Abstract
Background
This article discusses data from 3 randomized phase 3 trials, supporting a role for surgery in glioblastoma.
Methods
Data were reviewed by extent of resection during primary surgery from the ALA-Glioma Study (fluorescence-guided versus conventional resection), the BCNU wafer study (BCNU wafer versus placebo), and the EORTC Study 26981–22981 (radiotherapy versus chemoradiotherapy with temozolomide).
Results
For glioblastoma patients in the ALA study, median survival was 16.7 and 11.8 months for complete versus partial resection, respectively (P < 0.0001). Survival effects were maintained after correction for differences in age and tumor location. For glioblastoma patients who received ≥90% resection in the BCNU wafer study, median survival increased for BCNU wafer versus placebo (14.5 versus 12.4 months, respectively; P = 0.02), but no survival increase was found for <90% resection (11.7 versus 10.6 months, respectively; P = 0.98). In the EORTC study, absolute median gain in survival with chemoradiotherapy versus radiotherapy was greatest for complete resections (+4.1 months; P = 0.0001), compared with partial resections (+1.8 months; P = 0.0001), or biopsies (+1.5 months; P = 0.088), suggesting surgery enhanced adjuvant treatment.
Conclusion
Complete resection appears to improve survival and may increase the efficacy of adjunct/adjuvant therapies. If safely achievable, complete resection should be the surgical goal for glioblastoma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cytoreductive surgery for glioblastomas (GBM) has been performed for decades, initially with radical procedures including lobectomies and even hemispherectomies. While it has been acknowledged that surgery cannot cure GBM because of the diffuse nature of the disease, it has often been assumed that surgery provides some survival benefit. Surgery provides a rapid reduction of tumor bulk and mass effect, leading to symptom palliation, and provides tissue for histopathological diagnosis [22] Thus, the neurosurgery community has invested great efforts to improve the safety of maximal tumor resection, including costly intraoperative imaging modalities. Nevertheless, the value of extensive surgery for improving survival has repeatedly been challenged, with emphasis on risks of craniotomy and cost [16, 24–26, 30, 48].
There is no Class I evidence from well designed and adequately powered trials that conclusively demonstrates a survival benefit with surgery. In fact, some studies suggest that if there is a survival benefit it is modest and may be limited to select patients [2, 24, 35, 45]. The perception of resection as beneficial is largely based on a collection of data from retrospective and observational studies that assessed survival or disease progression by extent of resection [5, 6, 10, 19, 20, 27, 29, 37, 49]. It has been debated whether the cohorts analyzed in these studies were adequately balanced by known prognostic factors such as age and Karnofsky Performance Status (KPS) [16]. In fact, studies in which the distribution of such factors was assessed demonstrated that younger patients or patients with high KPS scores received more extensive resections [1, 9, 41]. Moreover, small and superficially located tumors are more likely to undergo extensive resections, and such tumors may intrinsically have a better prognosis [18, 37, 41]. Such biased data may influence the postulated effect of resection and thus confound conclusions regarding the prognostic role of resection as estimated by multivariate analysis.
Recently, 3 prospective, randomized phase 3 studies were conducted that employed surgical resection in addition to investigational agents in patients with newly diagnosed malignant glioma. The first of these studies investigated the support of resection by intraoperative fluorescent guidance with 5-aminolevulinic acid (5-ALA, Gliolan®, Medac GmbH, Hamburg, Germany) in malignant glioma patients [40]. The second study investigated the efficacy and safety of intracavitary chemotherapy with carmustine (BCNU) wafers (Gliadel® Wafer, Eisai Corporation North America, Woodcliff Lake, NJ) in malignant glioma patients [46], and the third study investigated the efficacy and safety of concomitant radiochemotherapy with temozolomide followed by sequential temozolomide (Temodar®, Schering Corp., Kenilworth, NJ) in glioblastoma patients [42]. The results of each of these studies led to the approval of the investigational agent for the treatment of patients with malignant gliomas (ALA study, BCNU wafer study) and glioblastomas (temozolomide study). Within all three trials, extent of resection and other prognostic factors were collected prospectively. Post-hoc analyses of these data provide similar results with respect to the impact of extent of resection on survival and its potential influence on the efficacy of adjunct/adjuvant therapies.
