Abstract
Purpose
To clarify the risk factors for complications after diverting ileostomy closure in patients who have undergone rectal cancer surgery.
Methods
The study group comprised 240 patients who underwent a diverting ileostomy at the time of lower anterior resection or internal anal sphincter resection, in our department, between 2004 and 2015. Univariate and multivariate analyses of 18 variables were performed to establish which of these are risk factors for postoperative complications.
Results
The most common complications were intestinal obstruction and wound infection. Univariate analysis showed that an age of 72 years or older (p = 0.0028), an interval between surgery and closure of 6 months or longer (p = 0.0049), and an operation time of 145 min or longer (p = 0.0293) were significant risk factors for postoperative complications. Multivariate analysis showed that age (odds ratio, 3.4236; p = 0.0025), the interval between surgery and closure (odds ratio, 3.4780; p = 0.0039), and operation time (odds 2.5179; p = 0.0260) were independent risk factors.
Conclusions
Age, interval between surgery and closure, and operation time were independent risk factors for postoperative complications after diverting ileostomy closure. Thus, temporary ileostomy closure should be performed within 6 months after surgery for rectal cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anal sphincter-preserving procedures, such as super-low anterior resection and internal anal sphincterotomy, are now performed regularly for patients with lower rectal cancer. The number of patients with a temporary diverting stoma created to protect the anastomosis or to achieve fecal diversion to prevent suture failure is increasing. However, complications such as intestinal obstruction, wound infection, and suture failure can develop after stoma closure [1–5]. Therefore, a diverting stoma created for postoperative safety should be closed as soon as the risk of initial treatment-related complications becomes negligible, allowing patients to resume their normal social activities. To preserve quality of life, the risk of complications developing after ileostomy closure should be minimized. The aim of this study was to define the risk factors for complications occurring after diverting ileostomy closure in patients who had undergone surgery for rectal cancer.
Materials and methods
The subjects of this study were 240 patients who underwent closure of a diverting ileostomy created at the time of surgery for lower rectal cancer, in our department, between September, 2004 and April, 2015 (Table 1). Twelve patients whose diverting ileostomy was created as an emergency for diffuse peritonitis caused by postoperative suture failure were excluded from the analysis. In principle, diverting ileostomy closure was indicated for all patients; however, the timing of surgery was decided after considering the patients’ wishes, age, activities of daily living, and social background; and after obtaining informed consent from the patient. Before ileostomy closure, barium enema examination was performed with Gastrografin to confirm the absence of suture failure and strictures of the anastomosis. Ileostomy closure was scheduled for 2–3 months after surgery.
We examined which of the following 18 variables were risk factors for post-closure surgical complications: age, sex, ASA score, tumor location (upper or lower rectum), preoperative chemoradiotherapy, diabetes mellitus, cardiac disease, respiratory disease, smoking, clinical stage of the disease, body-mass index, previous surgical procedures (open or laparoscopic), complications after previous surgery, surgical technique (lower anterior or intersphincteric resection), pathological stage, interval between surgery and ileostomy closure, operation time, and blood loss.
We used Chi-square tests (with Yates’ correction), Mann–Whitney U tests, and receiver-operating-characteristic curves, to divide the study variables into two groups to perform statistical analysis. Multivariate logistic regression analysis was used to analyze the risk factors. p values of less than 0.05 were considered to indicate significance. The above statistical analyses were performed using SPSS version 8.0 J (SPSS, Inc., Chicago, Ill, USA).
Procedure for ileostomy closure
After closing the ileostomy with 10 1-0 silk sutures, the skin was disinfected and surgery began. A skin incision was made in a spindle-like fashion around the sutured closure site. Next, the ileum was circumferentially dissected, mobilized in the peritoneal cavity, and lifted out of the wound. A functional end-to-end anastomosis was performed in all patients, using an automatic suturing device, to place three or four stitches. The end of the anastomosis was ligated using absorbable 4-0 sutures, and the anastomosis with the intestine was reinforced with two stitches. The wound was closed with two-layer sutures and the peritoneum and the fascia were closed with one absorbable 1-0 knotted suture. After high-pressure washing of the subcutaneous tissue with physiological saline, the skin was closed using 4-0 absorbable dermal sutures.
Results
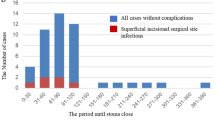
Ileostomy closure was performed in all 240 patients, with a postoperative length of stay of 8 days (range 5–54 days). The median follow-up after ileostomy closure was 65 months (range 9–135 months). Postoperative complications developed in 31 (12.9%) of the 240 patients, but there was no surgery-related death. Postoperative complications were as follows: intestinal obstruction (n = 16; 6.7%), wound infection (n = 13; 5.4%), pelvic abscess (n = 1: 0.4%), and suture failure (n = 1; 0.4%; Table 2). Coexisting cardiac diseases included hypertension (n = 22; 9.1%) and ischemic heart disease (n = 44; 18.3%) and coexisting respiratory diseases included obstructive ventilatory impairment (n = 15; 6.3%), restrictive ventilatory impairment (n = 4; 1.7%), and mixed ventilatory impairment (n = 1; 0.4%). Univariate analysis revealed that an age of 72 years or older (p = 0.0028), an interval between surgery and closure of 6 months or longer (p = 0.0049), and an operation time of 145 min or longer (p = 0.0293) were significant risk factors for postoperative complications (Table 3). On multivariate analysis, age (odds ratio, 3.4236; p = 0.0025), interval between surgery and closure (odds ratio, 3.4780; p = 0.0039), and operation time (odds ratio, 2.5179, p = 0.0260) were independent risk factors (Table 4).
