Abstract
Purpose
Although instrumented posterior lumbar interbody fusion (PLIF) has been becoming a popular and effective method for treating degenerative lumbar scoliosis, the clinical outcome is rarely reported. We retrospectively evaluated the clinical and radiographic outcomes in patients with degenerative lumbar scoliosis after instrumented PLIF.
Materials and methods
A total of 58 patient’s clinical characteristics had been reviewed retrospectively including clinical presentations, preoperative medical comorbidities, intraoperative status, and postoperative status. Oswestry disability index (ODI), visual analog scale (VAS), and patient satisfaction were evaluated before surgery and last follow-up period. The relationship between the difference of radiographic parameter and functional outcome was evaluated.
Results
Functional outcomes including ODI scores and VAS were significantly improved at the last visit. The ODI was 28.1 ± 8.0 before surgery and 12.2 ± 8.8 at the last visit. VAS was 7.4 ± 2.0 before surgery and 2.4 ± 2.0 at the last visit. Patient satisfaction was 72% at the last visit. ODI was significantly related to postoperative radiographic parameters including Cobb’s angle (p < 0.001), L4 inclination (p = 0.011), coronal balance (p = 0.007), lateral vertebral translation (p < 0.001), Nash–Moe grade (p = 0.033), Nash–Moe degree (p = 0.025), and sagittal balance (p = 0.041) Using multiple regression analysis, ODI was significantly related to female gender, number of levels fixed, coronal balance, lateral vertebral translation, and Nash–Moe degree. The was no significant correlation between postoperative radiographic parameters and pain (VAS). Only lateral vertebral translation demonstrated a significant correlation in multiple regression analysis.
Conclusions
Based on the VAS and ODI instrument, our studies demonstrated that instrumented PLIF for adult degenerative lumbar scoliosis can achieve a high rate of patient satisfaction and improvement in radiographic and clinical outcomes at a minimum of 2 years of follow-up.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Degenerative lumbar scoliosis had an increased incidence in the aged population, and a rising number of elderly patients suffering from degenerative lumbar scoliosis may be eligible for surgical intervention [58]. Although the etiology of degenerative lumbar scoliosis is not clear, the most commonly implicated causes included osteoporosis [2, 17, 28], degenerative disc disease [2, 17, 28, 44], and vertebral body compression fracture [32]. Patients with degenerative lumbar scoliosis typically present with symptoms of lower back pain, radicular pain, and neurogenic claudication [5]. The natural history of untreated adult lumbar scoliosis is progression of the curve, and bracing cannot prevent progression of the curve in this skeletally mature patient [6, 34, 41]. Surgical indications in patients with degenerative lumbar scoliosis include failure of conservative treatment, neurological deficit, and progression of deformity [17, 18, 31, 42, 45, 54, 55]. Degenerative lumbar scoliosis is a triaxial deformity consisting of axial rotation in the vertical axis, lateral translation toward the convexity of the curve, and anterior translation in the sagittal axis [49], so surgery for degenerative lumbar scoliosis remains challenging, including improvement of the outcomes and radiographic parameters.
Newer advance surgical techniques in spinal fusion with transpedicular instrumentation have markedly improved the ability to correct spinal rigid deformity and surgical outcome [42]. Various methods of surgery for degenerative lumbar scoliosis are used, including decompression alone, decompression and posterior fusion with instrumentation, and combined anterior and posterior fusion with instrumentation [29]. The values of interbody support provided by posterior lumbar interbody fusion (PLIF) have been proven and have become increasingly popular and effective [25, 40, 60]. PLIF can restore disc height, achieve anterior vertebral support, increase lumbar lordosis, and reestablish spinal stability [40, 59]. Instrumented PLIF is an alternative circumferential fusion and is via a posterior approach. Pateder et al. [48] reported that when combined with extensive posterior release, posterior only approach (PLIF or TLIF) is just as effective in coronal and sagittal plane balance correction as combined anterior and posterior surgery for adult lumbar scoliosis.