Influence of resection on survival
5-ALA fluorescence-guided resection and radiotherapy
In the 5-ALA study, patients with resectable, newly diagnosed malignant glioma were randomized to receive 5-ALA fluorescence-guided resection (n = 139) or conventional non-enhanced microsurgery (n = 131) [40]. Resection was followed by a standard course of fractionated radiotherapy (60 Gy). The primary study endpoints were the rate of complete resection—removal of all contrast-enhancing tumor on early (within 72 hours of surgery) magnetic resonance imaging (MRI)—and the 6-month progression-free survival (PFS) rate. The complete resection rate was 65% and 36% in the 5-ALA and conventional surgery groups, respectively. In logistic-regression models, the use of 5-ALA had the most important effect on the probability of complete resection (odds ratio = 3.41; 95% CI, 2.03–5.71; P < 0.0001), followed by age and tumor location, while performance status did not reach statistical significance. The 29% difference in the frequency of complete resections translated into a significantly improved 6-month PFS rate (41.0% versus 21.0%, respectively; P = 0.0003). Analysis of overall survival also favored surgery with 5-ALA over conventional surgery (15.2 versus 13.5 months; hazard ratio [HR] = 0.82; 95% CI, 0.62–1.07; P = 0.1). Although this difference was not statistically significant, it should be realized that the study was not powered to show differences in overall survival. A significant survival difference was observed in the whole study cohort between patients who received complete resection compared with partial resection: 17.9 months (95% CI, 14.3–19.4) versus 12.9 months (95% CI, 10.6–14.0), respectively (P < 0.0001).
To investigate the impact of resection in glioblastomas only, a post-hoc analysis of these data restratified the per-protocol cohort of patients by extent of resection, ie, complete versus partial, excluding all patients with grade III gliomas [41]. The resulting groups were balanced regarding a number of possible prognostic factors (eg, neurological function, preoperative tumor characteristics, additional treatments received), with the exception of age and tumor location (eloquent versus noneloquent), the latter of which was assessed by surgeons. The survival benefit associated with complete versus partial resection in the intent-to-treat (ITT) population was maintained in the per-protocol cohort (median survival, 16.7 versus 11.8 months, respectively; P < 0.0001), and the 2-year survival rate was significantly greater for complete versus partial resections (26.2% [95% CI, 18.5–34.6%] versus 7.0% [95% CI, 3.8–13.1%]). The survival advantage with complete resection was maintained when patients were substratified by age <60 years versus >60 years (Table 1), and the differences in age distributions in the substrata were no longer detectable. Median age was 52 and 54 years for complete and partial resection, respectively, in the subgroup <60 years of age, and 65 and 66 years, respectively, in the subgroup >60 years of age. The survival advantage also was maintained after substratification of patients by tumor location. Thus, both age and tumor location could be eliminated as confounding factors. In multivariate analysis, resection status had the strongest prognostic effect (HR for residual tumor = 1.752; 95% CI, 1.258–2.438; P = 0.0009).
In a subsequent analysis that evaluated survival by the Radiation Therapy Oncology Group recursive partitioning analysis (RPA), the survival advantage associated with complete versus partial resection was maintained in RPA class IV and V subgroups [33]. Complete resection was also favored for the RPA class III subgroup, but this did not reach statistical significance, likely because of the small sample size.
Surgery, BCNU wafers, and radiotherapy
In a randomized, double-blind, placebo-controlled, phase 3 trial by Westphal et al [46], 240 patients with newly diagnosed malignant glioma were randomized to receive resection with BCNU wafer or placebo wafer implantation (120 patients in each arm). Following resection and wafer implantation, patients received a standard course of fractionated radiotherapy (total dose, 55–60 Gy). Implantation of BCNU wafer resulted in significantly longer survival compared with placebo in the ITT population (13.9 versus 11.6 months; HR = 0.71, 95% CI, 0.52–0.96; P = 0.03) [25] with a tail of stable long-term survivors. The 2-year survival rate was 15.8% for BCNU wafer versus 8.3% for placebo (not significant), and the 3-year survival rate was 9.2% versus 1.7% (P = 0.01), respectively [47]. In the subgroup with GBM, there was a trend of improved survival for BCNU wafer versus placebo, although the difference was not statistically significant (13.5 versus 11.4 months; HR = 0.76, 95% CI, 0.55–1.05; P = 0.10) [46].
