Abstract
Background
Recent advances in minimally invasive surgery have allowed extended transsphenoidal approaches to treat large and complex lesions beyond the sella turcica including basal meningiomas, but the inclusion criteria and limitations of this approach remain unclear.
Methods
Retrospective review of 19 consecutive patients (5 males and 14 females aged from 43 to 79 years) with tuberculum sellae meningioma with a maximum diameter of less than 30 mm surgically treated between December 2006 and August 2011 by a single surgeon. Operative outcomes and limitation-based indications were investigated.
Findings
Total removal was achieved in 15 cases including Simpson’s grade 1 in 2 cases (78.9%). All tumor remnants were located in the lateral portion of the internal carotid artery (ICA), as indicated by preoperative magnetic resonance (MR) imaging. Additional oblique imaging along the longitudinal axis of the C1-2 portion of the ICA revealed a paradoxical presence of tumor in between both sides of the ICA in some patients, even in the case with lateral extension over the ICA on coronal MR imaging. Total removal could be achieved in these patients, and after the introduction of additional preoperative oblique MR imaging, total removal was achieved in all patients. Visual outcomes of eyes showed improvement in 23, remained steady in 11, and showed deterioration in 4, and 89.5% eyes recovered to a good state. Deterioration was caused by injury of a small vein in one patient and previous disruption of the arachnoidal sheath in the remaining three. One patient suffered cerebrospinal fluid leakage and required re-operation. None of the patients developed endocrinological deficits or required prolonged hormonal supplementation.
Conclusions
The extended transsphenoidal approach has equivalent potential to transcranial surgery for tuberculum sellae meningiomas with a maximum diameter of less than 30 mm. The tumors with lateral extension over the ICA have fewer chances of total removal. ICA-oriented simulation and surgical planning are important.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The transsphenoidal approach has been used to treat soft tumors such as pituitary adenomas or intrasellar craniopharyngiomas. Recent advances in minimally invasive surgery have developed modified extended approaches to treat large and complex lesions beyond the sella turcica, and the entire ventral skull base, from the crista galli up to and through the odontoid, and laterally to the cavernous sinus [2, 3, 6, 9–13]. The deep and narrow operative field requires delicate and skillful procedures, and special reconstruction techniques for the skull base are essential to prevent cerebrospinal fluid (CSF) leakage, but this approach allows the surgeon to work along the axis of the tumor and permits removal of tumors with minimal displacement or distortion of surrounding structures [2, 3, 6, 9–13]. In particular, meningiomas located in the anterior skull base can be treated more easily because of the potential for early devascularization of the main feeding arteries [5], early decompression of the medial side of the optic nerve by unflooring of optic canal [14], and direct visualization of the lower plane of the optic chiasm [1, 2, 7, 19]. The indications for surgical treatment include a maximum diameter of less than 2 to 3 cm [1, 2, 7], no encasement of the major arteries [1, 5], no parasellar extension [1, 5], narrow dural attachment [5], and no calcification [5]. However, most of these indications strongly depend on the surgeon’s personal impression, except for the tumor diameter. The limitations of this approach in the deep and narrow operative field have not been widely evaluated [1].
We describe our series of tuberculum sellae meningiomas treated by the extended transsphenoidal approach in a single institute, and discuss the optimal indications and limitations.
Materials and methods
This retrospective review identified 5 males and 14 females aged from 43 to 79 years (mean 58.9 years) with tuberculum sellae meningiomas with a maximum diameter of less than 30 mm who were treated using the extended transsphenoidal approach from a series of 425 pituitary-based lesions at the Department of Neurosurgery, Kohnan Hospital, between December 2006 and August 2011; the operations were performed by a single surgeon (Y.O.). Two patients had been previously treated using the transcranial approach, one tumor was recurrent after total removal, and the other tumor required a second operation after partial removal. Tumors mainly located in the planum sphenoidale or diaphragma sellae were excluded from this study. Exposure was extended to the posterior ethmoidal sinus in addition to opening of the sellar floor through the sphenoidal sinus because of the tumor size in all patients. Minor modifications were adopted based on the anatomical characteristics of the tumors, including removal of the unilateral middle turbinate, and unflooring of the optic canal according to lateral extension or intrusion into the optic canal of the tumor. A surgical microscope and neuroendoscope were utilized as appropriate during the operation. Reconstruction of the skull base was performed with autologous fascia tightly sutured to the dural edge of the sellar floor, fortified with epidural attachment of muscle pieces, and the entire surface of the dural window was wrapped with a mucosal flap of the sphenoidal sinus. No type of marsupialization was performed. Postoperative prophylactic use of antibiotics was included for 7 days.
