Abstract
Background
Although acetazolamide-challenged single-photon emission CT (SPECT) is recommended before carotid endarterectomy (CEA) and carotid artery stenting (CAS), given the relationship between preoperative decreased cerebrovascular reserve (CVR) and postoperative cerebral hyperperfusion syndrome (CHS), it is controversial whether all cases should be checked.
Methods
I-IMP-SPECT at rest was performed for 65 operative cases of carotid stenoses. At preoperative MR angiography we classified cases into two groups: G, featuring an anterior communicating artery with bilateral A1 with/without posterior communicating arteries; and P, a poor-escape-route group which did not match these criteria. Postoperative rCBF patterns were divided into two types: B, bilateral rCBF increase; and I, ipsilateral rCBF increase.
Results
Cases with high postoperative increase rate of rCBF were most frequently found in Group P and the Type I cases (p < 0.001). All four cases with hyperemia or hyperperfusion belonged to Group P. Only two out of 48 patients in Group G were Type I, both demonstrating a preoperative rCBF decrease rate more than 10 % as compared to the contralateral side.
Conclusions
From the present study, preliminary analysis of escape routes by preoperative MR angiography before surgical treatment of carotid stenosis is recommended and CVR investigation with acetazolamide-challenge SPECT should be considered for those relatively few cases with poor escape routes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cerebral hyperperfusion syndrome (CHS) occurs in 0.2–18.9 % [8] of cases after surgical treatment of carotid stenosis, sometimes leading to deleterious intracerebral hemorrhage [1, 12, 16]. Since it has been reported to be closely associated with low cerebral vascular reserve (CVR), preoperative acetazolamide-challenge single-photon emission CT (SPECT) has been recommended for prediction purposes [5, 14]. It is, however, controversial as to whether every case needs preoperative drug-challenge SPECT, considering the potential side effects of acetazolamide [17], the relatively low frequency of CHS, and medico-economic aspects [11, 14].
Other risk factors for CHS have been well-studied, such as severe ipsilateral stenosis over 90 %, perioperative hypertension and use of antiplatelet agents or other anticoagulants [9, 20]. Impaired collateral blood flow secondary to advanced occlusive disease has also been reported to increase risk. The presence of collateral vessels has, furthermore, been a focus of attention [4, 18, 21], but generally as suppliers of blood flow to the perfusing area. Absence of such vessels was found to be associated with vulnerability of the affected area, although Hosoda et al. [4] reported the degree of internal carotid artery (ICA) stenosis to be a more significant determinant of CVR than collateral pathways. When viewed from the drainage side, however, the anterior communicating artery (AcoA), bilateral A1 branches of anterior cerebral artery (ACA) and posterior communicating artery (PcoA) could work as postoperative evacuation routes of increased blood from a reconstructed ICA to the operative hemispheres.
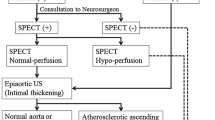
We, therefore, investigated whether it might be possible to narrow down cases with a high likelihood of hyperperfusion after carotid endarterectomy (CEA) or carotid artery stenting (CAS)—in other words, those truly needing confirmation of CVR with acetazolamide-challenge SPECT—by screening for the presence of escape routes by preoperative MR angiography with or without plain SPECT.
Patients and methods
Patient population and surgical treatments
From November 2004 to August 2011, 95 consecutive cases with carotid stenoses underwent surgical treatment at Nagoya City University Hospital. Among them, a total of 65 patients (70.0 ± 5.6 y/o, M:F = 55:10, symptomatic : asymptomatic = 45:20, mean degrees of stenosis 77.9 ± 10.7 %) who fulfilled the following criteria were enrolled in the present study: 1) having either CEA or CAS surgical treatment for unilateral internal carotid artery stenosis of 60 % or over; 2) showing no major cerebral infarction on either side of the cerebral hemisphere on MRI; 3) maintaining useful function (modified Rankin Scale, 0, 1 or 2); and 4) undergoing both pre- and postoperative regional cerebral blood flow (rCBF) studies with SPECT by autoradiography [7] (Fig. 1). As normalization in SPECT analysis has been reported to be biased and unreliable in cases with bilateral CBF reduction [6], bilateral carotid stenosis cases with contralateral IC stenosis over 60 % were excluded (mean degree of contralateral stenosis 12.9 ± 22.3 %). Excluded cases were three of occlusion and four of high-degree stenosis of contralateral carotid arteries. Eighteen cases were excluded for absence of preoperative SPECT due to operative schedule. Five cases were excluded for absence of immediate postoperative SPECT due to the patients’ condition. Among them, two cases with CHS, one embolic infarction, and one myocardial infarction received intensive care at ICU/CCU (intensive/coronary care unit) after CAS, while the remaining case showed remarkable restless after CEA which preclude keeping calm during the examination without sedatives which might affect rCBF. No patients were excluded for the preoperative presence of major infarction or severe disability. The ethics guidelines for clinical studies by the Japanese Health Labor and Welfare Ministry (2007) were strictly observed, while informed patient consent was not required for this retrospective study.
