Abstract
Purpose
Inflammatory biomarkers such as the neutrophil-to-lymphocyte ratio (NLR), lymphocyte-to-monocyte ratio (LMR), and platelet-to-lymphocyte ratio (PLR) are reportedly predictive of the long-term outcomes of several cancers. We evaluated their correlations with the post-surgical long-term outcomes of patients with mass-forming (MF) intrahepatic cholangiocarcinoma (ICC).
Methods
The subjects of this study were 52 patients who underwent hepatic resection for MF-ICC at our hospital. We measured the cutoff values of NLR, LMR and PLR, using receiver operating characteristic curves, and compared the survival rates of patients with high vs. those with low values. We also evaluated a prognostic scoring system based on significant inflammatory biomarkers.
Results
The cutoff values for NLR, LMR, and PLR were 1.93, 4.78, and 98, respectively. The high-NLR and low-LMR groups had significantly worse prognoses than the low-NLR and high-LMR groups. We designed a scoring system using the inflammation score (IS) based on NLR and LMR values, stratifying patients into three groups with scores of 0, 1, or 2. The IS was significantly correlated with overall survival (OS), with 5-year survival rates by the IS score of 100% for 0, 61% for 1, and 32% for 2 (P = 0.011). The IS was found to be an independent predictor of OS in multivariate analysis.
Conclusions
Our IS scoring system may predict long-term outcomes after surgery for MF-ICC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intrahepatic cholangiocarcinoma (ICC) is the second most common primary liver cancer after hepatocellular carcinoma (HCC) and is treated with surgical resection when possible [1,2,3]. However, recurrence rates after ICC surgery are high and survival is poor, with 5-year recurrence-free survival and 5-year overall survival (OS) rates ranging from 2 to 39% and 5–56%, respectively [4].
Inflammatory biomarkers, such as the neutrophil-to-lymphocyte ratio (NLR), lymphocyte-to-monocyte ratio (LMR), and platelet-to-lymphocyte ratio (PLR), have been studied widely as prognostic markers for long-term outcomes of several cancers [5,6,7]. These biomarkers are also reported to be important predictors of long-term outcome after ICC surgery [8,9,10]. However, these studies rarely consider the macroscopic types of ICC, which are thought to have different prognoses after surgery, according to their type [11,12,13,14,15,16,17].
We examined the correlations between inflammatory biomarkers and the long-term outcomes of patients who underwent surgery for the mass-forming (MF) subtype of ICC. Our cohort was limited to patients with MF-ICC to reduce the heterogeneity related to different macroscopic types, and because MF is reported to be the predominant ICC subtype [18, 19]. We also evaluated a new scoring system that we devised for comprehensive inflammatory status based on plural inflammatory biomarkers.
Methods
Patients
Patients who underwent hepatic resections for ICC at our hospital between May, 1998 and May, 2017 were eligible for this study. We excluded patients who had received preoperative therapy, such as radiotherapy or chemotherapy; those who had another malignant disease; those who underwent bile-duct reconstructions; those who died of postoperative complications within 30 days after surgery; those who underwent non-curative resections; and those with combined hepatocellular-cholangiocarcinoma. This study was approved by the institutional review board of the Graduate School of Medical Sciences, Kyushu University (No. 30-578). All study participants were given the opportunity to opt out.
Surgical procedure and postoperative follow-up strategy
The details of our surgical techniques and patient follow-up procedures for ICC have been reported previously [14, 20, 21]. Basically, anatomical hepatic resection was performed for patients with adequate postoperative remnant liver volume and function. For patients with cirrhosis, or those who appeared unlikely to have adequate liver volume after surgery, parenchymal-sparing hepatectomy was selected. Lymphadenectomy around the hepatoduodenal ligament was performed for patients whose preoperative imaging studies and intraoperative findings indicated possible lymph node metastasis.
