Abstract
Background
Working with patients with intracranial aneurysms, we have developed a clinical suspicion that there may be differences in the rupture rate of aneurysms depending on the aneurysm’s anatomical location. The aim of the study was to examine the anatomical distribution of ruptured and unruptured intracranial aneurysms in a defined population.
Method
We retrospectively included all patients with an aneurysm treated in our institution between 1 January 1990 and 31 December 1999, and collected the relevant data from the individual patient files. With the Koivisto categories for aneurysm location, we gathered the aneurysms into four categories: ACA, MCA, ICA, and VBA.
Findings
Four hundred forty-four aneurysms were included in the study: 361 in SAH patients and 83 in patients without SAH. ACA aneurysms were over-represented in the ruptured group (36.0% vs. 9.6%, p < 0.0001). MCA aneurysms were more frequent in the unruptured group (51.8% vs. 29.6%, p < 0.0002). Ruptured ACA aneurysms were over-represented among males (p < 0.0001), whereas ruptured ICA aneurysms were more frequent among females (p < 0.0001). Ruptured aneurysms in the posterior circulation were more frequently found on the left side (p < 0.0001).
Conclusion
This study shows that the anatomical distribution of aneurysms is different in SAH patients compared with patients with unruptured aneurysms. Haemodynamic features of the vessel of origin may explain the differences we have found. Furthermore, this study suggests that it is of particular importance to treat patients with incidentally found ACA aneurysms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Due to more frequent use of cerebral MRI in the evaluation of minor symptoms, increasing numbers of patients are diagnosed with unruptured intracranial aneurysms (UIA) that prompt counselling. A recent MRI study of healthy volunteers identified a 1.8% prevalence of intracranial aneurysms [28]. Thus, the question of how we should deal with these incidentally found aneurysms poses a problem, and as of yet no solution has been found. Internationally, there is no consensus on how to manage UIAs [18]. As the effects of aneurysm rupture are potentially devastating [3, 23], information on all aspects of rupture risk is important in the counselling of patients with UIAs.
Over the years we have developed a clinical suspicion that there may be differences in the rupture rate of aneurysms depending on the aneurysm’s anatomical location. More specifically, it is our impression that anterior communicating artery aneurysms (AComA) present more frequently as the cause of an acute subarachnoid haemorrhage (SAH) compared with aneurysms in other locations. This observation seems to be in line with data underlying a Finnish study investigating the use of routine cerebral angiography after surgery for saccular aneurysms in which the ratio between ruptured and unruptured AComA was 2.5 [15]. If aneurysms in certain locations are more prone to rupture than others, it is important to clarify not only that such differences exist, but also to identify possible mechanisms behind them.
Reviewing the literature, we found conflicting data on the anatomical distribution of intracranial aneurysms, as well as ethnic differences [10, 11, 16, 22]. The majority of authors recognise female gender, smoking, and hypertension as independent risk factors for intracranial aneurysm formation [12–14, 29]. Much of the debate has also been centred on aneurysm size and if there is an ultimate threshold predicting increased rupture risk [20]. Some evidence also points to aneurysm location as an independent variable predicting rupture, in which basilar tip, AComA, and posterior communicating artery aneurysms (PComA) may all have an increased rupture risk [1, 6, 11, 30]. However, these observations have been made in populations known to have special risk factors for rupture (Japanese and Finnish), and in potentially biased cohorts [1], [7]. It is also possible that regional flow differences may contribute to aneurysm formation. Interestingly, it has been shown that unilateral ligation of the common carotid artery in hypertensive rats can produce AComA aneurysms [8]. In computer simulation studies of aneurysms factors like small impact zone, higher flow rate entering the aneurysm, elevated maximum wall shear stress (WSS), disturbed intra-aneurysmal flow, and narrow jets have been associated with increased risk of rupture [4, 5]. Regarding WSS, Shojima et al. found by mathematical simulation of 20 MCA vessels with aneurysms that maximum WSS occurred near the aneurysm neck and that a low WSS in the aneurysm tip may facilitate aneurysm growth and later rupture due to aneurysm wall degeneration[24].
In the current study of a stable population in a defined geographical region, we have compared unruptured with ruptured aneurysms with respect to anatomical location. The aim was to see if there was a different anatomical distribution of the aneurysms in the two patient groups.