a Patient selection and grouping. A total of 65 out of 95 surgically treated patients with unilateral carotid stenosis were selected as fulfilling our established criteria. Cases with good escape routes such as bilateral A1 of anterior cerebral arteries and anterior communicating artery (AcoA) from blood perfusing area by the reconstructed operation were classified as Group G, while cases with poor escape routes formed Group P. Postoperative states were divided into Type B with bilateral blood increase or distribution and Type I with ipsilateral increase
Surgical indications for the treatment of carotid stenosis adhered to the criteria of NASCET [13] and ACAS [3] studies. For cases with conditions matching the criteria for CEA-high-risk patients in the SAPPHIRE [22] study, such as severe heart or lung disease, age older than 80 years, and/or occlusion or high-degree stenosis of the contralateral carotid artery, CAS was chosen rather than CEA (CAS 28 cases; 70.5 ± 6.0 y/o, M:F = 27:1, symptomatic : asymptomatic = 19:9, mean degrees of stenosis 75.6 ± 11.4 %, mean degrees of contralateral stenosis 13.9 ± 24.4 %). From November 2010, patients >70 years old without other high-risk factors underwent CEA according to the results of the CREST [2] study which advocated CEA priority for the treatment of elderly patients (CEA 37 cases; 69.7 ± 5.4 y/o, M:F = 28:9, symptomatic : asymptomatic = 26:11, mean degree of stenosis 79.8 ± 9.8 %, mean degree of contralateral stenosis 12.4 ± 21.6 %). CEA was performed in a standard way with intraluminal shunt and primary closure and CAS using either a PRECISE® (Cordis, Bridgewater, NJ) stent or a Wallstent® (Boston Scientific, Freemont, CA) and filter (Angioguard XP®, Cordis, Bridgewater, NJ), distal balloon (PercuSurge® Guardwire, Medtronic, Santa Rosa, CA) and/or flow reversal (Patlive®, Terumo Clinical Supply, Japan) protection devices.
Evaluation by MR angiography
MR angiography was preoperatively performed in all patients within 1 month before surgery, evaluating the delineation of bilateral A1 of ACA, AcoA and bilateral PcoA. Three-dimensional time-of-flight (TOF) MR angiographs were obtained with a 1.5-T imaging system (Gyroscan Integra, Philips, Netherlands) using a sensitivity-encoding parallel-imaging head coil. Scan parameters were as follows: 3D-T1 fast field echo sequence, TR 17 ms, TE 6.9 ms, flip angle 20°, section thickness 1.2 mm, field-of-view 17.0 cm, number of excitations one, scan time 3 min 38 s, three slabs, 120 slices.
We classified the cases into two groups by the delineation of vessels with preoperative MR angiography as follows: Group G, good-escape-route group with AcoA and bilateral A1 with/without ipsilateral PcoA; and Group P, poor-escape-route group which did not fulfill the criteria of Group G. Patterns of escape routes observed in this series are shown in Fig. 2.
Variation in collateral pathways as escape routes observed in the enrolled cases. Dotted lines indicate estimated evacuation routes of increased blood flow from the reconstructed internal carotid artery (ICA). G1-4 belong to good-escape-route group (Group G) and P1-9 belong to the poor-escape-route group (Group P)
To avoid inter-reader variability, a single well-experienced neurosurgeon (HK) who was blinded to patient data at the time of judgment performed the above evaluation in random order.
Evaluation of CBF
Preoperative N-isopropyl-p-[123I]- iodoamphetamine (IMP)-SPECT at rest was performed within 1 month before the operation and postoperative SPECT 2 days after the operation in all cases. After a drip infusion line was introduced intravenously, subjects were given a 1-min injection of 123I-IMP, 167 MBq intravenously while resting in the supine position with their eyes open. Data acquisition was performed at a midscan time of 30 min after the 123I-IMP administration for the scan duration of 20 min. SPECT images were obtained using a dual-head gamma camera system (E.CAM; Siemens, Erlangen, Germany) equipped with high-resolution fan-beam collimators. For data acquisition, we used a 128 × 128 matrix for 36 steps of 5°, in a 422-mm field of view, at 5-mm slice thickness. The acquisition time was 30 s per step. The images were reconstructed using the filtered back projection technique, with attenuation correction made by detecting the edge of the object. An attenuation coefficient of 0.05 cm−1, a Butterworth filter (cutoff = 0.4 cycle/cm; order = 8), and a ramp filter were used for image reconstruction.