After discharge, all patients underwent regular screening for recurrence with ultrasonography and measurement of tumor markers such as CEA and CA19-9. Computerized tomography (CT) scanning was also performed every 6 months. If recurrence was suspected, additional imaging studies such as magnetic resonance imaging (MRI) were performed. When ICC recurrence was confirmed by imaging studies, patients underwent additional hepatectomy or systemic chemotherapy, according to the size, site, and number of tumors, and the patients’ general condition.
The administration of postoperative adjuvant chemotherapy in this setting was decided by the physician because of the lack of consensus on the benefit of adjuvant chemotherapy for ICC [22]. Physicians decided on the appropriateness of adjuvant chemotherapy by considering pathological findings and the patient’s general condition. Gemcitabine hydrochloride was used in the regimen.
Inflammatory biomarkers
Data on inflammatory biomarkers, including NLR, LMR, and PLR, were obtained from preoperative complete blood counts (CBC). NLR, LMR, and PLR were calculated as the absolute counts of neutrophils, lymphocytes, and platelets, divided by the absolute counts of lymphocytes, monocytes, and lymphocytes, respectively. We used preoperative CBC data from when patients had no sign of infection. Cutoff values of these markers were measured using receiver operating characteristics (ROC) curves. As a comprehensive evaluation of inflammatory status, we assessed a scoring system using inflammatory biomarkers that were significantly correlated with long-term outcomes.
Outcomes and statistical analysis
Patient data, including clinical characteristics, laboratory data, operative findings, pathological findings, and survival data, were obtained from a prospectively maintained institutional database. Tumor stages were assessed according to the American Joint Committee on Cancer (AJCC) classification system, 8th edition. Active hepatitis B or C were defined as seropositivity for hepatitis B surface antigen or hepatitis C antibody, respectively. Alcoholic hepatitis and non-alcoholic steatohepatitis were defined, taking into consideration the patients’ social history and pathological findings of non-cancerous parts of the surgical specimens. If the non-cancerous surgical sample showed F4-stage fibrosis, the patient was deemed as having cirrhosis.
Patients were divided into high- and low-value groups for each inflammatory biomarker. The characteristics and survival rates of the high and low value groups were compared.
Statistical analysis
Statistical analyses were performed using the Wilcoxon rank-sum test for examining differences in continuous variable distributions, and Fisher’s exact test for categorical variables. Survival curves were analyzed using the Kaplan–Meier method and compared using the log-rank test. We used the inflammatory biomarkers that were significantly associated with survival rates to calculate the score to evaluate the patients’ comprehensive inflammation conditions. The score was designated as the inflammation score (IS). The usefulness of the IS was assessed using the Kaplan–Meier method and log-rank test.
The Cox proportional hazards model was used for univariate and multivariate survival analyses. Factors, including IS, that were significantly associated with survival rates in univariate analyses, were included in the multivariate analyses to assess their independence. P < 0.05 was considered significant. All of the analyses were conducted using JMP software (SAS Institute, Cary, NC).
Results
Sample size and inflammatory biomarker values classified by macroscopic types
We identified 52 patients with MF-ICC, 7 with MF + periductal infiltrating (PI)-ICC, 4 with PI-ICC, and 1 with intraductal growth (IG)-ICC, who met our inclusion criteria. Figure 1 is a flowchart of patient inclusion and exclusion criteria and Table 1 summarizes the mean values of inflammatory biomarkers by macroscopic type. In this study, we analyzed only patients with MF-ICC.
Patient characteristics and inflammatory biomarker cutoff values
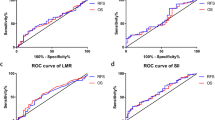
We based our ROC curves on mortality 5 years after surgery (Fig. 2). The cutoff values of inflammatory biomarkers were 1.93 for NLR, 4.78 for LMR, and 98 for PLR. Tables 2, 3 and 4 summarize the patients’ clinicopathological characteristics in the high and low value groups for each of these inflammatory biomarkers, respectively. Cirrhosis was significantly associated with NLR and PLR, tumor size with NLR, and AJCC stage with LMR, but no other factors showed significant associations.
