on the use of CT angiography with 3D reconstruction, two studies detected the presence of fenestrations in 10.5 and 12.9 % of angiography cases [6, 7]. The most recent known study, again involving the application of 3DRA, demonstrated intracranial arterial fenestrations in 28 % of the patient population [1].
Spontaneous subarachnoid haemorrhage (SAH) is generally caused by the rupture of a cerebral arterial aneurysm. The gold standard with which to locate the source of the bleeding, usually an aneurysm, is four-vessel 2D angiography; however, in 5 to 15 % of the cases the source of the haemorrhage remains undetected, even after repeated angiography and multimodal neuroradiological evaluation. In several published series, the prognosis of patients undergoing this idiopathic SAH (ISAH) has been found to be better than that in those with a demonstrable bleeding source (aneurysmal SAH = ASAH) [8–12]. In a subpopulation of the angiography-negative SAH patients (i.e. the ISAH cases), the extravasated blood is seen to be confined to the cisterns around the midbrain (perimesencephalic SAH) on early CT scans. This subpopulation constitutes 1/3 to 2/3 of the ISAH cases, regarded as involving the most benign type, usually with mild clinical symptoms and signs and a good outcome [9]. The aetiology of ISAH is still unclear. Possible explanations include undetectable aneurysms, ruptured microaneurysms, arterial dissection or vascular malformations [11, 13–16].
Following the introduction of the 3DRA method in daily clinical work, we too observed a high rate of fenestrations among our patients. Fenestrations were identified in many of the ISAH cases, even though no hint was to be found in the literature regarding fenestrations as a possible source of SAH.
These preliminary findings led us to conduct a prospective systematic investigation of this problem, including the incidence of fenestrations in patients admitted for the treatment of intracranial aneurysm(s), the incidence of fenestrations in patients admitted for the treatment of SAH and the incidence of fenestrations in patients with ISAH. The relationship of the location of the arterial fenestrations with that of the clot as assessed by CT was also studied.
Methods
Angiography
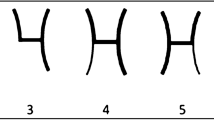
In all patients with possible intracranial aneurysms (a clinical diagnosis of subarachnoid bleeding or an accidental finding with other imaging modalities), conventional four- or six-vessel intra-arterial digital subtraction angiography is performed. When an aneurysm is suspected, 3DRA is also performed on the vessel harbouring the aneurysm in order to confirm its presence and to evaluate its anatomy. 3DRA of the ACoA complex is additionally performed routinely in all cases because of the high occurrence rate of aneurysms in this location and since the intricate structure of this complex does not allow appropriate examination by means of conventional 2D angiography because of the limited number of projection angles. Special care was taken to look for the presence of fenestrations in all investigations.
Angiographic Imaging was performed on a biplane neuroangiographic unit (Integris Allura; Philips Medical Systems, Best, The Netherlands), while 3DRA was performed with an 8-s 180° rotational run with the acquisition of 100 images, 3–4 ml of contrast material being injected per second into the internal carotid or vertebral artery. On a dedicated workstation, 3D reconstruction was achieved in a maximal matrix of 1,024 × 1,024 × 1,024.
Patient material
This consecutive, prospective study included all patients between January 2009 and April 2011 who were investigated and treated for CT-proven spontaneous SAH and also those who were referred to our institution following the accidental discovery of aneurysms elsewhere. A total of 287 patients were investigated during this period, of whom 174 presented with spontaneous subarachnoid bleeding as proven by CT within 48 h postbleeding, while the remaining 113 patients presented with various complaints and accidentally discovered non-ruptured aneurysms. The suspicion of an aneurysm was based on either CT or CT angiography or MR or MR angiography.
In the ISAH cases, despite the CT-proven subarachnoid haematoma, no bleeding source could be identified on high-resolution, six-vessel cerebral catheter angiograms with 3D rotational images and by consecutive, repeated cerebral catheter angiography or CTA/MRA examinations.
Patients with ISAH were further categorised as having either perimesencephalic or non-perimesencephalic SAH on the basis of the CT criteria defined by van Gijn et al. [17]. According to this grouping, in perimesencephalic SAH the centre of the haemorrhage was located ventrally to the brainstem, mainly in the interpeduncular cistern, with or without extension to the ambient, chiasmatic and horizontal part of the Sylvian cisterns, and without intraventricular blood, except for blood resulting from sedimentation effects.