Analysis of brain SPECT was performed using a 3-dimensional stereotactic region of interest (ROI) template 3DSRT® [version 3 (FineSRT®), Fuji film RI Pharma Co., Tokyo, Japan] [19], applying anatomical standardization and an ROI template for the whole brain with the SPM (statistical parametric mapping) algorithm as reported previously [20]. Briefly, FineSRT is fully automated whole brain ROI analysis software, and there is no dispersion derived from differences in the subject, observer, or facility with excellent reproducibility. For SPECT data analysis using FineSRT, the patient’s brain data are first combined with those in Talairach’s stereotactic brain atlas in normalization. The automated ROI template was placed on the brain, and a radioisotope (RI) count was determined for each ROI and each segment, where each segment consisted of many ROIs. The template ROI used for FineSRT consisted of 1,624 ROIs with 46 segmented areas on each side, referring to Brodmann’s and brain vessel perfusion areas. FineSRT is good at sampling, even for surface and sulcus gray matter activity, while the other widely-used normalization method, 3D-SSP, is not capable of such sampling [6].
Postoperative rCBF patterns of all cases were divided into two types as follows: Type B, showing almost even CBF increase in bilateral ROIs in both cerebral hemispheres; and Type I, showing ipsilateral rCBF increase on the operative side more than twice that of the contralateral side in more than three ROIs. There were no cases that showed more rCBF increase in the contralateral side than the ipsilateral one.
Postoperative hyperemia and hyperperfusion were respectively defined as rCBF increases of more than 80 and 100 % [14] compared to the preoperative values in more than one ROI. CHS was defined as having symptoms like seizures, deterioration of consciousness level, focal neurological signs, with or without postoperative ICH, and no evidence of new postoperative ischemia. Postoperative systolic blood pressure (BP) was maintained within the normal range (120–140 mmHg) with intravenous administration of nicardipine if necessary.
Statistical analysis
All statistical evaluations were performed with statistical software (Statview version 5.0, SPS, NC), and all results are presented as mean ± SD values. Wilcoxon ranking analysis was used to compare the increase rate of rCBF between the operative and the contralateral sides. For the comparison of rCBF increase rates between Groups G and P or Types B and I, the Mann-Whitney U-test was applied. For multivariate analysis, a logistic regression model was used. Values of p < 0.01 were considered significant.
Results
The characteristics and data for all cases are shown in Table 1. Among 65 enrolled cases, 48 (73.8 %) belonged to Group G (CEA:CAS = 25:23) and 17 (26.2 %) to Group P (CEA:CAS = 12:5) (Fig. 1). The type B postoperative rCBF pattern was observed in 49 cases (75.4 %) and Type I in 16 (24.6 %). Forty-six cases (95.8 %) in Group G and three (17.6 %) in Group P were Type B. Two cases in Group G (4.2 %) and 14 cases (82.4 %) in Group P were Type I. There were no remarkable differences between CEA and CAS. A comparison of mean postoperative increase rates of rCBF on the operative side to those on the contralateral side revealed a significant difference in Group P (24.8 ± 25.8 vs. 19.8 ± 24.8 %, p < 0.001), but not Group G (17.3 ± 15.5 vs. 15.3 ± 15.7 %).
The mean increase rates of rCBF on the operative side were 17.3 ± 15.5 % in Group G and 24.8 ± 25.8 % in Group P (p < 0.001), whereas they were 16.8 ± 16.0 % in Type B and 27.0 ± 24.6 % in Type I (p < 0.001). Cases with a high postoperative increase rate of rCBF were most frequently found in Group P and Type I (Fig. 3). The same tendency was observed for both CEA and CAS, although the rCBF increase rate was generally higher in CAS cases (14.7 ± 17.4 % vs. 24.3 ± 19.9 %, p < 0.001).
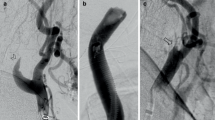
Hyperemia and CHS
There were two patients that showed hyperemia, one undergoing CAS (Case 58, Table 1) and the other CEA (Case 60). Both patients belonged to Group P (bilateral A1 but without AcoA, P9 in Fig. 2) and were Type I. Although the mean rCBF increase rates of the operative sides were 83.8 and 82.8 %, respectively, neither patient showed any neurological symptoms due to hyperemia.
