Abstract
Background
Ruptured blister-like aneurysms arising at non-branching sites of the internal carotid artery (BLICAA’s) sometimes cause disaster during aneurysm repair because of their characteristic configurations. Our study was designed to establish the best surgical strategies for such aneurysms.
Method
Eighteen BLICAA’s (0.9% of all treated aneurysms) treated at our institute from January 1994 to July 2006 were retrospectively analysed using the database and imaging studies. We assessed the management outcome with the modified Rankin Scale (mRS). The average follow-up period was 17 months.
Findings
Their ages ranged from 30 to 68 years with a mean age of 50. There were 16 females, and two males). The angiographic diameter of the aneurysmal sac sranged from 1.4 to 5 mm with a mean diameter of 2.5 mm. The common origins were dorso-medial (n = 7) or dorsal (n = 6) wall of the ICA. Fifteen patients underwent wrapping with cellulose fabric and clipping. Of the remainder, each underwent direct clipping, suturing, or trapping. The overall outcome was mRS 1 in 11 patients (78.0%), two in three patients, three in one patient, one in one patient, and five in two patients. Intra-operative premature rupture occurred in six patients. There was no rebleeding during the follow-up period. Cerebral infarctions following carotid trapping after premature rupture and stenosis after suturing of perforated carotid wall were causes of mortality. The causes of morbidity included initial brain insult and vasospasm.
Conclusions
The surgeon should be ware of the high risk of premature rupture during dissection of BLICAA’s. Wrapping with cellulose fabric (Bemsheet®) and holding clipping technique could be chosen as the optimal surgical modality for prevention of rebleeding from these lesions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ruptured blister-like aneurysms arising at non branching site of the internal carotid artery (BLICAA’s) sometimes bring disaster during aneurysm repair because of their characteristic configurations. They are fragile, broad-based aneurysms without an identifiable neck which can rupture during dissection and cause post-operative rebleeding more frequently than normal saccular aneurysms [1, 7]. This study was designed to establish the best surgical strategies for these lesions.
Clinical materials and methods
From January 1994 to July 2006, 2,015 consecutive patients with intracranial aneurysms were treated by surgical or endovascular methods at our institute. Of these, 448 patients presented with ruptured aneurysms at the ICA. We selected ruptured blister-like aneurysms at non-branching sites of the ICA as confirmed by operative findings. Aneurysms at branching sites of the ICA, such as ICA bifurcation, IC-ophthalmic artery, cavernous portion of ICA, and IC-superior hypophyseal artery were excluded. Eighteen (0.9% of all patients, 4% of ruptured ICA aneurysms) patients had blister-like aneurysms. These patients were analysed retrospectively according to the following factors: age, sex, side, past history of hypertension, origin of the aneurysm on the circumference of the ICA wall, Hunt & Hess grade, operative methods, temporary clipping time, and clinical outcomes. The classification of the aneurysm location was based on anatomical angiographic evidence. We assessed the management outcome using with the modified Rankin Scale. The average follow-up period was 17 months (range: 6–50 months).
Results
The incidence of BLICAA’s comprised 0.9% of all treated intracranial aneurysms, and 4.0% of ruptured ICA aneurysms. The mean age of the patients was 50 years. Sixteen patients were women and two were men. Ten lesions were located on the right side and eight were on the left. A past history of hypertension was observed in six patients. Most were located on the dorso-medial wall (n = 7) or dorsal wall (n = 6). The pre-operative grade determined by the Hunt & Hess classification showed grade II in four patients, grade III in ten patients, and grade IV in four patients. None were classified as grade I clinically. The mean duration from bleed to operation was 3 days. All operations were performed with somato-sensory evoked potential (SEP) monitoring. The blister-like aneurysms were treated by direct clipping in one patient, holding clipping and wrapping in fifteen patients, suturing of ICA in one patient, and trapping of the ICA in one patient. No patient needed extra-cranial intra-cranial arterial bypass (EIAB). The mean time of temporary clipping was 14.4 min. Intra-operative bleeding occurred in six patients, and was treated by clipping in one, trapping in one, suturing in one, and clipping to secure wrapping in three patients. The trapping procedure was done due to laceration of the fragile aneurysm wall, and resulted in brain infarction and death ten days after operation. In the patient who undewent suturing of the ICA, the aneurysmal wall was perforated during dissection of a haematoma, and repaired using 9-0 nylon. This patient died seven days after the operation because of brain swelling due to ICA stenosis. It may have also resulted from a long period of temporary clipping (36 min) and poor general condition of the patient. In those who had clipping on wrapping material, direct surgical clipping was difficult and carried the risk of premature rupture; clipping on wrapping material (cellulose fabric) encircling the entire circumference of the ICA was applied without injury to the perforators. No patients had post-operative bleeding. Post-operative complications included global infarction, hemiparesis, hydrocephalus, and Terson’s syndrome. Two patients with global infarction died, two presented with transient or permanent complete hemiparesis, and one patient with Terson’s syndrome experienced decreased visual acuity. Post-operative hydrocephalus needing a ventriculo-peritoneal shunt operation occurred in six patients. The overall outcome was mRS 1 in 11 patients (78.0%), two in three patients, three in one patient, four in one patient, and five in two patients (Table 1.).
