Abstract
Purpose
To evaluate whether preoperative biopsy affects the outcomes of patients undergoing at least lobectomy for stage I lung adenocarcinoma.
Methods
We reviewed the medical records of patients who underwent surgery for stage I lung adenocarcinoma between 2006 and 2013. Tumor recurrence and survival were compared between patients who underwent preoperative biopsy, including computed tomographic-guided needle biopsy and transbronchial biopsy, and those who underwent intraoperative frozen section.
Results
Among 509 patients, 229 patients (44.9%) underwent preoperative biopsy and 280 patients had lung adenocarcinoma diagnosed by intraoperative frozen section (reference group). Recurrence developed in 65 (12.8%) patients within a median follow-up period of 54.4 months. Multivariate analysis demonstrated that preoperative biopsy (OR 1.97, p = 0.045), radiological solid appearance (OR 5.43, p < 0.001), and angiolymphatic invasion (OR 2.48, p = 0.010) were independent predictors of recurrence. In the overall cohort, preoperative biopsy appeared to worsen 5-year disease-free and overall survival significantly (76.6% vs. 93.0%, p < 0.001; and 83.8% vs. 94.5%, p = 0.002, respectively) compared with the reference group. After propensity matching, multivariable logistic regression still identified preoperative biopsy as an independent predictor of overall recurrence (OR 2.21, p = 0.048) after adjusting for tumor characteristics.
Conclusion
Preoperative biopsy might be considered a prognosticator of recurrence of stage I adenocarcinoma of the lungs in patients who undergo at least anatomic lobectomy without postoperative adjuvant chemotherapy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Preoperative computed-tomography-guided needle biopsy (CTGNB) for pulmonary lesions has become more popular with the availability of higher-resolution precise chest imaging techniques and fewer procedure-related complications [1, 2]. Tissue diagnosis through small-piece biopsies to confirm the pathological diagnosis of lung cancer is also important for deciding on the most appropriate treatment strategy, especially for patients with advanced non-small cell lung cancer (NSCLC). As therapy for NSCLC patients becomes more individualized, further tissue samples for molecular analysis, in addition to routine histopathological examinations, are being required to decide on the appropriate therapy strategy and for enrollment into clinical trials [3,4,5]. Although the same as preoperative small piece tissue biopsy, CTGNB generally provides more tissue, allowing for more detailed molecular analysis than trans-bronchoscopic biopsy (TBB) [6].
There is still controversy among surgeons about whether preoperative biopsy increases the possibility of recurrence, such as CTGNB in pleural seeding and other forms of recurrence [7], especially for tumors located peripherally, close to the visceral pleura [8]. Malignant implantation after CTGNB has also been reported by multiple investigators [7,8,9,10]. Consequently, it has been suggested that patients with a solitary pulmonary nodule who are good operative candidates and amenable to a potentially curative resection would benefit from direct surgical exploration without a preoperative percutaneous biopsy [8, 11]. Moreover, preoperative tissue diagnosis adds time, costs, and procedural risks, especially for early stage lung cancers, and may not be needed for treatment decisions or could even delay treatment. Therefore, direct surgical excision by minimally invasive video-assisted thoracic surgery (VATS) without preoperative tissue diagnosis remains one of the treatment strategies suggested by clinical guidelines if lung cancer is highly suspected based on clinical presentation [12]. Thus, it is still not established if preoperative biopsy before early-stage NSCLC resection promotes curative treatment. To clarify this issue, the present study evaluates the relationships between tumor recurrence of stage I lung adenocarcinoma and preoperative biopsy.
Patients and methods
Patient selection
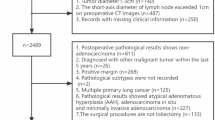
We reviewed the medical records of patients who underwent pulmonary resection for lung cancer between January, 2006 and December, 2013 from the prospective registered database at Taipei Veterans General Hospital. Clinical demographic characteristics such as age, sex, smoking history, pulmonary function, preoperative serum carcinoembryonic antigen (CEA) level (normal range: less than 5 ng/mL), histologic type of tumor, tumor size, presence of lymphovascular invasion, presence of pleural invasion, and methods of tissue proof for diagnosis were recorded for further analysis. Thoracic oncologic experts decided whether to perform preoperative biopsy or intraoperative wedge resection after evaluating the probability of malignancy and discussing with the patients the pros and cons of the different approaches. This study was approved by our hospital’s Institutional Review Board and informed consent was waived (approval no. 2016-03-009CC). During this period, there were 982 patients who underwent pulmonary resection for diagnosed pathological stage I NSCLC. To minimize the confounding bias of recurrence related to perioperative issues, this study excluded 145 sublobar resections, 5 R1 resections, 4 surgical deaths, 82 non-adenocarcinomas, and 237 patients who received postoperative adjuvant chemotherapy for high-risk factors, considering the possibility of disease recurrence [12]. Finally, 509 patients who underwent at least anatomic lobectomy without postoperative adjuvant chemotherapy for lung adenocarcinoma were included for further analysis. During the same period, 2097 patients underwent pulmonary resection based on evidence suggestive of lung cancer, 959 of whom had a preoperative biopsy done, which confirmed a diagnosis of lung cancer. Of the 1138 patients who underwent pulmonary resection without a preoperative definitive diagnosis, 287 had a final diagnosis of a benign pulmonary lesion (25.2%; Fig. 1).