All patients were regularly followed up after the start of the prospective study, with a regular careful search for clinical events suggestive of rebleeding or anatomical recanalization of an occluded aneurysm.
Statistical analysis
The data and variables in the various groups of patients were analysed using the χ 2 test. A p value of 0.05 or less was considered statistically significant.
Results
Among the 174 patients with spontaneous SAH an aneurysm was diagnosed as the cause of the bleeding in 153, whereas in 21 (12.1 %) the source remained unidentified (ISAH) on the use of six-vessel cerebral catheter angiography supplemented with 3D reconstruction (Fig. 1). In 14 of these 21 ISAH cases a second and in 6 even a third catheter angiography or CTA/MRA examination was performed. In 16 of the 21 (76.2 %) ISAH patients, the initial CT scans revealed perimesencephalic SAH. Four ISAH patients exhibited diffuse bleeding symmetrically filling the basal cisterns, and in 1 patient a blood clot was present frontally in the interhemispheric fissure.
Of the 153 patients with ASAH, 113 were female and 41 male (female:male ratio: 2.8:1). Of the 21 ISAH patients, 11 were female and 10 male (female:male ratio: 1.1:1). The difference in sex distribution between the ASAH and ISAH patients was close to being statistically significant (p = 0.08).
Fenestrations were present in 62 (23.3 %) of the 266 patients with an aneurysm (113 occidental and 153 ruptured aneurysms), in 27 (23.9 %) of the 113 patients admitted with an accidental aneurysm and in 35 (22.9 %) of the 153 patients with ASAH.
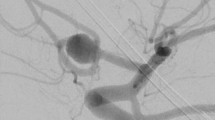
Concerning the incidence of fenestrations in patients with ISAH, fenestrations were detected in 20 of the 21 ISAH patients, i.e. a rate of 95.2 %. The frequency of fenestration occurrence in the ISAH group was significantly higher than in the other two groups (p < 0.01) (Fig. 1). Eighteen fenestrations were located in the ACoA region (Fig. 2a, b, c, d; Fig. 3a, b, c, d), while the remaining two were associated with the basilar artery complex (Fig. 4a, b).
a 2D carotid angiogram of both sizes in an ISAH patient in conventional AP view showing no abnormallity. b 3D reconstruction of the ACoA region following rotational angiography reveals the possible presence of fenestration of the ACoA. c-d 2D angiography in a non-conventional angle, which is perpendicular to the plane of the fenestration suspected on the 3D image, confirms the presence of fenestrations of the ACoA
a 2D carotid angiogram of both sizes in another ISAH patient in conventional AP view showing no abnormallity. b 3D reconstruction of the ACoA region following rotational angiography reveals the possible presence of fenestration of the ACA-ACoA junction. (c-d) 2D angiography in a non-conventional angle, which is perpendicular to the plane of the fenestration suspected on the 3D image, confirms the presence of fenestrations of the ACA-ACoA junction
The overall incidence of fenestrations in different locations in the ASAH group was ACoA-ACA: 66 %, ACM: 9 %, ACP-ACoP: 6 %, ACI: 3 % and AB: 20 %. In the patients operated on with accidental aneurysms, the incidence was ACoA-ACA: 52 %, ACM: 19 %, ACP-ACoP: 4 %, ACI: 7 % and AB: 11 %, while in two cases fenestrations were found on the PICA.
The ISAH patients have been regularly followed up, and no clinical episodes indicative of rebleeding have been reported to date.
Discussion
The radiological demonstration of fenestrations used to be exceptional despite the knowledge of their more frequent detection in autopsy and surgical studies [2–4]. With the advent of 3D reconstruction and the improvement in the resolution of imaging modalities, however, it has become possible to depict the thin channels of fenestrations. In recent years, the reported incidence of angiographically demonstrated fenestrations has increased continuously [1, 5–7]. The overall rate of fenestrations revealed in our patient population is nearly identical to that reported by van Rooij et al. (28.6 % vs. 28 %), the most recent report on the angiographic demonstration of intracranial arterial fenestrations [1]. Fenestrations were previously not suspected of being the origin of ISAH, but our present findings of the presence of intracranial arterial fenestrations in nearly all of our ISAH cases (95.2 %), in marked contrast with the more infrequent occurence in patients with aneurysmal bleeding and in patients harbouring non–ruptured aneurysms (22.9 and 23.9 %, respectively), permit the assumption that fenestrations may be one of the possible sources of the bleeding.