Overall survival
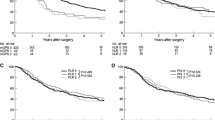
Figure 3 shows the OS rates in relation to each inflammatory biomarker. The 5-year OS rates were 83% for the low-NLR group vs. 42% for the high-NLR group (P = 0.031); 81% for the high-LMR group vs. 37% for the low-LMR group (P < 0.01); and 57% for the low-PLR group vs. 51% for the high-PLR group (P = 0.84).
Disease-free survival
The low LMR group had significantly worse disease-free survival (DFS) than the high LMR group. Although we assumed that the high NLR group would have worse DFS than the low NLR group, there was no significant difference between them. The 5-year DFS rates in the low-NLR and high-NLR groups were 56% and 34%, respectively (P = 0.23), and those in high-LMR and low-LMR groups were 58% and 30%, respectively (P = 0.014). The DFS in the high- and low-value PLR groups did not differ significantly (Fig. 4).
Comprehensive evaluation of inflammatory biomarkers
As NLR and LMR were significantly associated with the OS of ICC patients, we designed an inflammation score (IS) system that allotted one point each to patients with high NLR or low LMR, and two points for both, thus stratifying patients into three groups by scores 0, 1, or 2. The 5-year OS of the patients differed significantly according to their IS, being 100% for 0, 61% for 1, and 32% for 2 (P = 0.011; Fig. 5). The 5-year DFS rates were not significantly different (P = 0.078; Fig. 6).
Predictive factors for OS
Tables 5 and 6 show the univariate and multivariate analyses. The cut-off values for absolute neutrophil and lymphocyte counts were calculated using ROC curves based on mortality 5 years after surgery. In the univariate analysis, tumor size > 50 mm, AJCC classification stage III/IV, NLR, LMR, and IS were risk factors for shorter OS. In the multivariate analysis, we did not include all inflammatory biomarkers in the same analysis because of the multicollinearity problem, but included a single inflammatory biomarker in each analysis. For the same reason, we included only the AJCC classification stage, except for tumor size, in the analyses. As prognostic factors, NLR, LMR, and IS were independent from the AJCC classification stage.
Discussion
We found that NLR and LMR were significantly associated with the long-term outcomes of patients with MF-ICC. Moreover, the scoring system based on NLR and LMR was a possible prognostic factor for the long-term outcome of these patients. This implies a synergistic effect of NLR and LMR on long-term outcome, even though they include a common factor, the lymphocyte count, and are both indicators of inflammatory status in a host. Therefore, to identify high-risk patients, we should consider both of these inflammatory biomarkers. Although various assessment methods combine NLR and LMR, our simple method to calculate IS can distinguish patients according to their prognoses and it is easy to use in clinical practice.
It has been suggested that tumor-infiltrating lymphocytes (TILs) are antitumor effector cells associated with better long-term outcomes for HCC [23]. In our preliminary study, the ratio of lymphocytes among peripheral white blood cells was correlated with a better prognosis (data not shown), and this might reflect the effect of TILs in the tumor microenvironment (TME). In the TME, neutrophils work as tumor-associated neutrophils (TANs) [24]. Furthermore, tumor-associated macrophages (TAMs), which originate from peripheral macrophages, are also an important component of the TME [25]. TANs and TAMs have similar effects on tumor progression, such as tumor growth, extracellular matrix remodeling, angiogenesis, and immunosuppression, but they have some differences in signaling pathways [25]. These differences may have clinical implications, according to the results of our study. In our previous study, the ratio of CD3+ and CD68+ cells in HCC sections (as shown by immunohistochemical analysis) were significantly associated with LMR values [26]. This is a rationale for the relationship between peripheral blood cell analysis and inflammation and immune status in the TME.