Preoperative radiological evaluation
The radiologic finding of a tumor was defined by thin-section computed tomography (CT), which involved multidimensional slicing and reconstruction into axial, coronal, and sagittal views. Tumor characteristics from the preoperative chest CT were read by two independent observers blinded to the final pathological diagnosis and stage, and assigned to one of the following three groups based on axial CT imaging in a preoperative tumor shadow disappearance rate measurement (TDR) [13]: pure ground-glass nodule (GGN) type, defined as TDR of more than 80%; mixed type, defined as TDR of more than 20% but less than 80%; and solid-dominant type, defined as GGN components less than 20%. Subpleural location of the tumor was defined as a tumor in contact with the visceral pleural on preoperative CT imaging [8]. Discordance on any of the radiological criteria was recorded after a consensus was reached.
CT-guided percutaneous core needle biopsy
After localization, the puncture site was sterilized and draped. Local anesthesia (2% xylocaine) was injected and a 19G coaxial introducing needle was advanced toward the lesion under CT guidance through the chest wall. A 20G biopsy gun was used. The specimen, which usually comprised more than four strips of tissue core, was collected for cytology and pathology. Follow-up chest CT was immediately carried out to check whether there was hemothorax or pneumothorax. All the CTGNBs were performed by two specialized thoracic radiologists (C-K C, M-H W).
Transbronchial biopsy
Patients were given premedication of 2% lidocaine inhalation and local spraying with 10% lidocaine to inhibit the cough reflux. The biopsy forceps (FB-20C, Olympus) were advanced via the working channel of the bronchoscope (BF-260 or BF-P60, Olympus). Under fluoroscopy-guidance, the forceps were advanced further into the lesion, their cups were opened, and the biopsy was taken. Hemostasis was achieved with diluted epinephrine (1:1000) spraying when necessary. A minimum of four adequate specimens were collected for cytology and pathology.
Surgery
To eliminate the variation in the resected extension, only patients who underwent anatomic lobar resection were included in this study. Mediastinal evaluation included mediastinoscopy, intraoperative lymphadenectomy, or preoperative positron emission tomography (PET) scan. Patients underwent either radical mediastinal lymphadenectomy (the majority) or mediastinal node sampling, according to the surgeon’s preference. Adequate lymph node sampling was defined as removal of at least 15 lymph nodes and included three N2 stations [12]. PET scan was performed for 308 patients (60.5%), most of whom had a preoperative tissue diagnosis and were covered by Taiwan National Health Insurance.
Pathology examination
The pathologic stage was diagnosed using the seventh TNM system for lung cancer [14]. Visceral pleural invasion (VPI) was classified according to the proposal of IASLC [15]. VPI was examined first in tumor sections with hematoxylin and eosin staining. Elastic stains were performed in tumor sections when the status of VPI was indeterminable by hematoxylin and eosin staining [16]. PL1 is defined as a tumor that invades beyond the elastic layer and PL2 is defined as a tumor that extends to the visceral pleural space. PL1 and PL2 indicate VPI and are T2 descriptors. In the current study, pathologic PL0 was defined as being without VPI, whereas pathologic PL1 and PL2 were defined as being with VPI. Angiolymphatic invasion was defined as either vascular invasion or lymphatic permeation. Tumors were further classified according to the International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society (IASLC/ATS/ERS) classification [17] by two specialized thoracic pathologists (Y-C.Y, T-Y.C). Each tumor was reviewed using comprehensive histological subtyping, recording the percentage of each histological component in 5% increments. The predominant pattern was defined according to the most dominant pattern. For recurrence analysis, the tumors were further divided into low grade (lepidic/acinar/papillary predominant) and high grade (micropapillary/solid predominant) in a risk model proposed by Yoshizawa et al. [18].