Materials and methods
Hospital structure and population under study
The organisation of the neurosurgical services in Norway has been reported previously [9]. Briefly, in the study period, Norway had five university clinics with neurosurgical departments, each serving smaller local hospitals in one health region. A health region consisted of a geographical area with a well-defined population. There was no geographical overlap between the five health regions. Haukeland University Hospital was the university hospital on the southwestern coast of Norway, serving three counties. Our department was the only neurosurgical referral centre for all hospitals within this region. Thus, all patients that were diagnosed with an intracranial aneurysm in our health region, ruptured or not, were evaluated by our team. The patient leak from our region to other neurosurgical centres was negligible. During the study period the total population in our health region increased from 855,542 in 1991 to 908,589 in 1999 [26].
Patients
The patients included in this retrospective study were identified from the hospital database of diagnosis and treatment in the period from 1 January 1990 through 31 December 1999. The search was performed with registration of every patient in the period with diagnosis codes of 430 and 437.3 (International Classification of Diseases 9) or I60.0-I60.9 and I67.1 (International Classification of Diseases 10). These were the diagnostic codes assigned to patients with ruptured intracranial aneurysms (RIA) or UIAs in our hospital during the study period. Patients with subarachnoid haemorrhage from an arterio-venous malformation or from an unknown source, including perimesencephalic SAH, were excluded. Demographic data and clinical state on admission according to the Hunt and Hess score were registered for all patients. Angiographic data were extracted from the neuroradiology reports. The Koivisto categories [17] for aneurysm location were used:
-
1.
ACA: anterior cerebral artery, anterior communicating artery, pericallosal artery
-
2.
MCA: middle cerebral artery
-
3.
ICA: internal carotid artery, ophthalmic artery, posterior communicating artery, anterior choroidal artery
-
4.
VBA: vertebrobasilar arteries
Statistical analysis
All analyses were performed with SPSS 14.0 for Windows (SPSS, Inc., Chicago, IL). An α-level of 0.05 was used as the significance level in all tests. Group comparisons were performed with Student's t test for normally distributed continuous variables or Mann-Whitney U test for continuous or ordered categorical variables with abnormal distribution. Contingency tables were analysed with Fisher's exact test for dichotomized variables or χ2 statistics.
Results
General characteristics
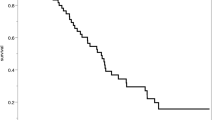
The median crude rate of intracranial aneurysms referred to our centre was 5.7/100,000 per year, increasing from 3.5/100,000 in 1991 to 6.38/100,000 in 1999. The annual number of patients with SAH increased similarly in the study period from 18 (1990) to 50 (1999) (Table 1). The median number of SAH patients each year was 36.5. In total there were 483 intracranial aneurysms in 421 patients registered and evaluated in our hospital in the 10-year period. Three hundred sixty-one aneurysms had ruptured and caused SAH. The remaining 60 patients, all without a previous SAH history, had a total of 83 UIAs. We excluded 39 UIAs in patients that presented with SAH from another aneurysm, leaving 444 aneurysms eligible for analysis. These 444 aneurysms were found in 421 patients: 197 aneurysms in men (44.4%) and 247 aneurysms in women (55.6%). The female over-representation was statistically significant (p = 0.017). The median age of the patients was 50.9 (range 19.6-86.6 years); interestingly, men were significantly younger than women (48.2 years vs. 53.8 years, p < 0.0001).
Ruptured aneurysms
The median age of the 361 SAH patients was 50.8 (range 19.6–86.6), with men being significantly younger than women (48.6 vs. 53.8 years, p < 0.0001). There were 170 aneurysms in men and 191 in women (p = 0.27). With the Koivisto categories the following distribution of aneurysms was found: ACA 36.0%, MCA 29.6%, ICA 24.4%, and VBA 10.0%. For the ACA, there were 121 (93.1%) AComA, 6 (4.6%) pericallosal, 1 A2 (0.8%), and 2 (1.6%) anterior aneurysms.
ACA aneurysms were over-represented among men (49 F, 81 M, p < 0.0001), and ICA aneurysms were over-represented among women (64 F, 24 M, p < 0.0001). For MCA and VBA aneurysms, there were no significant gender differences (Table 2).
Two-hundred nineteen of the aneurysms (60.7%) could be lateralised to the right or to the left of the anatomical midline. There was a significant difference in sidedness between aneurysms in the anterior and posterior circulation (p < 0.0001). This difference was caused solely by a left sidedness for ruptured VBA aneurysms (Table 3). Also, when comparing supra- and infratentorially located aneurysms, there was a significant difference in sidedness (Table 4).