Axial, coronal, and sagittal T1-weighted magnetic resonance (MR) imaging, with and without contrast medium, and T2-weighted MR imaging (Signa Excite HD 3 T; General Electric Medical Systems, Milwaukee, Wis., USA) were performed preoperatively and within a few days after the operation in all patients, and preoperative oblique imaging along the longitudinal axis of C1-2 portion of internal carotid artery (ICA) was additionally performed in patients treated since September 2008. Maximal diameter was measured on the axial, coronal, and sagittal sections, and the tumor volume was calculated as A × B × C /2 [8, 15]. The removal rate was evaluated with Simpson’s grading [18]. Pituitary endocrinological status was evaluated, and the visual acuity and the visual field using the Humphrey field analyzer were also evaluated both preoperatively and 11 days after the operation. During follow-up at intervals of 6 months patients were investigated with the same sequence of MR imaging using a 3.0-T system. The mean follow-up period was 35.8 months (range 6–59 months).
The surgical specimens were immediately fixed for histological and immunohistochemical examinations with 10% buffered formalin, embedded in paraffin, and serial sections were cut to 3 μm thickness. Hematoxylin and eosin, and periodic acid-Schiff staining was performed in all cases. The avidin-biotin-peroxidase complex method was applied for immunohistochemical staining for epithelial membrane antigen (Dako Corp., Carpinteria, Calif., USA), keratin (Dako Corp.), vimentin (Dako Corp.), and Ki-67 (MIB-1, Dako Corp., 1:100).
The surgical policy was explained preoperatively to the patients, and the study design was approved by the Ethics Committee of Kohnan Hospital 2011.
Results
Postoperative histological examination revealed that nine tumors were the meningothelial type, five were the transitional type, three were the calcified psammomatous type, and two were atypical meningiomas with nuclear atypism.
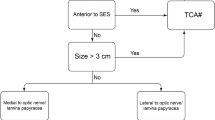
Simpson’s grade 1 removal was achieved in 2 cases and Simpson’s grade 2 removal in 13 cases. However, small tumor remnants persisted in the lateral portion of the ICA and resulted in Simpson’s grade 3 removal in four cases. The maximum diameter of the tumor ranged from 9 to 29 mm, but the maximum diameter was 20 mm or more in all Simpson’s grade 3 cases (Fig. 1, left). In contrast, the tumor volume ranged from 0.28 to 9.25 ml, whereas the tumor volume was 2.38, 1.58, 1.92, and 9.25 ml in the Simpson’s grade 3 cases (Fig. 1, right). All tumor remnants were located in the lateral portion of the ICA. Oblique imaging along the longitudinal axis of the C1-2 portion of the ICA revealed paradoxical presence of tumor in between both sides of the ICA in some patients, even in the tumor with lateral extension over the ICA, as seen on the coronal MR image. Gross total removal could be achieved in these cases (Fig. 2). The tumor with lateral extension over the ICA on both coronal and oblique MR imaging could not be removed and resulted in subtotal removal (Fig. 3). All cases of non-total removal were included in the first ten patients treated (cases 1–10 in Table 1), and gross total removal was achieved in all patients after the introduction of additional oblique MR imaging (cases 11–19 in Table 1).
Fourteen of 19 patients achieved postoperative improvement of visual acuity; it remained steady in 3 and deteriorated in 2 (Fig. 4, left). Evaluation of each eye showed improvement in 23 eyes; 11 remained steady and 4 deteriorated (Fig. 4, right). The most common outcome was improvement in one eye and remaining steady in the other. Deterioration of visual acuity was caused by injury of a vein with 150-μm diameter in one case, previous disruption of the arachnoidal sheath in the exit of the optic canal in two cases, and direct and tight adhesion of the tumor to the lower plane of the optic chiasm in one case.