Follow-up
Operative mortality included death from all causes within 30 days of surgery or beyond 30 days, but during the same hospitalization. Postoperative surveillance was scheduled every 3 months for the first 2 years, every 6 months for the third to fifth year, and then annually thereafter. Chest computed tomography scan was performed every 6 months for 2 years, and then annually. Local recurrence was defined as tumor recurrence in a contiguous anatomic site, including the ipsilateral hemithorax and mediastinum, after surgical resection. Distant recurrence was defined as tumor recurrence in the contralateral lung or outside the hemithorax and mediastinum after surgical resection. Local recurrence with pleural dissemination (LRPD) was defined as progressive increase in the growth of pleural nodules radiologically or malignant pleural effusion cytologically when recurrence had been confirmed initially. Recurrences were confirmed by tissue biopsy or diagnosed clinically by the multidisciplinary lung cancer committee. For patients with an enlarged solitary pulmonary nodule that developed after the first operation, CTGNB or surgical biopsy was performed for tissue proof if indicated, and comprehensive histological subtyping compared with original tumor was performed to distinguish metachronous metastasis. Patients with synchronous un-resected GGNs and metachronous tumors were excluded at the beginning of the study, to distinguish ipsilateral and contralateral recurrence [19]. Overall survival (OS) was defined as the interval between the date of surgical resection and the date of either death or last follow-up. Disease-free survival (DFS) was defined as the interval between the date of surgical resection and the date of first recurrence or the last date of follow-up. Observation was censored at the last follow-up when a patient was alive and recurrence-free or had died without recurrence. Except for 11 patients lost to follow-up, all patients were followed up until September 30, 2015 (follow-up rate 97.8%).
Statistical analysis
Statistical analysis was performed using the Statistical Package for the Social Sciences, version 17.0 (SPSS, Chicago, IL, USA). All continuous data are expressed as means and the standard deviation. Categorical variables were analyzed by the Chi-square test. Continuous variables were analyzed by the two-sample t test or the Mann–Whitney U test. Logistic regression analysis was performed for the predictors of overall tumor recurrence. Univariate predictors for the end point of recurrence with probability values less than 0.1 were selected for inclusion in the multivariate model. Odds ratios plus 95% confidence intervals (CI) are presented. Survival curves were calculated by the Kaplan–Meier method. Logrank tests were used to identify significance between groups (p < 0.05). Because non-random assignment can lead to selection bias and invalid estimates of survival, we applied Propensity Score Matching (PSM), which is the predicted probability of a subject’s preoperative biopsy approach based on basic characteristics such as gender, age, smoking history, CEA level, tumor size, tumor location, and preoperative radiology pattern, to reduce selection bias and make the two groups more similar. A multivariate logistic regression model was used to calculate the propensity score for each patient’s preoperative biopsy approach. Standardized differences were calculated for all pre-exposure variables used in matching. All data analysis was rechecked by the medical statistician/co-author (H-S.C).
Results
Clinicopathologic demographics of 509 patients
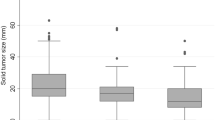
There were 234 men (46.0%) and 275 women (54.0%) included in the final analysis (Table 1). The median age was 62.0 years (range 26–87) and fewer than half of the patients were current or former smokers (31.4%). The mean preoperative serum CEA level was 3.26 ng/ml. According to the preoperative radiological pattern and tumor location, there were 153 (30.1%) patients in the pure GGN group, 181 (35.6%) in the mixed GGN group, and 175 (34.4%) in the solid pattern group; with 317 (62.3%) and 192 (37.7%) tumors assigned as non-subpleural and subpleural lesions, respectively. The median size of the resected tumors was 1.97 cm (range 0.5–5.0). The mean number of removed lymph nodes was 19.8 ± 9.1. The vast majority of tumors were diagnosed pathologically as invasive adenocarcinomas (91.9%) but included 41 tumors (8.1%) diagnosed as pre/minimally invasive adenocarcinomas. The pathological TNM stages were pT1a, pT1b, pT2a in 195 (38.3%), 79 (15.5%), and 235 (46.2%) patients, respectively. The most common pleural status of tumor invasion was PL0 (n = 289, 56.8%), followed by PL1 (n = 186, 36.5%) and PL2 (n = 34, 6.7%). The most common pathological diagnosis was moderate differentiated (n = 339, 66.6%) without angiolymphatic invasion (ALI, n = 441, 86.6%). Tumors with high grade (micropapillary/solid) predominate pattern were defined by comprehensive histological subtyping in 47 patients (9.2%). Pulmonary resection was performed by video-assisted thoracic surgery (VATS) in 328 patients (64.4%). A total of 308 patients (60.5%) underwent a preoperative whole-body positron emission tomography/computed tomography (PET/CT) scan to rule out mediastinal and distant metastasis.