Illustrative clinical examples
Patient 16
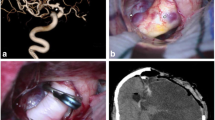
A 61-year-old woman was admitted for treatment of a recurrent oligodendroglioma of the right frontal lobe. She was alert and had no focal neurological deficit. She underwent a craniotomy and removal of the tumour and remained without any neurological deficit. Her post-operative course was uneventful, but on post-operative day 7, she showed sudden deterioration of consciousness. Follow-up computed tomography revealed diffuse subarachnoid haemorrhage (SAH). Conventional cerebral angiography showed a broad neck aneurysm measuring 3.5 × 2.7 mm dorso-medial wall of the left ICA. In view of her unstable vital signs and impaired state of cardiac function, we performed an operation for obliteration of the aneurysm 14 days after the bleed. Her pre-operative Hunt and Hess grade was IV. A left pterional craniotomy was performed and the cervical ICA was exposed. After dissection of the blister-like aneurysm, direct clipping was performed with a L-shaped ring clip without any complication. A small residual bulging portion of the aneurysm was wrapped with cellulose fabric and holding clip. She subsequently underwent a ventriculo-peritoneal shunt operation for post-haemorrhagic hydrocephalus, and was transferred to the Department of Rehabilitation for comprehensive rehabilitation. Her mRS was 4 (Fig. 1).
Illustrative example-patient 16: a brain CT; b angiogram showing SAH due to ruptured blister-like left ICA aneurysm (arrow). Operative procedure c and d showing direct clipping with L-shaped ring clip e a small residual bulging portion of the aneurysm (arrow) was wrapped with cellulose fabric f application of holding clip
Patient 17
A 58-year-old woman was drowsy when transferred for treatment of aneurysmal SAH and the CT brain showed diffuse SAH. Conventional cerebral angiography showed a blister-like aneurysm measuring 1.7 × 1.4 mm on the dorsal wall of the right IC2 segment. On admission a, right pterional craniotomy was performed after lumbar drainage and cervical ICA exposure. The anterior clinoid process was drilled out for proper operative view and space to insert cellulose fabric without ophthalmic artery injury. After inserting cellulose fabric encircling the ICA with peri-aneurysmal haematoma, an L-shaped holding clip was applied. No adverse event occurred during the operation. The patient was discharged on post-operative day 14 without a focal neurological deficit (Fig. 2).
Case 12
A 52 year old woman presented with SAH with CT blood pattern of Fisher grade 3. Conventional cerebral angiography revealed a BLICAA measuring 4.0 × 2.7 mm on the dorsal wall of the right IC2 segment. On the next day, right pterional craniotomy was performed after lumbar drainage and cervical ICA exposure. After encircling the ICA and peri-aneurysmal haematoma with cellulose fabric, a holding clip was applied. No adverse event occurred during the operation. The post-operative angiogram taken 21 days after surgery revealed angiographic vasospasm but there was no residual sac of the aneurysm. The patient was discharged on post-operative days 22 without focal neurological deficit except Terson’s syndrome (Fig. 3).