During the BCNU study, data on extent of resection were captured by the investigators prospectively at participating institutions from the reports made by the local neuroradiologists on radiographs mandated to be taken 24 to 48 hours postoperatively. The preferred radiographic method was tumor volume on MRI, but tumor area and CT scans were also used. There was no centralized radiographic review. Complete resection was defined as removal of ≥ 90% of tumor tissue as measured on postoperative radiographs compared with preoperative scans. When these data were analyzed, 48% and 44% of patients in the BCNU wafer and placebo groups, respectively, received complete resections in the ITT population as documented in case report forms (Table 2). In the complete resection subgroup, median survival was significantly greater for BCNU wafer than for placebo (14.8 versus 12.6 months; P = 0.01). In the partial resection subgroup, median survival was 12.1 and 11.2 months, respectively (P = 0.39).
For patients with GBM, the results were very similar, with a median survival of 14.5 months for BCNU wafer versus 12.4 months for placebo (P = 0.02) in the complete resection subgroup, and 11.7 and 10.6 months, respectively (P = 0.98), in the partial resection subgroup.
These data suggest that survival improved in patients receiving complete resection compared with partial resection in both the BCNU and placebo wafer arms [25]. The survival advantage of BCNU wafers compared with placebo was significant in the complete resection subgroup but did not reach statistical significance in the partial resection subgroup. For the ITT population, the absolute median gain in survival time with BCNU wafer versus placebo was +2.2 months for complete resection and +0.9 months for partial resection.
Concomitant radiochemotherapy followed by adjuvant temozolomide
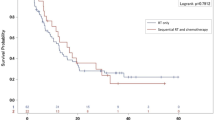
The EORTC-NCIC trial (EORTC 26981–22981; NCIC CE.3) study was a randomized, multicenter trial in 573 patients with newly diagnosed malignant glioma [42]. Patients were randomized to receive radiotherapy alone (2 Gy/day for 5 days a week over a course of 6 weeks) or radiotherapy with continuous daily temozolomide (75 mg/m2/day, 7 days a week) followed by 6 cycles of temozolomide (150–200 mg/m2 for 5 days during each 28-day cycle). In the primary report, Stupp et al. observed a significant survival benefit with temozolomide [42]. Median survival was 14.6 months in the radiochemotherapy group versus 12.1 months in the radiotherapy only group (HR = 0.63; 95% CI, 0.52–0.75; P < 0.001), and the 2-year survival rate was 26.5% (95% CI, 21.2–31.7) versus 10.4% (95% CI, 6.8–14.1), respectively. Long-term follow-up demonstrated that the survival benefit with temozolomide was maintained at 3 years (16.7% versus 4.3%, respectively; P < 0.0001) z31].
During this study, extent of resection was reported per surgeon assessment on clinical and/or radiological grounds. The study did not mandate postoperative imaging (although it was recommended) nor centrally review imaging. Ninety-three patients (16%) had a diagnostic biopsy only, 254 patients (44%) had partial resections, and 226 patients (39%) had complete resections. A Cox analysis adjusting for age and performance status demonstrated that the treatment effect remained significant in the resected group (HR = 0.63; 95% CI, 0.51–0.76; P < 0.0001) but not in the biopsied group (HR = 0.69; 95% CI, 0.45–1.05; P = 0.084).
The clinical impact of resection was examined further in a post-hoc analysis of survival by extent of resection [43]. While this study was not designed to assess survival by extent of resection and assessment of the surgeon is less accurate than radiographic assessment [1], the data indicate that the more complete the resection, the more prolonged the survival (Table 3). Absolute median gain in survival time with radiochemotherapy versus radiotherapy alone was greatest in patients with complete resections (+4.1 months) compared with those with incomplete resections (+1.8 months) or biopsies (+1.5 months), although this increase did not meet statistical significance in tests for interaction (test for heterogeneity, P = 0.24). The Kaplan-Meier survival data corresponded to a risk reduction for radiochemotherapy versus radiotherapy alone of 43% in patients who received complete resection (P = 0.0001), 35% for partial resection (P = 0.0001), and a nonsignificant decrease of 31% for biopsy (P = 0.088). Adjuvant temozolomide appeared to have the greatest survival impact in patients who received complete resection, suggesting that the effectiveness of temozolomide may be related to the extent of resection.