Preoperative biopsy was performed in 229 patients (45.0%) as CTGNB in 183 and 46 TBB in 46. The other 280 patients (55.0%) who did not receive preoperative biopsy were assigned as the reference group. Most of the patients in the reference group underwent intraoperative wedge resection for frozen section to confirm malignancy first, followed by lobectomy. Only eight patients (2.9%) in the reference group underwent intraoperative lobectomy directly without initial wedge resection. Sputum cytology had identified NSCLC in four of these patients preoperatively and another four patients underwent intraoperative lobectomy directly due to the central location of the tumor and a higher probability of malignancy suspected clinically. The preoperative biopsy group comprised older patients, more tumors located close to the pleura, more radiologically solid tumors, larger tumors, more TNM pT2a stages, more pleural invasion, more VATS approaches, and more preoperative PET/CT scans than the reference group (Table 1).
Table 2 compares the recurrence patterns between the groups. Disease recurrence was identified in 65 (12.8%) patients during a median follow-up period of 54.4 months. The median recurrence times were 18.8, 31.5 and 25.7 months for the CTGNB, TBB, and reference groups, respectively (p = 0.038). According to the recurrence categories, 19 patients (3.7%) had local recurrence only, 11 (2.2%) had distant recurrence only, and 35 (6.9%) had local and distant recurrence. Local recurrence with pleural dissemination (LRPD) was diagnosed in 11 of these patients (2.2%).
Table 3 summarizes the analysis of prognostic factors for soverall recurrence. Preoperative biopsy (including CTGNB and TBB), older age, larger tumors, tumors located in the subpleural area, tumors with a radiological solid appearance, tumors with pleural invasion, poorly differentiated tumors, a tumor presentation of ALI, and a high grade of predominant pattern were significantly associated with an increased risk of overall recurrence. Multivariate analysis revealed that preoperative biopsy (odds ratio (OR) 1.97, p = 0.045), tumors with a radiological solid-appearance (OR 5.43, p < 0.001), and presentation of ALI (OR 2.48, p = 0.010) were the independent risk factors for overall recurrence after surgical resection of stage I lung adenocarcinomas. Although CTGNB and TBB were each significant factors for overall recurrence in univariate analysis, neither of these procedures achieved significance in multivariate analysis.
Survival analysis
There was a significant difference in disease-free (Fig. 2a) and overall (Fig. 2b) survival between the preoperative biopsy and reference groups (p = 0.002 and p < 0.001; Fig. 2). In Cox-regression analysis, preoperative biopsy (hazard ratio (HR) 2.160, p = 0.010), a radiographic solid appearance of the tumor (HR 4.445, p < 0.001), and tumor presentation of ALI (HR 2.186, p = 0.005) were independent predictors for worse disease-free survival (Supplemental Table 1). Preoperative biopsy was not an independent predictor for worse overall survival (data not shown). Because nonrandom assignment can lead to selection bias and invalid estimates of survival, we conducted further propensity score-matching (PSM) to reduce selection bias and make the two groups more similar. A multivariate logistic regression model was used to calculate the propensity score for each patient’s preoperative biopsy approach. PSM identified that further comparison was needed for 149 patients in each group and there was no statistical difference in any variable between the groups except in whether preoperative PET/CT scan was done (Table 4). After matching, multivariable logistic regression modeling still demonstrated that preoperative biopsy was an independent predictor of overall recurrence (OR 2.214, p = 0.048; 95% confidence interval 1.008–4.862; Table 5) and Cox-regression modeling still demonstrated that preoperative biopsy was an independent predictor for worse disease-free survival (Supplemental Table 2). Figure 2c, d shows the survival curves for DSF and OS after matching, respectively.
