Abstract
Purpose
Familial adenomatous polyposis (FAP)-associated desmoid tumor (DT) is sometimes life threatening. However, the optimal treatment for DTs has not been established. The aim of this study was to analyze the outcomes of surgical and pharmacological treatments for DT in Japanese FAP patients.
Methods
We retrospectively reviewed the data of 303 patients who underwent colectomy for FAP between 2000 and 2012. We analyzed 41 patients with DTs in which the location was apparent. The selection of treatment for intra-abdominal DTs was also evaluated according to Church’s classification.
Results
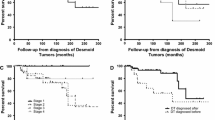
Surgery was frequently used to treat extra-abdominal DTs. Multimodal treatments, including surgery, and the administration of non-steroidal anti-inflammatory drugs, hormonal therapy, and chemotherapy were widely used for intra-abdominal DTs. The most effective pharmacological treatment was cytotoxic chemotherapy, which was associated with a response rate of 45.5% and a disease control rate of 72.7%. After a median follow-up period of 53.0 months, the 5-year DT-specific survival rate in patients with stage IV disease was 71.4%; in contrast, the rate in patients with other stages was 100%. Four-stage IV patients died of DT due to uncontrollable rapid progression. No cytotoxic chemotherapy was administered; however, incomplete resection was performed in three cases.
Conclusion
Our findings will provide clues that may help physicians in selecting the optimal strategy for this rare disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Familial adenomatous polyposis (FAP) is a complex genomic syndrome that is associated with the presence of large numbers (˃100) of colorectal adenomatous polyps with high malignant potential. If not treated using prophylactic colectomy, patients have an almost 100% risk of developing colorectal cancer (CRC). Patients with FAP often develop CRC by approximately 40 years of age [1]. As a prophylactic or curative procedure for FAP, restorative proctocolectomy with ileal pouch anal anastomosis (IPAA) or total colectomy with ileorectal anastomosis (IRA) are now widely indicated. Thus, the recent increase in the performance of prophylactic colectomy has reduced the risk of death from CRC in FAP patients [2]. Moreover, the extra-colonic manifestations of FAP have become more clinically apparent [3]. Among these, desmoid tumor (DT) has now become the leading cause of death in FAP patients who undergo prophylactic colectomy [2, 4].
DTs are rare fibroblastic benign tumors that can arise sporadically or in association with FAP. DTs are estimated to occur in 10–25% of FAP patients [2]. Surgical therapy is widely used as the initial treatment for DTs of the abdominal wall, but is less frequently indicated for mesenteric DTs because of the high risk of recurrence and because extensive resection is associated with a high risk of mortality [5–7]. Alternative therapies, such as radiotherapy, hormonal therapy, and nonsteroidal anti-inflammatory drugs (NSAIDs), have shown limited success in the treatment of intra-abdominal DTs [8]. Recent reports have also encouraged the administration of cytotoxic chemotherapy to FAP patients with DTs. However, a few limited cohort studies have reported the results of pharmacological treatments [9–11]. The optimal treatment for DTs in FAP patients has not been established and medical and surgical treatments have not been standardized due to a lack of clinical data regarding this rare disease.
In this study, we collected the data from the patient files of the Japanese Society for Cancer of the Colon and Rectum (JSCCR) registry. The aim of the present study was to analyze the outcomes of the surgical and pharmacological treatments of Japanese FAP patients with DTs. We reviewed our experience to provide clues for selecting the optimal strategy for this rare disease.
Methods
JSCCR registry
This investigation was conducted by the JSCCR Retrospective Cohort Study of the Familial Adenomatous Polyposis group in Japan. The data from 303 FAP patients who underwent colorectal surgery between 2000 and 2012 were collected from 23 member institutions of the JSCCR. The inclusion criteria for this study were FAP patients who underwent surgical resection from January 2000 to December 2012 with any of the following conditions: (a) >100 polyps in the colon and rectum; (b) a family history of FAP if there were <100 polyps in the colon and rectum; and (c) a germline mutation of the APC gene. The diagnosis of DT was ascertained based on a combination of clinical examinations, surgical exploration, and radiological evaluation. This study included patients who were diagnosed with DTs before the diagnosis of FAP, and those who were diagnosed at the same time or after initial colectomy. We analyzed the history of DT according to the location: extra-abdominal (or abdominal wall), intra-abdominal (or mesenteric), or mixed. Intra-abdominal DTs were also classified according to Church’s classification (Fig. 1) [12]. We clarified the following patient characteristics: surgical treatment for DTs; pharmacological treatment including NSAIDs, hormonal therapy, cytotoxic chemotherapy, and tyrosine kinase inhibitors; the response to treatment; and the prognosis. The study protocol was approved by the Ethical Committees of both the JSCCR and each institution.