In the quest for the mysterious cause of the idiopathic bleeding, undetected or thrombosed aneurysms have been of major concern, but repeat angiography has yielded a definite lesion in only a minor proportion of the cases [18–21]. The possibility of a false-negative first angiography finding is lowest in the perimesencephalic SAH group, although a ruptured aneurysm, especially if located in the posterior circulation, can cause this haemorrhage pattern [8, 21].
Another finding against the possible aneurysmal origin of the ISAH is the difference in sex distribution between ISAH and ASAH. In contrast with the female predilection in ASAH, more male patients presented with angiographically negative SAH [9, 12, 22, 23]. We have experienced a similar situation: in ASAH the female:male ratio was 2.8:1, while in ISAH it was 1.1:1, a difference that nearly reached statistical significance, despite the small sample size in the ISAH group.
In perimesencepahlic haemorrhage, the localised, limited extent of bleeding, the slow onset of the symptoms and the benign clinical course suggest a low-flow, low-pressure source.
Ruptured microaneurysms on basilar artery perforators, a ruptured dissecting haematoma of the basilar artery, capillary teleangiectasia and a cryptic arterio-venous malformation have all been suggested as possible causes [11, 13, 14, 24, 25]. Regardless of the methods of investigation, and even with the aid of surgical exploration, researchers have failed to identify any source of the haemorrhage in most of the cases [13]. The primitive drainage pattern of the basal vein of Rosenthal was recently shown to occur significantly more frequently in patients with perimesencephalic bleeding than in ASAH or control patients, an observation that led to the hypothesis a causative role of anomalous venous drainage [16, 26]. Interestingly, a similar proportion of a primitive drainage pattern was observed in non-perimesencephalic ISAH cases. The investigators suggested the possibility that patients with ISAH may show different presentations of the same pathological entity. Thus, the origin of the bleeding may be the same, but there may be differences in the total amount of blood filling the subarachnoid space [16].
Abnormal drainage of the basal vein of Rosenthal was reported to be present in only half of the ISAH cases, whereas, fenestrations were detected in nearly all of our cases.
Fenestrations are thought to originate from the inappropriate fusion of paired embryologic vessels or from the incomplete obliteration of primitive vascular anastomoses during the development of the cerebral vascular system [3, 27]. The primitive drainage pattern of the basal vein of Rosenthal is a result of the maldevelopment of longitudinal anastomoses between the primitive veins during the embryo stage [28]. Hence, fenestrations and the persistence of the primitive veins could be two presentations of a common vascular developmental anomaly.
We cannot state definitively that fenestrations are the origin of ISAH, but they may be associated with the true source of the bleeding. The nearly 100 % incidence suggests a strong connection. A structural wall weakness, a defect in the muscularis layer of the vessel at each end of the fenestrations, was identified, which could theoretically make them prone to rupture [29–31]. Apart from two fenestrations on the basilar artery, all were located in the ACoA region in our case material. The clot localisation was perimesencephalic in 16 and symmetrically diffuse in 4 patients harbouring fenestrations, and there was therefore no obvious discrepancy between the supposed source and the location of the blood. A bleeding source in the ACoA region and a clot situated in front of the brainstem might seem to be conflicting from an anatomical perspective, but we consider that it is not impossible that sedimentation of the extravasated blood in the subarachnoidal, cisternal space would cause this pattern in a recumbent patient. The only ISAH patient in whom fenestration was not detected had a haematoma confined to the interhemispheric fissure.
The rupture of the thin (sometimes 0.1–0.3 mm) channels of a fenestration might result in less severe bleeding than the rupture of an aneurysm measuring several millimetres, which could be an explanation for the milder symptoms and better outcome that are specific to ISAH.