There were two CAS patients showing CHS during the investigated period. As their poor conditions prevented SPECT 2 days after the operation, which was mandatory to fulfill the criteria of the enrollment, both patients were excluded from further analysis (Fig. 1). The first case was a 74-yearold man with atrial fibrillation controlled with warfarin underwent CAS for 83 % asymptomatic stenosis of right carotid. Preoperative evaluation revealed right A1 without AcoA and left A1 on MR angiography, placing him in this study’s Group P. There were no apparent low rCBF areas on the preoperative SPECT at rest. A postoperative CT disclosed massive intracranial hemorrhage (ICH) on the right hemisphere after successful stent placement. The other case was an 80-year-old woman with 95 % stenosis of the right carotid. Preoperative MR angiography demonstrated right A1 and AcoA without left A1, again corresponding to Group P. A mild decrease in the right hemisphere (85 % of the normal value) was observed on preoperative SPECT at rest. She showed hypovolemic shock due to bleeding for anticoagulation after successful stent placement but recovered without neurological deficit. On the sixth postoperative day, she showed sudden general convulsion and deterioration of consciousness with no evidence of new infarction, presumed to be ascribable to hyperperfusion or reperfusion syndrome [10]. Postoperative SPECT after one month revealed a relative rCBF increase on the operative side, corresponding to Type I in the present study (data not shown).
Evaluation of type I in group G
In Group G, only two patients (4.2 %) were classified as Type I (Fig. 1). One was a 58-year-old man with symptomatic 90 % stenosis of the right carotid artery in the CEA group. The other was a 77-year-old man in the CAS group with symptomatic 76 % stenosis of the right carotid artery. MR angiography showed bilateral A1 and AcoA in both. Although postoperative SPECT showed no apparent differences in mean rCBF values of the right and the left sides (42.3 ± 3.1 vs. 39.1 ± 4.0, 47.3 ± 5.1 vs. 47.2 ± 4.9 ml/100 g/min), the rCBF increase rate in the operative side was higher than that in the contralateral side in both patients (29.4 ± 10.9 vs. 5.6 ± 3.9 %, p < 0.001; 28.5 ± 5.0 vs. 5.3 ± 6.4 %, p < 0.001) due to preoperative low mean rCBF in the operative side (30.9 ± 3.1 vs. 34.9 ± 4.4 ml/100 g/min, p < 0.001; 36.7 ± 3.2 vs. 45.1 ± 6.6 ml/100 g/min, p < 0.001). The degrees of preoperative rCBF decrease in the operative side compared to the contralateral side of both patients were more than 10 % (11.5 and 18.6 %, respectively). On the other hand, among the remaining 46 patients in Group G showing Type B, most of the patients (93.5 %) demonstrated less than 10 % preoperative rCBF decrease rate in the operative side compared to the contralateral side, with only three patients as exceptions (Table 1). There may be a tendency that in Group G the patients with preoperative low rCBF on the operative side as compared to the contralateral side show postoperative predominant unilateral rCBF increase which may lead to hyperemia/hyperperfusion.
Involvement of PcoA
In Group G, the rCBF increase rates of both sides for the patients with ipsilateral PcoA were 16.4 ± 15.9 vs. 14.6 ± 16.2 % (N.S.), while those for the patients without ipsilateral PcoA were 17.9 ± 15.5 vs. 15.8 ± 15.6 % (N.S.). In Group P, the rCBF increase rates of both sides for the patients with ipsilateral PcoA were 28.4 ± 32.6 vs. 22.7 ± 26.6 % (p < 0.001), while those for the patients without ipsilateral PcoA were 23.4 ± 23.9 vs. 19.4 ± 25.1 % (p < 0.001). The presence of PcoA, thus, did not affect the difference in the laterality of the rCBF increase. Logistic regression analysis revealed an absence of ipsilateral A1 and AcoA to be a significant independent factor for postoperative Type I (both p < 0.001), but not bilateral PcoA as well as contralateral A1 (data not shown).
Discussion
In the present study, the cases with poor escape routes evaluated by preoperative MR angiography and with unilateral postoperative rCBF increase in the operative side tended to demonstrate a high increase rate of rCBF which may lead to hyperemia/hyperperfusion.