Although instrumented PLIF has been becoming a popular and effective method for treating degenerative lumbar scoliosis, the clinical outcome is rarely reported. We retrospectively evaluated the clinical and radiographic outcomes in patients with degenerative lumbar scoliosis after instrumented PLIF.
Materials and methods
Inclusion and exclusion criteria
We analyzed patients with degenerative lumbar scoliosis ongoing posterior instrumented interbody cage fusion at the Kaohsiung Medical University Hospital from May 2004 to January 2007. Our surgical indications include failure of conservative treatment, neurological deficit, intractable pain, and progression of deformity. Inclusion criteria consisted of: (1) patient having been diagnosed of degenerative lumbar scoliosis—the definition of degenerative lumbar scoliosis being Cobb angle more than 10° [3]; (2) age >50 years at time of diagnosis; (3) refractory to medical treatment for 6 months; (4) corrected with posterior instrumented lumbar interbody fusion; and (5) follow-up >24 months. Exclusion criteria consisted of: (1) prior spinal trauma or fracture; (2) spinal malignancy; (3) spinal infection; and (4) adult idiopathic scoliosis. Sixty-one patients conformed to the above inclusion criteria. During the follow-period, three patients (3/61) were lost to follow-up.
Clinical characteristics
Clinical presentations
A total of 58 patient’s clinical characteristics had been reviewed retrospectively. The average age of the patients was 68.9 ± 8.5 years (range 51–83 years). There were 11 men and 47 women. All patients presented back pain, 45 patients presented radiculopathy, and 30 patients presented claudication.
Preoperative medical comorbidities
Twenty-nine of 58 (50%) patients had two or more medical comorbidities. Osteoporosis (38/58) and hypertension (34/58) were the most common comorbidities (Table 1). The commonly implicated causes in our series included osteoporosis (40/58, 69%), degenerative disc disease (58/58, 100%), and vertebral body compression fracture (8/58, 14%).
Surgical techniques and perioperative status
Some of the central tenets to consider when treating adult patients with degenerative scoliosis are: (1) decompression of the neural elements for symptoms relief; (2) correction of sagittal balance as well as coronal and rotational deformity for spinal balance; (3) optimizing conditions for osteogenesis and fusion for stability of spine; and (4) prevention of the progression of curves [5]. Decompression, correction of the deformity, and stabilization are important surgical strategies in patients with degenerative lumbar scoliosis. First, decompression of the entire neural component in the stenois segments was performed by removing the hypertrophic ligmentum flavum, facet joint, and performing the lamainectomy and facetomy. Secondary, the extent of fixation and fusion were determined to the uppermost vertebrae and the lowermost vertebrae. Posterior pedicle screw instrumentation not only allows for correction of the deformity but also stabilization of the spine after the decompression.
Third, correction of deformity was performed. The shape of the rod was adjusted by the contour of screw placement and the angle of lordosis. The contouring rod was set in the convex side firstly. Modified bilateral apical derotation maneuver [7] was performed for the correction of scoliosis. A rod derotation maneuver and distraction on the concavity of the curve were used for spine realignment. After the first derotation, the pedicles were inserted again in the convey side. The second contouring rod was set in the convey side again. Correction of the deformity is done to as maximal a degree as possible. Finally, posterior lumbar interbody fusion was performed on all of our patients to stabilize the realigned spine.
Perioperative status included intraoperative blood loss, operative time, the number of levels fused and fixed, and the number of decompression level (Table 1).
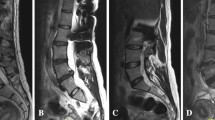
Radiological examinations
Thoracolumbar anterioposterior and lateral standing radiographs were reviewed preoperatively and postoperatively. The Cobb angle, L3 inclination, L4 inclination, lateral apical translation, and coronal balance were measured in the coronal axis. Nash–Moe grade and Nash–Moe degree were measured in the axial axis [46]. Lumbar lordosis, sacral inclination, and sagittal balance were measured in the sagittal axis [13]. The Cobb’s angle of scoliosis in our patients was between 10° and 34°. Radiographic parameters were shown in Table 3.