Desmoid tumor staging system established by Church [12]
The surgical procedures for FAP
We performed restorative proctocolectomy as well as IPAA, and total proctocolectomy (TPC) with permanent ileostomy. IPAA consists of ileoanal anastomosis (usually performed by means of mucosectomy with hand-sewn anastomosis), and ileoanal canal anastomosis (usually performed by stapled anastomosis). Partial colectomy (PC) and IRA are designated as surgical procedures that could be performed without the use of proctocolectomy. TPC or PC was also indicated for older patients or those with coexisting advanced CRC.
The classification of FAP
We defined the patients with ≥100 polyps in the colon and rectum as having classic FAP, and those with <100 polyps as having attenuated FAP. Classic FAP was also classified into the sparse (100–1000 polyps) and profuse (>1000 polyps) types. The mutation data were not collected, because we could not obtain informed consent; however, germline mutations of the APC gene were confirmed in some of the cases.
The pharmacological treatments for DT
The pharmacological treatments included NSAIDs, sulindac, meloxicam, celecoxib, hormonal therapy, tamoxifen, luteinizing hormone-releasing hormone (LH-RH) agonist, tyrosine kinase inhibitor, imatinib, sunitinib, or cytotoxic chemotherapy. Different cytotoxic chemotherapy regimens were used, these included combinations of doxorubicine (DOX), methotrexate (MTX), vinblastine (VBL), cyclophosphamide (CYC), carboplatin (CARBO), and dacarbazine (DTIC). The combination regimens included dacarbazine-based chemotherapy (DTIC with DOX or VBL or CYC or CARBO), and methotrexate-based chemotherapy (MTX plus VBL). The details of each regimen including the doses and administration schedules were not compiled in our study.
The success of a pharmacological treatment was defined based on the regression or the stabilization of the DTs on computed tomography (CT) or magnetic resonance imaging (MRI). The responses were categorized as follows: progressive disease (PD; a radiologically confirmed increase in size in comparison to the previous imaging), stable disease (SD; no radiologically confirmed increase or decrease in size in comparison to previous imaging), partial response (PR; a radiologically confirmed decrease in size in comparison to previous imaging), or complete response (CR; the radiological disappearance of the DTs). The responses to each regimen were also calculated as the proportion of PR/CR in the same treatment lines.
Statistical analysis
The JMP software program (version 7, SAS Institute, Cary, NC, USA) was used to perform the statistical analyses. The data are presented as the median (range). Contingency tables were analyzed using Fisher’s exact test or a χ 2 test with Yates’ correction. Correlations between continuous and categorical variables were evaluated using the Mann–Whitney U test. Kaplan–Meier survival curves were constructed and differences were analyzed using the log-rank test. P values of <0.05 were considered to indicate statistical significance.
Results
The study population
Among the 303 patients with FAP who were registered in the JSCCR registry database, 48 (15.8%; male, n = 19; female, n = 29) patients had DTs. The rate of female patients was high in comparison to the rate of female FAP patients without DTs (p = 0.0548). Among these 48 patients, 16 (33.3%) were diagnosed with DTs before initial colectomy, and 32 (66.7%) had DTs after surgery. The locations of the DTs in the 48 patients were classified as follows: extra-abdominal (n = 8), intra-abdominal (n = 25), mixed (n = 8), and unknown (n = 7). In the present study, we excluded the cases in which the location was unknown. Thus, 41 patients were included in the analysis. The demographic information of the patients is summarized in Table 1. Thirty (73.2%) patients were diagnosed with a DT diagnosed after the initial colectomy. Intra-abdominal and mixed DTs were definitively diagnosed after surgery more frequently than extra-abdominal DTs (89.7 vs. 50.0%; p = 0.0152). Among the 41 patients, 35 (85.4%) had received medical and/or surgical treatment for DTs, while 6 (14.6%) received no treatment for their DTs.