Illustrative example-patient 12 a brain CT b angiogram showing blister-like right ICA aneurysm (arrow). The aneurysm was obliterated by wrapping with cellulose fabric and a holding clip, c the post-operative angiogram taken 21 days after surgery revealed angiographic vasopasm but no residual sac of the aneurysm
Discussion
Pathogenesis
The histopathological characteristics of blister-like aneurysms revealed localised wall defects of the ICA due to atherosclerotic ulceration and penetration into the degenerated internal elastic lamina. As reported by Ishikawa et al. [3] the focal wall defects covered with clot and fibrous tissue and the walls of the aneurysm are composed of only adventitia. These lesions are not true aneurysms, because true berry aneurysms have thickened intima and adventitia in the wall [11]. Stehbens et al. [11] reported that early aneurysmal changes were accompanied by atherosclerotic changes in the parent vessels. Nakagawa et al. reported that aneurysms arising from the superior wall of the ICA were associated with atherosclerosis of the parent vessels [3, 6]. Some reports speculated that blister-like aneurysm of the superior wall of the ICA might be a result of arterial dissection [3, 6] However dissecting aneurysms show an intimal flap and a false lumen, which are not present in blister-like aneurysms. Therefore, the blister-like aneurysms have a different pathological structure to other aneurysms. Haemodynamic stress as well as atherosclerosis is now thought to be an important factor in the formation of a blister-like aneurysms, because the dorso-medial wall of the supraclinoid ICA is curved and the turbulence of blood flow impinges on the arterial wall [1, 6]. It has been noted that blister-like aneurysms tend to progress to a saccular appearance. Abe et al [1] speculated that a saccular lesion results from blood clot covering a focal wall defect. The blood clot organises and grows to become a saccular lesion, so the lesion has none of the normal arterial structures in its wall and is a false aneurysm.
Therapeutic options
Several treatment options including surgical and endovascular methods have been introduced for treatment of blister-like aneurysms. The surgical treatments such as clipping, wrapping, clipping on wrapping material are the mainstay of treatment, although the risk of rebleeding or intra-operative premature rupture are high due to the fragile aneurysmal wall. Endovascular treatment is also another treatment method available more recently.
Direct surgical clipping is still preferred by some authors. Parallel clipping of the ICA is recommended to avoid tearing of the aneurysmal neck [1, 6, 10]. However, direct clipping has lead to a poor outcomes according to many reports [1, 7]. According to Ogawa clipping with resultant ICA stenosis may also cause an undesirable outcome but wrapping only did not prevent rebleeding and was associated with a high incidence of postoperative bleeding and death [7]. Yanaka et al [13] reported successful treatment for repairing an aneurysmal tear at its base with suturing and an encircling clip. Unfortunately, in our series, one patient with an aneurysmal wall laceration at its base was treated only by suturing of the ICA, and died due to severe cerebral infarction.
Clipping to secure various wrapping materials (gauze, muscle, muscle fascia, cellulose fabric, Gore-Tex) after enveloping the entire circumference of the ICA has been observed to be effective in reinforcing the fragile blister-like aneurysms [6, 7]. The problems associated with this method are complications such as rebleeding, regrowth, risk of perforator injury, and difficulty in identifying the border of the wrapping [1, 7]. McNeely et al [5] reported a patient with SAH from a blister-like aneurysm treated by wrapping with gauze and intra-aneurysmal coil packing. Initial angiography on admission showed a shallow dilatation of the medial aspect of the distal right ICA. The blister-like aneurysm was treated by wrapping with gauze, but not in a circumferential manner because of a perforator. Repeat angiography showed significant growth of the saccular aneurysm. The lesion was treated by coil embolisation successfully. However, Deshmukh et al report on a series with long-term clinical and angiographic follow-up of 63 patients with unclippable wrapped or clip-wrapped intracranial aneurysms with a mean follow-up of 44.1 months indicating that the protection against regrowth or rebleeding of aneurysms was satisfactory [2]. In our series, 15 patients were treated by wrapping with cellulose fabric (Bemsheet®) and holding clipping, and none had post-operative rebleeding, although the follow-up period was short with a mean of only 17 months.
Tanoue et al. [12] also reported rapid growth of blister-like aneurysms into saccular configuration over a short period of time. Kim et al. [4] opine that all ICA dorsal wall aneurysms with configurational change are not false aneurysms. Aneurysms at the dorso-medial wall of ICA, which had grown into a saccular configuration from a previous suspicious tiny bulge, were treated surgically and confirmed to be true aneurysms by histopathological examination. They suspected that the initial blister-like bulge might have been the result of a partial occlusion and recanalisation by thrombus.