Functional outcomes
Oswestry disability index (ODI), visual analog scale (VAS), and patient satisfaction were evaluated before surgery and last follow-up period. Patient satisfaction was classified as satisfied or dissatisfied according to self-reported outcomes at the last visit.
Postoperative complications
Postoperative complications were categorized both as early or late complications and minor or major complications (Table 2), including 39 (68%) early perioperative complications and 12 (28%) late complications. Early complications included pulmonary congestion (17%), ileus (36%), delirium (7%), and wound infection (10%). Late complications included adjacent segment disease (12%) and loosening of screws (14%). The average follow-up period was 38.7 ± 11.0 months (range 24–59 months), with a minimum of 2 years’ follow up.
Statistical analysis
Comparisons of the radiographic parameter of patients with degenerative lumbar scoliosis before surgery and the last follow-up period were made using paired t tests. The relationship between the difference of radiographic parameter and functional outcome was evaluated by the Pearson correlation analysis. Linear regression analysis was used to assess the factors related to the clinical outcomes and the radiographic outcomes. All statistical results were established significant if p < 0.05. The analysis was performed with the SPSS 15.0 package software.
Results
The functional outcomes including ODI scores and VAS were significantly improved at the last visit (Table 3). The ODI was 28.1 ± 8.0 before surgery and 12.2 ± 8.8 at the last visit. The VAS was 7.4 ± 2.0 before surgery and 2.4 ± 2.0 at the last visit. Patient satisfaction was 72% at the last visit. Patient excellent satisfaction was 33% (19/58) and good satisfaction was 36% (20/58) at the last visit.
Although no significant correlation between preoperative radiographic parameters and pain (VAS), the preoperative lumbar lordosis angle was significantly related to the Oswestry disability index scores (p = 0.021, Table 4). There was no significant correlation between postoperative radiographic parameters and pain (VAS, Table 5). ODI was significantly related to postoperative radiographic parameters including Cobb’s angle (p < 0.001), L4 inclination (p = 0.011), coronal balance (p = 0.007), lateral vertebral translation (p < 0.001), Nash–Moe grade (p = 0.033), Nash–Moe degree (p = 0.025), and sagittal balance (p = 0.041, Table 5).
Linear regression analysis was used to evaluate the correlation between ODI and difference in radiographic parameters and clinical parameters (Table 6). Female gender, number of levels fixed, Cobb’ angle, coronal balance, lateral vertebral translation, Nash–Moe degree, and Nash–Moe grade significantly correlated with ODI in simple regression analysis. However, ODI was significantly related to female gender, number of levels fixed, coronal balance, lateral vertebral translation, and Nash–Moe degree in multiple regression analysis.
Linear regression analysis was also used to evaluate factors related to difference in the visual analog scale (Table 7). VAS was significantly related to Cobb’ angle, coronal balance, lateral vertebral translation, and Nash–Moe degree; Nash–Moe grade demonstrated significant correlation in simple regression analysis. Only lateral vertebral translation demonstrated significant correlation in multiple regression analysis.
Discussion
Our studies demonstrated that instrumented PLIF in a patient with degenerative lumbar scoliosis can achieve high rates of patient satisfaction and improvement in radiographic and clinical outcomes. The current study focuses on the VAS and ODI instruments outcomes because these were the most consistently used measures. Various clinical and radiographic factors were analyzed to understand the effect of instrumented PLIF for adult degenerative lumbar scoliosis.
Age and gender
An increasing number of elderly patients are undergoing operative treatment for degenerative lumbar disease. Surgery-related complications or mortality were increased in elderly patients [1, 9, 20, 60]. However, some authors have reported that posterior lumbar decompression and fusion can be safely performed in the elderly with a low complication rate [10] and that the age of patients was not a contraindication for surgery [42]. In our study, the age of patients has no significant relation to the clinical outcomes and complications.