Discussion
Nonsurgical biopsy for tissue diagnosis is important in lung cancer treatment. Tissue-based diagnosis helps oncologists to identify the subtype of NSCLC and to do additional molecular testing to personalize medicine treatment, especially for advanced NSCLC [3]. To maximize the volume of tissue for histological subtyping and genotyping, biopsies are encouraged as long as the safety of the procedure can be guaranteed [20]. Nonetheless, preoperative biopsy remains controversial for early-stage NSCLC, for which the gold standard is lobectomy and lymph node dissection.
In clinical practice, unexpected pleural seeding is detected at thoracotomy or VATS in 3–6% of patients [21, 22], which is difficult to attribute to preoperative biopsy or the natural course of tumor growth. Furthermore, recurrence including pleural dissemination is common in patients with locally advanced lung cancer. The current study focused on patients with pathological instead of clinical stage I NSCLC or all stages to minimize the factors that may affect tumor recurrence after curative-intent pulmonary resection for early stage NSCLC. We also excluded patients with factors that could affect prognosis such as those who underwent sublobar resections, those who received postoperative adjuvant chemotherapy because of a high risk of disease recurrence [12], and those with a histopathologic diagnosis of NSCLC other than adenocarcinoma.
LRPD development after surgical resection of early stage NSCLC is rare, with an incidence of 2–9% according to our results and those of other studies, no matter what preoperative diagnostic modalities are used [8, 9, 23]. The low incidence of LRPD makes statistical analysis difficult. It is also evident that seeded cancer cells do not always generate pleural dissemination [10], as this probably requires several factors, such as adhesion, vascular generation and transformation. In the present study, the incidences of LRPD in the CTGNB, TBB, and reference groups were 4.9%, 2.2%, and 0.4%, respectively. Preoperative CTGNB worsened the incidence of LRPD significantly (p = 0.003) and was the only independent risk factor for LRPD (OR 6.379, p = 0.022) in the multivariate logistic regression analysis (Supplemental Table 3). A similar finding was noted in other surgical series [8, 9]. Conversely, Asakura and his colleagues reported no significant difference in the incidence of pleural recurrence after CTGNB or non-CTGNB in resected pathological stage I NSCLC in their series [23]. In their study, only 1 (0.8%) patient in the CTGNB group (124 patients), and 2 (1.0%) patients in the non-CTGNB group (197 patients) suffered pleural recurrence initially. A significantly smaller tumor size and fewer patients with microscopic pleural invasion (pT2a) in their CTGNB group than in the present study (16.1% vs. 56.8%) might contribute at least in part to the difference in their results from ours. In contrast, whether preoperative incisional biopsy or cutting needle biopsy increases recurrence did not show correlated results for other types of malignancy, such as breast cancer [24] and malignant melanoma [25].
Our study demonstrated that preoperative biopsy, tumors with radiological solid-appearance, and tumors with ALI were independent predictors of overall tumor recurrence. These three predictors also worsened the disease-free survival of patients with stage I adenocarcinoma significantly. Our results echo the recommendation of clinical guidelines [12]: “based on risk factors and radiologic appearance (solid-appearance), patients with a strong clinical suspicion of stage I or II lung cancer do not require biopsy before surgery”. Thus, preoperative biopsy on a radiological solid-appearance tumor may worsen the rate of tumor recurrence of resected stage I NSCLC. In this clinical scenario, surgical biopsy, such as thoracoscopic wedge resection, or intraoperative needle aspiration [26], is suggested when the probability of malignancy is high (> 65%) and a fully informed patient prefers to undergo a definitive diagnostic procedure [27]. In Taiwan, whole body PET CT is covered by National Health Insurance only after tissue diagnosis has confirmed lung cancer preoperatively to complete staging work-up. As a functional imaging modality to identify malignancy, whole body PET is also useful for identifying the possibility of mediastinal lymph node metastasis [28] and the degree of malignancy of NSCLC, which might affect the surgeons’ decision-making about extending parenchymal resection before the operation; for example, performing sublobar resection for a radiological GGN [29] vs. lobar resection for a tumor with solid appearance. Therefore, the time consumed includes the sequential of tissue proof, waiting for the pathology report, referral to specialists, and an appointment for whole body PET to complete tumor staging, usually delaying surgery for more than 2 months from the date of initial suspicion of malignancy of a pulmonary nodule. If we define “time-lag” as an interval between the tissue proofs to surgical intervention, the average “time-lag” in the preoperative biopsy group in our series was 20.4 days (2–90; median 18 day), vs. 0 (by the above definition) in the reference groups. Although the consequence of this delay in surgery on oncologic outcomes of lung cancer is controversial [30], it did increase anxiety in cancer patients. Most importantly, preoperative biopsy itself can complicate the preoperative workup, add further delays to treatment, and may not influence treatment decisions.
