Abstract
Purpose
This retrospective study investigates the safety of neoadjuvant chemotherapy with oxaliplatin capecitabine (CapeOx), followed by laparoscopic surgery, for lower rectal cancer, and its efficacy in preserving the sphincter.
Methods
Ten patients with diagnosed lower rectal cancer received three or four cycles of neoadjuvant CapeOx chemotherapy, prior to undergoing low anterior resection or intersphincteric resection, with total mesorectal excision. The primary outcomes were R0 resection and the rate of sphincter preservation.
Results
Nine patients completed CapeOx as scheduled and a partial response was achieved in four; thus, the overall response rate was 40% (n = 4/10). After surgical intervention, 80% of tumors displayed downstaging. Postoperative anastomosis leakage developed in one patient. The distance from the anal verge to the tumor increased by 60% (median 1.5 cm) after CapeOx treatment. The anal sphincter was preserved in all patients and all pathological distal and radial margins were negative (R0 resections). A pathological complete response was achieved in one patient.
Conclusions
Neoadjuvant CapeOx chemotherapy is a promising approach, because it extended the distance from the anus to the tumor. Subsequent laparoscopic intervention for advanced lower rectal cancer could allow for safe preservation of the sphincter.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The combination of preoperative radiotherapy and fluorouracil (RT + 5FU) chemotherapy has been shown to reduce the local recurrence of rectal cancer. Consequently, the National Comprehensive Cancer Network (NCCN 20th) standardized this regimen in Europe [1]. Neoadjuvant therapy has also been shown to be beneficial for reducing recurrence. In 2004, a randomized trial in Germany established the superiority of preoperative fluorouracil-based chemoradiotherapy [2, 3]. Preoperative chemoradiotherapy combined with a total mesorectal excision (TME) improved local tumor control and sphincter-preservation rates in patients with locally advanced rectal cancer [4,5,6]. Although RT + 5FU regimens can reduce tumor volume, they do not have as much influence on distant micro metastases as intensive chemotherapy. With this in mind, Peeter KC et al. suggested that preoperative radiotherapy for rectal cancer had no effect on overall survival, which is principally determined by distant metastases [7]. Combinations of capecitabine and oxaliplatin, known as “CapeOx regimens”, have been established for the treatment of metastases and are used as adjuvant chemotherapy for colorectal cancer. According to one report, the CapeOx response rate was approximately 47.0% and progression-free survival was 8.0 months [8].
In another recent report, the efficacy of intensive neoadjuvant chemotherapy for advanced colorectal cancer was comparable to that achieved with the conventional fluorouracil-based chemoradiotherapy [9]. However, CapeOx has not been investigated for its safety or efficacy as a neoadjuvant chemotherapy in conjunction with laparoscopic surgery for advanced lower rectal cancer. We conducted this retrospective study to investigate the efficacy of neoadjuvant CapeOx chemotherapy combined with lower laparoscopic low anterior resection (LAR) or intersphincteric resection (ISR). As outcomes, we evaluated changes in the distance between the anal verge (AV) and the tumor and the sphincter-preservation rate.
Materials and methods
Patient recruitment
The subjects of this study were patients with high-risk lower rectal cancer, who underwent laparoscopic LAR or ISR after neoadjuvant CapeOx chemotherapy, between October, 2011 and January, 2013. We identified 29 patients with advanced lower rectal cancer treated during this period. We defined high risk as the presence of T3 or T4 disease or lymph nodes on magnetic resonance imaging (MRI) or computed tomography (CT) scans and a decision from the attending physician that tumor downstaging was desirable before performing R0 surgery or that sphincter preservation would be difficult. The decision to administer CapeOx neoadjuvant chemotherapy was made by the attending physician. This study was approved by the Ethics Committee of our institution (Approval Number: 15144).
Neoadjuvant treatment
Neoadjuvant CapeOx chemotherapy was scheduled to be administered in three or four cycles. Each 3 week cycle comprised oxaliplatin (130 mg/m2, in 5% glucose) on day 1, and oral capecitabine (1000 mg/m2) twice daily, from days 1 to 14, followed by a 7 day treatment-free interval. Toxicity was assessed before each 3 week cycle, according to the National Cancer Institute Common Terminology Criteria for Adverse Events, version 4.0.