Our study showed that female gender was a prognostic factor related to difference in Oswestry disability index scores in patients with degenerative lumbar scoliosis. Previous studies reported an influence of gender on back and leg visual analog scale, Oswestry disability index [33, 43], and patients’ satisfaction [53] in patients undergoing spinal surgery. The reason of sex-related difference in spine surgery is still unknown. The reasons for gender differences in lumbar spine stenosis surgery are probably multifactor due to physiological, pharmacological, and psychological aspects [53]. Therefore, the gender of the patient must be taken into consideration as a crucial factor when performing the surgery in lumbar degenerative disease, especially in scoliosis.
Osteoporosis
Degenerative lumbar scoliosis is common in the elderly population and in particular in postmenopausal women as a consequence of osteoporosis. The incidence of osteoporosis increased with increasing age [11]. Osteoporosis is considered as a significant risk factor for spine instrumentation failure [15, 22, 30, 52]. So some authors attempt to find the fixation strategies for osteoporotic bone [5]. The strategies are targeted either toward taking advantage of the relatively stronger cortical bone [14] or toward augmenting the fixation of a pedicle screw within the existing trabecular bone [56]. In our cases, we routinely perform bone cement augmentation through the pedicle into the vertebral body.
Extension of the fixation and fusion
Determining the extent of the fixation and whether a fusion extends to the sacrum were important surgical strategies in patient with degenerative scoliosis. Several principles were proposed to decide the extent of fixation and fusion: (1) The instrumentation and fixation should not be confined in the deformity to prevent adjacent segment diseases [13, 55] and to prevent the progression of the scoliotic curvature [34, 57]. (2) The instrumentation and fixation should not end in the junction of thoracolumbar spine or sondyliosthesis to maintain sagittal balance or thoracic compensation [13, 34, 37, 55]. (3) Uppermost instrumented vertebrae were determined to restore the balance of spine and to correct the deformity. Most authors demonstrated that the most horizontal vertebrae should be chosen for upper instrumented vertebrae that could correct the deformity completely [34, 35]. In our cases, we choose the most horizontal upper endplate of adjacent two vertebrae as the upper instrumented vertebrae. Using this way to find the upper instrumented vertebrae, the extent of fixation should be shortened as possible under the spinal balance. (4) The level of rotatory subluxation, severe lateral listhesis, or spondylolisthesis must be fused to maintain the stability of the corrected spine. (5) Short segment fixation and fusion is appropriate for the patients with small scoliototic curvatures, without or mild spine imbalance [13, 34, 57]. (6) Long segment fixation and fusion is applied in patients with a larger scoliotic curvature or with severe spinal imbalance. In our study, the level of fixation was significantly related to the difference of functional outcomes between before and after instrumented posterior lumbar interbody cage fusion. Our study demonstrated that the number of level fixed can affect the patient outcome and satisfaction and that short segment fixation is preferred.
Fusion extension to sacrum
Fusion extent to the sacrum in patients with degenerative lumbar scoliosis still remains controversial. Long segment constructs with extension to the sacrum has a better radiographic correction [6], but fusion to the sacrum requires more procedures and more postoperative pseudoarthrodesis [23, 36, 38]. In contrast, arthrodesis at L5 can develop the subsequent progression of L5 S1 segment degeneration [6, 8, 24, 39]. The indications for fusion to the sacrum have been suggested as follows: (1) lumbosacral segment instability due to spondylolisthesis or previous instability [6, 24, 50]; (2) advanced or severe degeneration in the lumbosacral segment [6, 24, 50]; (3) scoliosis or deformity involving the lumbosacral region [6, 24, 50]; and (4) sagittal imbalance and lumbar hypolordosis before surgery [12]. In our study, 21 (21/58, 36%) patients had fusion extension to the sacrum in our series. Fusion extension to the sacrum was not a significant factor relating to the functional outcomes, but we must be meticulous in determining whether to fuse the sacrum in patients with degenerative lumbar scoliosis.