Preoperative biopsy can damage the basement membrane of tumors, which might increase metastasis through lymphatic or hematogenous dissemination [7]. Therefore, it is reasonable to avoid using this modality in patients with perioperative high-risk factors that might worsen this phenomenon. In the present study, preoperative biopsy was an independent predictor of overall tumor recurrence. Although the surgical results of the pre/minimal invasive adenocarcinoma presenting radiologically as pure GGN or partly solid GGN preoperatively were excellent [17, 31], there are no reports or recommendations that focus specifically on the relationship between preoperative biopsy (especially CTGNB) for pre/minimal invasive adenocarcinoma and the exacerbation of any form of tumor recurrence. As in previous studies, there was no tumor recurrence in 41 patients with pre/minimal invasive adenocarcinoma in this study, although 11 of them (26.8%) had preoperative CTGNB. A similarly excellent result was observed from the preoperative radiological appearance of chest CT in this study. No pattern of recurrence was seen in 153 patients with pure GGN diagnosed preoperatively, 36 (23.5%) of whom also underwent preoperative CTGNB. Therefore, with the increasing frequency of low-dose chest CT screening recommended for high risk NSCLC patients [32], CTGNB seems reasonable and safe if there is clinical and radiological suspection of “early” stage NSCLC, such as pure GGN. Some patients are hesitant to undergo surgical resection before a definitive diagnosis is obtained, to avoid so-called unnecessary thoracotomy/VATS or overdiagnosis. Patients who elect alternative treatment modalities often refuse or cannot tolerate surgery. Around 10–30% of pulmonary nodules resected were finally diagnosed as benign lesions. This incidence was relatively high compared with reports in the literature [33], but our study reflected true daily clinical practice and this may have been influenced by multiple factors. Importantly, we do not advocate that patients with a pulmonary lesion should undergo an operation directly without preoperative biopsy, but we do emphasize that the need for a tissue proof before surgery should be considered carefully based on the probability of malignancy according to clinical guidelines and clinical judgement.
The major limitations of this study were its retrospective design and the limited number of patients, especially the fact that there were only 65 patients with overall recurrence and 11 with LRPD. Another limitation was that different biopsy procedures such as CTGNB and TBB may influence surgical outcomes differently, but they were not propensity-matched individually because the incidence of events (recurrence) was exceedingly low, such as 11 for LRPD, which did not allow us to draw a statistical association. Nevertheless, the main strength is that we narrowed down our inclusion criteria and focused only on pathological stage I adenocarcinoma patients who underwent at least anatomic lobectomy resection without postoperative adjuvant chemotherapy. Our results highlight the risks of preoperative biopsy, and that it is unnecessary for a patient with strong clinical suspicion of early stage lung cancer. Early referral of this kind of patient to a sophisticated multidisciplinary lung cancer team that includes thoracic surgeons may provide the best personalized care. Moreover, there are still unmeasured confounders for prognosis such as pre-biopsy risk of lung cancer and/or competing diagnosis, and peripheral vs. central location, which may lead to residual confounding and limit the interpretation of results. Therefore, we performed propensity score matching to minimize differences in demographic and clinical characteristics between preoperative biopsy and intraoperative resection. Although there were no significant differences between pre-exposure variables except in the patients who had a preoperative PET scan, possible selection bias cannot be excluded even after propensity score matching.
Conclusions
Preoperative biopsy was significantly associated with overall tumor recurrence among the variables in our study for stage I adenocarcinoma of lung patients who underwent at least anatomic lobectomy without postoperative adjuvant chemotherapy. To avoid tumor recurrence of early stage lung cancer, the need for tissue proof before surgery should be considered carefully, especially for the tumors with a radiological solid appearance. Because of the retrospective nature of the current study and the relatively small number of tumor recurrences and LRPD, a further prospective study should be done to evaluate the survival benefit of preoperative biopsy for early stage NSCLC patients.
