Abstract
Background
Chronic subdural hematoma is characterized by blood in the subdural space that evokes an inflammatory reaction. Numerous factors potentially associated with recurrence of chronic subdural hematoma have been reported, but these factors have not been sufficiently investigated. In this study, we evaluated the independent risk factors of recurrence.
Methods
We analyzed data for 420 patients with chronic subdural hematoma treated by the standard surgical procedure for hematoma evacuation at our institution.
Results
Ninety-two (21.9 %) patients experienced at least one recurrence of chronic subdural hematoma during the study period. We did not identify any significant differences between chronic subdural hematoma recurrence and current antiplatelet therapy. The recurrence rate was 7 % for the homogeneous type, 21 % for the laminar type, 38 % for the separated type, and 0 % for the trabecular type. The rate of recurrence was significantly lower in the homogeneous and trabecular type than in the laminar and separated type. We performed a multivariate logistic regression analysis and found that postoperative midline shifting (OR, 3.6; 95 % CI, 1.618-7.885; p = 0.001), diabetes mellitus (OR, 2.2; 95 % CI, 1.196-3.856; p = 0.010), history of seizure (OR, 2.6; 95 % CI, 1.210-5.430; p = 0.014), width of hematoma (OR, 2.1; 95 % CI, 1.287-3.538; p = 0.003), and anticoagulant therapy (OR, 2.7; 95 % CI, 1.424-6.960; p = 0.005) were independent risk factors for the recurrence of chronic subdural hematoma.
Conclusions
We have shown that postoperative midline shifting (≥5 mm), diabetes mellitus, preoperative seizure, preoperative width of hematoma (≥20 mm), and anticoagulant therapy were independent predictors of the recurrence of chronic subdural hematoma. According to internal architecture of hematoma, the rate of recurrence was significantly lower in the homogeneous and the trabecular type than the laminar and separated type.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic subdural hematoma (CSDH) is a common type of intracranial hemorrhage in elderly patients [26]. Several different methods of surgery for CSDH have been suggested. The three most commonly used techniques are twist-drill craniostomy, burr-hole craniostomy, and craniotomy [26]. Burr-hole craniostomy with a closed drainage system is the most popular surgical technique worldwide [6, 14, 19]. The standard treatment for CSDH is surgical evacuation, which usually results in great improvement of neurological symptoms. Some authors suggest that CSDH is not a benign disease in the elderly due to its recurrence rate and perioperative mortality rate [8]. Numerous factors potentially associated with recurrence of CSDH have been reported, but the factors influencing their recurrence have not been sufficiently investigated [1, 2, 5, 9, 11–13, 18, 20, 25, 27]. CSDH has a significant recurrence rate, ranging from 9.2 to 26.5 % [17, 26].
The aim of this study was to define independent predictors for the recurrence of CSDH. We hypothesized that treatment with antiplatelet or anticoagulant drug, postoperative presence of midline shifting, and preoperative symptom with seizure influences the recurrence of CSDH. In this study, we reviewed a series of 420 consecutive surgical cases of CSDH treated at our institution, and retrospectively analyzed factors related to recurrence.
Materials and methods
We used our institutional medical data search system to identify all adult patients who underwent surgery for evacuation of CSDH between January 2006 and July 2011. The study protocol was approved by our Institutional Review Board. We retrospectively analyzed 420 patients with CSDH who were admitted to our Department of Neurosurgery. Recurrence was defined as the occurrence of symptoms and signs attributable to an ipsilateral hematoma seen on a brain computed tomographic (CT) scan within 3 months of the original drainage procedure. Reoperation was indicated if the original neurological deficit increased, recurred, or did not improve, or a new neurological deficit arose that needed further surgery (burr-hole craniostomy with drainage). All patients received treatment without dexamethasone. We treated bilateral hematoma as one case, and both sides received the same treatment.
Surgical procedures
All patients underwent a one burr-hole craniotomy with closed-system drainage (Type B ventricle drainage tube; Hanako Medical, Urawa, Japan) under local anesthesia with lidocaine.
If the international normalized ratio (INR) on admission was more than 1.5, vitamin K was administered intravenously to the patient.
Prothrombin time (PT) and INR were rechecked and vitamin K was repeated if the PT/INR was still more than 1.5. All patients were kept in the supine position, with the closed-system drainage maintained 50 cm below head level. Antiplatelet or anticoagulant agents were restarted after the surgical wound was healed, in the patients who had been taking these agents before surgery. Whether residual hematoma was seen on CT scans of the brain, all drainage catheters were removed after 72 h in both groups.