Evaluation items
The change in the distance between the AV and the tumor was evaluated by performing a digital examination and endoscopy (CF-260AI: Olympus).
Change in the depth of tumor invasion
Before and after neoadjuvant chemotherapy, the depth of tumor invasion was measured on CT or MRI scans. Postoperative evaluations were based on pathological findings.
Surgery
All patients underwent either laparoscopic LAR or ISR under general anesthesia. Each surgical procedure was undertaken at the surgeon’s discretion, with consideration of the distance between the AV and the tumor. Surgical complications were classified according to the Japan Clinical Oncology Group postoperative complications criteria [10]. In some operations, hyaluronate-carboxymethyl cellulose membrane was used to prevent postoperative adhesion [11].
Adjuvant chemotherapy
Adjuvant chemotherapy was given at the attending physician’s discretion.
Histological classifications of the response to neoadjuvant chemotherapy were based on the eighth edition of the “The Guidelines of Japanese classification of colorectal carcinoma” [12] as follows:
-
Grade 0 (no effect): no tumor cell necrosis or degeneration was observed in response to treatment.
-
Grade 1 (minimal or mild effect): (a) Minimal effect: Tumor cell necrosis or degeneration was present in less than 1/3 of the entire lesion. (b) Mild effect: Tumor cell necrosis or degeneration was present in more than 1/3, but less than 2/3 of the entire lesion.
-
Grade 2 (moderate effect): Prominent tumor cell necrosis, degeneration, lytic changes, and/or disappearance were observed in more than 2/3 of the lesion, although viable tumor cells remained.
-
Grade 3 (marked effect): Necrosis and/or lytic changes were observed throughout the lesion, with substituting fibrosis, with or without granulomatous changes. No viable tumor cells remained.
Endpoints
This study evaluated the following endpoints: the rate of response to neoadjuvant chemotherapy; the rate of tumor down-staging; pathological effects; and the rate of sphincter preservation following laparoscopic surgery.
Results
Ten patients (seven males, three females) with advanced lower rectal cancer were enrolled at Osaka University hospital (Table 1). The median age was 65 years (range 44–74 years), and all patients had an Eastern Cooperative Oncology Group (ECOG) performance status of zero. Nine patients completed the course of neoadjuvant chemotherapy.
Neoadjuvant CapeOx therapy
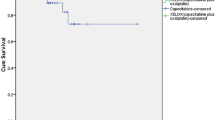
There was no grade 3 or higher adverse event. One patient failed to complete chemotherapy because of grade-2 liver dysfunction; thus, the overall response rate was 40% (n = 4/10) and the partial response (PR) and stable disease (SD) rates were 40% (n = 4/10) and 60% (n = 6/10), respectively. The depth of tumor invasion, determined by imaging analyses, was demonstrably reduced by 30% after chemotherapy (Fig. 1). The distance from the AV to the tumor increased by 60% (median distance 1.5 cm) after CapeOx (Fig. 2).
Surgery
All operations were either laparoscopic (LAR, n = 8) or ISR (n = 2), with no case of open surgery, regardless of age [13]. A temporary ileostomy was required in eight patients and not required in two of those who underwent LAR. After the operation, the tumor down-staging rate was 80% (Fig. 3). Postoperative anastomosis leakage developed in one patient. The median length of the distal margin was 2.5 cm and the anus was preserved in all patients. The pathological distal and radial margins were negative (R0 resections).
Treatment altered cancer staging. Staging before and after chemotherapy (chemo) shows that neoadjuvant CapeOx chemotherapy altered the TNM stage (Ver.7). Diagnoses before and after neoadjuvant chemotherapy were based on digital examination, endoscopy, CT, and MRI. Postoperative diagnoses were based on pathologic examinations
One patient requested a sphincter-preserving operation, but the attending physician advised that an abdominoperineal resection would be more appropriate; thus, neoadjuvant CapeOx was recommended. After CapeOx, the distance of the tumor from the dentate line (DL) changed from 1 to 2 cm. After the subsequent ISR, the pathological DL was negative. Another patient also requested a sphincter-preserving operation and the distance of the tumor from the DL changed from 1.5 to 2.5 cm after CapeOx. After LAR, the pathological DL was negative.