Postoperative CSF leakage was seen in case 1 with widely dissected dural attachment, and this disappeared at re-operation. Fibrin glue was used only in this case, and the others were reconstructed with autologous tissue only. No patients had preoperative endocrinological deficiency, and none of the patients required hormonal supplementation within 3 postoperative days.
During the follow-up period, one patient experienced tumor recurrence (case 1) at 59 months after the operation and required Gammma Knife surgery. No other patients experienced tumor progression, including four patients with Simpson’s grade 3 removal, and they were observed serially.
There was transient nasal discomfort in some patients, but all of the complaints disappeared without any special treatment in 3 months. No other complication related to the operation was seen throughout the hospitalization period.
Discussion
This study found no significant relationship between tumor volume and removal rate in tumors with a maximum diameter of less than 3 cm. Total removal of significantly calcified tumors was also possible (Fig. 5). We also found that presumptive encasement of the ICA and/or A1 based on MR imaging could be re-evaluated as absence of encasement by changing the scanning angles. ICA-oriented surgical simulation could be helpful, as shown in cases 11–19, indicating the importance of additional oblique scanning or reconstruction of already scanned slices. However, this suggests limited advantages for the transsphenoidal approach over the transcranial approach, even for small tumors such as clinoidal meningioma, which tends to extend laterally over the ICA.
Postoperative visual recovery generally depends strongly on the tumor volume and affected duration of the optic pathway [5, 14]. The transcranial approach results in 25–80% postoperative visual improvement (mean 56%), 30% unchanged, and 3–30% deterioration (mean 13%) [5]. The transsphenoidal approach tends to provide a higher rate of improvement, but there is a great difference in surgical experience between the two approaches, and larger tumor volume can be treated by the transcranial approach [4, 5, 14]. Three of four patients with visual deterioration in this series had more or less disrupted arachnoidal sheaths of the optic nerve and/or chiasm. Therefore, the arachnoidal plane should be essentially preserved [7, 19], and aggressive dissection should be avoided if the arachnoidal plane is already disrupted. We must keep in mind that only a few tumors were malignant variants with high growth potential among skull base meningiomas [16].
Endocrinological disturbance has been reported as a major complication, but our series included no cases of tight adhesion to the anterior lobe or pituitary stalk, and no patient suffered hormonal disturbance. Since the introduction of the extended transsphenoidal approach at our institute in March 2006, CSF leakage has occurred in 1 of 92 surgeries, which was also included in this study. We expect further experience to lower the incidence of CSF leakage still more.
Finally, we emphasize the minor but important advantage of the transsphenoidal approach of being less invasiveness for elderly and/or flow-compromised patients [1]. We previously reported a case of successful treatment of basal meningioma associated with moyamoya syndrome, which is included in this series (case 14) [17].
Instead of a small series of experiences, this report discusses the tumor progression rate after using the extended transsphenoidal approach for the first time. Successive and long-term follow-up data are needed.
Conclusion
This series of patients with tuberculum sellae meningiomas with a maximum diameter of less than 3 cm treated using the extended transsphenoidal approach shows that this approach has equivalent potential to transcranial surgery in experienced hands. However, tumors with lateral extension over the ICA have fewer chances of total removal, and ICA-oriented simulation and surgical planning are important.