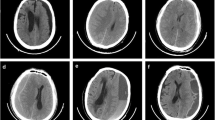
All hematomas were classified into four types according to internal architecture, which corresponded to possible stages in the natural history of CSDH: homogeneous, laminar, separated, and trabecular types [11]. The homogeneous type was defined as a hematoma that exhibited homogeneous density (low–high) (Fig. 1a) [11]. The laminar type was defined as a subtype of the homogeneous type that had a thin high-density layer along the inner membrane (Fig. 1b) [11]. The separated type was defined as a hematoma containing two components of different densities with a clear boundary lying between them; that is, a lower-density component located above a higher-density component (Fig. 1c) [11]. The trabecular type was defined as a hematoma with inhomogeneous contents and a high-density septum running between the inner and outer membrane on a low-density to isodense background (Fig. 1d) [11].
Computerized tomography scans demonstrating classification of CSDHs according to their internal architectures. a The homogeneous type was defined as a hematoma that exhibited homogeneous density (low–high). b The laminar type was defined as a subtype of the homogeneous type that had a thin high-density layer along the inner membrane. c The separated type was defined as a hematoma containing two components of different densities with a clear boundary lying between them; that is, a lower density component located above a higher density component. d The trabecular type was defined as a hematoma with inhomogeneous contents and a high-density septum running between the inner and outer membrane on a low-density to isodense background
Radiologic measures of the CSDH, including width of hematoma, midline shift, hematoma side, and hematoma type, were taken before and after the procedure. These measurements were determined at the maximum thickness at the level of lateral ventricles. Preoperative midline shift, brain atrophy, and maximum hematoma thickness were determined based on CT scans obtained immediately before surgery. According to preoperative CT scans, the hematoma collection was classified as hypodense, isodense, hyperdense, or mixed, on the basis of the density of hematoma relative to brain tissue [20].
Brain atrophy was classified into three stages: no or mild atrophy, definite atrophy, such as dilated sulci, and severe atrophy, such as widely dilated sulci and subdural space [13]. The presence of postoperative midline shifting was assessed based on CT scans obtained 6–7 days after surgery.
Statistical analysis
Variables considered in the statistical analysis included sex, age, hypertension, diabetes mellitus, heart disease, cerebrovascular disease, liver disease, atrial fibrillation, antiplatelet or anticoagulant therapy, seizure, hematoma density, internal architecture of hematoma, brain atrophy and multiplicity of hematoma cavity. Statistical analyses were performed using the Statistical Package for the Social Sciences for Microsoft Windows (Version 18.0; SPSS, Inc., Chicago, IL, USA). For comparisons of recurrence, we divided patients into two groups based on width of hematoma (≥20 mm and <20 mm), presence of preoperative midline shifting (≥10 mm and <10 mm), and presence of postoperative midline shifting (≥5 mm and <5 mm).
We performed a univariate analysis to assess the relationships between each variable and the recurrence of CSDH by applying the Mann–Whitney U test and the Chi-square test. The Mann–Whitney test was used for non-categorical variables (age, width of hematoma, and preoperative midline shifting). One-way ANOVA analysis was performed to determine the independent association (internal architecture, hematoma density, cause of CSDH, and brain atrophy) of the recurrence. The following variables were tested in multivariate logistic regression analysis: sex, hypertension, diabetes mellitus, antiplatelet or anticoagulant therapy, liver disease, history of seizure, multiplicity of hematoma cavity, width of hematoma, presence of preoperative midline shifting, and presence of postoperative midline shifting. Multivariate logistic regression analysis with a forward stepwise method was performed to determine the independent association of the recurrence. Adjusted odds ratios (OR) and their 95 % confidence intervals (CI) were calculated. Significance was set at a p value of less than 0.05.