Radiographic correction and clinical outcome
The functional outcomes including ODI scores and VAS were significantly improved after surgery (Table 3). Our study demonstrated that the posterior interbody fusion with instrumentation improves not only in ODI but also in VAS associated with degenerative lumbar scoliosis in the elderly. Interestingly, there was no significant correlation between preoperative radiographic parameters and VAS; the preoperative lumbar lordosis angle was significantly related to ODI. The was no significant correlation between postoperative radiographic parameters and VAS. However, ODI was significantly related to postoperative radiographic parameters. This indicated that better radiographic corrections have better disability improvement (ODI), but not pain (VAS), associated with degenerative lumbar scoliosis in the elderly. VAS is a subjective pain estimator and is usually improved after surgical intervention. Our result demonstrated that VAS is slightly affected by radiographic parameters. ODI is a complex functional outcome estimator and is influenced by the paragraphic parameters and clinical parameters.
Scoliosis represents a complex three-dimensional rotational deformity that affects the spine in the coronal, sagittal, and axial planes. Some authors attempt to find the correction strategies in scoliosis. Correction strategies should be devised to normalize both sagittal balance and coronal and rotational deformity [5, 47]. Such a balanced spinal posture provides for decreased energy requirements with ambulation, limits pain and fatigue, improves cosmesis and patient satisfaction, and limits complications associated with unresolved deformities [35]. Most studies have demonstrated a correlation between radiographic correction and clinical improvement in patients with adult scoliosis [4, 16, 19, 26, 51], but restoration of spine balance is the important factor associated with a good clinical outcome [21, 26, 27] and pain relief [35, 51]. Restoring the balance of the spine in the coronal, axial, and sagittal axes was a more important factor relating to prognosis than other radiographic parameters in patients with degenerative lumbar scoliosis in surgical planning. Interestingly, the difference between preoperative and postoperative Cobb’s angle was not found to have a significant correlation in our multivariate analysis in both ODI and VAS scores. This may have been because of the lower values of surgical correction of Cobb’s angle of the patients included in this study. The association between Cobb’s angle correction and ODI or VAS needs further investigation.
Conclusions
Based on the commonly reported clinical outcome measures, the VAS and ODI instruments, instrumented PLIF for adult degenerative lumbar scoliosis can achieve a high rate of patient satisfaction and improvement in radiographic and clinical outcomes at a minimum of 2 years’ follow-up.
References
Acosta FL, Cloyd JM, Aryan HE, Ames CP (2009) Perioperative complications and clinical outcomes of multilevel circumferential lumbar spinal fusion in the elderly. J Clin Neurosci 16:69–73
Aebi M (2005) The adult scoliosis. Eur Spine J 14:925–948
Aebi M, Marchesi MD (1998) The degenerative adult scoliosis classification and indication for treatment. Spine State Art Rev 12:73–84
Betz RR, Harms J, Clements DH 3rd, Lenke LG, Lowe TG, Shufflebarger HL, Jeszenszky D, Beele B (1999) Comparison of anterior and posterior instrumentation for correction of adolescent thoracic idiopathic scoliosis. Spine (Phila Pa 1976) 24:225–239