Discussion
The controversy surrounding the value of surgery in malignant glioma has not been investigated in well-controlled and adequately powered prospective trials and likely never will be. Historically, the relationship between extent of resection and survival has been primarily described in retrospective, observational studies [1, 4, 27, 39, 44]. Because of their retrospective and uncontrolled design, these studies have been criticized for potentially confounded results. Biased distribution of patients may have caused differences between study groups for known prognostic factors, such as age, tumor location, and KPS [8, 34, 38]. For example, patients recommended for aggressive surgical resection are often younger than those recommended for biopsy [29]. Biased distribution of prognostic factors may have concurrently influenced survival and extent of resection [16]. Also, there was no centralized review for neuropathology in these studies [36].
To our knowledge, there is only 1 randomized, prospective study that examined the effectiveness of resection in malignant glioma [45]. In this small study, 30 patients over the age of 65 years were randomized to receive biopsy or resection. Histological diagnosis confirmed malignant glioma in 13 biopsy patients and 10 resection patients. All patients received radiotherapy. There was a significant but modest improvement in median survival for resection versus biopsy (171 days versus 85 days, respectively; P = 0.035), but no significant difference in time to deterioration (105 days versus 72 days, respectively; P = 0.057). When adjusted for tumor grade, resection was more favorable than biopsy for both survival (HR = 2.621; 95% CI, 1.035–6.641; P = 0.0422) and time to deterioration (HR = 2.757; 95% CI, 1.004–7.568; P = 0.0491). Unfortunately, this study was not adequately powered to draw definitive conclusions (the trial is subject to chance findings) and excluded younger patients who have been shown to benefit from resection more than older patients [29].
There is a substantial collection of prospective and retrospective data supporting resection over biopsy in malignant glioma (summarized in Laws et al.) [29]. Unfortunately, data on extent of resection were not captured in the majority of studies for about 40 years, as most centers did not have the infrastructure to accurately assess extent of resection. When it became included in phase 3 trials, resection was frequently used for stratification, but these trials were not specifically designed or powered to examine the relationship between survival and extent of resection, which was often based on local neuroradiology evaluations without uniform protocols. While almost all meaningful glioma trials of the last decade have had centralized neuropathological evaluation [36] centralized radiographic review of resection has been the exception, although it has been performed in more recent trials, including the 5-ALA trial [40]. Despite this limitation, the availability and quality of resection data have improved in recent studies to a standard that allows an attempt at correlative analyses.
The 3 clinical trials reviewed here further support the use of resection in glioblastoma and maximal tumor resection [40–43, 46]. These 3 studies were well-controlled, prospective, randomized trials that assessed various treatment options for malignant glioma, and each study prospectively collected resection data. Most of the patients in the 5-ALA and BCNU wafer trials were glioblastoma patients, as were all patients in the temozomide study. Thus, these studies provide evidence on the relationship between resection and survival and between resection and the efficacy of adjuvant therapies. More extensive resection was associated with improved outcome, and in the temozolomide and BCNU wafer studies the survival benefit of the study treatment appeared to be most favorable in patients who received extensive resection.
It is important to recognize caveats to the results reported here. Because of the patient selection process, there are limitations to the generalizability of the results as the cohorts of patients from these 3 studies represent a more narrow population than that observed in the community setting. These studies excluded patients with low KPS. Resection was mandatory in the 5-ALA and BCNU wafer studies with a goal of maximal tumor resection in both. Patients with tumors deemed only partially resectable were excluded in the 5-ALA study.
Furthermore, the 3 studies were not designed or powered to assess the relationship between resection and survival. The data were post-hoc subgroup analyses of glioblastoma patients and are subject to confounding influences. Resection data were centrally reviewed only in the 5-ALA study. In the temozolomide study, extent of resection was captured by the surgeon and was based on clinical or radiographic assessment [1]. In the BCNU wafer study, radiographic assessment of resection was not centralized. It is unclear whether the surgical subgroups were balanced with respect to known and unknown prognostics factors. In the temozolomide and BCNU studies, the surgical subgroups are likely to differ as surgical decisions are affected by tumor characteristics (eg, size and location) and the status of the patient (eg, age). It will be important to determine whether the relationship between complete resection and temozolomide or BCNU wafer is maintained with more rigorous statistical analyses that adjust for other known prognostic factors. A smaller randomized phase 2 study in newly diagnosed GBM patients (N = 110) with a similar protocol as the EORTC-NCIC trial did not find an association between the extent of surgery and survival [3]. However, only 17% of patients received complete resection and the small sample size limits the power of subgroup analyses. Since the number of grade III gliomas in the 5-ALA and BCNU wafer studies was small (no grade III tumors were included in the temozolomide study), our conclusions cannot be conferred to grade III glioma patients based on the present data.