References
Bowers CA, Altay T, Couldwell WT (2011) Surgical decision-making strategies in tuberculum sellae meningioma resection. Neurosurg Focus 30(5):E1
Couldwell WT, Weiss MH, Rabb C, Liu JK, Apfelbaum RI, Fukushima T (2004) Variations on the standard transsphenoidal approach to the sellar region, with emphasis on the extended approaches and parasellar approaches: Surgical experience in 105 cases. Neurosurgery 55:539–550
de Divitiis E, Cappabianca P, Cavallo LM (2002) Endoscopic transsphenoidal approach: adaptability of the procedure to different sellar lesions. Neurosurgery 51:699–707
de Divitiis E, Cavallo LM, Esposito F, Stella L, Messina A (2007) Extended endoscopic transsphenoidal approach for tuberculum sellae meningiomas. Neurosurgery 61(5 Suppl 2):229–238
de Divitiis E, Esposito F, Cappabianca P, Cavallo LM, de Divitiis O (2008) Tuberculum sellae meningiomas: high route or low route? A series of 51 consecutive cases. Neurosurgery 62:556–563
Dusick JR, Esposito F, Kelly DF, Cohan P, DeSalles A, Becker DP, Martin NA (2005) Extended direct endonasal transsphenoidal approach for nonadenomatous suprasellar tumors. J Neurosurg 102:832–841
Frank G, Pasquini E (2010) Tuberculum sellae meningioma: the extended transsphenoidal approach–for the virtuoso only? World Neurosurg 73:625–626
Huttner HB, Steiner T, Hartmann M, Kohrmann M, Juettler E, Mueller S, Wikner J, Metdig-Lamade U, Schramm P, Schwab S, Schellinger PD (2006) Comparison of ABC/2 estimation technique to computer-assisted planimetric analysis in warfarin-related intracerebral parenchymal hemorrhage. Stroke 37:404–408
Kaptain GJ, Vincent DA, Sheehan JP, Laws ER Jr (2001) Transsphenoidal approaches for the extracapsular resection of midline suprasellar and anterior cranial base lesions. Neurosurgery 49:94–101
Kassam A, Snyderman CH, Mintz A, Gardner P, Carrau RL (2005) Expanded endonasal approach: the rostrocaudal axis. Part I. Crista galli to the sella turcica. Neurosurg Focus 19(1):E3
Kassam A, Snyderman CH, Mintz A, Gardner P, Carrau RL (2005) Expanded endonasal approach: the rostrocaudal axis. Part II. Posterior clinoids to the foramen magnum. Neurosurg Focus 19(1):E4
Kassam AB, Gardner P, Snyderman C, Mintz A, Carrau R (2005) Expanded endonasal approach: fully endoscopic, completely transnasal approach to the middle third of the clivus, petrous bone, middle cranial fossa, and infratemporal fossa. Neurosurg Focus 19(1):E6
Kassam AB, Snyderman C, Gardner P, Carrau R, Spiro R (2005) The expanded endonasal approach: a fully endoscopic transnasal approach and resection of the odontoid process: technical case report. Neurosurgery 57(1 Suppl):E213
Kitano M, Taneda M, Nakao Y (2007) Postoperative improvement in visual function in patients with tuberculum sellae meningiomas: results of the extended transsphenoidal and transcranial approaches. J Neurosurg 107:337–346
Kothari RU, Brott T, Broderick J, Barsan WG, Sauerbeck LR, Zuccarello M, Khoury J (1996) The ABCs of measuring intracerebral hemorrhage volumes. Stroke 27:1304–1305
McGovern SL, Aldape KD, Munsell MF, Mahajan A, DeMonte F, Woo SY (2010) A comparison of World Health Organization tumor grades at recurrence in patients with non-skull base and skull base meningiomas. J Neurosurg 112:925–933
Ogawa Y, Tominaga T (2011) Moyamoya syndrome associated with basal meningioma successfully treated by the modified transsphenoidal approach: Case report. Skull Base Reports
Simpson D (1957) The recurrence of intracranial meningiomas after surgical treatment. J Neurol Neurosurg Psychiatry 20:22–39
Wang Q, Lu XJ, Ji WY, Yan ZC, Xu J, Ding YS, Zhang J (2010) Visual outcome after extended endoscopic endonasal transsphenoidal surgery for tuberculum sellae meningiomas. World Neurosurg 73:694–700
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ogawa, Y., Tominaga, T. Extended transsphenoidal approach for tuberculum sellae meningioma—What are the optimum and critical indications?. Acta Neurochir 154, 621–626 (2012). https://doi.org/10.1007/s00701-011-1266-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-011-1266-0