Results
Table 1 shows the baseline characteristics of the patients. There were 334 men (70.3 %) and 86 women (29.7 %) in the study, ranging in age from 37 to 92 years (median age, 67.34 years). Male predominance was found in our operative database. Histories of hypertension were present in 126 patients (30 %), and a history of diabetic mellitus (DM) was present in 73 patients (17.4 %). Sixty-eight (16.2 %) patients presented with bilateral CSDH. The histories revealed past mild or moderate head trauma in 237 cases (56.4 %). Other risk factors included oral anticoagulation (warfarin) in 8.1 %, antiplatelet drugs (aspirin) in 27.9 %, and liver diseases (liver cirrhosis and hepatocellular carcinoma) in 10.7 %. One patient with severe coagulopathy developed postoperative epidural bleeding and underwent craniotomy. One patient developed intracerebral hemorrhage during surgery, and eventually suffered severe disability as the result of therapy. Infection occurred in eight patients (1.9 %). Seven patients (1.7 %) with superficial wound infection underwent superficial wound revision in addition to intravenous antibiotic therapy. In one case (0.1 %), deep infection developed at 1 week, which required craniotomy. The recurrence rate was 21.9 % (76.1 % in men and 23.9 % in women). The 420 CSDH patients were classified into four groups according to the density on CT scan: high (20 cases), iso- (178 cases), low (47 cases), and mixed (174 cases). There were no significant differences between hematoma density and recurrence of CSDH or between brain atrophy and recurrence of CSDH. The homogeneous type of CSDH was seen in 36.9 % of cases (155 lesions), the laminar type in 26.9 % (113 lesions), the separated type in 29.1 % (122 lesions), and the trabecular type in 7.1 % of cases (30 lesions). The recurrence rate in the homogeneous type was 7 %, 21 % in the laminar type, 38 % in the separated type, and 0 % in the trabecular type. The rate of recurrence was significantly lower in the homogeneous and the trabecular type than the laminar and separated type (Table 2). Ninety-two (21.9 %) patients experienced at least one recurrence of CSDH during the study period. Of these, 80 patients (87.0 %) underwent one reoperation, ten patients (10.9 %) had two reoperations, and two (2.1 %) had three reoperations. Although men had a higher recurrence rate, the difference was not significant. The age of the patients was not significantly related with recurrence (mean age with and without recurrence, 70.59 and 68.36 years, respectively). Patients with CSDH recurrence tended to have a history of DM, antiplatelet drugs, anticoagulant therapy, liver disease, presence of seizure, internal architecture of hematoma, width of hematoma, and postoperative midline shifting. Table 1 shows the results of the univariate analysis of the association between the recurrence of CSDH and each risk factor. We performed a multivariate logistic regression analysis and found that postoperative midline shifting (OR, 3.6; 95 % CI, 1.618–7.885; p = 0.001), diabetes mellitus (OR, 2.2; 95 % CI, 1.196–3.856; p = 0.010), history of seizure (OR, 2.6; 95 % CI, 1.210–5.430; p = 0.014), width of hematoma (OR, 2.1; 95 % CI, 1.287–3.538; p = 0.003), and anticoagulant therapy (OR, 2.7; 95 % CI, 1.424–6.960; p = 0.005) were independent risk factors for the recurrence of CSDH (Table 3). We did not detect significant differences between CSDH recurrence and current antiplatelet therapy.
Discussion
The pathophysiology of CSDH development appears to be complex, and the related literature is controversial. Numerous risk factors for recurrence of CSDH have been reported, including bleeding tendency, intracranial hypotension, advanced age, brain atrophy, bilateral CSDH, hematoma density, hematoma type, DM, postoperative posture, surgical techniques, postoperative subdural air accumulation, inflammatory cytokines, alcohol abuse, and multiplicity of hematoma cavity [1, 2, 5, 9, 11–13, 18, 20, 25, 27].
We found that the presence of postoperative midline shifting, DM, preoperative seizure, width of hematoma, and anticoagulant therapy are independent predictors for the recurrence of CSDH.