Despite the limitations of these analyses, the data reviewed here support the value of maximal resection in the multimodality treatment of glioblastoma. The concept that resection may also enhance the efficacy of adjuvant therapies is novel and expands the benefits of surgical intervention beyond immediate relief of symptoms due to mass effect and a rapid and logarithmic kill of tumor cells. The question remains about the underlying mechanisms. One mechanism may be the beneficial effect on hypoxia-related phenomena. On MRI, a central core of contrast-enhancing tumor with necrosis is surrounded by a wide margin of invading cells. This enhancing region is known to be hypoxic. Hypoxia influences the behavior of tumor cells by activating genes involved in the adaptation to hypoxic stress (eg, angiogenesis), representing an important indicator of cancer prognosis [7, 11, 21, 50]. Hypoxia is associated with aggressive growth, metastasis, and poor response to treatment [23, 28]. Central GBM cells appear to proliferate more readily than they invade [14] which may affect short-term prognosis. The marginal region of the tumor has more angiogenesis [17] and tumor cells in this region may be less proliferative, more migratory, and more resistant to apoptosis, which likely contributes to treatment resistance [14].
Hypotheses also suggest that interstitial fluid pressure (IFP) may affect the penetration and residence time of chemotherapy agents. Increased IFP in glioma tumors with increased permeability may produce a pressure gradient that distributes chemotherapy agents into necrotic areas or into surrounding brain tissue where it is absorbed and cleared, thus limiting the residence time of the cytotoxic agents in the marginal region [32]. Following resection, there is an initial increase in IFP in the immediate postoperative period because of cerebral edema. Once edema is resolved, IFP decreases and the direction of fluid flow reverses toward the resection cavity [14]. With intracavitary chemotherapy, the increase in IFP in the immediate postoperative period because of edema, particularly with BCNU wafer, [15] may improve the limited penetration of antitumor agents into the infiltrating zone [12, 13]. Systemic chemotherapy, on the other hand, is generally delivered a few weeks after resection when edema has been resolved and there is a decrease in IFP, particularly in the marginal zone, and permeability is limited from cytokine production of tumor cells within that zone. Thus, decreasing IFP may prolong the drug residence time in the marginal zone [32]. Regardless of the potential mechanism for improving the effectiveness of adjuvant treatments with complete resection, the problem remains that undetectable infiltrative tumor stem-like cells or tumor repopulating cells persist and eventually develop into detectable recurrence.
Conclusion
Treatment of patients with malignant glioma demands multimodal approaches that deliver highly effective anti-tumor agents. Rapid, local tumor control afforded by surgery sets the stage for other treatments to become more efficacious. The collection of clinical data currently available supports the use of surgery for the management of glioblastoma. Surgery improves survival and may enhance the efficacy of adjunct/adjuvant therapies. The 3 prospective, randomized trials reported here support this view. Future treatment studies should continue to collect resection data prospectively, preferably by centralized radiographic review, so that results can be analyzed by the extent of resection to determine the relationship between resection, other treatment modalities, and survival.