Treatment selection
Among the 35 patients who received treatment for DTs, 21 (60.0%) underwent surgery. Surgery was frequently selected for extra-abdominal DTs, while medical treatment as well as surgery was more commonly selected for intra-abdominal DTs (Fig. 2). NSAIDs were administered to 22 of the 35 (62.9%) patients. Only 7 of the 22 (31.8%) patients received NSAIDs as a single agent therapy, mainly for extra-abdominal DTs. In addition, 6 of the 12 (50.0%) patients who underwent complete DT resection received NSAIDs as adjuvant therapy. Hormonal therapy was administered to 15 of the 35 (42.9%) patients; one patient received hormonal therapy alone. Chemotherapy was also administered to 14 of the 35 (40.0%) patients.
We also evaluated the selection of treatments for intra-abdominal DTs according to Church’s classification [12]. The Church’s classifications of the patients were as follows: stage I (n = 11), stage II (n = 0), stage III (n = 8), and stage IV (n = 7). Multi-modal treatments, including surgery, NSAIDs, hormonal therapy, and chemotherapy were introduced in each stage (Table 2). The mean number of treatments was 2 (1 in stage I, 2.5 in stage III, and 2.1 in stage IV). In comparison to the stage I and III patients, chemotherapy was administered significantly less frequently to stage IV patients, (p = 0.0112).
Surgical treatments
Among the 21 patients who underwent surgery, 12 (57.4%) underwent complete resection. Ten of the 11 (91.0%) patients with limited abdominal wall DTs, including patients with mixed DTs, underwent complete resection, while complete resection was less frequently performed in cases involving limited intra-abdominal DTs (7/15 [46.7%]). Seven of twelve (58.3%) patients who underwent complete resection also received medical treatment including NSAIDs (n = 6), and hormonal therapy (n = 5) as adjuvant therapy.
Pharmacological treatments
None of the patients who were treated with NSAIDs and/or hormonal therapy without chemotherapy showed a partial or complete response. Chemotherapy included cytotoxic agents and tyrosine kinase inhibitors. Overall, 19 treatment lines were administered to patients with DTs, these included 1st to 3rd line chemotherapy regimens (Table 3). Eleven treatment lines of cytotoxic chemotherapy achieved a response rate (RR) of 45.5% (5/11), and a progression-free or regression rate of 72.7% (8/11). Eight treatment lines that included tyrosine kinase inhibitors achieved an RR of 25.0% (2/8), and a progression-free or regression rate of 75.0% (6/8). Among the cytotoxic chemotherapy regimens, the most frequently used regimen was DTIC plus DOX (5 lines; RR, 40%); followed by MTX plus VBL (3 lines; RR, 66.7%). In our study, only 2 patients experienced severe toxicities, this included one patient who developed Grade 3 neutropenia while being treated with DTIC plus DOX, and one patient who developed Grade 4 neutropenia while being treated with MTX plus VBL. The others patients had no toxicities.
Survival
The median follow-up period from the initial colectomy for FAP was 53.0 months. Among the 302 patients with FAP, 4 died due to DTs and 16 died of other causes (CRC, n = 14; gastric cancer, n = 1; other malignancy, n = 1). There were no significant differences in the 5-year overall survival of patients with and without DTs (93.5 and 93.5%, respectively); however, the rate of CRC in patients with DTs was significantly lower than that in patients without DTs (37.5 vs. 64.3%; p = 0.0007). Furthermore, there were no significant differences in 5-year DT-specific survival between the patients whose DTs were diagnosed at colectomy and those who developed DTs after colectomy (83.3 and 96.4%, p = 0.7238). According to Church’s classification [12], the 5-year DT-specific survival in stages I, and III was 100%, while it was 71.4% in stage IV. The details of the 4 stage IV patients who died from their DTs are shown in Table 4. None of the 4 patients had malignancies (such as CRC). None of the patients was treated with cytotoxic chemotherapy; 2 of the patients underwent incomplete resection followed by hormonal therapy including NSAIDs; 1 received hormonal therapy including NSAIDs, and 1 underwent incomplete resection in combination with tyrosine kinase inhibitor treatment.