Unruptured aneurysms
The median age of the 60 patients with unruptured aneurysms was 49.1 years (range 22.9–80.4 years). Men were significantly younger than women (45.6 vs. 53.7 years, p = 0.005)
There were 27 aneurysms in men and 56 in women (p = 0.001). The distribution of aneurysms was: ACA 9.6%, MCA 51.8%, ICA 33.7%, and VBA 4.8%. Forty-seven (56.6%) of the unruptured aneurysms could be assigned to either the right or the left side in the intracranial circulation; there was however no significant sidedness present for these aneurysms.
Comparison between ruptured and unruptured aneurysms
There was no difference in gender for ruptured aneurysms, but men were under-represented among the UIAs (p = 0.0196). Median age was similar (50.8 and 49.1, p = 0.85) in the two groups (RIA and UIA), but men were significantly younger in both categories (p < 0.0001 and p = 0.005, respectively). Anatomically, ACA aneurysms were much more frequent in the RIA group (36.0% vs. 9.6%, p < 0.0001), while MCA aneurysms were more frequent in the UIA group (51.8% vs. 29.6%, p < 0.0002). For the ICA and VBA locations, no significant differences were found between the RIAs and the UIAs aneurysms (Table 5 for details).
Discussion
In the present population-based study of 444 intracranial aneurysms, we found a significant over-representation of ACA aneurysms in SAH patients in comparison to patients with UIAs. In fact, the frequency of ACA aneurysms was more than three times higher in the RIA than in the UIA group of aneurysms. MCA aneurysms, on the other hand, were clearly over-represented in the UIA group. For SAH patients, ACA aneurysms were over-represented in men, and ICA aneurysms in women. These results support our clinical suspicion, namely that ACA aneurysms seem to have a higher rupture risk, and thus possibly should be treated more aggressively than MCA aneurysms when found incidentally. The findings in our study are in line with data underlying a Finnish study [15]. In this study of more than 800 aneurysms, the distribution of ruptured and unruptured ACA and MCA aneurysms was 41% vs. 18% and 29% vs. 51%, respectively. Further, a three-dimensional angiography study of 155 consecutive aneurysms found the same over-representation (44.9 vs. 20.4%) of ACA aneurysms in ruptured vs. unruptured aneurysms [2]. Thus, evidence from different sources points to ACA aneurysms as being more prone to rupture than MCA aneurysms.
Furthermore, our study showed that ruptured VBA aneurysms were much more often found on the left side. This left-sided dominance in the posterior circulation may be explained by systematic differences in the intraluminal haemodynamics between the two sides, caused by asymmetries of the precerebral artery tree. It is a puzzling fact that in a study of 1,413 brains, only 34.5% had a balanced configuration of the circulus Willisi [27]. For the vertebral arteries, some interesting side differences between the right and the left side have been described, with the left side usually being the dominant. This applies both to normal variations in diameter and pathologically narrowed vessels [19, 21, 25]. Based on our results, we therefore hypothesise that dominant vertebral arteries on the left side may explain the observed left sidedness for ruptured VBA aneurysms. Correspondingly, one might ask whether such differences in vessel calibre could explain why ACA aneurysms were more frequent in the SAH group and MCA aneurysms in the UIA group. Could it be that a greater dimension of the feeding vessel would add to the flow and turbulence in the aneurysm? However, due to the design of the study we have no available data from the angiography investigations to enlighten this issue.
Men were significantly younger at diagnosis than women. The median difference was 5.2 years in the SAH group and 8.1 years in the UIA group. We have not identified any explanations for this age difference. With the anatomical distribution present in this study in mind, one might therefore argue that the indication for treating young men with ACA aneurysms is particularly strong.
Bearing in mind that this study was population-based from a single centre, we have identified a number of limitations. Although all patients diagnosed with an intracranial aneurysm in our region were routinely evaluated and treated in our department, there were some patients that never came to our attention. We have no information on the number of sudden deaths caused by SAH; however, intuitively this number should be low. Furthermore, some moribund SAH patients might not have been referred to our institution, since it is the medical team at the local community hospitals that decides whether to refer or not. In the studied period there was also a more conservative treatment policy for the older age groups. For SAH patients above 70 years, angiography and clipping were routinely not performed in the first part of the study period. Gradually, this regimen was changed and thus the oldest SAH patient in the material was 86.6 years. Nevertheless, the number of patients above 70 years should be low and thus conceivably not alter the main results of the study.
In conclusion, this retrospective, population-based study showed that there were anatomical differences in the distribution of intracranial aneurysms between SAH and UIA patients. The results indicate that laterality and vessel of origin are important factors contributing to the pathophysiology behind aneurysm formation and rupture. Finally, the study emphasises the importance of treating patients with incidentally found ACA aneurysms.