A pathological complete response was achieved in one patient (pT0, pN0, and M0; Fig. 4). Local recurrence was found 183 days after surgery in another patient.
Discussion
In Europe, the gold standard of neoadjuvant therapy for advanced rectal cancer is RT + 5FU or RT + capecitabine (NCCN 20th). Hida et al. reported that neoadjuvant chemoradiotherapy and TME were appropriate for advanced rectal cancer [14]; however, it remained a concern that the RT + 5FU regimens seemed less effective than intensive chemotherapy for controlling distant micro metastases, because survival is determined principally by distant metastases. Thus, it was suggested that preoperative radiotherapy did not provide any added benefit in treating rectal cancer, because it did not influence overall survival [7]. However, if a neoadjuvant intensive chemotherapy regimen was found to provide local control comparable to that achieved by RT + 5FU, then it may be considered useful in terms of long-term prognoses.
CapeOx has emerged as a useful therapeutic regimen for colorectal cancer [15,16,17,18]. The 3 week CapeOx chemotherapy schedule includes capecitabine, and an oral fluoropyrimidine used to treat metastatic colorectal cancer [19,20,21,22]. Capecitabine is also used as adjuvant therapy for high-risk stage II and III colon cancer [23]. The standard 21 day intermittent treatment schedule, consisting of 14 days of treatment, followed by a 7 day break, with intravenous oxaliplatin on the first day provides a convenient alternative to intravenous fluorouracil-based chemotherapy doublets, without compromising antitumor efficacy [8]. For this study, we selected CapeOx rather than the combination of folinic acid, oxaliplatin, and fluorouracil (FOLFOX) as neoadjuvant chemotherapy. FOLFOX is inconvenient for both patients and clinicians, because it requires a central venous access port and a pump for continuous infusion. These requirements were rendered redundant by the development of oral 5-FU-based preparations, such as capecitabine. Oral preparations reduce the risks of catheter-related problems, infection, thrombosis, skin dehiscence, and pneumothorax or bleeding [24, 25]. In fact, patients with advanced colorectal cancer reported that they preferred oral drugs to intravenous therapy because of their convenience and reduced toxicity [26]. However, preoperative chemotherapy has the following potential risks: overtreatment from inaccurate radiological staging, which can lead to severe toxicity in patients with low risk; bowel obstruction, caused by the primary tumor during preoperative therapy, which can result in emergency, but not radical surgery; and perioperative complications, including anastomosis leakage [27].
In this study, the disease-control rate achieved by neoadjuvant CapeOx chemotherapy was 100%. Although one patient did not complete the scheduled chemotherapy because of liver dysfunction, surgery was performed safely. The single case of postoperative anastomosis leakage did not require reoperation. Only three previous studies have described neoadjuvant chemotherapy for rectal cancer (Table 2) [9, 28, 29]. All those studies used Bevacizumab (Bmab), which affected the response rate; however, Bmab did not change the R0 resection rate or the pathological complete response rate. Uehara investigated the neoadjuvant regimen, XELOX (capecitabine + oxaliplatin) plus Bmab for poor-risk rectal cancer patients, but that treatment was associated with a high rate of anastomotic leakage, suggesting that nBmab was not suitable neoadjuvant chemotherapy for rectal cancer. Our observation that neoadjuvant chemotherapy increased the distance between the tumor and the AV or DL could not be compared with findings from other studies, which did not evaluate this outcome. We suggest that the neoadjuvant chemotherapy effects of extending the distance between the AV and the tumor and diminishing tumor invasion might have contributed to preservation of the anus and prevention of local recurrence.
This study has several limitations. First, the distance from the anal verge to the tumor was lengthened with tumor shrinkage, but this result was based on data from retrospective findings during endoscopic examination. Therefore, there was a possibility of measurement error, depending on examination conditions. Second, the change of distance, microscopically, was unknown. Future prospective studies on larger patient cohorts are needed to confirm our findings.
Conclusions
This study demonstrated that laparoscopic LAR or ISR can be performed safely in conjunction with the neoadjuvant therapy, CapeOx, for rectal cancer. This method increased the distance from the AV to the tumor, improved the anus preservation rate, increased the R0 resection rate, and reduced local recurrence. We speculate that this method may also help control distant metastases, but further study is needed to investigate this possibility.