Discussion
Our single-center trial demonstrated that age (72 years or older), an interval of 6 months or longer from ileostomy creation to closure, and an operation time of 145 min or longer were risk factors for complications developing after diverting ileostomy closure in patients who had undergone surgery for rectal cancer.
A covering ileostomy may be created transiently to achieve fecal diversion and thereby protect the anastomosis and prevent the occurrence of suture failure in patients who have undergone lower anterior resection or anal sphincter-preserving surgery with sphincterotomy. In recent years, the number of patients with an ileostomy is increasing with the dissemination of anal sphincter-preserving surgery. Therefore, it is important to decrease the incidence of complications occurring after ileostomy closure; however, ileostomy closure may require an extended incision because of intraperitoneal adhesion or serosal injury of the elevated intestine caused by losing track of the layer to be dissected when passing from the body surface to the peritoneal cavity. Although few studies have reported complications occurring after ileostomy closure, the incidence of complications is estimated to be 10–30% [6], so ileostomy closure cannot be considered a safe surgical procedure. Intestinal obstruction accounts for 50–70% of all complications [7]. Factors contributing to the development of complications after ileostomy closure include adjuvant therapy, underlying disease, the interval from ileostomy creation to closure, and the technique used for anastomosis [7–10]. Intestinal obstruction is the main complication after ileostomy closure and, accordingly, was the most common complication in our study, occurring in 6.7% of patients. As for the relationship between the anastomosis and intestinal obstruction occurring after transient ileostomy closure, the incidence of intestinal obstruction has been reported to be similar in patients with a hand-sewn anastomosis and those with a stapled anastomosis. However, Hasegawa et al. [8] reported that the incidence of intestinal obstruction was significantly higher in patients with a hand-sewn anastomosis (14%) than in those with a functional end-to-end anastomosis (3%) and recommended a functional end-to-end anastomosis. Thus, we now perform a functional end-to-end anastomosis in our hospital. As for the cause of postoperative intestinal obstruction, the intestine distal to the stoma may become thinner than the distal intestine through which stools passed before stoma closure, increasing the risk of postoperative edema at the site of anastomosis. Williams et al. [11] reported that the caliber of a mechanically stapled functional end-to-end anastomosis might become greater than that of a hand-sewn end-to-end anastomosis, thereby decreasing the risk of intestinal obstruction caused by anastomotic edema. Moreover, the long-term lack of stool passage can lead to decreased contractility, reduced smooth-muscle strength, and villus atrophy in the distal intestine [12]. Animal studies have suggested that structural changes in the intestinal mucosa caused by the lack of stool passage might alter the barrier mechanism of the intestine [13].
The difference between ileostomy and colostomy lies in the fact that the colon is associated with a high incidence of complications related to surgical closure of the stoma, particularly wound infection [14]. Because ileostomy closure is more straightforward than colostomy closure [15], we perform temporary ileostomy in our hospital. The incidence of surgical-site infection of the incised tissue surface has been reported to range broadly from 2 to 40% [16], and was relatively low (5.4%) in the present series. It is important to prevent postoperative complications in patients undergoing initial surgery for rectal cancer [17]. Early stoma closure is associated with a high incidence of wound infection, whereas late stoma closure is associated with a high risk of intestinal obstruction [18]. Thalheimer et al. [9] reported that many postoperative complications can occur after adjuvant chemoradiotherapy. In our study, 105 patients (44%) had preoperative chemoradiotherapy, but this was not found to be a risk factor for postoperative complications. Akiyoshi et al. [19] studied the complications that occurred after temporary ileostomy closure in 125 patients with rectal cancer and reported that male sex and wound infection after the rectal cancer surgery were independent risk factors. In our study, 14% of the patients suffered complications after surgery for rectal cancer, but these complications were not associated with diverting ileostomy closure. Five (2.1%) patients who underwent previous surgery had postoperative wound infection, one (20%) of whom had postoperative intestinal obstruction. Ultimately, it is important to prevent postoperative complications at the time of initial surgery for rectal cancer.
Vivian et al. [20] reported that 16.4% of 213 patients suffered postoperative complications. The risk factors were an age of 80 years or older and respiratory disease. We observed similar results for elderly patients. In a previous study, diverting ileostomy closure was performed within 8.5 weeks or 6 months or more after surgery, and postoperative complications showed a bimodal pattern of occurrence [7]. In the study by Vivian et al., 16.4% of the 213 subjects had postoperative complications and an age of 80 years or older was a risk factor. In our study of subjects 72 years or older, the results were similar. The following two factors were added to possible risk factors for postoperative complications: cardiac disease and respiratory disease. However, these two factors were not found to be risk factors for postoperative complications. In our study, ileostomy closure 6 months or more after surgery was a risk factor for postoperative complications, which highlights the importance of performing ileostomy closure within 3–6 months after surgery.