Width of hematoma and postoperative midline shifting
We found that width of hematoma and persistence of postoperative midline shifting are independent risk factors for recurrence of CSDH. We hypothesize that wider hematomas have increased tendency to recur because the subdural space is larger than a small lesion postoperatively. The intracranial pressure-volume function reflects the elastic properties of the brain parenchyma, the cerebrovascular bed, and the supporting dural structures within the rigid calvaria. Intracranial volume changes that result from the various mechanisms of spatial compensation are superimposed on the instantaneous pressure-volume function of brain elasticity. The elasticity function may be altered by disease such as hydrocephalus, advanced age, and brain atrophy [21, 22]. Persistence of the postoperative subdural cavity and residual air are risk factors for recurrence of CSDH [2, 13, 15]. Fukuhara and coworkers showed that advanced age, brain atrophy, large amount of hematoma, and prolonged compressed parenchyma influenced the brain elasticity [5]. Brains with high elastance tend to reexpand poorly, and poor reexpansion of the brain may lead to persistence of postoperative midline shifting [5]. Poor brain reexpansion is correlated with recurrence [25]. In the present study, the presence of postoperative midline shifting was assessed based on CT scans obtained 7 days after surgery. We hypothesize that prolonged symptom duration, advanced age, brain atrophy, width of hematoma, hematoma volume, and increased brain elastance may influence the persistence of postoperative midline shifting. A prolonged postoperative midline shifting may cause impaired adhesion between the inner and outer neomembranes and thus facilitate postoperative recurrence [10]. In a series reported by Stanisic and coworkers, the recurrence rate was significantly higher when the postoperative midline displacement was more than 5 mm compared to less displacement [23], and this is in agreement with our series. In the present study, postoperative midline shift ≥5 mm and/or preoperative hematoma width ≥20 mm are risk factors of recurrence. In these cases, we recommend maintenance of the drain for a longer period of time. Abouzari and coworkers showed that assuming a supine posture soon after burr-hole surgery was associated with a significantly decreased incidence of CSDH recurrence but not with a significant change in other position-related postsurgical complications [1]. Theoretically, bed rest and appropriate fluid administration may prevent hematoma recurrence by facilitation of brain re-expansion.
Diabetes mellitus (DM)
In this study, DM was an independent risk factor for recurrence of CSDH. Torihashi et al. suggested that DM may play a role in increasing the recurrence rate of CSDH, but were unable to determine the role DM plays in the development and recurrence of CSDH [25]. On the other hand, in a series reported by Yamamoto and coworkers the recurrence rate in patients without DM was higher than in those with DM, [27] which is not in agreement with our series. The blood of patients with DM has a high osmotic pressure and increased platelet aggregation, so DM may play a role in decreasing rebleeding in patients with CSDH [27]. On the other hand, exudation from the macrocapillaries in the outer membrane of CSDH plays an important role in the enlargement of chronic CSDH exudation [25]. We were surprised by the contradictory results related to the role in recurrence. This finding might be related to the relatively low frequency of recurrent cases, and consequently their small effect on the overall distribution of values within their cohorts. Further investigation is required to assess the influence of DM on recurrence of CSDH.
Preoperative history of seizure
In this study, preoperative history of seizure was an independent risk factor for recurrence of CSDH. In our institution, sodium valproate is the first-line antiepileptic drug administered to patients with history of seizure. Seizure is frequently associated with brain atrophy and repeated head trauma. Brain atrophy and repeated head trauma may play an impotent role in the recurrence of CSDH. Szupera and coworkers concluded that the valproate-stimulated synthesis of lipoxygenase eicosanoids and the inhibition of prostanoid production in the brain microvessels may contribute to the morphologic alterations of the capillaries in the brain [24]. In terms of alterations of the capillaries, valproate may play a role in increasing the recurrence of CSDH. Yamamoto and coworkers reported that an indirect effect of valproate by way of liver dysfunction may contribute to the recurrence of CSDH [27]. The direct effects of seizure (head trauma and brain atrophy) and of valproate (alteration of capillaries and liver dysfunction) may play a role in the recurrence of CSDH.
Anticoagulant therapy
Considering the increasing number of aged patients who use antiplatelet and anticoagulant medications, attention should be focused on the possible risks of these treatments. Theoretically, it is plausible that the use of antiplatelets and anticoagulants has a positive influence on the recurrence of CSDH. In the previous studies, there was no association between medication with antiplatelets or anticoagulants and recurrence of CSDH [7, 25, 27]. On the other hand, we concluded that anticoagulant therapy is an independent risk factor for the recurrence of CSDH in a multivariate regression model. This finding could reflect the fact that our institution is a tertiary referral hospital and there are a lot of patients who have been taking anticoagulant for a long time. One study reported that the role of antiplatelet and anticoagulant drugs failed to show a significant difference in recurrence of CSDH [25]. They concluded that the reason for this finding may be that the patients were not adequately anticoagulated, especially in the non-recurrence group [25]. However, in our study, 87.5 % of the patients (70 of 80) had a PT/INR of more than 1.5 in the non-recurrence group, and 85.7 % in the recurrence group (12 of 14). We concluded that in adequately anticoagulated patients, anticoagulant therapy is an independent risk factor for the recurrence of CSDH. However, we also failed to show a significant difference between antiplatelet and the recurrence of CSDH. In the past few years, the problem of “aspirin resistance” has been largely emphasized in the medical literature. Although the prevalence of aspirin resistance remains uncertain, previous studies have reported that it may affect between 5 % and 45 % of the population [3]. We hypothesize that aspirin resistance plays an important role in the conflicting results related to antiplatelet therapy and the recurrence of CSDH. A larger sample size and presence of aspirin resistance could validate the association between antiplatelet therapy and CSDH recurrence.