Endovascular ICA occlusion, with or without bypass surgery, is another treatment option for blister-like aneurysms[7]. This method is associated with the risk of graft occlusion and distal embolisation. Pelz et al [9] reported two patients with blister-like aneurysms successfully treated by combined endovascular and neurosurgical therapy. Having established that the patient tolerated trial occlusion of the cervical ICA for 30 min without an adverse effect, permanent balloon occlusion was completed. The subsequent angiogram showed continued filling of the aneurysm via a collateral supply, a second operation with surgical trapping of the aneurysm was performed with a permanent clip applied just proximal to the collateral artery followed by wrapping with muslin gauze was performed. The post-operative angiogram showed obliteration of the aneurysm. When the patient is unable to tolerate trial occlusion, trapping of the aneurysm with bypass surgery should be considered. In the recent report from Park et al., seven patients with BLICAA’s were treated with endovascular methods, but intra-aneurysmal coiling could not protect the patients from aneurysmal regrowth or rebleeding. The excellent outcomes were expected in patients who underwent ICA trapping after a balloon occlusion test and they concluded that endovascular ICA trapping is a convenient and safe method [8].
Conclusion
The surgeons should be aware of the high risk of premature rupture during dissection of BLICAA’s. Wrapping with cellulose fabric (Bemsheet®) along with the holding clipping technique could be chosen as the optimal surgical modality for prevention of rebleeding from these lesions.
References
Abe M, Tabuchi K, Yokoyama H, Uchino A (1998) Blood “blister”-like aneurysms of the internal carotid artery. J Neurosurg 89:419–424
Deshmukh VR, Kakarla UK, Figueiredo EG, Zabramski JM, Spetzler RF (2006) Long-term clinical and angiographic follow-up of unclippable wrapped intracranial aneurysms. Neurosurgery 58:434–442
Ishikawa T, Nakamura N, Houkin K, Nomura M (1997) Pathological consideration of a “blister-like” aneurysm at the superior wall of the internal carotid artery: case report. Neurosurgery 40:403–406
Kim JH, Kwon TH, Kim JH, Park YK, Chung HS (2006) Internal carotid artery dorsal wall aneurysm with configurational change: are they all false aneurysms? Surg Neurol 66:441–443
McNeely PD, Clarke DB, Baxter B, Vandorpe RA, Mendez I (2000) Endovascular treatment of a “blister-like” aneurysm of the internal carotid artery. Can J Neurol Sci 27:247–250
Nakagawa F, Kobayashi S, Takemae T, Sugita K (1986) Aneurysms protruding from the dorsal wall of the internal carotid artery. J Neurosurg 65:303–308
Ogawa A, Suzuki M, Ogasawara K (2000) Aneurysms at non-branching sites in the surpaclinoid portion of the internal carotid artery: internal carotid artery trunk aneurysms. Neurosurgery 47:578–586
Park JH, Park IS, Han DH, Kim SH, Oh CW, Kim JE, Kim HJ, Han MH, Kwon OK (2007) Endovascular treatment of blood “blister”-like aneurysms of the internal carotid artery. J Neurosurg 106:812–819
Pelz DM, Ferguson GG, Lownie SP, Kachur E (2003) Combined endovascular/neurosurgical therapy of blister-like distal internal carotid aneurysms. Can J Neurol Sci 30:49–53
Shigeta H, Kyoshima K, Nakagawa F, Kobayashi S (1992) Dorsal internal carotid artery aneurysms with special reference to angiographic presentation and surgical management. Acta Neurochir (Wien) 119:42–48
Stehbens WE (1989) Aetiology of intracranial berry aneurysms. J Neurosurg 70:823–831
Tanoue S, Kiyosue H, Matsumoto S, Yamashita M, Nagatomi H, Mori H (2004) Ruptured “blisterlike” aneurysm with a pseudo-aneurysm formation requiring delayed intervention with endovascular coil embolisation. Case report. J Neurosurg 101:159–162
Yanaka K, Meguro K, Nose T (2002) Repair of a tear at the base of a “blister”-like aneurysm with suturing and an encircling clip: technical note. Neurosurgery 50:218–221
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, JW., Choi, HG., Jung, JY. et al. Surgical strategies for ruptured blister-like aneurysms arising from the internal carotid artery: a clinical analysis of 18 consecutive patients. Acta Neurochir (Wien) 151, 125–130 (2009). https://doi.org/10.1007/s00701-008-0165-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-008-0165-5