Discussion
The prevalence of DTs (15.8%) in our study was comparable to the previously reported prevalence (10–25.0%) [2]. In addition, 80.5% of our DT cases had intra-abdominal or mixed DTs. Intra-abdominal or mixed DTs were especially frequent among the patients who were diagnosed after the initial colectomy. This finding is in accordance with studies that show that sporadic DTs are often present in the abdominal wall and extremities, whereas FAP-associated DTs are mostly found in the abdominal cavity after prophylactic colectomy [13, 14]. There are few reports on the treatment of DTs in FAP patients; however, surgery has historically been the mainstay treatment for abdominal DTs. In the present study, surgery was frequently used for extra-abdominal DTs, with a high rate of complete resection (91.0%), while medical treatment was frequently administered to patients with intra-abdominal DTs. Because intra-abdominal DTs tend to occur at the root of the small bowel mesentery, surgery frequently involves the loss of significant amounts of small bowel. Indeed, Smith et al. reported morbidity and mortality rates of 19 and 29%, respectively, in cases involving intra-abdominal DTs, due to the need for extensive intestinal resection [15]. Thus, nonsurgical management including NSAIDs, hormonal therapy, and chemotherapy are now more frequently used for the treatment of intra-abdominal DTs [11].
NSAIDs and hormonal therapy are commonly used as pharmacological agents. FAP-associated DTs are known to express cyclooxygenase 2 [16]; NSAIDs, including sulindac, inhibit cyclooxygenase and prostaglandin synthase [17]. A few reports have shown NSAID use to be associated with the remarkable shrinkage of DTs. Nieuwenhuis et al. [18] reported on 12 patients who were treated with NSAIDs and demonstrated a 5-year progression-free survival rate of 50.0%. The rates of regression or stabilization of DTs in patients treated with NSAIDs are reported to range from 27.6 to 29.0% [5, 11]. In our study, NSAIDs were administered to 22 (62.9%) of the patients who received treatment for DTs. Only 7 patients received NSAIDs alone—these cases mainly involved extra-abdominal DTs. The other patients received NSAIDs in combination with hormonal therapy, chemotherapy, and/or surgery.
Tamoxifen and LH-RH agonists were used as hormonal therapy; both demonstrated selective effects on estrogen receptors. There are reports of the application of hormonal therapy in the treatment DTs. While a few cases in these reports showed the stabilization of DTs; however, most cases showed no remarkable shrinkage [5, 11, 18]. More recently, Quast et al. [19] reported 62 patients who were treated with hormonal therapy combined with sulindac, and showed a RR of 37.1% and a disease control rate of 88.7%. In our study, hormonal therapy was administered to 15 (42.9%) patients who received treatment for DTs, and 14 (93.4%) received hormonal therapy combined with other therapies. None of the patients who received NSAIDs and/or hormonal therapy without chemotherapy showed a partial response or complete response. It seems likely that neither hormonal therapy nor NSAIDs have the ability to induce significant shrinkage of DTs in FAP patients.
Recently, Desurmont et al. [11] conducted a comparative study to assess the results of the different treatments used for FAP-associated DTs. The RRs were as follows: cytotoxic chemotherapy (including DOX, MTX, VBL, and cisplatin), 77%; tamoxifen, 40%; and sulindac, 28%. These authors concluded that chemotherapy was the most effective treatment, especially for intra-abdominal DTs. Several combinations of cytotoxic agents have recently been reported to be safe and effective for the treatment of FAP-associated DTs [20–30]. The most commonly used regimens include DOX plus DTIC and MTX plus VBL chemotherapy. Table 5 shows the details of the cytotoxic chemotherapies that were administered to FAP patients with DTs in previous studies. Although the number of patients in each study was too small, favorable RRs of 33–100% and 40–75% were achieved with DOX-based and MTX-based chemotherapy regimens, respectively. Our results are consistent with these previous studies, and showed the safety of cytotoxic chemotherapy regimens, with a favorable RR (45.5%; for all regimens); the most frequently used regimen was DITC plus DOX (RR, 40%), followed by MTX plus VBL (RR, 67%).