We found that NLR did not have a significant impact on DFS after surgery for MF-ICC. This negative result, especially considering the appearance of the Kaplan–Meier curve, may be due to the small sample size, which is this study’s main limitation. Although a previous report showed PLR to be significantly associated with the long-term outcomes of ICC patients, this study did not find PLR to be a significant predictor of the long-term outcomes of MF-ICC patients [9]. Our study included only patients with MF-ICC, which is reportedly relevant to hepatitis and liver cirrhosis [11, 12, 27, 28]. In our cohort, 56% of the patients had hepatitis (hepatitis B, hepatitis C, alcoholic hepatitis, and non-alcoholic steatohepatitis) and 13% had cirrhosis. Notably, the low PLR group tended to have a high prevalence of hepatitis, at 68% vs. 44% in the high-PLR group (P = 0.10) and a significantly high prevalence of cirrhosis of 28% vs. 0% in the high-PLR group (P = 0.0036). These factors may have affected the platelet counts and our results.
There were several limitations to this study. First, it was a retrospective analysis from a single center. Second, because we limited the subjects to only patients with MF-ICC without bile duct reconstruction, we had a small sample size. As patients with bile duct reconstruction may include those with hilar cholangiocarcinoma, we excluded them to eliminate possible unfavorable variability. We analyzed only MF type, but not PI type, IG type, and MF + PI type, because the latter three types are relatively rare and we were not able to collect an adequate number of cases to conduct valid analyses. The intention of this limitation was to curb the heterogeneity due to different macroscopic types. A previous report revealed that NLR and LMR had a significant impact on ICC, and a similar result was found in our study [10]. However, the previous study did not consider the differences in macroscopic types. Our study shows that inflammatory biomarkers affect MF-ICC significantly, but they may affect other macroscopic ICC types differently. As PI-ICC tended to have higher levels of PLR than MF-ICC, the usefulness of PLR may differ between MF-ICC and PI-ICC. Third, other factors, such as cirrhosis in NLR and PLR, tumor size in NLR, and AJCC classification stage in LMR, were uneven between the high and low value groups, which reflect this study’s retrospective design. Therefore, a larger-scale, multi-center prospective study is necessary to strengthen the statistical validity and power.
We used cutoff values derived from ROC curves. Similar previous reports on cholangiocarcinoma that used ROC curves to calculate cutoff values also had values for NLR [8, 10, 29] and LMR [10, 30, 31] that were consistent with ours, but the cutoff value for PLR in our study was lower [9, 32]. A possible reason for the low PLR cutoff value was that the ROC AUC was small for PLR and the cutoff value for optimal sensitivity and specificity can be unstable. A larger-scale study is needed to establish the optimal cutoff value for each parameter and to validate their wider applicability.
In conclusion, the findings of this study show that our scoring system based on inflammatory biomarkers could be useful for predicting the long-term outcomes after surgery for ICC. Moreover, as its predictive value is independent of tumor stage, it may be helpful for identifying high-risk patients.
References
Ikai I, Arii S, Okazaki M, Okita K, Omata M, Kojiro M, et al. Report of the 17th nationwide follow-up survey of primary liver cancer in Japan. Hepatol Res. 2007;37(9):676–91.
Aljiffry M, Abdulelah A, Walsh M, Peltekian K, Alwayn I, Molinari M. Evidence-based approach to cholangiocarcinoma: a systematic review of the current literature. J Am Coll Surg. 2009;208(1):134–47.
Bridgewater J, Galle PR, Khan SA, Llovet JM, Park JW, Patel T, et al. Guidelines for the diagnosis and management of intrahepatic cholangiocarcinoma. J Hepatol. 2014;60(6):1268–89.
Mavros MN, Economopoulos KP, Alexiou VG, Pawlik TM. Treatment and prognosis for patients with intrahepatic cholangiocarcinoma: systematic review and meta-analysis. JAMA Surg. 2014;149(6):565–74.
Sharaiha RZ, Halazun KJ, Mirza F, Port JL, Lee PC, Neugut AI, et al. Elevated preoperative neutrophil:lymphocyte ratio as a predictor of postoperative disease recurrence in esophageal cancer. Ann Surg Oncol. 2011;18(12):3362–9.