Abbreviations
- CTGNB:
-
Computed tomographic-guided needle biopsy
- TBB:
-
Trans-bronchial biopsy
- ALI:
-
Angiolymphatic invasion
- LRPD:
-
Local recurrence with pleural disseminations
- OR:
-
Odds ratio
- HR:
-
Hazard ratio
- DFS:
-
Disease-free survival
- NSCLC:
-
Non-small cell lung cancer
- VATS:
-
Video-assisted thoracic surgery
- CEA:
-
Carcinoembryonic antigen
- TDR:
-
Tumor shadow disappearance rate
- GGN:
-
Pure ground glass nodule
- PET:
-
Positron emission tomography
- VPI:
-
Visceral pleural invasion
- IASLC:
-
International association for the study of lung cancer
References
Wu CC, Maher MM, Shepard JA. Complications of ct-guided percutaneous needle biopsy of the chest: Prevention and management. AJR Am J Roentgenol. 2011;196:W678–W682682.
Choo JY, Park CM, Lee NK, Lee SM, Lee HJ, Goo JM. Percutaneous transthoracic needle biopsy of small (≤ 1 cm) lung nodules under c-arm cone-beam CT virtual navigation guidance. Eur Radiol. 2013;23:712–9.
Tam AL, Kim ES, Lee JJ, Ensor JE, Hicks ME, Tang X, et al. Feasibility of image-guided transthoracic core-needle biopsy in the battle lung trial. J Thorac Oncol. 2013;8:436–42.
Kohman LJ, Gu L, Altorki N, Scalzetti E, Veit LJ, Wallen JM, et al. Biopsy first: lessons learned from cancer and leukemia group b (CALGB) 140503. J Thorac Cardiovasc Surg. 2017;153:1592–7.
Huang KY, Ko PZ, Yao CW, Hsu CN, Fang HY, Tu CY, et al. Inaccuracy of lung adenocarcino***ma subtyping using preoperative biopsy specimens. J Thorac Cardiovasc Surg. 2017;154:332 9 e1.
Ofiara LM, Navasakulpong A, Ezer N, Gonzalez AV. The importance of a satisfactory biopsy for the diagnosis of lung cancer in the era of personalized treatment. Curr Oncol. 2012;19:S16–S23.
Nakajima J. Preoperative pathological diagnosis of lung cancer: Is it always necessary? Ann Thorac Cardiovasc Surg. 2012;18:183–5.
Inoue M, Honda O, Tomiyama N, Minami M, Sawabata N, Kadota Y, et al. Risk of pleural recurrence after computed tomographic-guided percutaneous needle biopsy in stage I lung cancer patients. Ann Thorac Surg. 2011;91:1066–71.
Matsuguma H, Nakahara R, Kondo T, Kamiyama Y, Mori K, Yokoi K. Risk of pleural recurrence after needle biopsy in patients with resected early stage lung cancer. Ann Thorac Surg. 2005;80:2026–31.
Sawabata N, Ohta M, Maeda H. Fine-needle aspiration cytologic technique for lung cancer has a high potential of malignant cell spread through the tract. Chest. 2000;118:936–9.
Kara M, Alver G, Sak SD, Kavukcu S. Implantation metastasis caused by fine needle aspiration biopsy following curative resection of stage IB non-small cell lung cancer. Eur J Cardiothorac Surg. 2001;20:868–70.
NCCN. NCCN guidelines version 3 2018, non-small cell lung cancer; 2018. https://www.nccn.org/professinals/physician_fls/f_guidelinesasp#nscl.
Takamochi K, Nagai K, Yoshida J, Suzuki K, Ohde Y, Nishimura M, et al. Pathologic N0 status in pulmonary adenocarcinoma is predictable by combining serum carcinoembryonic antigen level and computed tomographic findings. J Thorac Cardiovasc Surg. 2001;122:325–30.
Edge SB, Compton CC. The American joint committee on cancer: the 7th of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010;17:1471–4.
Travis WD, Brambilla E, Rami-Porta R, Vallieres E, Tsuboi M, Rusch V, et al. Visceral pleural invasion: pathologic criteria and use of elastic stains: proposal for the 7th of the TNM classification for lung cancer. J Thorac Oncol. 2008;3:1384–90.
Hung JJ, Jeng WJ, Hsu WH, Chou TY, Lin SF, Wu YC. Prognostic significance of the extent of visceral pleural invasion in completely resected node-negative non-small cell lung cancer. Chest. 2012;142:141–50.
Travis WD, Brambilla E, Noguchi M, Nicholson AG, Geisinger KR, Yatabe Y, et al. International association for the study of lung cancer/American Thoracic Society/European Respiratory Society international multidisciplinary classification of lung adenocarcinoma. J Thorac Oncol. 2011;6:244–85.