Despite the development of imaging techniques, the source of the bleeding remains unidentified in 10 % of the patients with SAH. Although these patients tend to have fewer complications and are expected to have a better outcome, hydrocephalus, vasospasm and rebleeding may occur, and some may even die or be forced to live with serious disabilities. Even after "benign" perimesencephalic SAH, neuropsychological problems are frequent. It is quite clearly not a harmless disease, and its origin should be pinpointed. Sources other than an aneurysm have been suspected, but this question is so far unresolved.
Conclusions
We detected arterial fenestrations in 23.9 % of our patients admitted for the treatment of an unruptured intracranial aneurysm and in 22.9 % of those treated for an intracranial aneurysm causing SAH. In contrast, in the patients in whom the source of the SAH was not found (ISAH), arterial fenestrations were located in 95.2 %. In view of the significantly higher frequency of such fenestrations (usually overlooked) in ISAH, arterial fenestrations may be one of the likely candidates as the source of ISAH.
References
van Rooij SB, van Rooij WJ, Sluzewski M, Sprengers ME (2009) Fenestrations of intracranial arteries detected with 3D rotational angiography. AJNR Am J Neuroradiol 30:1347–1350
Gomes FB, Dujovny M, Umansky F, Berman SK, Diaz FG, Ausman JI, Mirchandani HG, Ray WJ, Mirchandani HG, Ray WJ (1986) Microanatomy of the anterior cerebral artery. Surg Neurol 26:129–141
Sanders WP, Sorek PA, Mehta BA (1993) Fenestration of intracranial arteries with special attention to associated aneurysms and other anomalies. AJNR Am J Neuroradiol 14:675–680
Serizawa T, Saeki N, Yamaura A (1997) Microsurgical anatomy and clinical significance of the anterior communicating artery and its perforating branches. Neurosurgery 40:1211–1216
de Gast AN, van Rooij WJ, Sluzewski M (2008) Fenestrations of the anterior communicating artery: incidence on 3D angiography and relationship to aneurysms. AJNR Am J Neuroradiol 29:296–298
Bayrak AH, Senturk S, Akay HO, Ozmen CA, Bukte Y, Nazaroglu H (2011) The frequency of intracranial arterial fenestrations: a study with 64-detector CT-angiography. Eur J Radiol 77:392–396
Bharatha A, Aviv RI, White J, Fox AJ, Symons SP (2008) Intracranial arterial fenestrations: frequency on CT angiography and association with other vascular lesions. Surg Radiol Anat 30:397–401
Andaluz N, Zuccarello M (2008) Yield of further diagnostic work-up of cryptogenic subarachnoid hemorrhage based on bleeding patterns on computed tomographic scans. Neurosurgery 62:1040–1046
Greebe P, Rinkel GJ (2007) Life expectancy after perimesencephalic subarachnoid hemorrhage. Stroke 38:1222–1224
Ildan F, Tuna M, Erman T, Gocer AI, Cetinalp E (2002) Prognosis and prognostic factors in nonaneurysmal perimesencephalic hemorrhage: A follow-up study in 29 patients. Surg Neurol 57:160–165
Rinkel GJ, van Gijn J, Wijdicks EF (1993) Subarachnoid hemorrhage without detectable aneurysm. A review of the causes. Stroke 24:1403–1409
Sarabia R, Lagares A, Fernandez-Alen JA, Arikan F, Vilalta J, Ibáñez J, Maillo A, Gabarros A, Domínguez J, Horcajadas A, Ballenilla F, Rodríguez-Boto G, Llacer JL, Arrese I, de la Lama A, Santamarta D, Delgado P, Muñoz MF (2010) Idiopathic subarachnoid hemorrhage: a multicentre series of 220 patients. Neurocirugia (Astur) 21:441–451
Matsumaru Y, Yanaka K, Muroi A, Sato H, Kamezaki T, Nose T (2003) Significance of a small bulge on the basilar artery in patients with perimesencephalic nonaneurysmal subarachnoid hemorrhage. Report of two cases. J Neurosurg 98:426–429
Schievink WI, Wijdicks EF (2000) Origin of pretruncal nonaneurysmal subarachnoid hemorrhage: ruptured vein, perforating artery, or intramural hematoma? Mayo Clin Proc 75:1169–1173