Chan JC, Chan DL, Diakos CI, Engel A, Pavlakis N, Gill A, et al. The lymphocyte-to-monocyte ratio is a superior predictor of overall survival in comparison to established biomarkers of resectable colorectal cancer. Ann Surg. 2017;265(3):539–46.
Mano Y, Shirabe K, Yamashita Y, Harimoto N, Tsujita E, Takeishi K, et al. Preoperative neutrophil-to-lymphocyte ratio is a predictor of survival after hepatectomy for hepatocellular carcinoma: a retrospective analysis. Ann Surg. 2013;258(2):301–5.
Lin G, Liu Y, Li S, Mao Y, Wang J, Shuang Z, et al. Elevated neutrophil-to-lymphocyte ratio is an independent poor prognostic factor in patients with intrahepatic cholangiocarcinoma. Oncotarget. 2016;7(32):50963–71.
Chen Q, Dai Z, Yin D, Yang LX, Wang Z, Xiao YS, et al. Negative impact of preoperative platelet-lymphocyte ratio on outcome after hepatic resection for intrahepatic cholangiocarcinoma. Medicine (Baltimore). 2015;94(13):e574.
Wu Y, Ren F, Chai Y, Xue Z, Shen C, Zhang X, et al. Prognostic value of inflammation-based indexes for intrahepatic cholangiocarcinoma following curative resection. Oncol Lett. 2019;17(1):165–74.
Yamamoto M, Ariizumi S, Otsubo T, Katsuragawa H, Katagiri S, Nakano M, et al. Intrahepatic cholangiocarcinoma diagnosed preoperatively as hepatocellular carcinoma. J Surg Oncol. 2004;87(2):80–3.
Aishima S, Kuroda Y, Nishihara Y, Iguchi T, Taguchi K, Taketomi A, et al. Proposal of progression model for intrahepatic cholangiocarcinoma: clinicopathologic differences between hilar type and peripheral type. Am J Surg Pathol. 2007;31(7):1059–67.
Guglielmi A, Ruzzenente A, Campagnaro T, Pachera S, Valdegamberi A, Nicoli P, et al. Intrahepatic cholangiocarcinoma: prognostic factors after surgical resection. World J Surg. 2009;33(6):1247–54.
Uchiyama K, Yamamoto M, Yamaue H, Ariizumi S, Aoki T, Kokudo N, et al. Impact of nodal involvement on surgical outcomes of intrahepatic cholangiocarcinoma: a multicenter analysis by the Study Group for Hepatic Surgery of the Japanese Society of hepato-biliary-pancreatic surgery. J Hepatobiliary Pancreat Sci. 2011;18(3):443–52.
Yamamoto M, Takasaki K, Yoshikawa T, Ueno K, Nakano M. Does gross appearance indicate prognosis in intrahepatic cholangiocarcinoma? J Surg Oncol. 1998;69(3):162–7.
Morimoto Y, Tanaka Y, Ito T, Nakahara M, Nakaba H, Nishida T, et al. Long-term survival and prognostic factors in the surgical treatment for intrahepatic cholangiocarcinoma. J Hepatobiliary Pancreat Surg. 2003;10(6):432–40.
Shimada K, Sano T, Sakamoto Y, Esaki M, Kosuge T, Ojima H. Surgical outcomes of the mass-forming plus periductal infiltrating types of intrahepatic cholangiocarcinoma: a comparative study with the typical mass-forming type of intrahepatic cholangiocarcinoma. World J Surg. 2007;31(10):2016–22.
Meng ZW, Pan W, Hong HJ, Chen JZ, Chen YL. Macroscopic types of intrahepatic cholangiocarcinoma and the eighth edition of AJCC/UICC TNM staging system. Oncotarget. 2017;8(60):101165–74.