The patency of a collateral artery such as AcoA and of bilateral A1 arteries has been thought to relate to hyperperfusion after CEA/CAS because blood flow supplied from these vessels affects the rCBF and vascular reserve of the ACA and MCA areas [20]. In the present study, the importance of AcoA and A1 as escape routes was emphasized when the focus was excessive postoperative blood flow into the ICA-supplying area of the operative side.
Ogasawara et al. [14] reported that patients with postoperative hyperperfusion often featured a low vascular reserve, while Hosoda et al. [6] attached significance to baseline rCBF reduction for prediction of hyperperfusion. Not all patients, however, need investigation for CVR to predict hyperperfusion—especially considering the frequency of the event, the potential side effects of acetazolamide [17] and the medical costs of the procedure. Therefore, to avoid unessential examinations, cases with poor escape routes (Group P) are recommended to be selected by MR angiography first and then undergo further rCBF study with acetazolamide challenge to confirm the vascular reserve as designated in this study.
Regarding the concentration of blood flow in the hemisphere of the operative side, the present study indicated that there may be two major patterns of occurrence of hyperemia/hyperperfusion. One is the case in which a high rCBF increase rate on the operative side occurs even with intact escape routes because of preoperative decrease in the rCBF value [6], even though absolute postoperative rCBF values are comparable to those of the contralateral side. With this background, CHS or ICH may be evoked mainly due to the vulnerability of the perfused area. The other pattern involves a high rCBF increase rate with a higher absolute value of rCBF on the operative side as compared to the contralateral side because of the poor escape routes, leading to a unilateral abnormal rise.
In our series, the Group G cases showing Type I, which are at risk of hyperemia/hyperperfusion, numbered only two out of 48 patients (4.2 %). These cases showed a preoperative rCBF decrease rate more than 10 % compared to the contralateral side, though absolute values for postoperative rCBF of the cerebral hemisphere of the operative side remained normal. This is in line with previously reported results [6]. Therefore in Group G, hyperemia/hyperperfusion may arise under conditions of preoperative hypoperfusion of affected areas of ICA with stenosis, though the risk of CHS may be reduced because of divergence of blood flow through good escape routes. For the same reason, cases showing normal preoperative rCBF with decreased CVR could avoid CHS by limited, diffuse blood flow through escape routes.
Patients in whom poor escape routes were observed (Group P) in preoperative MR angiography occupied one fourth of all cases. In our series, all four cases with hyperemia or hyperperfusion belonged to this group. Among 17 Group P cases, 14 (82.4 %) showed Type I, which are thought to easily lead to hyperemia/hyperperfusion. So, patients with this group have higher risks for hyperemia/hyperperfusion. In the present study, the incidence of preoperatively depressed rCBF (more than 10 % compared to the contralateral side) was limited to only one in 17 in Group P cases (5.9 %). The preoperative depressions of rCBF of the two Group P hyperemia cases were small (5.0 and −0.5 %). These findings may suggest that a certain number of patients with hyperemia/hyperperfusion can be ascribed to the poor escape routes itself or cases with normal rCBF and decreased CVR. When patients with a decrease of rCBF and/or decreased CVR are added to the P-group cases, however, it is apparent that the possibility of CHS becomes greater, as previous researchers have described [5, 6, 14].
Therefore it can be argued that a CVR test with acetazolamide-challenge SPECT should be considered only in cases with poor escape routes (Group P). This would allow the narrowing down of candidates for drug-challenge SPECT to about one fourth of all patients. Where preoperative SPECT at rest is available, particular attention also should be paid to those few cases with good escape routes (Group G) having preoperatively depressed rCBF of the hemisphere of the ICA stenosis side. In most institutes, especially in small to medium-scale hospitals, post-CEA or CAS patients may be cared for in a general ward after the operation and if patients show severe headache or high BP in spite of ordinary BP treatment, strict systolic BP control under 100 using continuous drip infusion of nicardipine or diltiazem hydrochloride and ICU observation for sedation with thiopental or propofol [21]. We believe that our strategy using preoperative assessment of collateral pathways as escape routes would be useful to decide taking these advanced and aggressive measures to avoid CHS and also be cost-effective. It may be effective to decrease CHS cases with prophylactic administration of edaravon before carotid clamping in CEA for reduction of free radicals as pointed out by Ogasawara et al. [15] in suspected cases of hyperemia/hyperperfusion with poor escape routes.