In 2008, Church et al. [12] proposed a system for classifying intra-abdominal DTs into four stages based on the size, clinical presentation, and lesion severity, in an effort to optimize management through more defined guidelines (Fig. 2). Stage IV was the most advanced stage, with lesions measuring >20 cm, symptomatic disease, rapid growth, or intra-abdominal complications. In our study, the 5-year DT-specific survival was 100% in stage I–III, but only 71.4% in stage IV. Among our 302 patients, 4 with stage IV disease died as a result of their DTs. No cytotoxic chemotherapy was administered; however, 3 patients underwent incomplete resections in combination with other medical agents including NSAIDs, hormonal therapy, and tyrosine kinase inhibitors. All four patients died as a result of uncontrollable rapid progression, with a median DT-specific survival time of 12.4 months.
Based on these results, surgery as well as NSAIDs and hormonal therapy are considered the mainstay treatments for extra-abdominal DTs, and are able to stabilize DTs. However, we should consider the therapeutic approaches for intra-abdominal DTs, especially in cases involving stage IV disease, because it represents a potentially life-threatening condition. Harmful incomplete resection should be avoided, and the immediate use of cytotoxic chemotherapy may be important for achieving early tumor shrinkage in patients with stage IV DTs. Indeed, there is a report on the successful treatment of a 25-cm, extremely aggressive mesenteric DT by DOX plus DTIC [31].
The present study is associated with several limitations. First, our sample size was relatively too small—especially for the number of patients receiving each treatment—to draw any definitive conclusions. However, the present study was a nationwide multicenter study that included a relatively large number of patients with a rare disease, and the data derived from recent clinical practice is valuable. Second, the study was retrospective in nature. Ideally, our findings should be confirmed in a prospective study; however, this would be very difficult to achieve. Third, we did not collect the data related to the analysis of the patients’ APC genes because we could not obtain informed consent from the patients. Although the genotype-phenotype relationship is a well-known risk factor for DTs in FAP patients [32], the correlation between the specific APC mutation and the clinical outcomes has yet to be resolved. Fourth, we could not collect any data concerning the precise doses or schedules for each chemotherapy regimen or data on the detailed tumor size. Finally, the selection of surgical and/or medical treatments might have depended on the physician’s preference; and missing data, although limited, might have led to a bias in the interpretation of the results.
Nonetheless, to the best of our knowledge, this is the first study to analyze the outcomes of the surgical and pharmacological treatment of FAP-associated DTs in Japanese patients. We therefore believe that our findings will provide clues that will help physicians select the optimal treatment strategy for this rare disease.
In conclusion, a multimodal treatment approach that includes NSAIDs, hormonal therapy, chemotherapy, and surgery is important for FAP-associated DTs. Cytotoxic chemotherapy was found to be the most effective of these treatments, especially for intra-abdominal DTs. Because FAP-associated stage IV DTs are sometimes life-threatening, cytotoxic chemotherapy, which has the potential to result in early tumor shrinkage, may be important for achieving the best prognosis.
References
Hata K, Yamamoto Y, Kiyomatsu T, Tanaka T, Kazama S, Nozawa H, et al. Hereditary gastrointestinal cancer. Surg Today. 2016;46:1115–22.
Sturt NJ, Clark SK. Current ideas in desmoid tumours. Fam Cancer. 2006;5:275–85.
Sinha A, Tekkis PP, Gibbons DC, Phillips RK, Clark SK. Risk factors predicting desmoid occurrence in patients with familial adenomatous polyposis: a meta-analysis. Colorectal Dis. 2011;13:1222–9.
de Campos FG, Perez RO, Imperiale AR, Seid VE, Nahas SC, Cecconello I. Evaluating causes of death in familial adenomatous polyposis. J Gastrointest Surg. 2010;14:1943–9.
Clark SK, Neale KF, Landgrebe JC, Phillips RK. Desmoid tumours complicating familial adenomatous polyposis. Br J Surg. 1999;86:1185–9.
Latchford AR, Sturt NJ, Neale K, Rogers PA, Phillips RK. A 10-year review of surgery for desmoid disease associated with familial adenomatous polyposis. Br J Surg. 2006;93:1258–64.