Birknes JK, White AP, Albert TJ, Shaffrey CI, Harrop JS (2008) Adult degenerative scoliosis: a review. Neurosurgery 63:94–103
Bridwell KH, Glassman S, Horton W, Shaffrey C, Schwab F, Zebala LP, Lenke LG, Hilton JF, Shainline M, Baldus C, Wootten D (2009) Does treatment (nonoperative and operative) improve the two-year quality of life in patients with adult symptomatic lumbar scoliosis: a prospective multicenter evidence-based medicine study. Spine (Phila Pa 1976) 34:2171–2178
Bridwell KH, Lenke LG, Lewis SJ (2001) Treatment of spinal stenosis and fixed sagittal imbalance. Clin Orthop Relat Res 384:35–44
Brown KM, Ludwig SC, Gelb DE (2004) Radiographic predictors of outcome after long fusion to L5 in adult scoliosis. J Spinal Disord Tech 17:358–366
Carreon LY, Puno RM, Dimar JR 2nd, Glassman SD, Johnson JR (2003) Perioperative complications of posterior lumbar decompression and arthrodesis in older adults. J Bone Joint Surg Am 85:2089–2092
Cassinelli EH, Eubanks J, Vogt M, Furey C, Yoo J, Bohlman HH (2007) Risk factors for the development of perioperative complications in elderly patients undergoing lumbar decompression and arthrodesis for spinal stenosis: an analysis of 166 patients. Spine (Phila Pa 1976) 32:230–235
Chin DK, Park JY, Yoon YS, Kuh SU, Jin BH, Kim KS, Cho YE (2007) Prevalence of osteoporosis in patients requiring spine surgery: incidence and significance of osteoporosis in spine disease. Osteoporos Int 18:1219–1224
Cho KJ, Suk SI, Park SR, Kim JH, Choi SW, Yoon YH, Won MH (2009) Arthrodesis to L5 versus S1 in long instrumentation and fusion for degenerative lumbar scoliosis. Eur Spine J 18:531–537
Cho KJ, Suk SI, Park SR, Kim JH, Kim SS, Lee TJ, Lee JJ, Lee JM (2008) Short fusion versus long fusion for degenerative lumbar scoliosis. Eur Spine J 17:650–656
Coe JD, Warden KE, Herzig MA, McAfee PC (1990) Influence of bone mineral density on the fixation of thoracolumbar implants. A comparative study of transpedicular screws, laminar hooks, and spinous process wires. Spine (Phila Pa 1976) 15:902–907
Cook SD, Salkeld SL, Stanley T, Faciane A, Miller SD (2004) Biomechanical study of pedicle screw fixation in severely osteoporotic bone. Spine J 4:402–408
D’Andrea LP, Betz RR, Lenke LG, Clements DH, Lowe TG, Merola A, Haher T, Harms J, Huss GK, Blanke K, McGlothlen S (2000) Do radiographic parameters correlate with clinical outcomes in adolescent idiopathic scoliosis? Spine (Phila Pa 1976) 25:1795–1802
Daffner SD, Vaccaro AR (2003) Adult degenerative lumbar scoliosis. Am J Orthop 32:77–82
Dawson E, Bernbeck J (1998) The surgical treatment of low back pain. Phys Med Rehabil Clin N Am 9:489–495
Deviren V, Berven S, Kleinstueck F, Antinnes J, Smith JA, Hu SS (2002) Predictors of flexibility and pain patterns in thoracolumbar and lumbar idiopathic scoliosis. Spine (Phila Pa 1976) 27:2346–2349
Deyo RA, Cherkin DC, Loeser JD, Bigos SJ, Ciol MA (1992) Morbidity and mortality in association with operations on the lumbar spine. The influence of age, diagnosis, and procedure. J Bone Joint Surg Am 74:536–543
Djurasovic M, Glassman SD (2007) Correlation of radiographic and clinical findings in spinal deformities. Neurosurg Clin N Am 18:223–227
Dvorak MF, Pitzen T, Zhu Q, Gordon JD, Fisher CG, Oxland TR (2005) Anterior cervical plate fixation: a biomechanical study to evaluate the effects of plate design, endplate preparation, and bone mineral density. Spine (Phila Pa 1976) 30:294–301