Sakamoto Y, Kokudo N, Matsuyama Y, Sakamoto M, Izumi N, Kadoya M, et al. Proposal of a new staging system for intrahepatic cholangiocarcinoma: analysis of surgical patients from a nationwide survey of the Liver Cancer Study Group of Japan. Cancer. 2016;122(1):61–70.
Shimada M, Yamashita Y, Aishima S, Shirabe K, Takenaka K, Sugimachi K. Value of lymph node dissection during resection of intrahepatic cholangiocarcinoma. Br J Surg. 2001;88(11):1463–6.
Yamashita Y, Taketomi A, Morita K, Fukuhara T, Ueda S, Sanefuji K, et al. The impact of surgical treatment and poor prognostic factors for patients with intrahepatic cholangiocarcinoma: retrospective analysis of 60 patients. Anticancer Res. 2008;28(4C):2353–9.
Reames BN, Bagante F, Ejaz A, Spolverato G, Ruzzenente A, Weiss M, et al. Impact of adjuvant chemotherapy on survival in patients with intrahepatic cholangiocarcinoma: a multi-institutional analysis. HPB (Oxford). 2017;19(10):901–9.
Yao W, He JC, Yang Y, Wang JM, Qian YW, Yang T, et al. The prognostic value of tumor-infiltrating lymphocytes in hepatocellular carcinoma: a systematic review and meta-analysis. Sci Rep. 2017;7(1):7525.
Fridlender ZG, Sun J, Kim S, Kapoor V, Cheng G, Ling L, et al. Polarization of tumor-associated neutrophil phenotype by TGF-beta: "N1" versus "N2" TAN. Cancer Cell. 2009;16(3):183–94.
Galdiero MR, Bonavita E, Barajon I, Garlanda C, Mantovani A, Jaillon S. Tumor associated macrophages and neutrophils in cancer. Immunobiology. 2013;218(11):1402–10.
Mano Y, Yoshizumi T, Yugawa K, Ohira M, Motomura T, Toshima T, et al. Lymphocyte-to-monocyte ratio is a predictor of survival after liver transplantation for hepatocellular carcinoma. Liver Transpl. 2018;24(11):1603–11.
Zhang XF, Chakedis J, Bagante F, Beal EW, Lv Y, Weiss M, et al. Implications of intrahepatic cholangiocarcinoma etiology on recurrence and prognosis after curative-intent resection: a multi-institutional study. World J Surg. 2018;42(3):849–57.
Yamamoto M, Takasaki K, Nakano M, Saito A. Minute nodular intrahepatic cholangiocarcinoma. Cancer. 1998;82(11):2145–9.
Kumamoto Y, Kaizu T, Tajima H, Nishizawa N, Ei S, Igarashi K, et al. Neutrophil-to-lymphocyte ratio as a predictor of postoperative morbidity in patients with distal cholangiocarcinoma. Mol Clin Oncol. 2018;9(4):362–8.
Peng D, Lu J, Hu H, Li B, Ye X, Cheng N. Lymphocyte to monocyte ratio predicts resectability and early recurrence of Bismuth-Corlette type IV hilar cholangiocarcinoma. J Gastrointest Surg. 2019. https://doi.org/10.1007/s11605-018-04086-9.
Zhang Y, Shi SM, Yang H, Yang LX, Wang Z, Li XD, et al. Systemic inflammation score predicts survival in patients with intrahepatic cholangiocarcinoma undergoing curative resection. J Cancer. 2019;10(2):494–503.
Hu G, Liu Q, Ma JY, Liu CY. Prognostic significance of platelet-to-lymphocyte ratio in cholangiocarcinoma: a meta-analysis. Biomed Res Int. 2018;2018:7375169.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Masafumi Ohira and his co-authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ohira, M., Yoshizumi, T., Yugawa, K. et al. Association of inflammatory biomarkers with long-term outcomes after curative surgery for mass-forming intrahepatic cholangiocarcinoma. Surg Today 50, 379–388 (2020). https://doi.org/10.1007/s00595-019-01905-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-019-01905-7