The relevance of PcoA to collateral flow has been described previously [17], but no remarkable effect was observed in postoperative rCBF increase rates in either Groups G or P, whether ipsilateral PcoA was delineated or not, and bilateral PcoA was not a significant factor for unilateral rCBF increase on multivariate analysis. Thus the PcoA does not seem to be important at least as a postoperative escape route, in contrast to ipsilateral A1 and AcoA. Prediction of CHS by preoperative degree of MCA delineation by single slab 3.0-T MR angiography was proposed recently [11]. Cases with good delineation of MCA branches on the stenosis side appeared at low risk of decreased CVR, and hence CHS. With this method, cases with bilateral A1 but without AcoA so that blood flow to the ACA and MCA is supplied by each side of the ICA are considered to be at low risk of hyperperfusion due to sufficient preoperative blood flow and good CVR. In our present study, however, those cases seemed to be at high risk for hyperperfusion when escape routes were poor, concentrating cerebral blood flow on the operative hemisphere.
Differences between CEA and CAS regarding postoperative hyperperfusion have been discussed in several reports. Kaku et al. [9] reported the risk to be greater with CAS (6.6 % vs. 3.8 % for CEA). Ogasawara et al. [16] described a similar tendency, evaluating 4,494 patients. They also pointed out that hyperperfusion-associated ICH occurred most frequently within 12 h after CAS, but between 3 to 8 days after CEA. Moreover, subarachnoid hemorrhage was more often linked with CAS, and strict control of postoperative BP prevented the development of ICH after CEA but not after CAS. In the present study, the mean postoperative rCBF increase rate was higher after CAS than after CEA. Morrish et al. [12] described the possibility of a greater increase in CBF after CAS relative to CEA, at least acutely, and hence increased hyperperfusion injury, which corresponds to our results. The difference in timing and characteristics of ICH between CEA and CAS is thought to be ascribable to the strength of anticoagulation therapy, and the presence of ischemic cerebral lesions due to intraoperative emboli and reperfusion [16]. As far as escape routes are concerned, however, we could not find any obvious difference between CEA and CAS. Furthermore, no regional difference was detected in areas with increased rCBF, even by precise ROI analysis using FineSRT (data not shown).
There are some limitations to the present study which require mention. First, two CHS patients were not included in the present retrospective cohort for absence of immediate postoperative SPECT. However, two patients with ipsilateral hyperemia (rCBF increase >80 % compared to the preoperative state) were included in the cohort, both of which showed preoperative poor escape routes. We think this is an essentially valuable result to substantiate our hypothesis, since hyperperfusion (rCBF increase >100 % compared to the preoperative state) or CHS may not occur without ipsilateral rCBF increase as in hyperemia. On top of that, it may be important collateral evidence that both CHS patients in our study showing poor escape routes preoperatively which may lead to ipsilateral rCBF increase. Additional supplementary proof is that no description has been found in the previous major reports concerning CHS showing perilous bilateral rCBF increase as well as bilateral ICH due to CHS. All the representative cases shown in the literature demonstrated only ipsilateral rCBF increase [1, 4–6, 8, 9, 11, 12, 14, 16]. Secondly, the number of patients was relatively small, though the incidence of the CHS itself was also quite small. Further multi-center studies with larger numbers of patients are warranted to clarify the relationship between escape routes and hyperperfusion. Thirdly, the MRI used here was a 1.5-T system with lower spatial resolution than 3.0-T systems, though MR angiography with the 1.5-T system is accepted as more sensitive and specific for detection of decreased velocity of inflowing blood than that with 3.0-T systems [11]. Fourthly, although escape routes were evaluated with MR angiography by a single well-trained neurosurgeon blinded to the patient data in random order, the possibility of intraobserver bias cannot be precluded. Evaluation with authors including a radiologist showing the interobserver variability of their classification might be a better option. Fifthly, the nicardipine that was used to control the patients’ BP in the normotensive range may have affected their rCBF values. Lastly, the present result can not be applied to cases with a high degree of carotid stenosis bilaterally, because we limited the cases to unilateral stenosis to maintain the accuracy of rCBF evaluation by SPECT and normalization.
There appears to be no doubt that hemodynamic impairment is important for the occurrence of hyperperfusion. Making effective, economical and minimally invasive use of approaches to predict hyperperfusion by reduced CVR as proposed in the present study may have profound significance.
Conclusion
Preoperative evaluation and detection of poor escape routes with postoperative concentration of blood flow because of reconstructed ICA by MR angiography is recommended before surgical treatment of carotid stenoses. This should limit the cases that really need investigation of CVR by acetazolamide-challenge SPECT. If plain SPECT at rest is also affordable preoperatively, a drug-challenge test for CVR is reasonable for the few cases with decreased rCBF and good escape routes, as well as for those with poor escape routes.