Eck KR, Bridwell KH, Ungacta FF, Riew KD, Lapp MA, Lenke LG, Baldus C, Blanke K (2001) Complications and results of long adult deformity fusions down to l4, l5, and the sacrum. Spine (Phila Pa 1976) 26:E182–192
Edwards CC 2nd, Bridwell KH, Patel A, Rinella AS, Jung Kim Y, Berra AB, Della Rocca GJ, Lenke LG (2003) Thoracolumbar deformity arthrodesis to L5 in adults: the fate of the L5-S1 disc. Spine (Phila Pa 1976) 28:2122–2131
Enker P, Steffee AD (1994) Interbody fusion and instrumentation. Clin Orthop Relat Res 300:90–101
Glassman SD, Berven S, Bridwell K, Horton W, Dimar JR (2005) Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976) 30:682–688
Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F (2005) The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976) 30:2024–2029
Grubb SA, Lipscomb HJ, Coonrad RW (1988) Degenerative adult onset scoliosis. Spine (Phila Pa 1976) 13:241–245
Gupta MC (2003) Degenerative scoliosis: options for surgical management. Orthop Clin North Am 34:269–279
Halvorson TL, Kelley LA, Thomas KA, Whitecloud TS 3rd, Cook SD (1994) Effects of bone mineral density on pedicle screw fixation. Spine (Phila Pa 1976) 19:2415–2420
Heary RF (2004) Evaluation and treatment of adult spinal deformity. Invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2004. J Neurosurg Spine 1:9–18
Herkowitz HN, Kurz LT (1991) Degenerative lumbar spondylolisthesis with spinal stenosis. A prospective study comparing decompression with decompression and intertransverse process arthrodesis. J Bone Jt Surg Am 73:802–808
Herno A, Airaksinen O, Saari T, Miettinen H (1994) The predictive value of preoperative myelography in lumbar spinal stenosis. Spine (Phila Pa 1976) 19:1335–1338
Hwang DW, Jeon SH, Kim JW, Kim EH, Lee JH, Park KJ (2009) Radiographic progression of degenerative lumbar scoliosis after short segment decompression and fusion. Asian Spine J 3:58–65
Jackson RP, Simmons EH, Stripinis D (1989) Coronal and sagittal plane spinal deformities correlating with back pain and pulmonary function in adult idiopathic scoliosis. Spine (Phila Pa 1976) 14:1391–1397
Kim YJ, Bridwell KH, Lenke LG, Cho KJ, Edwards CC 2nd, Rinella AS (2006) Pseudarthrosis in adult spinal deformity following multisegmental instrumentation and arthrodesis. J Bone Joint Surg Am 88:721–728
Kim YJ, Bridwell KH, Lenke LG, Glattes CR, Rhim S, Cheh G (2008) Proximal junctional kyphosis in adult spinal deformity after segmental posterior spinal instrumentation and fusion: minimum five-year follow-up. Spine (Phila Pa 1976) 33:2179–2184
Kostuik JP, Hall BB (1983) Spinal fusions to the sacrum in adults with scoliosis. Spine (Phila Pa 1976) 8:489–500
Kuhns CA, Bridwell KH, Lenke LG, Amor C, Lehman RA, Buchowski JM, Edwards C 2nd, Christine B (2007) Thoracolumbar deformity arthrodesis stopping at L5: fate of the L5-S1 disc, minimum 5-year follow-up. Spine (Phila Pa 1976) 32:2771–2776
La Rosa G, Conti A, Cacciola F, Cardali S, La Torre D, Gambadauro NM, Tomasello F (2003) Pedicle screw fixation for isthmic spondylolisthesis: does posterior lumbar interbody fusion improve outcome over posterolateral fusion? J Neurosurg 99:143–150
Li G, Passias P, Kozanek M, Fu E, Wang S, Xia Q, Li G, Rand FE, Wood KB (2009) Adult scoliosis in patients over sixty-five years of age: outcomes of operative versus nonoperative treatment at a minimum two-year follow-up. Spine (Phila Pa 1976) 34:2165–2170