References
NCCN Clinical Practice Guidelines in Oncology: Rectal Cancer Version 2.2017. National Comprehensive Cancer Network. Abstract https://www.nccn.org/professionals/physician_gls/pdf/rectal.pdf (2016). Accessed 22 Dec 2016.
Sauer R, Becker H, Hohenberger W, Rödel C, Wittekind C, et al. German Rectal Cancer Study Group (2004) Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med. 2014;351:1731–40.
Sauer R, Liersch T, Merkel S, Fletkau R, Hohenberger W, Hess C, et al. Preoperative versus postoperative chemoradiotherapy for locally advanced rectal cancer: results of the German CAO/ARO/AIO-94 randomized phase III trial after a median follow-up of 11 years. J Clin Oncol. 2012;30:1926–33.
Camma C, Giunta M, Fiorica F, Pagilaro L, Craxi A, Cottone M. Preoperative radiotherapy for respectable rectal cancer: a meta-analysis. JAMA. 2000;284:1008–15.
Kapiteijn E, Marijnen CA, Nagtegaal ID, Putter H, Steup WH, Wiggers T, et al. Dutch Colorectal Cancer Group Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. N Engl J Med. 2001;345:638–46.
Bosset JF, Collette L, Calais G, Mineur L, Maingon P, Radosevic-lelic L, et al. Chemotherapy with preoperative radiotherapy in rectal cancer. N Engl J Med. 2006;355:1114–23.
Peeters KC, Marijnen CA, Nagtegaal ID, Kranenbarg EK, Putter H, Wiggers T, et al. The TME trial after a median follow-up of 6 years: increased local control but no survival benefit in irradiated patients with resectable rectal carcinoma. Ann Surg. 2007;246:693–701.
Cassidy J, Clarke S, Díaz-Rubio E, Scheithauer W, Figer A, Wong R, et al. Randomized phase III study of capecitabine plus oxaliplatin compared with fluorouracil/folinic acid plus oxaliplatin as first-line therapy for metastatic colorectal cancer. J Clin Oncol. 2008;26:2006–12.
Schrag D, Weiser MR, Goodman KA, Gonen M, Hollywood E, Cercek A, et al. Neoadjuvant chemotherapy without routine use of radiation therapy for patients with locally advanced rectal cancer: a pilot trial. J Clin Oncol. 2014;32:513–8.
Katayama H, Kurokawa Y, Nakamura K, Ito H, Kanemitsu Y, Matsuda N, et al. Extended Clavien-Dindo classification of surgical complications: Japan Clinical Oncology Group postoperative complications criteria. Surg Today. 2016;46:668–85.
Osawa H, Nishimura J, Hiraki M, Takahashi H, Haraguchi N, Hata T, et al. Regeneration of peritoneal mesothelial cells after placement of hyaluronate carboxymethyl-cellulose (Seprafilm®). Surg Today. 2017;47:130–6.
Watanabe T, Itabashi M, Shimada Y, Tanaka S, Ito Y, Ajioka Y, et al. Japanese Society for Cancer of the Colon and Rectum (JSCCR) Guidelines 2014 for treatment of colorectal cancer. Int J Clin Oncol. 2015;20:207–39.
Shiga M, Maeda H, Oba K, Okamoto K, Namikawa T, Fujisawa K, et al. Safety of laparoscopic surgery for colorectal cancer in patients over 80 years old: a propensity score matching study. Surg Today. 2017;27:1–8.
Hida J, Okuno K, Tokoro T. Distal dissection in total mesorectal excision, and preoperative chemoradiotherapy and lateral lymph node dissection for rectal cancer. Surg Today. 2014;44:2227–42.
Cassidy J, Tabernero J, Twelves C, Brunet R, Butts C, Conroy T, et al. XELOX (capecitabine plus oxaliplatin): active first-line therapy for patients with metastatic colorectal cancer. J Clin Oncol. 2004;22:2084–91.
Hochster HS, Hart LL, Ramanathan RK, Childs BH, Hainsworth JD, Cohn AL, et al. Safety and efficacy of oxaliplatin/fluoropyrimidine regimens with or without bevacizumab as first-line treatment of metastatic colorectal cancer (mCRC): final analysis of the TREE-Study. J Clin Oncol. 2006;24:18.