References
Abou-Chebl A, Yadav JS, Reginelli JP, Bajzer C, Bhatt D, Krieger DW (2004) Intracranial hemorrhage and hyperperfusion syndrome following carotid arterystenting. J Am Coll Cardiol 43:1596–1601
Brott TG, Hobson RW II, Howard G, Roubin GS, Clark WM, Brooks W, Mackey A, Hill MD, Leimgruber PP, Sheffet AJ, Howard VJ, Moore WS, Voeks JH, Hopkins LN, Cutlip DE, Cohen DJ, Popma JJ, Ferguson RD, Cohen SN, Blackshear JL, Silver FL, Mohr JP, Lal BK, Meschia JF, Investigators CREST (2010) Stenting versus endarterectomy for treatment of carotid-artery stenosis. N Engl J Med 363:11–23
Endarterectomy for asymptomatic carotid artery stenosis. Executive Committee for the Asymptomatic Carotid Atherosclerosis Study (1995) JAMA 273: 1421–1428
Hosoda K, Fijita S, Kawaguchi T, Shose Y, Shibata Y, Tamaki N (1998) Influence of degree of carotid artery stenosis and collateral pathways and effect of carotid endarterectomy on cerebral vasoreactivity. Neurosurgery 42:988–994
Hosoda K, Kawaguchi T, Shibata Y, Kamei M, Kidoguchi K, Koyama J, Fujita S, Tamaki N (2001) Cerebral vasoreactivity and internal carotid artery flow help to identify patients at risk for hyperperfusion after carotid endarterectomy. Stroke 32:1567–1573
Hosoda K, Kawaguchi T, Ishii K, Minoshima S, Kohmura E (2005) Comparison of conventional region of interest and statistical mapping method in brain single-photon emission computed tomography for prediction of hyperperfusion after carotid endarterectomy. Neurosurgery 57:32–41
Iida H, Itoh H, Nakazawa M, Hatazawa J, Nishimura H, Onishi Y, Uemura K (1994) Quantitative mapping of regional cerebral blood flow using Iodine-123-IMMP and SPECT. J Nucl Med 35:2019–1030
Iwata T, Mori T, Tajiri H, Nakazaki M (2011) Predictors of hyperperfusion syndrome before and immediately after carotid artery stenting in single-photon emission computed tomography and transcranial color-coded real-time sonography studies. Neurosurgery 68:649–656
Kaku Y, Yoshimura S, Kokuzawa J (2004) Factors predictive of cerebral hyperperfusion after carotid angioplasty and stent placement. AJNR Am J Neuroradiol 25:1403–1408
Karapanayiotides T, Meuli R, Devuyst G, Piechowski-Jozwiak B, Dewarrat A, Ruchat P, Von Segesser L, Bogoussiavsky J (2005) Postcarotid endarterectomy hyperperfusion or reperfusion syndrome. Stroke 36:21–26
Kuroda H, Ogasawara K, Hirooka R, Kobayashi M, Fujiwara S, Chida K, Ishigaki D, Otawara Y, Ogawa A (2009) Prediction of cerebral hyperperfusion after carotid endarterectomy using middle cerebral artery signal intensity in preoperative single-slab 3-dimensional time-of-flight magnetic resonance angiography. Neurosurgery 64:1065–1072
Morrish W, Grahovac S, Douen A, Cheung G, Hu W, Farb R, Kalapos P, Wee R, Hudon M, Agbi C, Richard M (2000) Intracranial hemorrhage after stenting and angioplasty of extracranial carotid stenosis. AJNR Am J Neuroradiol 21:1911–1916
North American Symptomatic Carotid Endarterectomy Trial Collaborators (1991) Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med 325:445–453
Ogasawara K, Yukawa H, Kobayashi M, Mikami C, Konno H, Terasaki K, Inoue T, Ogawa A (2003) Prediction and monitoring of cerebral hyperperfusion after carotid endarterectomy using single-photon emission computerized tomography scanning. J Neurosurg 99:504–510
Ogasawara K, Inoue T, Kobayashi M, Endo H, Fukuda T, Ogawa A (2004) Pretreatment with the free radical scavenger edaravone prevents cerebral hyperperfusion after carotid endarterectomy. Neurosurgery 55:1060–1067
Ogasawara K, Sakai N, Kuroiwa T, Hosoda K, Ihara K, Toyoda K, Sakai C, Nagata I, Ogawa A, Japanese Society for Treatment at Neck in Cerebrovascular Disease Study Group (2007) Intracranial hemorrhage associated with cerebral hyperperfusion syndrome following carotid endarterectomy and carotid artery stenting: retrospective review of 4494 patients. J Neurosurg 107:1130–1136
Saito H, Ogasawara K, Suzuki T, Kuroda H, Kobayashi M, Yoshida K, Kubo Y, Ogawa A (2011) Adverse effects of intravenous acetazolamide administration for evaluation of cerebrovascular reactivity using brain perfusion single-photon emission computed tomography in patients with major cerebral artery steno-occlusive diseases. Neurol Med Chir 51:479–483