Sheehan JM, Cloft H, Kassell NF (2000) Symptomatic delayed arterial spasm following non-aneurysmal perimesencephalic subarachnoid hemorrhage: a case report and review of the literature. Acta Neurochir (Wien) 142:709–712
Song JH, Yeon JY, Kim KH, Jeon P, Kim JS, Hong SC (2010) Angiographic analysis of venous drainage and a variant basal vein of Rosenthal in spontaneous idiopathic subarachnoid hemorrhage. J Clin Neurosci 17:1386–1390
van Gijn J, van Dongen KJ, Vermeulen M, Hijdra A (1985) Perimesencephalic hemorrhage: a nonaneurysmal and benign form of subarachnoid hemorrhage. Neurology 35:493–497
Bradac GB, Bergui M, Ferrio MF, Fontanella M, Stura G (1997) False-negative angiograms in subarachnoid haemorrhage due to intracranial aneurysms. Neuroradiology 39:772–776
Hashimoto H, Iida J, Hironaka Y, Okada M, Sakaki T (2000) Use of spiral computerized tomography angiography in patients with subarachnoid hemorrhage in whom subtraction angiography did not reveal cerebral aneurysms. J Neurosurg 92:278–283
Inamasu J, Nakamura Y, Saito R, Horiguchi T, Kuroshima Y, Mayanagi K, Orii M, Ichikizaki K (2003) “Occult” ruptured cerebral aneurysms revealed by repeat angiography: result from a large retrospective study. Clin Neurol Neurosurg 106:33–37
Rinkel GJ, Wijdicks EF, Hasan D, Kienstra GE, Franke CL, Hageman LM, Vermeulen M, van Gijn J (1991) Outcome in patients with subarachnoid haemorrhage and negative angiography according to pattern of haemorrhage on computed tomography. Lancet 338:964–968
Hui FK, Tumialan LM, Tanaka T, Cawley CM, Zhang YJ (2009) Clinical differences between angiographically negative, diffuse subarachnoid hemorrhage and perimesencephalic subarachnoid hemorrhage. Neurocrit Care 11:64–70
Kang DH, Park J, Lee SH, Park SH, Kim YS, Hamm IS (2009) Does non-perimesencephalic type non-aneurysmal subarachnoid hemorrhage have a benign prognosis? J Clin Neurosci 16:904–908
Hsu W, Pradilla G, Garonzik IM, Conway JE (2010) Pretruncal nonaneurysmal subarachnoid hemorrhage causing basilar artery vasospasm. Neurocrit Care 13:256–260
Park SQ, Kwon OK, Kim SH, Oh CW, Han MH (2009) Pre-mesencephalic subarachnoid hemorrhage: rupture of tiny aneurysms of the basilar artery perforator. Acta Neurochir (Wien) 151:1639–1646
Alen JF, Lagares A, Campollo J, Ballenilla F, Kaen A, Nunez AP, Lobato RD (2008) Idiopathic subarachnoid hemorrhage and venous drainage: are they related? Neurosurgery 63:1106–1111
Padget DH (1948) The development of the cranial arteries in the human embryo. Contrib Embryol 32:205–261
San Millan Ruiz D, Gailloud P, Rufenacht DA, Delavelle J, Henry F, Fasel JH (2002) The craniocervical venous system in relation to cerebral venous drainage. AJNR Am J Neuroradiol 23:1500–1508
Black SP, Ansbacher LE (1984) Saccular aneurysm associated with segmental duplication of the basilar artery. A morphological study. J Neurosurg 61:1005–1008
Crompton MR (1962) The pathology of ruptured middle-cerebral aneurysms with special reference to the differences between the sexes. Lancet 2:421–425
Finlay HM, Canham PB (1994) The layered fabric of cerebral artery fenestrations. Stroke 25:1799–1806
Conflicts of interest
The authors do not have any personal or institutional financial interest in the drugs, materials, or devices described in this submission.
Funding
The Hungarian National Research Council supported this study with grant TAMOP 4.2.2.A-11.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hudák, I., Lenzsér, G., Lunenkova, V. et al. Cerebral arterial fenestrations: a common phenomenon in unexplained subarachnoid haemorrhage. Acta Neurochir 155, 217–222 (2013). https://doi.org/10.1007/s00701-012-1587-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-012-1587-7