Marchesi DG, Aebi M (1992) Pedicle fixation devices in the treatment of adult lumbar scoliosis. Spine (Phila Pa 1976) 17:S304–309
Mariconda M, Zanforlino G, Celestino GA, Brancaleone S, Fava R, Milano C (2000) Factors influencing the outcome of degenerative lumbar spinal stenosis. J Spinal Disord 13:131–137
Murata Y, Takahashi K, Hanaoka E, Utsumi T, Yamagata M, Moriya H (2002) Changes in scoliotic curvature and lordotic angle during the early phase of degenerative lumbar scoliosis. Spine (Phila Pa 1976) 27:2268–2273
Nasca RJ (1989) Rationale for spinal fusion in lumbar spinal stenosis. Spine (Phila Pa 1976) 14:451–454
Nash CL Jr, Moe JH (1969) A study of vertebral rotation. J Bone Joint Surg Am 51:223–229
Oskouian RJ Jr, Shaffrey CI (2006) Degenerative lumbar scoliosis. Neurosurg Clin N Am 17:299–315
Pateder DB, Kebaish KM, Cascio BM, Neubaeur P, Matusz DM, Kostuik JP (2007) Posterior only versus combined anterior and posterior approaches to lumbar scoliosis in adults: a radiographic analysis. Spine (Phila Pa 1976) 32:1551–1554
Ploumis A, Transfeldt EE, Gilbert TJ Jr, Mehbod AA, Dykes DC, Perra JE (2006) Degenerative lumbar scoliosis: radiographic correlation of lateral rotatory olisthesis with neural canal dimensions. Spine (Phila Pa 1976) 31:2353–2358
Polly DW Jr, Hamill CL, Bridwell KH (2006) Debate: to fuse or not to fuse to the sacrum, the fate of the L5-S1 disc. Spine (Phila Pa 1976) 31:S179–184
Schwab FJ, Smith VA, Biserni M, Gamez L, Farcy JP, Pagala M (2002) Adult scoliosis: a quantitative radiographic and clinical analysis. Spine (Phila Pa 1976) 27:387–392
Seller K, Wahl D, Wild A, Krauspe R, Schneider E, Linke B (2007) Pullout strength of anterior spinal instrumentation: a product comparison of seven screws in calf vertebral bodies. Eur Spine J 16:1047–1054
Shabat S, Folman Y, Arinzon Z, Adunsky A, Catz A, Gepstein R (2005) Gender differences as an influence on patients’ satisfaction rates in spinal surgery of elderly patients. Eur Spine J 14:1027–1032
Simmons ED (2001) Surgical treatment of patients with lumbar spinal stenosis with associated scoliosis. Clin Orthop Relat Res 384:45–53
Simmons ED Jr, Simmons EH (1992) Spinal stenosis with scoliosis. Spine (Phila Pa 1976) 17:S117–120
Tan JS, Kwon BK, Dvorak MF, Fisher CG, Oxland TR (2004) Pedicle screw motion in the osteoporotic spine after augmentation with laminar hooks, sublaminar wires, or calcium phosphate cement: a comparative analysis. Spine (Phila Pa 1976) 29:1723–1730
Tribus CB (2003) Degenerative lumbar scoliosis: evaluation and management. J Am Acad Orthop Surg 11:174–183
Vanderpool DW, James JI, Wynne-Davies R (1969) Scoliosis in the elderly. J Bone Joint Surg Am 51:446–455
Wang JC, Mummaneni PV, Haid RW (2005) Current treatment strategies for the painful lumbar motion segment: posterolateral fusion versus interbody fusion. Spine (Phila Pa 1976) 30:33–43
Wu CH, Wong CB, Chen LH, Niu CC, Tsai TT, Chen WJ (2008) Instrumented posterior lumbar interbody fusion for patients with degenerative lumbar scoliosis. J Spinal Disord Tech 21:310–315
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tsai, TH., Huang, TY., Lieu, AS. et al. Functional outcome analysis: instrumented posterior lumbar interbody fusion for degenerative lumbar scoliosis. Acta Neurochir 153, 547–555 (2011). https://doi.org/10.1007/s00701-010-0909-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-010-0909-x