Martoni AA, Pinto C, Fabio FD, Lelli G, Rojas Limpe FL, Gentlile AL, et al. Capecitabine plus oxaliplatin (XELOX) versus protracted 5-fluorouracil venous infusion plus oxaliplatin (pvifox) as first-line treatment in advanced colorectal cancer: a GOAM phase II randomised study (FOCA trial). Eur J Cancer. 2006;42:3161–8.
Pfeiffer P, Sorbye H, Ehrsson H, Fokstuen T, Mortensen JP, Baltesgard L, et al. Short-time infusion of oxaliplatin in combination with capecitabine (XELOX30) as second-line therapy in patients with advanced colorectal cancer after failure to irinotecan and 5-fluorouracil. Ann Oncol. 2006;17:252–8.
Borner MM, Dietrich D, Stupp R, Morant R, Honegger H, Wernli M, et al. Phase II study of capecitabine and oxaliplatin in first- and second-line treatment of advanced or metastatic colorectal cancer. J Clin Oncol. 2002;20:1759–66.
Van Cutsem E, Twelves C, Cassidy J, Allman D, Bajetta E, Boyer M, et al. Oral capecitabine compared with intravenous fluorouracil plus leucovorin in patients with metastatic colorectal cancer: results of a large phase III study. J Clin Oncol. 2001;19:4097–106.
Van Cutsem E, Hoff PM, Harper P, Bukowski RM, Cunningham D, Dufour P, et al. Oral capecitabine vs intravenous 5-fluorouracil and leucovorin: integrated efficacy data and novel analyses from two large, randomized, phase III trials. Br J Cancer. 2004;90:1190–7.
Hoff PM, Ansari R, Batist G, Cox J, Kocha W, Kuperminc M, et al. Comparison of oral capecitabine versus intravenous fluorouracil plus leucovorin as first-line treatment in 605 patients with metastatic colorectal cancer: results of a randomized phase III study. J Clin Oncol. 2001;19:2282–92.
Twelves C, Wong A, Nowacki MP, Abt M, Burris H 3rd, Carrato A, et al. Capecitabine as adjuvant treatment for stage III colon cancer. N Engl J Med. 2005;352:2696–704.
Mansfield PF, Hohn DC, Fornage BD, Gregurich MA, Ota MD. Complications and failures of subclavian-vein catheterization. N Engl J Med. 1994;331:1735–8.
Zawacki WJ, Walker TG, DeVasher E, Halpern EF, Waltman AC, Wicky ST, et al. Wound dehiscence or failure to heal following venous access port placement in patients receiving bevacizumab therapy. J Vasc Interv Radiol. 2009;20:624–7.
Borner MM, Schoffski P, de Wit R, Caponigro F, Comella G, Sulkes A, et al. Patient preference and pharmacokinetics of oral modulated UFT versus intravenous fluorouracil and leucovorin: a randomised crossover trial in advanced colorectal cancer. Eur J Cancer. 2002;38:349–58.
Fujita F, Torashima Y, Kuroki T, Eguchi S. Risk factors and predictive factors for anastomotic leakage after resection for colorectal cancer: reappraisal of the literature. Surg Today. 2014;44:1595–602.
Uehara K, Hiramatsu K, Maeda A, Sakamoto E, Inoue M, Kobayashi S, et al. Neoadjuvant oxaliplatin and capecitabine and bevacizumab without radiotherapy for poor-risk rectal cancer: N-SOG 03 Phase II trial. Jpn J Clin Oncol. 2013;43:964–71.
Hasegawa J, Nishimura J, Mizushima T, Miyake Y, Kim HM, Takemoto H, et al. Neoadjuvant capecitabine and oxaliplatin(XELOX) combined with bevacizumab for high-risk localized rectal cancer. Cancer Chemother Pharmacol. 2014;73:1079–87.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We declare no conflicts of interest.
Funding
This study was not grant funded.
Rights and permissions
About this article
Cite this article
Hata, T., Takahashi, H., Sakai, D. et al. Neoadjuvant CapeOx therapy followed by sphincter-preserving surgery for lower rectal cancer. Surg Today 47, 1372–1377 (2017). https://doi.org/10.1007/s00595-017-1527-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-017-1527-5