References
Albert FK, Forsting M, Sartor K, Adams HP, Kunze S (1994) Early postoperative magnetic resonance imaging after resection of malignant glioma: objective evaluation of residual tumor and its influence on regrowth and prognosis. Neurosurgery 34:45–60
Ashby LS, Ryken TC (2006) Management of malignant glioma: steady progress with multimodal approaches. Neurosurg Focus 20:E3
Athanassiou H, Synodinou M, Maragoudakis E, Paraskevaidis M, Verigos C, Misailidou D, Antonadou D, Saris G, Beroukas K, Karageorgis P (2005) Randomized phase II study of temozolomide and radiotherapy compared with radiotherapy alone in newly diagnosed glioblastoma multiforme. J Clin Oncol 23:2372–2377
Barker FG 2nd, Prados MD, Chang SM, Gutin PH, Lamborn KR, Larson DA, Malec MK, McDermott MW, Sneed PK, Wara WM, Wilson CB (1996) Radiation response and survival time in patients with glioblastoma multiforme. J Neurosurg 84:442–448
Berger MS, Deliganis AV, Dobbins J, Keles GE (1994) The effect of extent of resection on recurrence in patients with low grade cerebral hemisphere gliomas. Cancer 74:1784–1791
Ciric I, Vick NA, Mikhael MA, Cozzens J, Eller T, Walsh A (1990) Aggressive surgery for malignant supratentorial gliomas. Clin Neurosurg 36:375–383
Collingridge DR, Piepmeier JM, Rockwell S, Knisely JP (1999) Polarographic measurements of oxygen tension in human glioma and surrounding peritumoural brain tissue. Radiother Oncol 53:127–131
Curran WJ Jr, Scott CB, Horton J, Nelson JS, Weinstein AS, Fischbach AJ, Chang CH, Rotman M, Asbell SO, Krisch RE, Nelson F (1993) Recursive partitioning analysis of prognostic factors in three Radiation Therapy Oncology Group malignant glioma trials. J Natl Cancer Inst 85:704–710
Curran WJ Jr, Scott CB, Horton J, Nelson JS, Weinstein AS, Nelson DF, Fischbach AJ, Chang CH, Rotman M, Asbell SO, Powlis W (1992) Does extent of surgery influence outcome for astrocytoma with atypical or anaplastic foci (AAF)? A report from three Radiation Therapy Oncology Group (RTOG) trials. J Neurooncol 12:219–227
Devaux BC, O'Fallon JR, Kelly PJ (1993) Resection, biopsy, and survival in malignant glial neoplasms. A retrospective study of clinical parameters, therapy, and outcome. J Neurosurg 78:767–775
Evans SM, Judy KD, Dunphy I, Jenkins WT, Hwang WT, Nelson PT, Lustig RA, Jenkins K, Magarelli DP, Hahn SM, Collins RA, Grady MS, Koch CJ (2004) Hypoxia is important in the biology and aggression of human glial brain tumors. Clin Cancer Res 10:8177–8184
Fleming AB, Saltzman WM (2002) Pharmacokinetics of the carmustine implant. Clin Pharmacokinet 41:403–419
Fung LK, Ewend MG, Sills A, Sipos EP, Thompson R, Watts M, Colvin OM, Brem H, Saltzman WM (1998) Pharmacokinetics of interstitial delivery of carmustine, 4-hydroperoxycyclophosphamide, and paclitaxel from a biodegradable polymer implant in the monkey brain. Cancer Res 58:672–684
Giese A, Bjerkvig R, Berens ME, Westphal M (2003) Cost of migration: invasion of malignant gliomas and implications for treatment. J Clin Oncol 21:1624–1636
Gottfried ON, Deogaonkar M, Way DL (2000) Postoperative cerebral edema after intracavitary implantation of Gliadel(R) wafers for treatment of malignant gliomas [abstract]. J Invest Med 48(1):79A
Hess KR (1999) Extent of resection as a prognostic variable in the treatment of gliomas. J Neurooncol 42:227–231
Holash J, Maisonpierre PC, Compton D, Boland P, Alexander CR, Zagzag D, Yancopoulos GD, Wiegand SJ (1999) Vessel cooption, regression, and growth in tumors mediated by angiopoietins and VEGF. Science 284:1994–1998
Jeremic B, Milicic B, Grujicic D, Dagovic A, Aleksandrovic J, Nikolic N (2004) Clinical prognostic factors in patients with malignant glioma treated with combined modality approach. Am J Clin Oncol 27:195–204
Keles GE, Anderson B, Berger MS (1999) The effect of extent of resection on time to tumor progression and survival in patients with glioblastoma multiforme of the cerebral hemisphere. Surg Neurol 52:371–379