Internal architecture of hematoma
Nakaguchi and coworkers classified CSDH into the following four types based on the internal architecture and density of hematomas: homogeneous stage (stage 1), a separated or multilayered stage (stage 2), and a trabecular stage (stage 3) [11]. They suggested that CSDH originates as the homogeneous type and sometimes develops into the laminar type, and then matures as the separated type and is finally absorbed as the trabecular type [11]. Among the internal architectures of CSDH, the separated type had the highest recurrence rate [11, 16, 23]. In this study, the rate of recurrence was significantly lower in the homogeneous (p = 0.042) and the trabecular type (p =0.001) than in other types, and higher in the separated type than others (p = 0.001). The findings of recent experimental studies have revealed that blood in the subdural space evokes an inflammatory reaction [4]. They concluded that in the separated type, the concentrations of these cytokines were higher than those in the other groups, whereas in trabecular hematomas, the concentrations of cytokines were lower than those in the other groups [4]. We hypothesize that these findings are associated with the pathogenesis of CSDH. Therefore, when the inflammatory reaction is severe, such as with the separated type, the CSDH is more active with a higher recurrence rate and the levels of inflammatory markers are very high. On the other hand, in the very early (homogeneous type) or very late (trabecular type) stages, the CSDH is less active, with a lower recurrence rate and the levels of inflammatory markers are very low. In case of laminar or separated type on CT scan, the operation could be delayed unless severe symptoms are present.
Limitation
The present study was a retrospective study, and therefore may have sources of bias and variation. A prospective study with a larger number of cases is needed.
Conclusions
In patients with postoperative midline shifting (≥5 mm), DM, preoperative seizure, preoperative width of hematoma (≥20 mm), and anticoagulant therapy are independent predictors for the recurrence of CSDH. This information might be helpful for predicting the recurrence of CSDH. According to the internal architecture of hematoma, the rate of recurrence was significantly lower in the homogeneous and the trabecular type than the in the laminar and separated type.
Abbreviations
- CSDH:
-
Chronic subdural hematoma
- PT:
-
Prothrombin time
- INR:
-
International normalized ratio
- DM:
-
Diabetic mellitus
- OR:
-
Odd ratio
- CI:
-
Confidence interval
References
Abouzari M, Rashidi A, Rezaii J, Esfandiari K, Asadollahi M, Aleali H, Abdollahzadeh M (2007) The role of postoperative patient posture in the recurrence of traumatic chronic subdural hematoma after burr-hole surgery. Neurosurgery 61:794–797, discussion 797
Amirjamshidi A, Abouzari M, Eftekhar B, Rashidi A, Rezaii J, Esfandiari K, Shirani A, Asadollahi M, Aleali H (2007) Outcomes and recurrence rates in chronic subdural haematoma. Br J Neurosurg 21:272–275
Cattaneo M (2004) Aspirin and clopidogrel: efficacy, safety, and the issue of drug resistance. Arterioscler Thromb Vasc Biol 24:1980–1987
Frati A, Salvati M, Mainiero F, Ippoliti F, Rocchi G, Raco A, Caroli E, Cantore G, Delfini R (2004) Inflammation markers and risk factors for recurrence in 35 patients with a posttraumatic chronic subdural hematoma: a prospective study. J Neurosurg 100:24–32
Fukuhara T, Gotoh M, Asari S, Ohmoto T, Akioka T (1996) The relationship between brain surface elastance and brain reexpansion after evacuation of chronic subdural hematoma. Surg Neurol 45:570–574
Lind CR, Lind CJ, Mee EW (2003) Reduction in the number of repeated operations for the treatment of subacute and chronic subdural hematomas by placement of subdural drains. J Neurosurg 99:44–46
Lindvall P, Koskinen LO (2009) Anticoagulants and antiplatelet agents and the risk of development and recurrence of chronic subdural haematomas. J Clin Neurosci 16:1287–1290
Miranda LB, Braxton E, Hobbs J, Quigley MR (2011) Chronic subdural hematoma in the elderly: not a benign disease. J Neurosurg 114:72–76