Schomer DF, Marks MP, Steinberg GK, Johnstone IM, Boothroyd DB, Ross MR, Pelc NJ, Enzmann DR (1994) The anatomy of the posterior communicating artery as a risk factor for ischemic cerebral infarction. N Engl J Med 330:1565–1570
Takeuchi R, Sengoku T, Matsumura K (2006) Usefulness of fully automated constant ROI analysis software for the brain: 3DSRT and FineSRT. Radiat Med 24:538–544
Torigai T, Mase M, Ohno T, Katano H, Nishikawa Y, Sakurai K, Sasaki S, Toyama J, Yamada K (2011) Usefulness of dual and fully automated measurements of cerebral blood flow during balloon occlusion test of the internal carotid artery. J Stroke Cerebrovasc Dis. doi:10.1016/j.jstrokecerebrovasdis.2011.07.015
van Mook WNKA, Rennenberg RJMW, Schurink GW, van Oostenbrugge RJ, Mess WH, Hofman PAM (2005) Cerebral hyperperfusion syndrome. Lancet Neurol 4:877–888
Yadav JS, Wholey MH, Kunts RE, Fayad P, Katzen BT, Mishkel GJ, Bajwa TK, Whitlow P, Strickman NE, Jaff MR, Popma JJ, Snead DB, Cutlip DE, Firth BG, Ouriel K, Stenting and angioplasty with protection in patients at high risk for endarterectomy investigators (2004) Protected carotid-artery stenting versus endarterectomy in high-risk patients. N Engl J Med 351:1493–1501
Acknowledgments
We thank Norimasa Takayanagi, Daiichi Radioisotope Laboratory for his technical support regarding 3DSRT and FineSRT, and Naoko Abe, Kojiro Hirose and all other staff for their invaluable assistance with SPECT.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comment
Here is an excellent communication with a novel idea and hypothesis from an experienced carotid intervention group in Nagoya. The goal was to identify preoperatively anatomical arterial characteristics, specifically predictably poor runoff (the P group), that could predict potential postoperative hyperemia and hyperpefusion syndromes.
As a preamble, I should say that it has not been our policy to perform SPECT scans in the routine workup of carotid surgery patents. Our rate of postoperative intracerebral hemorrhage is vanishing small (almost zero) for unclear reasons, so we have not developed a practice strategy to predict at-risk patients. Katano and colleagues, however, with this sentinel work, have convinced me that a clearer understanding of the risks and a rational evaluation strategy are worthwhile.
To summarize succinctly, patients with a good escape route (G) based on collateral anatomy, had low risk of hyperperfusion clinically or by SPECT. Three quarters of their patients were G type patients. Only two of these developed ipsilateral hyperpefusion post-treatemnt (Group I). By contrast, poor-runoff patients (P) were at high risk to revert to the I group and to have clinical symptoms as well.
So I am convinced that these authors can predict in their practice which patients are at risk for hyperemia based on anatomy (P) and thus can narrow down the focus of SPECT studies based on preoperative MRA data. The question is, what should we do with the information? To me, patients needing CEA or CAS for established indications will receive treatment whether they are “P” patients or not. Perhaps I would be more aggressive about ICU care and strict blood pressure control postoperatively based on “P” status, or SPECT data, but strict BP control and ICU observation are already my practice standard. This may account for the fact that despite my imperfect knowledge of this pathophysiology, we essentially never seen postoperative hyperperfusion syndrome or intracerebral hemorrhage, even though we sometimes have patients anticoagulated postoperatively, for prosthetic heart valves or bilateral symptomatic carotid disease.
I have learned from the Nagoya team here, and I better understand the physiology of collateral circulation as a result, and this in itself is worthwhile to the readership.
Christopher Miranda Loftus
Philadelphia, USA
Rights and permissions
About this article
Cite this article
Katano, H., Mase, M., Sakurai, K. et al. Revaluation of collateral pathways as escape routes from hyperemia/hyperperfusion following surgical treatment for carotid stenosis. Acta Neurochir 154, 2139–2149 (2012). https://doi.org/10.1007/s00701-012-1498-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-012-1498-7