Reference
(1998) Unruptured intracranial aneurysms—risk of rupture and risks of surgical intervention. International Study of Unruptured Intracranial Aneurysms Investigators. N Engl J Med 339:1725–1733. doi:10.1056/NEJM199812103392401
Beck J, Rohde S, Berkefeld J, Seifert V, Raabe A (2006) Size and location of ruptured and unruptured intracranial aneurysms measured by three-dimensional rotational angiography. Surg Neurol 65:18–25. doi:10.1016/j.surneu.2005.05.019 discussion 25–17
Broderick JP, Brott T, Tomsick T, Miller R, Huster G (1993) Intracerebral hemorrhage more than twice as common as subarachnoid hemorrhage. J Neurosurg 78:188–191
Castro MA, Putman CM, Sheridan MJ, Cebral JR (2009) Hemodynamic patterns of anterior communicating artery aneurysms: a possible association with rupture. AJNR Am J Neuroradiol 30:297–302. doi:10.3174/ajnr.A1323
Cebral JR, Castro MA, Burgess JE, Pergolizzi RS, Sheridan MJ, Putman CM (2005) Characterization of cerebral aneurysms for assessing risk of rupture by using patient-specific computational hemodynamics models. AJNR Am J Neuroradiol 26:2550–2559
Fogelholm R, Hernesniemi J, Vapalahti M (1993) Impact of early surgery on outcome after aneurysmal subarachnoid hemorrhage. A population-based study. Stroke 24:1649–1654
Guillemin F (2008) [Critical analysis of the ISUIA study: The methodological point of view]. J Neuroradiol
Hashimoto N, Handa H, Nagata I, Hazama F (1980) Experimentally induced cerebral aneurysms in rats: Part V. Relation of hemodynamics in the circle of Willis to formation of aneurysms. Surg Neurol 13:41–45
Helland CA, Krakenes J, Moen G, Wester K (2006) A population-based study of neurosurgical and endovascular treatment of ruptured, intracranial aneurysms in a small neurosurgical unit. Neurosurgery 59:1168–1175. doi:10.1227/01.NEU.0000245627.93215.BF discussion 1175–1166
Hernesniemi J, Vapalahti M, Niskanen M, Tapaninaho A, Kari A, Luukkonen M, Puranen M, Saari T, Rajpar M (1993) One-year outcome in early aneurysm surgery: a 14 years experience. Acta Neurochir (Wien) 122:1–10. doi:10.1007/BF01446980
Inagawa T, Hada H, Katoh Y (1992) Unruptured intracranial aneurysms in elderly patients. Surg Neurol 38:364–370. doi:10.1016/0090-3019(92)90023-G
Juvela S (2001) Cigarette smoking and death following subarachnoid hemorrhage. J Neurosurg 95:551–554
Juvela S (2002) Hypertension and aneurysmal subarachnoid hemorrhage. Wien Klin Wochenschr 114:285–286
Juvela S (2002) Risk factors for aneurysmal subarachnoid hemorrhage. Stroke 33:2152–2153. doi:10.1161/01.STR.0000029381.77791.3A author reply 2152–2153
Kivisaari RP, Porras M, Ohman J, Siironen J, Ishii K, Hernesniemi J (2004) Routine cerebral angiography after surgery for saccular aneurysms: is it worth it? Neurosurgery 55:1015–1024. doi:10.1227/01.NEU.0000141043.07303.60
Koffijberg H, Buskens E, Granath F, Adami J, Ekbom A, Rinkel G, Blomqvist P (2007) Subarachnoid haemorrhage in Sweden 1987–2002: regional incidence and case fatality rates. J Neurol Neurosurg Psychiatry
Koivisto T, Vanninen R, Hurskainen H, Saari T, Hernesniemi J, Vapalahti M (2000) Outcomes of early endovascular versus surgical treatment of ruptured cerebral aneurysms. A prospective randomized study. Stroke 31:2369–2377
Komotar RJ, Mocco J, Solomon RA (2008) Guidelines for the surgical treatment of unruptured intracranial aneurysms: the first annual J. Lawrence pool memorial research symposium—controversies in the management of cerebral aneurysms. Neurosurgery 62:183–193 discussion 193–184
Lovrencic-Huzjan A, Demarin V, Bosnar M, Vukovic V, Podobnik-Sarkanji S (1999) Color Doppler flow imaging (CDFI) of the vertebral arteries—the normal appearance, normal values and the proposal for the standards. Coll Antropol 23:175–181
Mitchell P, Gholkar A, Vindlacheruvu RR, Mendelow AD (2004) Unruptured intracranial aneurysms: benign curiosity or ticking bomb? Lancet Neurol 3:85–92. doi:10.1016/S1474-4422(03)00661-6