Soravia C, Berk T, McLeod RS, Cohen Z. Desmoid disease in patients with familial adenomatous polyposis. Dis Colon Rectum. 2000;43:363–9.
Berk T, Cohen Z, McLeod RS, Stern HS. Management of mesenteric desmoid tumours in familial adenomatous polyposis. Can J Surg. 1992;35:393–5.
Schnitzler M, Cohen Z, Blackstein M, Berk T, Gallinger S, Madlensky L, et al. Chemotherapy for desmoid tumors in association with familial adenomatous polyposis. Dis Colon Rectum. 1997;40:798–801.
Gega M, Yanagi H, Yoshikawa R, Noda M, Ikeuchi H, Tsukamoto K, et al. Successful chemotherapeutic modality of doxorubicin plus dacarbazine for the treatment of desmoid tumors in association with familial adenomatous polyposis. J Clin Oncol. 2006;24:102–5.
Desurmont T, Lefèvre JH, Shields C, Colas C, Tiret E, Parc Y. Desmoid tumour in familial adenomatous polyposis patients: responses to treatments. Fam Cancer. 2015;14:31–9.
Church J, Lynch C, Neary P, LaGuardia L, Elayi E. A desmoid tumor-staging system separates patients with intra-abdominal, familial adenomatous polyposis-associated desmoid disease by behavior and prognosis. Dis Colon Rectum. 2008;51:897–901.
Nieuwenhuis MH, Lefevre JH, Bülow S, Järvinen H, Bertario L, Kernéis S, et al. Family history, surgery, and APC mutation are risk factors for desmoid tumors in familial adenomatous polyposis: an international cohort study. Dis Colon Rectum. 2011;54:1229–34.
Lynch HT, Fitzgibbons R Jr. Surgery, desmoid tumors, and familial adenomatous polyposis: case report and literature review. Am J Gastroenterol. 1996;91:2598–601.
Smith AJ, Lewis JJ, Merchant NB, Leung DH, Woodruff JM, Brennan MF. Surgical management of intra-abdominal desmoid tumours. Br J Surg. 2000;87:608–13.
Colombo C, Foo WC, Whiting D, Young ED, Lusby K, Pollock RE, et al. FAP-related desmoid tumors: a series of 44 patients evaluated in a cancer referral center. Histol Histopathol. 2012;27:641–9.
Vasen HF, Möslein G, Alonso A, Aretz S, Bernstein I, Bertario L, et al. Guidelines for the clinical management of familial adenomatous polyposis (FAP). Gut. 2008;57:704–13.
Nieuwenhuis MH, Mathus-Vliegen EM, Baeten CG, Nagengast FM, van der Bijl J, van Dalsen AD, et al. Evaluation of management of desmoid tumours associated with familial adenomatous polyposis in Dutch patients. Br J Cancer. 2011;104:37–42.
Quast DR, Schneider R, Burdzik E, Hoppe S, Möslein G. Long-term outcome of sporadic and FAP-associated desmoid tumors treated with high-dose selective estrogen receptor modulators and sulindac: a single-center long-term observational study in 134 patients. Fam Cancer. 2016;15:31–40.
Tsukada K, Church JM, Jagelman DG, Fazio VW, Lavery IC. Systemic cytotoxic chemotherapy and radiation therapy for desmoid in familial adenomatous polyposis. Dis Colon Rectum. 1991;34:1090–2.
Patel SR, Benjamin RS. Desmoid tumors respond to chemotherapy: defying the dogma in oncology. J Clin Oncol. 2006;24:11–2.
Lynch HT, Fitzgibbons R Jr, Chong S, Cavalieri J, Lynch J, Wallace F, et al. Use of doxorubicin and dacarbazine for the management of unresectable intra-abdominal desmoid tumors in Gardner’s syndrome. Dis Colon Rectum. 1994;37:260–7.
Hamilton L, Blackstein M, Berk T, McLeod RS, Gallinger S, Madlensky L, et al. Chemotherapy for desmoid tumours in association with familial adenomatous polyposis: a report of three cases. Can J Surg. 1996;39:247–52.