Keles GE, Chang EF, Lamborn KR, Tihan T, Chang CJ, Chang SM, Berger MS (2006) Volumetric extent of resection and residual contrast enhancement on initial surgery as predictors of outcome in adult patients with hemispheric anaplastic astrocytoma. J Neurosurg 105:34–40
Knisely JP, Rockwell S (2002) Importance of hypoxia in the biology and treatment of brain tumors. Neuroimaging Clin N Am 12:525–536
Kole M, Rock J (2002) Malignant Glioma Surgery: Complication Avoidance. Neurosurgery Quarterly 12:251–258
Koritzinsky M, Seigneuric R, Magagnin MG, van den Beucken T, Lambin P, Wouters BG (2005) The hypoxic proteome is influenced by gene-specific changes in mRNA translation. Radiother Oncol 76:177–186
Kowalczuk A, Macdonald RL, Amidei C, Dohrmann G 3rd, Erickson RK, Hekmatpanah J, Krauss S, Krishnasamy S, Masters G, Mullan SF, Mundt AJ, Sweeney P, Vokes EE, Weir BK, Wollman RL (1997) Quantitative imaging study of extent of surgical resection and prognosis of malignant astrocytomas. Neurosurgery 41:1028–1036
Kreth FW, Berlis A, Spiropoulou V, Faist M, Scheremet R, Rossner R, Volk B, Ostertag CB (1999) The role of tumor resection in the treatment of glioblastoma multiforme in adults. Cancer 86:2117–2123
Kreth FW, Warnke PC, Scheremet R, Ostertag CB (1993) Surgical resection and radiation therapy versus biopsy and radiation therapy in the treatment of glioblastoma multiforme. J Neurosurg 78:762–766
Lacroix M, Abi-Said D, Fourney DR, Gokaslan ZL, Shi W, DeMonte F, Lang FF, McCutcheon IE, Hassenbusch SJ, Holland E, Hess K, Michael C, Miller D, Sawaya R (2001) A multivariate analysis of 416 patients with glioblastoma multiforme: prognosis, extent of resection, and survival. J Neurosurg 95:190–198
Lal A, Peters H, St Croix B, Haroon ZA, Dewhirst MW, Strausberg RL, Kaanders JH, van der Kogel AJ, Riggins GJ (2001) Transcriptional response to hypoxia in human tumors. J Natl Cancer Inst 93:1337–1343
Laws ER, Parney IF, Huang W, Anderson F, Morris AM, Asher A, Lillehei KO, Bernstein M, Brem H, Sloan A, Berger MS, Chang S, Investigators GO (2003) Survival following surgery and prognostic factors for recently diagnosed malignant glioma: data from the Glioma Outcomes Project. J Neurosurg 99:467–473
Mendez I, Jacobs P, MacDougall A, Schultz M (2001) Treatment costs for glioblastoma multiforme in Nova Scotia. Can J Neurol Sci 28:61–65
Mirimanoff R, Mason W, Van den Bent M (2007) Is long-term survival in glioblastoma possible? Updated results of the EORTC/NCIC Phase III randomized trial on radiotherapy (RT) and concomitant and adjuvant temozolomide (TMZ) versus RT alone [abstract]. Int J Radiat Oncol Biol Phys 69(3 Suppl):S2
Navalitloha Y, Schwartz ES, Groothuis EN, Allen CV, Levy RM, Groothuis DR (2006) Therapeutic implications of tumor interstitial fluid pressure in subcutaneous RG-2 tumors. Neuro Oncol 8:227–233
Pichlmeier U, Bink A, Schackert G, Stummer W, ALA Glioma Study Group (2008) Resection and survival in glioblastoma multiforme: An RTOG recursive partitioning analysis of ALA study patients. Neuro Oncol 10:1025–1034
A Report of the Medical Research Council Brain Tumour Working Party (1990) Prognostic factors for high-grade malignant glioma: development of a prognostic index. J Neurooncol 9:47–55
Quigley MR, Maroon JC (1991) The relationship between survival and the extent of the resection in patients with supratentorial malignant gliomas. Neurosurgery 29:385–388
Scott CB, Nelson JS, Farnan NC, Curran WJ Jr, Murray KJ, Fischbach AJ, Gaspar LE, Nelson DF (1995) Central pathology review in clinical trials for patients with malignant glioma. A Report of Radiation Therapy Oncology Group 83–02. Cancer 76:307–313
Simpson JR, Horton J, Scott C, Curran WJ, Rubin P, Fischbach J, Isaacson S, Rotman M, Asbell SO, Nelson JS, Weinstein AS (1993) Influence of location and extent of surgical resection on survival of patients with glioblastoma multiforme: results of three consecutive Radiation Therapy Oncology Group (RTOG) clinical trials. Int J Radiat Oncol Biol Phys 26:239–244