Nagatani K, Takeuchi S, Sakakibara F, Otani N, Nawashiro H (2011) Radiological factors related to recurrence of chronic subdural hematoma. Acta Neurochir (Wien) 153:1713
Nakaguchi H, Tanishima T, Yoshimasu N (2000) Relationship between drainage catheter location and postoperative recurrence of chronic subdural hematoma after burr-hole irrigation and closed-system drainage. J Neurosurg 93:791–795
Nakaguchi H, Tanishima T, Yoshimasu N (2001) Factors in the natural history of chronic subdural hematomas that influence their postoperative recurrence. J Neurosurg 95:256–262
Nakajima H, Yasui T, Nishikawa M, Kishi H, Kan M (2002) The role of postoperative patient posture in the recurrence of chronic subdural hematoma: a prospective randomized trial. Surg Neurol 58:385–387, discussion 387
Oishi M, Toyama M, Tamatani S, Kitazawa T, Saito M (2001) Clinical factors of recurrent chronic subdural hematoma. Neurol Med Chir (Tokyo) 41:382–386
Ramachandran R, Hegde T (2007) Chronic subdural hematomas–causes of morbidity and mortality. Surg Neurol 67:367–372, discussion 372–363
Robinson RG (1984) Chronic subdural hematoma: surgical management in 133 patients. J Neurosurg 61:263–268
Sakakibara F, Tsuzuki N, Uozumi Y, Nawashiro H, Shima K (2011) Chronic subdural hematoma–recurrence and prevention. Brain Nerve 63:69–74
Santarius T, Hutchinson PJ (2004) Chronic subdural haematoma: time to rationalize treatment? Br J Neurosurg 18:328–332
Santarius T, Kirkpatrick PJ, Ganesan D, Chia HL, Jalloh I, Smielewski P, Richards HK, Marcus H, Parker RA, Price SJ, Kirollos RW, Pickard JD, Hutchinson PJ (2009) Use of drains versus no drains after burr-hole evacuation of chronic subdural haematoma: a randomised controlled trial. Lancet 374:1067–1073
Santarius T, Lawton R, Kirkpatrick PJ, Hutchinson PJ (2008) The management of primary chronic subdural haematoma: a questionnaire survey of practice in the United Kingdom and the Republic of Ireland. Br J Neurosurg 22:529–534
Scotti G, Terbrugge K, Melancon D, Belanger G (1977) Evaluation of the age of subdural hematomas by computerized tomography. J Neurosurg 47:311–315
Sklar FH, Beyer CW Jr, Clark WK (1980) Physiological features of the pressure-volume function of brain elasticity in man. J Neurosurg 53:166–172
Sklar FH, Diehl JT, Beyer CW Jr, Clark WK (1980) Brain elasticity changes with ventriculomegaly. J Neurosurg 53:173–179
Stanisic M, Lund-Johansen M, Mahesparan R (2005) Treatment of chronic subdural hematoma by burr-hole craniostomy in adults: influence of some factors on postoperative recurrence. Acta Neurochir (Wien) 147:1249–1256, discussion 1256–1247
Szupera Z, Mezei Z, Kis B, Gecse A, Vecsei L, Telegdy G (2000) The effects of valproate on the arachidonic acid metabolism of rat brain microvessels and of platelets. Eur J Pharmacol 387:205–210
Torihashi K, Sadamasa N, Yoshida K, Narumi O, Chin M, Yamagata S (2008) Independent predictors for recurrence of chronic subdural hematoma: a review of 343 consecutive surgical cases. Neurosurgery 63:1125–1129, discussion 1129
Weigel R, Schmiedek P, Krauss JK (2003) Outcome of contemporary surgery for chronic subdural haematoma: evidence based review. J Neurol Neurosurg Psychiatry 74:937–943
Yamamoto H, Hirashima Y, Hamada H, Hayashi N, Origasa H, Endo S (2003) Independent predictors of recurrence of chronic subdural hematoma: results of multivariate analysis performed using a logistic regression model. J Neurosurg 98:1217–1221
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comment
This is an important paper that deals with a common disease in the neurosurgical practice. The information on the recurrence rate and its prediction has a practical aspect. The independent recurrence rate on antiplatelet treatment is an important contribution to the decision-making on re-employment of antiplatelet treatment in patients after drainage of CSDH.
Moshe Hadani
Tel Hashomer, Israel
Rights and permissions
About this article
Cite this article
Chon, KH., Lee, JM., Koh, EJ. et al. Independent predictors for recurrence of chronic subdural hematoma. Acta Neurochir 154, 1541–1548 (2012). https://doi.org/10.1007/s00701-012-1399-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-012-1399-9