Based on the findings of our study, a large randomized controlled trial should be performed in Japan to define more clearly the risk factors for complications after diverting ileostomy closure and establish more effective ways to prevent postoperative complications.
References
Gooszen AW, Geelkrken RH, Hermans J, Lagaay MB, Gooszen HG. Temporary decompression after colorectal surgery:randomized comparison of loop ileostomy and loop colostomy. Br J Surg. 1998;85:76–9.
Kaidar-Person O, Person B, Wexner SD. Complication of construction and closure of temporary loop ileostomy. J Am Coll Surg. 2005;201:759–73.
Katayama H, Kurokawa Y, Nakamura K, Ito H, Kanemitsu Y, Masuda N, et al. Extended Clavien-Dindo classification of surgical complications: Japan Clinical Oncology Group postoperative complications criteria. Surg Today. 2016;46:668–85.
Osawa H, Nishimura J, Hiraki M, Takahashi H, Haraguchi N, Hata T, et al. Regeneration of peritoneal mesothelial cells after placement of hyaluronate carboxymethyl-cellulose (Seprafilm®). Surg Today. 2017;47:130–6.
Shiga M, Maeda H, Oba K, Okamoto K, Namikawa T, Fujisawa K, et al. Safety of laparoscopic surgery for colorectal cancer in patients over 80 years old: a propensity score matching study. Surg Today. 2017. doi:10.1007/s00595-017-1470-5.
Wong KS, Remzi FH, Gorgun E, Arrigain S, Church JM, Preen M, et al. Loop ileostomy closure after restorative proctocolectomy:outcome in 1,504 patients. Dis Colon Rectum. 2005;48:243–50.
Perez RO, Habr-Gama A, Seid VE, Proscurshim I, Sousa AH Jr, Kiss DR, et al. Loop ileostomy morbidity: timing of closure matters. Dis Colon Rectum. 2006;49:1539–45.
Hasegawa H, Radley S, Morton DG, et al. Stapled versus sutured closure of loop ileostomy:a randomized controlled trial. Ann Surg. 2000;231:202–24.
Thalheimer A, Bueter M, Kortuem M, Thiede A, Meyer D. Morbidity of temporary loop ileostomy in patients with colorectal cancer. Dis Colon Rectum. 2006;49:1011–7.
Carlsen E, Bergan AB. Loop ileostomy: technical aspects and complications. Eur J Surg. 1999;165:140–3.
Williams NS, Nasmyth DG, Jones D. Defunctioning stomas: a prospective controlled trial comparing loop ileostomy with loop traial comparing loop ileostomy with loop transverse colostomy. Br J Surg. 1986;73:566–70.
Williams L, Armstrong M, Finan P, Sagar P, Burke D. The effect of faecal diversion on human ileum. Gut. 2007;56:796–801.
Pinto FE Jr, Brandt CT, Medeiros Ada C, de Oliveira AJ, Jerônimo SM, de Brito HM. Bacterial translocation in rats nonfunctioning diverted distal colon. Acta Cir Bras. 2007;22:195–201.
Lertsithichai P, Rattanapichart P. Temporary ileostomy versus temporary colostomy: a meta-analysis of complications. Asian J Surg. 2004;27:202–10.
Reid K, Pockney P, Pollitt T, Draganic B, Smith SR. Randomized clinical trial of short-term outcomes following purse-string versus conventional ileostomy closure wounds. Br J Surg. 2010;97:1511–7.
Shellito PC. Complications of abdominal stoma surgery. Dis Colon Rectum. 1998;41:1562–72.
den Dulk M, Smit M, Peeters KC, Kranenbarg EM, Rutten HJ, Wiggers T, et al. A multivariate analysis of limiting factors for stoma reversal in patients with rectal cancer entered into the total mesorectal excision (TME) trial: a retrospective study. Lancet Oncol. 2007;8:297–303.
Alves A, Panis Y, Doussei B, Benoist S, Vicaut E. Randomized clinical trial of early versus delayed temporary stoma closure after proctectomy. Br J Surg. 2008;95:693–8.
Akiyoshi T, Fujimoto Y, Konishi T, Kuroyanagi H, Ueno M, Oya M, et al. Complications of loop ileostomy closure in patients with rectal tumor. World J Surg. 2010;34:1937–42.
Man VC, Choi HK, Law WL, Foo DC. Morbidities after closure of ileostomy: analysis of risk factors. Int J Colorectal Dis. 2016;31:51–7.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nakamura, T., Sato, T., Naito, M. et al. Risk factors for complications after diverting ileostomy closure in patients who have undergone rectal cancer surgery. Surg Today 47, 1238–1242 (2017). https://doi.org/10.1007/s00595-017-1510-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-017-1510-1