Steltzer KJ, Sauvé KI, Spence AM, Griffin TW, Berger MS (1997) Corpus callosum involvement as a prognostic factor for patients with high-grade astrocytoma. Int J Radiat Oncol Biol Phys 38:27–30
Stummer W, Novotny A, Stepp H, Goetz C, Bise K, Reulen HJ (2000) Fluorescence-guided resection of glioblastoma multiforme by using 5-aminolevulinic acid-induced porphyrins: a prospective study in 52 consecutive patients. J Neurosurg 93:1003–1013
Stummer W, Pichlmeier U, Meinel T, Wiestler OD, Zanella F, Reulen HJ, ALA-Glioma Study Group (2006) Fluorescence-guided surgery with 5-aminolevulinic acid for resection of malignant glioma: a randomised controlled multicentre phase III trial. Lancet Oncol 7:392–401
Stummer W, Reulen HJ, Meinel T, Pichlmeier U, Schumacher W, Tonn JC, Rohde V, Oppel F, Turowski B, Woiciechowsky C, Franz K, Pietsch T, ALA-Glioma Study Group (2008) Extent of resection and survival in glioblastoma multiforme: identification of and adjustment for bias. Neurosurgery 62:564–576
Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn U, Curschmann J, Janzer RC, Ludwin SK, Gorlia T, Allgeier A, Lacombe D, Cairncross JG, Eisenhauer E, Mirimanoff RO, European Organisation for Research and Treatment of Cancer Brain Tumor and Radiotherapy Groups; National Cancer Institute of Canada Clinical Trials Group (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352:987–996
van den Bent MJ, Stupp R, Mason W, Mirimanoff RO, Lacombe D, Gorlia T (2005) Impact of extent of resection on overall survival in newly-diagnosed glioblastoma after chemo-irradiation with temozolomide: further analysis of EORTC study 26981 (abstract). Eur J Cancer (Suppl 2):134
Vecht CJ, Avezaat CJ, van Putten WL, Eijkenboom WM, Stefanko SZ (1990) The influence of the extent of surgery on the neurological function and survival in malignant glioma. A retrospective analysis in 243 patients. J Neurol Neurosurg Psychiatry 53:466–471
Vuorinen V, Hinkka S, Färkkilä M, Jääskeläinen J (2003) Debulking or biopsy of malignant glioma in elderly people - a randomised study. Acta Neurochir (Wien) 145:5–10
Westphal M, Hilt DC, Bortey E, Delavault P, Olivares R, Warnke PC, Whittle IR, Jääskeläinen J, Ram Z (2003) A phase 3 trial of local chemotherapy with biodegradable carmustine (BCNU) wafers (Gliadel wafers) in patients with primary malignant glioma. Neuro Oncol 5:79–88
Westphal M, Ram Z, Riddle V, Hilt D, Bortey E, Executive Committee of the Gliadel Study Group (2006) Gliadel wafer in initial surgery for malignant glioma: long-term follow-up of a multicenter controlled trial. Acta Neurochir (Wien) 148:269–275
Whittle IR (2002) Surgery for gliomas. Curr Opin Neurol 15:663–669
Winger MJ, Macdonald DR, Cairncross JG (1989) Supratentorial anaplastic gliomas in adults. The prognostic importance of extent of resection and prior low-grade glioma. J Neurosurg 71:487–493
Zagzag D, Zhong H, Scalzitti JM, Laughner E, Simons JW, Semenza GL (2000) Expression of hypoxia-inducible factor 1 alpha in brain tumors: association with angiogenesis, invasion, and progression. Cancer 88:2606–2618
Acknowledgments
We would like to thank Dr. Roger Stupp for insightful comments on the manuscript. We also want to thank Susan Wingeron, Michael Raffin and Donna Stefanoni from Nexus Communications, Inc. (North Wales, PA) for their editorial assistance, which was financially supported by Archimedes Pharma.
Conflicts of interest
Walter Stummer, MD, PhD, has received research funding from Medac GmbH and is a consultant with Medac GmbH. Martin J. van den Bent, MD, PhD, is a consultant for MSD and is member of the MSD speakersbureau. Manfred Westphal, MD, PhD, has received honoraria from Ark Therapeutics and Archimedes Pharma.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stummer, W., van den Bent, M.J. & Westphal, M. Cytoreductive surgery of glioblastoma as the key to successful adjuvant therapies: new arguments in an old discussion. Acta Neurochir 153, 1211–1218 (2011). https://doi.org/10.1007/s00701-011-1001-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-011-1001-x