Poritz LS, Blackstein M, Berk T, Gallinger S, McLeod RS, Cohen Z. Extended follow-up of patients treated with cytotoxic chemotherapy for intra-abdominal desmoid tumors. Dis Colon Rectum. 2001;44:1268–73.
Yamamoto H, Oshiro R, Nishimura J, Uemura M, Haraguchi N, Hata T, et al. Low-dose dacarbazine-doxorubicin therapy against intra-abdominal desmoid tumors. Oncol Rep. 2013;29:1751–5.
Weiss AJ, Lackman RD. Low-dose chemotherapy of desmoid tumors. Cancer. 1989;64:1192–4.
Skapek SX, Hawk BJ, Hoffer FA, Dahl GV, Granowetter L, Gebhardt MC et al. Combination chemotherapy using vinblastine and methotrexate for the treatment of progressive desmoid tumor in children. J Clin Oncol. 1998;16:3021–7.
Reich S, Overberg-Schmidt US, Bührer C, Henze G. Low-dose chemotherapy with vinblastine and methotrexate in childhood desmoid tumors. J Clin Oncol. 1999;17:1086.
Azzarelli A, Gronchi A, Bertulli R, Tesoro JD, Baratti D, Pennacchioli E, et al. Low-dose chemotherapy with methotrexate and vinblastine for patients with advanced aggressive fibromatosis. Cancer. 2001;92:1259–64.
Weiss AJ, Horowitz S, Lackman RD. Therapy of desmoid tumors and fibromatosis using vinorelbine. Am J Clin Oncol. 1999;22:193–5.
Ezumi K, Yamamoto H, Takemasa I, Nomura M, Ikeda M, Sekimoto M, et al. Dacarbazine-Doxorubicin therapy ameliorated an extremely aggressive mesenteric desmoid tumor associated with familial adenomatous polyposis: report of a case. Jpn J Clin Oncol. 2008;38:222–6.
Slowik V, Attard T, Dai H, Shah R, Septer S. Desmoid tumors complicating Familial Adenomatous Polyposis: a meta-analysis mutation spectrum of affected individuals. BMC Gastroenterol. 2015;15:84.
Acknowledgements
The authors would like to acknowledge all of the patients and their families. In addition to the investigators in the author list, we acknowledge the following investigators who participated in this study: Koji Komori, Department of Gastroenterological Surgery Aichi Cancer Center Hospital, Aichi; Kenjiro Kotake, Department of Surgery, Tochigi Cancer Center, Tochigi; Takeshi Nagasaka, Department of Gastroenterological Surgery, Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Sciences, Okayama; Hirotoshi Hasegawa, Department of Surgery, Keio University School of Medicine, Tokyo; Motoi Koyama, Department of Gastroenterological Surgery, Hirosaki University Graduate School of Medicine, Aomori; Yoshito Akagi, Department of Surgery, Kurume University School of Medicine, Kurume, Fukuoka; Toshimasa Yatsuoka, Department of Gastroenterological Surgery, Saitama Cancer Center, Saitama; Masataka Ikeda, Department of Surgery, National Hospital Organization, Osaka National Hospital, Osaka; Kensuke Kumamoto, Department of Organ Regulatory Surgery, Fukushima Medical University School of Medicine, Fukushima; Kiyotaka Kurachi, Department of Surgery 2, Hamamatsu University School of Medicine, Shizuoka;Toshiaki Watanabe, Department of Surgical Oncology, Graduate School of Medicine, The University of Tokyo, Tokyo; Kohji Tanakaya, Department of Surgery, Iwakuni Clinical Center, Yamaguchi; Kazuhiko Yoshimatsu, Department of Surgery, Tokyo Women’s Medical University Medical Center East, Tokyo.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The present study was supported in part by a grant-in-aid for Cancer Research from the Ministry of Health, Labor and Welfare, and by the Japanese Society for Cancer of the Colon and Rectum.
Conflict of interest
The authors declare no conflicts of interest in association with the present study.
Rights and permissions
About this article
Cite this article
Inoue, Y., Ishida, H., Ueno, H. et al. The treatment of desmoid tumors associated with familial adenomatous polyposis: the results of a Japanese multicenter observational study. Surg Today 47, 1259–1267 (2017). https://doi.org/10.1007/s00595-017-1500-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-017-1500-3