Yoshizawa A, Motoi N, Riely GJ, Sima CS, Gerald WL, Kris MG, et al. Impact of proposed IASLC/ATS/ERS classification of lung adenocarcinoma: prognostic subgroups and implications for further revision of staging based on analysis of 514 stage I cases. Mod Pathol. 2011;24:653–64.
Yu YC, Hsu PK, Yeh YC, Huang CS, Hsieh CC, Chou TY, et al. Surgical results of synchronous multiple primary lung cancers: similar to the stage-matched solitary primary lung cancers? Ann Thorac Surg. 2013;96:1966–74.
Dietel M, Bubendorf L, Dingemans AM, Dooms C, Elmberger G, Garcia RC, et al. Diagnostic procedures for non-small-cell lung cancer (NSCLC): recommendations of the European Expert Group. Thorax. 2016;71:177–84.
Iida T, Shiba M, Yoshino I, Miyaoka E, Asamura H, Date H, et al. Surgical intervention for non-small-cell lung cancer patients with pleural carcinomatosis: results from the Japanese Lung Cancer Registry in 2004. J Thorac Oncol. 2015;10:1076–82.
Okamoto T, Iwata T, Mizobuchi T, Hoshino H, Moriya Y, Yoshida S, et al. Pulmonary resection for lung cancer with malignant pleural disease first detected at thoracotomy. Eur J Cardiothorac Surg. 2012;41:25–30.
Asakura K, Izumi Y, Yamauchi Y, Nakatsuka S, Inoue M, Yashiro H, et al. Incidence of pleural recurrence after computed tomography-guided needle biopsy in stage I lung cancer. PLoS ONE. 2012;7:e42043.
Peters-Engl C, Konstantiniuk P, Tausch C, Haid A, Hoffmann B, Jagoutz-Herzlinger M, et al. The impact of preoperative breast biopsy on the risk of sentinel lymph node metastases: analysis of 2502 cases from the Austrian Sentinel Node Biopsy Study Group. Br J Cancer. 2004;91:1782–6.
Martin RC 2nd, Scoggins CR, Ross MI, Reintgen DS, Noyes RD, Edwards MJ, McMasters KM. Is incisional biopsy of melanoma harmful? Am J Surg. 2005;190:913–7.
Matsuoka T, Sonobe M, Date H. Intraoperative fine-needle aspiration biopsy (FNA) for lung cancer: diagnostic value and risk of pleural dissemination. Surg Today. 2015;45:695–9.
Gould MK, Donington J, Lynch WR, Mazzone PJ, Midthun DE, Naidich DP, et al. Evaluation of individuals with pulmonary nodules: when is it lung cancer? Diagnosis and management of lung cancer, 3rd ed: American college of chest physicians evidence-based clinical practice guidelines. Chest. 2013;143:e93S–e120S.
Broderick SR, Meyers BF. Pet staging of mediastinal lymph nodes in thoracic oncology. Thorac Surg Clin. 2012;22:161–6.
Tsutani Y, Miyata Y, Nakayama H, Okumura S, Adachi S, Yoshimura M, et al. Prediction of pathologic node-negative clinical stage Ia lung adenocarcinoma for optimal candidates undergoing sublobar resection. J Thorac Cardiovasc Surg. 2012;144:1365–71.
Quarterman RL, McMillan A, Ratcliffe MB, Block MI. Effect of preoperative delay on prognosis for patients with early stage non-small cell lung cancer. J Thorac Cardiovasc Surg. 2003;125:108–13 (discussion 13–4).
Yanagawa N, Shiono S, Abiko M, Ogata SY, Sato T, Tamura G. New IASLC/ATS/ERS classification and invasive tumor size are predictive of disease recurrence in stage I lung adenocarcinoma. J Thorac Oncol. 2013;8:612–8.
National Lung Screening Trial Research Trial, Aberle DR, Adams AM, Berg CD, Black WC, Clapp JD, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365:395–409.
Grogan EL, Weinstein JJ, Deppen SA, Putnam JB Jr, Nesbitt JC, Lambright ES, et al. Thoracic operations for pulmonary nodules are frequently not futile in patients with benign disease. J Thorac Oncol. 2011;6:1720–5.
Funding
Taipei Veterans General Hospital-National Yang-Ming University Excellent Physician Scientists Cultivation Program, No. 105-V-B-035.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Huang, CS., Hsu, PK., Chen, CK. et al. Preoperative biopsy and tumor recurrence of stage I adenocarcinoma of the lung. Surg Today 50, 673–684 (2020). https://doi.org/10.1007/s00595-019-01941-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-019-01941-3