Park JH, Kim JM, Roh JK (2007) Hypoplastic vertebral artery: frequency and associations with ischaemic stroke territory. J Neurol Neurosurg Psychiatry 78:954–958. doi:10.1136/jnnp. 2006.105767
Rinkel GJ, Djibuti M, Algra A, van Gijn J (1998) Prevalence and risk of rupture of intracranial aneurysms: a systematic review. Stroke 29:251–256
Sarti C, Tuomilehto J, Salomaa V, Sivenius J, Kaarsalo E, Narva EV, Salmi K, Torppa J (1991) Epidemiology of subarachnoid hemorrhage in Finland from 1983 to 1985. Stroke 22:848–853
Shojima M, Oshima M, Takagi K, Torii R, Hayakawa M, Katada K, Morita A, Kirino T (2004) Magnitude and role of wall shear stress on cerebral aneurysm: computational fluid dynamic study of 20 middle cerebral artery aneurysms. Stroke 35:2500–2505. doi:10.1161/01.STR.0000144648.89172.0f
Songur A, Gonul Y, Ozen OA, Kucuker H, Uzun I, Bas O, Toktas M (2008) Variations in the intracranial vertebrobasilar system. Surg Radiol Anat
StatisticsNorway (2006) Population changes in the counties and the country 1951–2006. Statistisc Norway Oslo
Stehbens WE (1963) Aneurysms and anatomical variation of cerebral arteries. Arch Pathol 75:45–64
Vernooij MW, Ikram MA, Tanghe HL, Vincent AJ, Hofman A, Krestin GP, Niessen WJ, Breteler MM, van der Lugt A (2007) Incidental findings on brain MRI in the general population. N Engl J Med 357:1821–1828. doi:10.1056/NEJMoa070972
Wermer MJ, van der Schaaf IC, Algra A, Rinkel GJ (2007) Risk of rupture of unruptured intracranial aneurysms in relation to patient and aneurysm characteristics: an updated meta-analysis. Stroke 38:1404–1410. doi:10.1161/01.STR.0000260955.51401.cd
Wiebers DO, Whisnant JP, O'Fallon WM (1981) The natural history of unruptured intracranial aneurysms. N Engl J Med 304:696–698
Author information
Authors and Affiliations
Corresponding author
Additional information
Comment
In this population based study, the authors try to analyze the characteristics of a ruptured aneurysm based on a retrospective analysis of 444 aneurysms in 421 aneurysms, looking specifically at the gender, location and sidedness. Follow-up data on the unruptured aneurysms have not been analyzed and hence the natural history is unavailable.
In this well-written article, apart from giving us a good demographic profile of ruptured aneurysms in a defined population, most of the findings are in consonance with available data [1, 2]. The tendency for even small aneurysms in the anterior cerebral artery location to bleed has been described [3, 4]. One possibly unique finding of unknown significance was the left-sided preponderance for ruptured posterior circulation aneurysms.
The authors conclusion that young males with anterior cerebral artery aneurysms need to be treated aggressively is justified.
References:
1. Juvela S, Porras M, Poussa K. Natural history of unruptured intracranial aneurysms: probability of and risk factors for aneurysm rupture. J Neurosurg. 2000 Sep;93(3):379–87.
2. Wermer MJ, van der Schaaf IC, Algra A, Rinkel GJ . Risk of rupture of unruptured intracranial aneurysms in relation to patient and aneurysm characteristics: an updated meta-analysis. Stroke. 2007 Apr;38(4):1404–10.
3. Forget TR Jr, Benitez R, Veznedaroglu E, Sharan A, Mitchell W, Silva M, Rosenwasser RH. A review of size and location of ruptured intracranial aneurysms. Neurosurgery. 2001 Dec;49(6):1322–5
4. Castro MA, Putman CM, Sheridan MJ, Cebral JR. Hemodynamic patterns of anterior communicating artery aneurysms: A possible association with rupture. AJNR Am J Neuroradiol. 2009 Jan 8(Epub).
R. Kariyattil
Kerala, India
Rights and permissions
About this article
Cite this article
Aarhus, M., Helland, C.A. & Wester, K. Differences in anatomical distribution, gender, and sidedness between ruptured and unruptured intracranial aneurysms in a defined patient population. Acta Neurochir 151, 1569–1574 (2009). https://doi.org/10.1007/s00701-009-0316-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-009-0316-3